Children’s Perceptions of Dental Experiences and Ways to Improve Them
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Participants
2.2. Study Parameters
2.3. Sample Size
2.4. Conceptual Frameworks and Data Analysis
3. Results
3.1. Description of Participant Characteristics
3.2. Description of Themes, Subthemes, and Associated Sample Participant Quotes
3.2.1. Theme 1: Establishing a Therapeutic Relationship
Dental Team Characteristics
“They comforted me. They let me squeeze their hands. I was really scared. They helped me get through it. They were kind.”P3
“They ask basic questions every time I go there. The same questions over and over again. It gets boring. I wish they would ask me personal questions and tell me about themselves.”P2
Effective Open Communication
“It made me feel nervous at first. But [the dentist] always listened to what you were saying, and they never ignored you. They kept the conversations going. I felt happy because there were finally some people who understood what I was talking about, and they really listened to me.”P11
3.2.2. Theme 2: Shared Power and Responsibility
Personal Autonomy and Advocacy
“I would like to pick the flavours of polishing paste/topical fluoride. It would make my mouth more comfortable since I cannot eat anything.”P2
“Sometimes using the suction makes your mouth really dry. Closing your mouth is helpful, but most times it is not possible because your mouth must be open, making your mouth dry. A few times I asked to get it removed. [When the dentist removed it], it was better because my mouth felt normal again.”P4
Self-Directed Support
“By breathing it takes my mind off of some of the stuff that hurts, and I feel better.”P8
“It’s just part of life [dealing with unpleasant experiences]. You are going to have to deal with it. It doesn’t matter if it hurts. So, before [the treatment] I get my body prepared. [This way] I can be calm, and focus. That will help me get ready for it.”P11
3.2.3. Theme 3: Getting to Know the Person
Participants’ Lived Experiences
“There are lots of chairs next to each other and there is nothing to do there. You are just thinking and waiting for your appointment.”P12
“The drill is the scariest part because it’s very sharp and has a loud sound.”P4
“The medicine from the needle was really uncomfortable. I felt weird stuff coming into my mouth and it just tasted bitter.”P5
“I think the X-ray machine would bump into me, and I would fall, hit my head or get hurt.”P7
“Well, with the needles I was really scared. I am afraid of getting the flu shot, and it reminded me of that. So, I didn’t want to do it.”P3
“Some people get scared [during their dental visits], and they cannot let their feelings out because people are looking at them. Instead of fearing everything they can have privacy.”P3
Participants’ Wishes, Needs, and Values
“We could set up a few drawing activities in the corner, this way the children would have something to do instead of just being bored of waiting.”P4
“If there’s more laughing gas and we could use laughing gas a little bit more often for the freezing.”P5
“…Maybe not having them see the needle or having them distracted is much more helpful. You could have them [the dentist] talk about something else so that they don’t have to worry about the needle at all.”P4
“The paper film cuts my mouth and is close to my throat. It feels like I am going to swallow it. Maybe they can put a clip or something soft on it.”P2
“The dentist can explain steps and show the materials that they have so you know they don’t hurt. That way you are not nervous and know you will be okay.”P12
“Maybe the dentists can show me the tools that they are using. Maybe I can hold some of the instruments that way I would not fear them. It would help if they showed me the tools and let me hold them.”P8
“Having my parents there would make me feel safe. When they are there, nothing would happen to me.”P9
“I am used to having my mom stay with me. I get really nervous if I am around people and my mom isn’t there. Having her there makes me comfortable because I am used to seeing her.”P3
3.2.4. Theme 4: Empowering the Person
The CARD™ System
“CARD™ is really good. I [get] to choose my own favourite cards and choose when to use it on my own and where I would do it.”P10
“The CARD™ system was very great. You can have Ask, Comfort, Relax, and Distract, they are very good if you’re very scared, stressed, or tired. It’s a very good improvement for the dentist.”P12
Coping Strategies
“The dental X-ray makes me uncomfortable. I want to ask, ‘Can I see what the dentist is doing?’ so I can know what’s going to happen in advance and have the dentist tell me what actually is going to happen.”P2
“For the dental suction, I would say ‘How will it feel?’ That way I would be prepared for it, so if I had the dental suctioning I would not freak out.”P11
“My favourite card would behaving a favourite object or toy like a stress ball or squishy, just because when you are really stressed, having that object in your hand and squishing it diverts your mind off of it.”P4
“I like to take deep belly breaths. some deep breaths can help you calm yourself down if you are stressed or scared to go [see the dentist]. You can take deep breaths that way you know you are going to be okay and that everything is going to be fine.”P12
“I want my parents to sit next to me. That way I would not be scared,because my mom makes me comfortable and I know if I feel something wrong, my parents will help me.”P8
(i) Distraction
“I would like towatch a movie or have a video to distract me. That way I would be distracted from anything I’m worrying about if I’m sitting on a chair waiting for what is going to happen.”P11
“I can listen to music. I can concentrate on the music and not think about what would happen and feel calm.”P10
(ii) Nitrous Oxide Sedation
“I want the laughing gas. I think it helped a lot. When they gave me the needle, I felt the pain. But with the laughing gas I didn’t feel anything. It was a lot more comfortable than the needle.”P5
(iii) Treatment Breaks
“Before treatment, I want a break so I can think about things, take a deep breath so that you are ready if something bad is about to happen.”P6
“I want to ask to take breaks. Sometimes it gets really tiring to stay [with my mouth] open in one position for a long time.”P4
(iv) Privacy
“It would be the privacy; you don’t want other people looking at you or worrying about you. So, I prefer privacy.”P3
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Klingberg, G.; Broberg, A.G. Dental fear/anxiety and dental behaviour management problems in children and adolescents: A review of prevalence and concomitant psychological factors. Int. J. Paediatr. Dent. 2007, 17, 391–406. [Google Scholar] [CrossRef] [PubMed]
- Cianetti, S.; Lombardo, G.; Lupatelli, E.; Pagano, S.; Abraha, I.; Montedori, A.; Caruso, S.; Gatto, R.; De Giorgio, S.; Salvato, R. Dental fear/anxiety among children and adolescents. A systematic review. Eur. J. Paediatr. Dent. 2017, 18, 121–130. [Google Scholar] [PubMed]
- Asl, A.; Shokravi, M.; Jamali, Z.; Shirazi, S. Barriers and drawbacks of the assessment of dental fear, dental anxiety and dental phobia in children: A critical literature review. J. Clin. Pediatr. Dent. 2017, 41, 399–423. [Google Scholar] [CrossRef] [PubMed]
- Appukuttan, D. Strategies to manage patients with dental anxiety and dental phobia: Literature review. Cosmet. Investig. Dent. 2016, 8, 35–50. [Google Scholar] [CrossRef] [PubMed]
- Abrahamsson, K.; Berggren, U.; Hallberg, L.; Carlsson, S. Ambivalence in coping with dental fear and avoidance: A qualitative study. J. Health Psychol. 2002, 7, 653–664. [Google Scholar] [CrossRef]
- Bedi, R.; Sutcliffe, P.; Donnan, P.; McConnachie, J. The prevalence of dental anxiety in a group of 13-and 14-year-old Scottish children. Int. J. Paediatr. Dent. 1992, 2, 17–24. [Google Scholar] [CrossRef]
- Kakkar, M.; Wahi, A.; Thakkar, R.; Vohra, I.; Shukla, A. Prevalence of dental anxiety in 10–14 years old children and its implications. J. Clin. Anesth. Pain Med. 2016, 16, 199–202. [Google Scholar] [CrossRef]
- Van Meurs, P.; Howard, K.; Versloot, J.; Veerkamp, J.; Freeman, R. Child coping strategies, dental anxiety and dental treatment: The influence of age, gender and childhood caries prevalence. Eur. J. Paediatr. Dent. 2005, 6, 173–178. [Google Scholar] [PubMed]
- Ray, J.; Boman, U.; Bodin, L.; Berggren, U.; Lichtenstein, P.; Broberg, A. Heritability of dental fear. J. Dent. Res. 2010, 89, 297–301. [Google Scholar] [CrossRef] [PubMed]
- Nicolas, E.; Bessadet, M.; Collado, V.; Carrasco, P.; Rogerleroi, V.; Hennequin, M. Factors affecting dental fear in French children aged 5–12 years. Int. J. Paediatr. Dent. 2010, 20, 366–373. [Google Scholar] [CrossRef]
- Klingberg, G. Dental anxiety and behaviour management problems in paediatric dentistry—A review of background factors and diagnostics. Eur. Arch. Dent. 2008, 9, 11–15. [Google Scholar] [CrossRef]
- Campbell, C. Dental Fear and Anxiety in Pediatric Patients: Practical Strategies to Help Children Cope, 3rd ed.; Springer: Gewerbestrasse, Switzerland, 2017; pp. 3–152. [Google Scholar]
- Peretz, B.; Kharouba, J. Dental anxiety among Israeli children and adolescents in a dental clinic waiting room. Pediatr. Dent. 2013, 35, 252–256. [Google Scholar] [PubMed]
- Gustafsson, A.; Broberg, A.; Bodin, L.; Berggren, U.; Arnrup, K. Dental behaviour management problems: The role of child personal characteristics. Int. J. Paediatr. Dent. 2010, 20, 242–253. [Google Scholar] [CrossRef] [PubMed]
- Locker, D.; Liddell, A.; Dempster, L.; Shapiro, D. Age of onset of dental anxiety. J. Dent. Res. 1999, 78, 790–796. [Google Scholar] [CrossRef] [PubMed]
- Klingberg, G.; Broberg, A. Temperament and child dental fear. Pediatr. Dent. 1998, 20, 237–243. [Google Scholar] [PubMed]
- Murad, M.; Ingle, N.; Assery, M. Evaluating factors associated with fear and anxiety to dental treatment—A systematic review. J. Fam. Med. Prim. Care 2020, 9, 4530–4535. [Google Scholar] [CrossRef] [PubMed]
- Armfield, J.; Heaton, L. Management of fear and anxiety in the dental clinic: A review. Aust. Dent. J. 2013, 58, 390–407. [Google Scholar] [CrossRef] [PubMed]
- Van Wijk, A.; Hoogstraten, J. Anxiety and pain during dental injections. J. Dent. 2009, 37, 700–704. [Google Scholar] [CrossRef]
- Van Wijk, A.; Makkes, P. Highly anxious dental patients report more pain during dental injections. Br. Dent. J. 2008, 205, 142–143. [Google Scholar] [CrossRef] [PubMed]
- Armfield, J.; Stewart, J.; Spencer, A. The vicious cycle of dental fear: Exploring the interplay between oral health, service utilization and dental fear. BMC Oral Health 2007, 7, 1–15. [Google Scholar] [CrossRef]
- De Jongh, A.; Adair, P.; Meijerink-Anderson, M. Clinical management of dental anxiety: What works for whom? Int. Dent. J. 2005, 55, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Morgan, A.; Rodd, H.; Porritt, J.; Baker, S.; Creswell, C.; Newton, T.; Williams, C.; Marshman, Z. Children’s experiences of dental anxiety. Int. J. Paediatr. Dent. 2017, 27, 87–97. [Google Scholar] [CrossRef] [PubMed]
- Aartman, I.; Hoogstraten, J.; Schuurs, A. Self-report measurements of dental anxiety and fear in children: A critical assessment. ASDC J. Dent. Child. 1998, 65, 252–258. [Google Scholar] [PubMed]
- Yon, M.; Chen, K.; Gao, S.; Duangthip, D.; Lo, E.; Chu, C. An introduction to assessing dental fear and anxiety in children in healthcare. Healthcare 2020, 8, 86. [Google Scholar] [CrossRef]
- Gao, X.; Hamzah, S.; Yiu, C.; McGrath, C.; King, N. Dental fear and anxiety in children and adolescents: Qualitative study using YouTube. J. Med. Internet Res. 2013, 15, e2290. [Google Scholar] [CrossRef]
- Jones, L.; Huggins, T. The rationale and pilot study of a new paediatric dental patient request form to improve communication and outcomes of dental appointments. Child Care Health Dev. 2013, 39, 869–872. [Google Scholar] [CrossRef]
- Jones, L. Validation and randomized control trial of the e-SAID, a computerized paediatric dental patient request form, to intervene in dental anxiety. Child Care Health Dev. 2015, 41, 620–625. [Google Scholar] [CrossRef] [PubMed]
- Rodd, H.; Timms, L.; Noble, F.; Bux, S.; Porritt, J.; Marshman, Z. ‘Message to dentist’: Facilitating communication with dentally anxious children. Dent. J. 2019, 7, 69. [Google Scholar] [CrossRef]
- Noble, F.; Kettle, J.; Hulin, J.; Morgan, A.; Rodd, H.; Marshman, Z. ‘I would rather be having my leg cut off than a little needle’: A supplementary qualitative analysis of dentally anxious children’s experiences of needle fear. Dent. J. 2020, 8, 50. [Google Scholar] [CrossRef] [PubMed]
- Abrahamsson, K.; Berggren, U.; Hallberg, L.; Carlsson, S. Dental phobic patients’ view of dental anxiety and experiences in dental care: A qualitative study. Scand. J. Caring Sci. 2002, 16, 188–196. [Google Scholar] [CrossRef] [PubMed]
- Wilson, S.; Cody, W. An analysis of behavior management papers published in the pediatric dental literature. Pediatr. Dent. 2005, 27, 331–338. [Google Scholar] [PubMed]
- Ten Berge, M. Dental fear in children: Clinical consequences. Suggested behaviour management strategies in treating children with dental fear. Eur. Arch. Paediatr. Dent. 2008, 9, 41–46. [Google Scholar] [CrossRef]
- Freedman, T.; Taddio, A.; McMurtry, C.M.; Wong, H.; MacDonald, N.; McDowall, T.; deVlaming-Kot, C.; Alderman, L. Pain Pain Go Away Team. Involving stakeholders in informing the development of a knowledge translation (KT) intervention to improve the vaccination experience at school. Paediatr. Child Health 2019, 24, S19–S28. [Google Scholar] [CrossRef] [PubMed]
- Taddio, A.; Alderman, L.; Freedman, T.; McDowall, T.; McMurtry, C.; MacDonald, N.; DeVlaming-Kot, C.; Alfieri-Maiolo, A. The CARD™ system for improving the vaccination experience at school: Results of a small-scale implementation project on program delivery. J. Paediatr. Child Health 2019, 24, S54–S67. [Google Scholar] [CrossRef] [PubMed]
- Taddio, A.; Gudzak, V.; Jantzi, M.; Logeman, C.; Bucci, L.; MacDonald, N.; Moineddin, R. Impact of the CARD (Comfort Ask Relax Distract) system on school-based vaccinations: A cluster randomized trial. Vaccine 2022, 40, 2802–2809. [Google Scholar] [CrossRef] [PubMed]
- Taddio, A.; Ilersich, A.; Ilersich, A.; Schmidt, C.; Chalmers, G.; Wilson, E.; McMurtry, C.; MacDonald, N.; Bucci, L.; Freedman, T.; et al. Piloting the CARD™ system for education of students about vaccination: Does it improve the vaccination experience at school? J. Paediatr. Child Health 2019, 24, S35–S41. [Google Scholar] [CrossRef]
- Taddio, A.; McMurtry, C.; Bucci, L.; MacDonald, N.; Ilersich, A.; Ilersich, A.; Alfieri-Maiolo, A.; DeVlaming-Kot, C.; Alderman, L.; BAS McDowall, T.; et al. Overview of a knowledge translation (KT) project to improve the vaccination experience at school: The CARD™ system. J. Paediatr. Child Health 2019, 24, S3–S18. [Google Scholar] [CrossRef]
- Rebok, G.; Riley, A.; Forrest, C.; Starfield, B.; Green, B.; Robertson, J.; Tambor, E. Elementary school-aged children’s reports of their health: A cognitive interviewing study. Qual. Life Res. 2001, 10, 59–70. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V.; Weate, P. Using thematic analysis in sport and exercise research. In Routledge Handbook of Qualitative Research in Sport and Exercise; Smith, B., Sparkes, A.C., Eds.; Routledge: London, UK, 2016; pp. 213–227. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Francis, J.; Johnston, M.; Robertson, C.; Glidewell, L.; Entwistle, V.; Eccles, M.; Grimshaw, J. What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol. Health 2010, 25, 1229–1245. [Google Scholar] [CrossRef]
- Shahnavaz, S.; Rutley, S.; Larsson, K.; Dahllöf, G. Children and parents’ experiences of cognitive behavioral therapy for dental anxiety–a qualitative study. Int. J. Paediatr. Dent. 2015, 25, 317–326. [Google Scholar] [CrossRef] [PubMed]
- Sharma, T.; Bamford, M.; Dodman, D. Person-centred care: An overview of reviews. Contemp. Nurse 2015, 51, 107–120. [Google Scholar] [CrossRef]
- Hsieh, H.; Shannon, S. Three approaches to qualitative content analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef] [PubMed]
- Mayring, P. Qualitative content analysis. Companion Qual. Res. 2004, 1, 159–176. [Google Scholar]
- Zhou, Y.; Cameron, E.; Forbes, G.; Humphris, G. Systematic review of the effect of dental staff behaviour on child dental patient anxiety and behaviour. Patient Educ. Couns. 2011, 85, 4–13. [Google Scholar] [CrossRef]
- Hamasaki, T.; Soh, I.; Takehara, T.; Hagihara, A. Applicability of both dentist and patient perceptions of dentists’ explanations to the evaluation of dentist-patient communication. Community Dent. Health 2011, 28, 274–279. [Google Scholar] [PubMed]
| Dental Procedure and Description | Associated Questions |
|---|---|
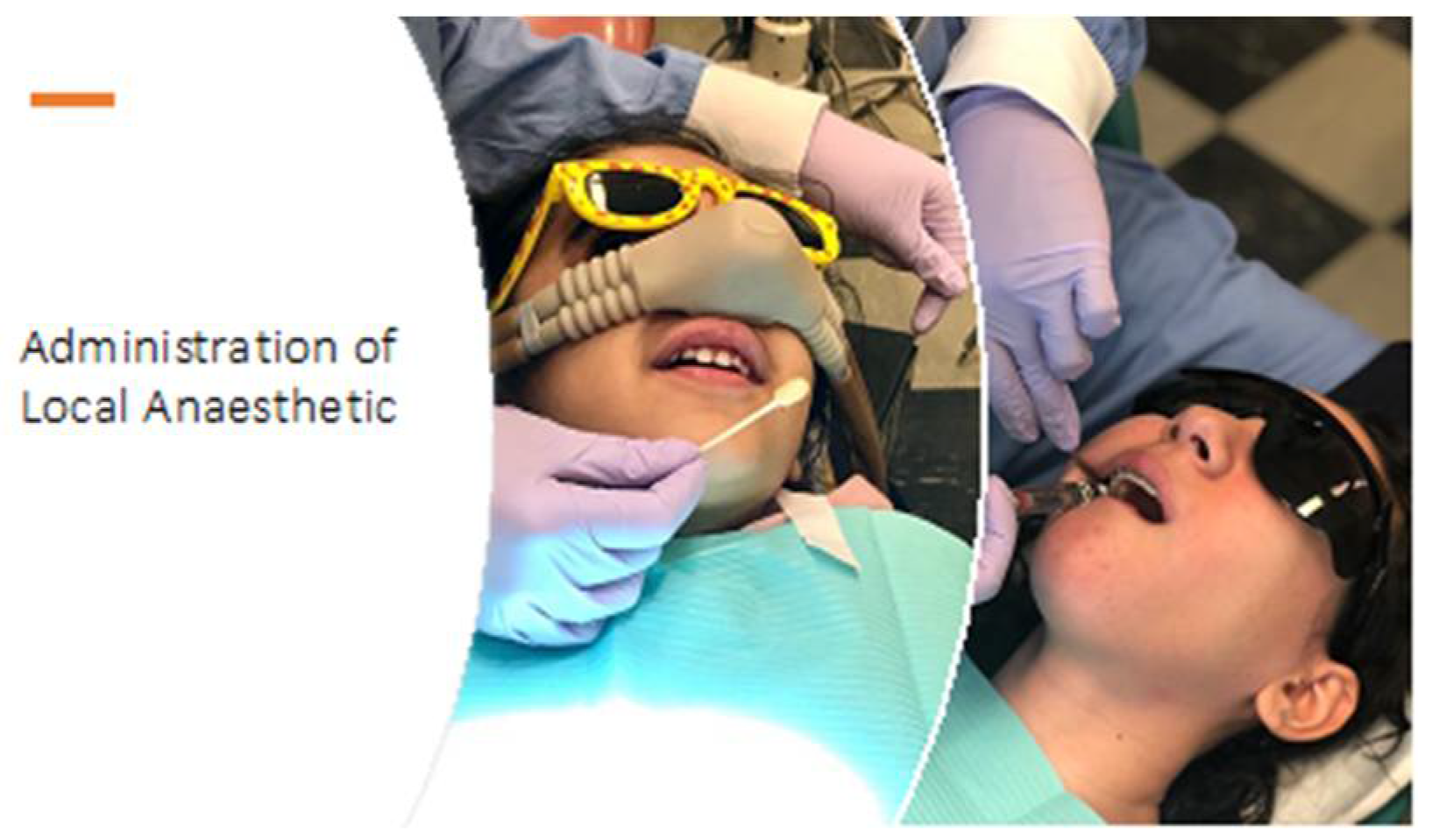
| Administration of local anaesthetic Sometimes the dentist puts your tooth/teeth to sleep for a while so they can fix them without bothering you. To do this, they first apply a jelly beside your tooth which numbs the area. Then, they give you a needle. | Do you remember ever having the dentist put your tooth/teeth to sleep? If NO, then move to the next question. If YES, proceed with the questions below:
|
| CARD™ Letter Category | Coping Options |
|---|---|
| Comfort | ○ Wear comfortable clothing |
| ○ Have a parent sit next to you | |
| ○ Have a parent comfort you (hold your hand or rub your shoulder) | |
| ○ Hold a favourite object or toy | |
| ○ Have privacy | |
| Ask | ○ Why am I going? |
| ○ What will happen? | |
| ○ Can I see what the dentist is doing? | |
| ○ How long will it take? | |
| ○ How will it feel? | |
| ○ Can I take breaks? | |
| ○ How will the dentist know when I want to take a break? | |
| ○ Can my parents stay? | |
| ○ Can I bring a favourite object or toy? | |
| ○ Can I wear the ‘astronaut nose’ (laughing gas)? * | |
| ○ What will the ‘astronaut nose’ feel like? * | |
| Relax | ○ Take deep belly breaths (pretend you are blowing a balloon) |
| ○ Do some self-talk (tell yourself you can handle this) | |
| ○ Wear the ‘astronaut nose’ (laughing gas) * | |
| ○ Have a parent stay with you | |
| ○ Have the dentist help you practice relaxation techniques | |
| ○ Tense your muscles to prevent dizziness | |
| Distract | ○ Listen to the dentist tell stories, jokes or sing |
| ○ Listen to a parent tell stories, jokes or sing | |
| ○ Watch a movie or video | |
| ○ Listen to audiobook or music with headphones | |
| ○ Hold your favourite object or toy | |
| ○ Allow yourself to daydream |
| Mean (SD) or Frequency (%) | |
|---|---|
| Gender, male | 7 (58%) |
| Age, years | 9.8 (1.48) |
| Ethnicity Asian (South Asian/West Asian) White/European Black/African/Caribbean Mixed Ethnicity | 5 (42%) 3 (25%) 2 (17%) 2 (17%) |
| Total number of visits | 8.5 (9.02) |
| Types of visits Invasive procedures 1 Non-invasive procedures 2 | 9 (75%) 3 (25%) |
| Themes | Subthemes and Descriptions |
|---|---|
|
|
|
|
|
|
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Modabber, M.; Campbell, K.M.; McMurtry, C.M.; Taddio, A.; Dempster, L.J. Children’s Perceptions of Dental Experiences and Ways to Improve Them. Children 2022, 9, 1657. https://doi.org/10.3390/children9111657
Modabber M, Campbell KM, McMurtry CM, Taddio A, Dempster LJ. Children’s Perceptions of Dental Experiences and Ways to Improve Them. Children. 2022; 9(11):1657. https://doi.org/10.3390/children9111657
Chicago/Turabian StyleModabber, Melika, Karen M. Campbell, C. Meghan McMurtry, Anna Taddio, and Laura J. Dempster. 2022. "Children’s Perceptions of Dental Experiences and Ways to Improve Them" Children 9, no. 11: 1657. https://doi.org/10.3390/children9111657
APA StyleModabber, M., Campbell, K. M., McMurtry, C. M., Taddio, A., & Dempster, L. J. (2022). Children’s Perceptions of Dental Experiences and Ways to Improve Them. Children, 9(11), 1657. https://doi.org/10.3390/children9111657







