Improved Mortality of Patients with Gastroschisis: A Historical Literature Review of Advances in Surgery and Critical Care from 1960–2020
Abstract
:1. Introduction
2. Materials and Methods
3. Results
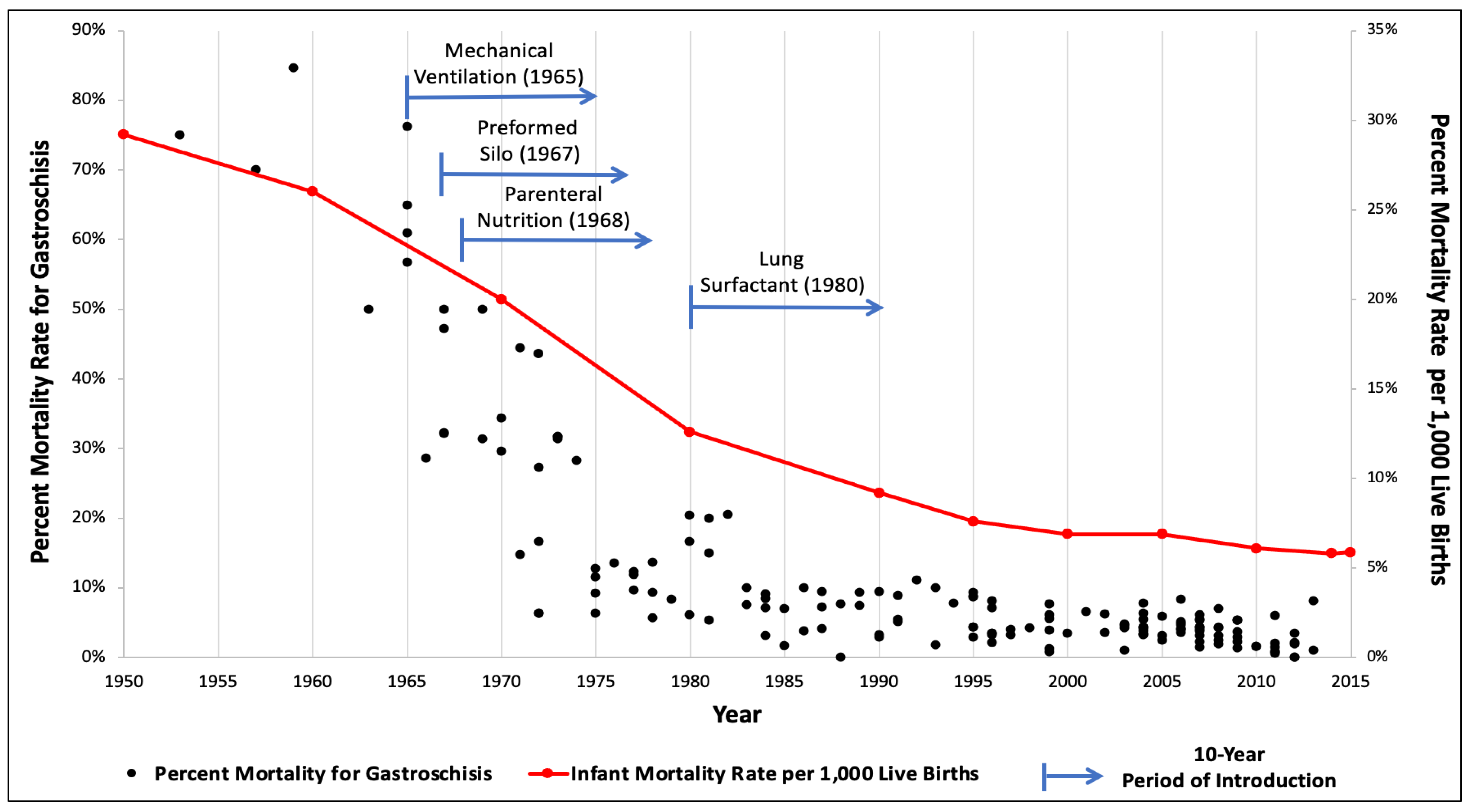
3.1. Improved Survival in Gastroschisis Infants
3.2. Implementation of Clinical Interventions
3.3. Current and Future Considerations
3.3.1. Timing of Delivery
3.3.2. Complex Gastroschisis
3.3.3. Low- and Middle-Income Countries
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Witt, R.G.; Zobel, M.; Padilla, B.; Lee, H.; MacKenzie, T.C.; Vu, L. Evaluation of Clinical Outcomes of Sutureless vs. Sutured Closure Techniques in Gastroschisis Repair. JAMA Surg. 2019, 154, 33. [Google Scholar] [CrossRef]
- Anderson, J.E.; Galganski, L.A.; Cheng, Y.; Stark, R.A.; Saadai, P.; Stephenson, J.T.; Hirose, S. Epidemiology of gastroschisis: A population-based study in California from 1995 to 2012. J. Pediatr. Surg. 2018, 53, 2399–2403. [Google Scholar] [CrossRef]
- Arnold, H.E.; Baxter, K.J.; Short, H.L.; Travers, C.; Bhatia, A.; Durham, M.M.; Raval, M.V. Short-term and family-reported long-term outcomes of simple versus complicated gastroschisis. J. Surg. Res. 2018, 224, 79–88. [Google Scholar] [CrossRef]
- Friedman, A.M.; Ananth, C.V.; Siddiq, Z.; D’Alton, M.E.; Wright, J.D. Gastroschisis: Epidemiology and mode of delivery, 2005–2013. Am. J. Obstet. Gynecol. 2016, 215, 348.e1–348.e9. [Google Scholar] [CrossRef]
- Jones, A.M.; Isenburg, J.; Salemi, J.; Arnold, K.E.; Mai, C.T.; Aggarwal, D.; Arias, W.; Carrino, G.E.; Ferrell, E.; Folorunso, O.; et al. Increasing Prevalence of Gastroschisis—14 States, 1995–2012. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 23–26. [Google Scholar] [CrossRef]
- South, A.P.; Stutey, K.M.; Meinzen-Derr, J. Metaanalysis of the prevalence of intrauterine fetal death in gastroschisis. Am. J. Obstet. Gynecol. 2013, 209, 114.e1–114.e13. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention, National Center for Health Statistics. Table 11. Infant Mortality Rates, by Race: United States, Selected Years 1950–2015; Centers for Disease Control and Prevention, National Center for Health Statistics: Atlanta, GA, USA, 2016. Available online: https://www.cdc.gov/nchs/data/hus/2016/011.pdf (accessed on 26 January 2022).
- Thomas, D.V.; Fletcher, G.; Sunshine, P.; Schafer, I.A.; Klaus, M.H. Prolonged respirator use in pulmonary insufficiency of newborn. JAMA 1965, 193, 183–190. [Google Scholar] [CrossRef] [PubMed]
- Schuster, S.R. A new method for the staged repair of large omphaloceles. Surg. Gynecol. Obstet. 1967, 125, 837–850. [Google Scholar]
- Wilmore, D.W.; Dudrick, S.J. Growth and development of an infant receiving all nutrients exclusively by vein. JAMA 1968, 203, 860–864. [Google Scholar] [CrossRef]
- Fujiwara, T.; Chida, S.; Watabe, Y.; Maeta, H.; Morita, T.; Abe, T. Artificial surfactant therapy in hyaline-membrane disease. Lancet 1980, 315, 55–59. [Google Scholar] [CrossRef]
- Donald, I.; Lord, J. Augmented respiration studies in atelectasis neonatorum. Lancet 1953, 261, 9–17. [Google Scholar] [CrossRef]
- Skarsgard, E.D. Management of gastroschisis. Curr. Opin. Pediatr. 2016, 28, 363–369. [Google Scholar] [CrossRef]
- Moore, T.C.; Stokes, G.E. Gastroschisis: Report of two cases treated by a modification of the gross operation for omphalocele. Surgery 1953, 33, 112–120. [Google Scholar]
- Shermeta, D.W.; Haller, J.A., Jr. A new preformed transparent silo for the management of gastroschisis. J. Pediatr. Surg. 1975, 10, 973–975. [Google Scholar] [CrossRef]
- Lansdale, N.; Hill, R.; Gull-Zamir, S.; Drewett, M.; Parkinson, E.; Davenport, M.; Sadiq, J.; Lakhoo, K.; Marven, S. Staged reduction of gastroschisis using preformed silos: Practicalities and problems. J. Pediatr. Surg. 2009, 44, 2126–2129. [Google Scholar] [CrossRef]
- Kunz, S.N.; Tieder, J.S.; Whitlock, K.; Jackson, J.C.; Avansino, J.R. Primary fascial closure versus staged closure with silo in patients with gastroschisis: A meta-analysis. J. Pediatr. Surg. 2013, 48, 845–857. [Google Scholar] [CrossRef]
- Schlatter, M. Preformed silos in the management of gastroschisis: New progress with an old idea. Curr. Opin. Pediatr. 2003, 15, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Blane, C.; Wesley, J.R.; DiPietro, M.; White, S.; Coran, A. Gastrointestinal complications of gastroschisis. Am. J. Roentgenol. 1985, 144, 589–591. [Google Scholar] [CrossRef]
- Phillips, J.D.; Raval, M.V.; Redden, C.; Weiner, T.M. Gastroschisis, atresia, dysmotility: Surgical treatment strategies for a distinct clinical entity. J. Pediatr. Surg. 2008, 43, 2208–2212. [Google Scholar] [CrossRef]
- Carnaghan, H.; James, C.P.; Charlesworth, P.B.; Ghionzoli, M.; Pereira, S.; Elkhouli, M.; Baud, D.; De Coppi, P.; Ryan, G.; Shah, P.S.; et al. Antenatal corticosteroids and outcomes in gastroschisis: A multicenter retrospective cohort study. Prenat. Diagn. 2020, 40, 991–997. [Google Scholar] [CrossRef]
- Johnson, D.G. Total intravenous nutrition in newborn surgical patients: A three-year perspective. J. Pediatr. Surg. 1970, 5, 601–605. [Google Scholar] [CrossRef]
- Barseghyan, K.; Aghajanian, P.; Miller, D.A. The prevalence of preterm births in pregnancies complicated with fetal gastroschisis. Arch. Gynecol. Obstet. 2012, 286, 889–892. [Google Scholar] [CrossRef]
- Soll, R. Synthetic surfactant for respiratory distress syndrome in preterm infants. Cochrane Database Syst. Rev. 1998, 1998, CD001149. [Google Scholar] [CrossRef]
- Sparks, T.N.; Shaffer, B.L.; Page, J.; Caughey, A.B. Gastroschisis: Mortality risks with each additional week of expectant management. Am. J. Obstet. Gynecol. 2017, 216, 66.e1–66.e7. [Google Scholar] [CrossRef]
- Cain, M.A.; Salemi, J.L.; Tanner, J.P.; Mogos, M.F.; Kirby, R.S.; Whiteman, V.E.; Salihu, H.M. Perinatal Outcomes and Hospital Costs in Gastroschisis Based on Gestational Age at Delivery. Obstet. Gynecol. 2014, 124, 543–550. [Google Scholar] [CrossRef] [PubMed]
- Baud, D.; Lausman, A.; Alfaraj, M.A.; Seaward, G.; Kingdom, J.; Windrim, R.; Langer, J.C.; Kelly, E.N.; Ryan, G. Expectant Management Compared With Elective Delivery at 37 Weeks for Gastroschisis. Obstet. Gynecol. 2013, 121, 990–998. [Google Scholar] [CrossRef]
- Grant, N.H.; Dorling, J.; Thornton, J.G. Elective preterm birth for fetal gastroschisis. Cochrane Database Syst. Rev. 2013, 6, CD009394. [Google Scholar] [CrossRef]
- Crawford, R.A.F.; Ryan, G.; Wright, V.M.; Rodeck, C.H. The importance of serial biophysical assessment of fetal wellbeing in gastroschisis. BJOG Int. J. Obstet. Gynaecol. 1992, 99, 899–902. [Google Scholar] [CrossRef] [PubMed]
- Raymond, S.L.; Hawkins, R.B.; Peter, S.D.S.; Downard, C.D.; Qureshi, F.G.; Renaud, E.; Danielson, P.D.; Islam, S. Predicting Morbidity and Mortality in Neonates Born With Gastroschisis. J. Surg. Res. 2020, 245, 217–224. [Google Scholar] [CrossRef]
- Raitio, A.; Lahtinen, A.; Syvänen, J.; Kemppainen, T.; Löyttyniemi, E.; Gissler, M.; Hyvärinen, A.; Helenius, I. Gastroschisis in Finland 1993 to 2014—Increasing Prevalence, High Rates of Abortion, and Survival: A Population-Based Study. Eur. J. Pediatr. Surg. 2020, 30, 536–540. [Google Scholar] [CrossRef] [PubMed]
- Bergholz, R.; Boettcher, M.; Reinshagen, K.; Wenke, K. Complex gastroschisis is a different entity to simple gastroschisis affecting morbidity and mortality—A systematic review and meta-analysis. J. Pediatr. Surg. 2014, 49, 1527–1532. [Google Scholar] [CrossRef]
- Arnold, M.A.; Chang, D.C.; Nabaweesi, R.; Colombani, P.M.; Bathurst, M.A.; Mon, K.S.; Hosmane, S.; Abdullah, F. Risk stratification of 4344 patients with gastroschisis into simple and complex categories. J. Pediatr. Surg. 2007, 42, 1520–1525. [Google Scholar] [CrossRef]
- Wales, P.W.; de Silva, N.; Kim, J.H.; Lecce, L.; Sandhu, A.; Moore, A.M. Neonatal short bowel syndrome: A cohort study. J. Pediatr. Surg. 2005, 40, 755–762. [Google Scholar] [CrossRef]
- Abubakar, K.M. Complications of Mechanical Ventilation. In Textbook of Clinical Pediatrics, 2nd ed.; Springer: Berlin/Heidelberg, Germany, 2012; pp. 251–256. [Google Scholar]
- Samuels, N.; van de Graaf, R.A.; de Jonge, R.C.J.; Reiss, I.K.M.; Vermeulen, M.J. Risk factors for necrotizing enterocolitis in neonates: A systematic review of prognostic studies. BMC Pediatr. 2017, 17, 105. [Google Scholar] [CrossRef]
- Ferreira, R.G.; Mendonça, C.R.; de Moraes, C.L.; Tacon, F.S.D.A.; Ramos, L.L.G.; e Melo, N.C.; Sbragia, L.; Amaral, W.N.D.; Ruano, R. Ultrasound Markers for Complex Gastroschisis: A Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 5215. [Google Scholar] [CrossRef]
- Durmaz, L.-O.; Brunner, S.E.; Meinzer, A.; Krebs, T.F.; Bergholz, R. Fetal surgery for gastroschisis—A review with emphasis on minimally invasive procedures. Children 2022, 9, 416. [Google Scholar] [CrossRef] [PubMed]
- Joyeux, L.; Belfort, M.A.; De Coppi, P.; Basurto, D.; Valenzuela, I.; King, A.; De Catte, L.; Shamshirsaz, A.A.; Deprest, J.; Keswani, S.G. Complex gastroschisis: A new indication for fetal surgery? Ultrasound Obstet. Gynecol. 2021, 58, 804–812. [Google Scholar] [CrossRef]
- Wright, N.J.; Sekabira, J.; Ade-Ajayi, N. Care of infants with gastroschisis in low-resource settings. Semin. Pediatr. Surg. 2018, 27, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Wright, N.J.; Leather, A.J.; Ade-Ajayi, N.; Sevdalis, N.; Davies, J.; Poenaru, D.; Ameh, E.; Ademuyiwa, A.; Lakhoo, K.; Smith, E.R.; et al. Mortality from gastrointestinal congenital anomalies at 264 hospitals in 74 low-income, middle-income, and high-income countries: A multicentre, international, prospective cohort study. Lancet 2021, 398, 325–339. [Google Scholar] [CrossRef]
- Wright, N.J.; Langer, M.; Norman, I.C.; Akhbari, M.; Wafford, Q.E.; Ade-Ajayi, N.; Davies, J.; Poenaru, D.; Sevdalis, N.; Leather, A. Improving outcomes for neonates with gastroschisis in low-income and middle-income countries: A systematic review protocol. BMJ Paediatr. Open 2018, 2, e000392. [Google Scholar] [CrossRef]
- Vidyasagar, D.; Velaphi, S.; Bhat, V.B. Surfactant Replacement Therapy in Developing Countries. Neonatology 2011, 99, 355–366. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Georgeades, C.; Mowrer, A.; Ortega, G.; Abdullah, F.; Salazar, J.H. Improved Mortality of Patients with Gastroschisis: A Historical Literature Review of Advances in Surgery and Critical Care from 1960–2020. Children 2022, 9, 1504. https://doi.org/10.3390/children9101504
Georgeades C, Mowrer A, Ortega G, Abdullah F, Salazar JH. Improved Mortality of Patients with Gastroschisis: A Historical Literature Review of Advances in Surgery and Critical Care from 1960–2020. Children. 2022; 9(10):1504. https://doi.org/10.3390/children9101504
Chicago/Turabian StyleGeorgeades, Christina, Alyssa Mowrer, Gezzer Ortega, Fizan Abdullah, and Jose H. Salazar. 2022. "Improved Mortality of Patients with Gastroschisis: A Historical Literature Review of Advances in Surgery and Critical Care from 1960–2020" Children 9, no. 10: 1504. https://doi.org/10.3390/children9101504
APA StyleGeorgeades, C., Mowrer, A., Ortega, G., Abdullah, F., & Salazar, J. H. (2022). Improved Mortality of Patients with Gastroschisis: A Historical Literature Review of Advances in Surgery and Critical Care from 1960–2020. Children, 9(10), 1504. https://doi.org/10.3390/children9101504




