Intrinsic Kidney Pathology in Children and Adolescents Following COVID-19 Vaccination: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
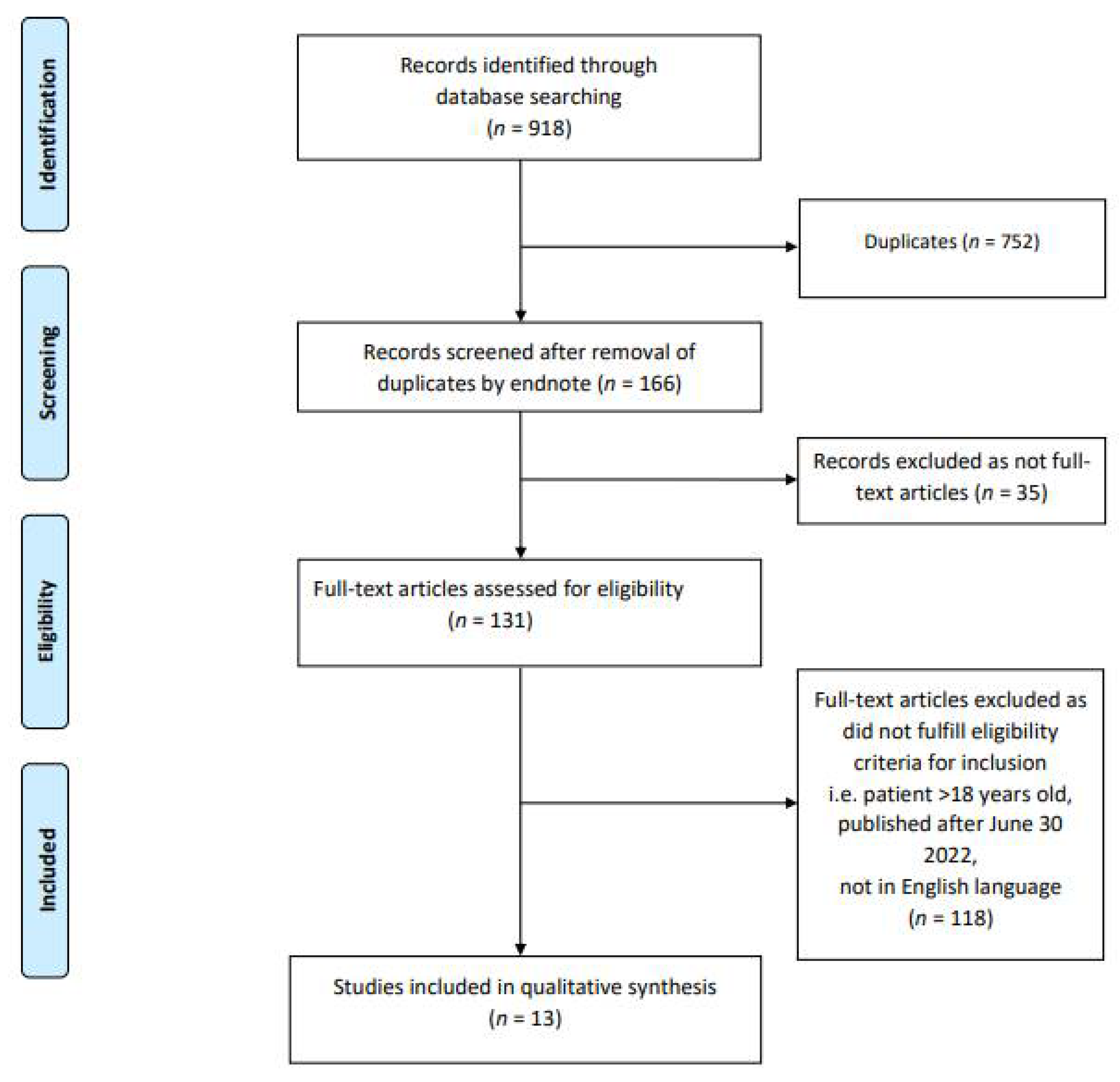
2.2. Search Strategy and Study Selection
2.3. Data Extraction
2.4. Study Registration
3. Results
3.1. IgA Nephropathy
3.2. Nephrotic Syndrome and Tubulointerstitial Nephritis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 18 September 2022).
- Chakraborty, I.; Maity, P. COVID-19 outbreak: Migration, effects on society, global environment and prevention. Sci. Total Environ. 2020, 728, 138882. [Google Scholar] [CrossRef] [PubMed]
- Ewer, K.J.; Barrett, J.R.; Belij-Rammerstorfer, S.; Sharpe, H.; Makinson, R.; Morter, R.; Flaxman, A.; Wright, D.; Bellamy, D.; Bittaye, M.; et al. T cell and antibody responses induced by a single dose of ChAdOx1 nCoV-19 (AZD1222) vaccine in a phase 1/2 clinical trial. Nat. Med. 2021, 27, 270–278. [Google Scholar] [CrossRef] [PubMed]
- Ali, K.; Berman, G.; Zhou, H.; Deng, W.; Faughnan, V.; Coronado-Voges, M.; Ding, B.; Dooley, J.; Girard, B.; Hillebrand, W.; et al. Evaluation of mRNA-1273 SARS-CoV-2 vaccine in adolescents. N. Engl. J. Med. 2021, 385, 2241–2251. [Google Scholar] [CrossRef]
- Walter, E.B.; Talaat, K.R.; Sabharwal, C.; Gurtman, A.; Lockhart, S.; Paulsen, G.C.; Barnett, E.D.; Muñoz, F.M.; Maldonado, Y.; Pahud, B.A.; et al. Evaluation of the BNT162b2 COVID-19 vaccine in children 5 to 11 years of age. N. Engl. J. Med. 2022, 386, 35–46. [Google Scholar] [CrossRef] [PubMed]
- Creech, C.B.; Anderson, E.; Berthaud, V.; Yildirim, I.; Atz, A.M.; Melendez Baez, I.; Finkelstein, D.; Pickrell, P.; Kirstein, J.; Yut, C.; et al. Evaluation of mRNA-1273 COVID-19 vaccine in children 6 to 11 years of age. N. Engl. J. Med. 2022, 386, 2011–2023. [Google Scholar] [CrossRef]
- FDA. FDA Briefing Document: EUA Amendment Request for Use of the Moderna COVID-19 Vaccine in Children 6 Months through 17 Years of Age. Available online: https://www.fda.gov/media/159189/download (accessed on 18 July 2022).
- Sahin, U.; Muik, A.; Derhovanessian, E.; Vogler, I.; Kranz, L.M.; Vormehr, M.; Baum, A.; Pascal, K.; Quandt, J.; Maurus, D.; et al. COVID-19 vaccine BNT162b1 elicits human antibody and TH1 T cell responses. Nature 2020, 586, 594–599. [Google Scholar] [CrossRef]
- Pegu, A.; O’Connell, S.E.; Schmidt, S.D.; O’Dell, S.; Talana, C.A.; Lai, L.; Albert, J.; Anderson, E.; Bennett, H.; Corbett, K.S.; et al. Durability of mRNA-1273 vaccine–induced antibodies against SARS-CoV-2 variants. Science 2021, 373, 1372–1377. [Google Scholar] [CrossRef]
- Kronbichler, A.; Anders, H.J.; Fernandez-Juárez, G.M.; Floege, J.; Goumenos, D.; Segelmark, M. Immunonephrology Working Group of the ERA-EDTA (European Renal Association—European Dialysis and Transplant Association). Recommendations for the use of COVID-19 vaccines in patients with immune-mediated kidney diseases. Nephrol. Dial. Transplant. 2021, 36, 1160–1168. [Google Scholar] [CrossRef]
- Stevens, K.I.; Frangou, E.; Shin, J.I.; Anders, H.J.; Bruchfeld, A.; Schönermarck, U.; Hauser, T.; Westman, K.; Fernandez-Juarez, G.M.; Floege, J.; et al. Perspective on COVID-19 vaccination in patients with immune-mediated kidney diseases: Consensus statements from ERA-IWG and EUVAS. Nephrol. Dial. Transplant. 2022, 37, 1400–1410. [Google Scholar] [CrossRef]
- Wu, H.H.L.; Kalra, P.A.; Chinnadurai, R. New-Onset and Relapsed Kidney Histopathology Following COVID-19 Vaccination: A Systematic Review. Vaccines 2021, 9, 1252. [Google Scholar] [CrossRef]
- Fenoglio, R.; Lalloni, S.; Marchisio, M.; Oddone, V.; De Simone, E.; Del Vecchio, G.; Sciascia, S.; Roccatello, D. New Onset Biopsy-Proven Nephropathies after COVID Vaccination. Am. J. Nephrol. 2022, 53, 325–330. [Google Scholar] [CrossRef] [PubMed]
- Bomback, A.S.; Kudose, S.; D’Agati, V.D. De novo and relapsing glomerular diseases after COVID-19 vaccination: What do we know so far? Am. J. Kidney Dis. 2021, 78, 477–480. [Google Scholar] [CrossRef] [PubMed]
- Li, N.L.; Coates, P.T.; Rovin, B.H. COVID-19 vaccination followed by activation of glomerular diseases: Does association equal causation? Kidney Int. 2021, 100, 959–965. [Google Scholar] [CrossRef] [PubMed]
- Alshami, A.; on behalf of the Pediatric Nephrology Clinical Pathway Development Team; Roshan, A.; Catapang, M.; Jöbsis, J.J.; Kwok, T.; Polderman, N.; Sibley, J.; Sibley, M.; Mammen, C.; et al. Indications for kidney biopsy in idiopathic childhood nephrotic syndrome. Pediatr. Nephrol. 2017, 32, 1897–1905. [Google Scholar] [CrossRef] [PubMed]
- Hanna, C.; Hernandez, L.P.; Bu, L.; Kizilbash, S.; Najera, L.; Rheault, M.N.; Czyzyk, J.; Kouri, A.M. IgA nephropathy presenting as macroscopic hematuria in 2 pediatric patients after receiving the Pfizer COVID-19 vaccine. Kidney Int. 2021, 100, 705–706. [Google Scholar] [CrossRef] [PubMed]
- Horino, T.; Sawamura, D.; Inotani, S.; Ishihara, M.; Komori, M.; Ichii, O. Newly diagnosed IgA nephropathy with gross haematuria following COVID-19 vaccination. QJM Int. J. Med. 2022, 115, 28–29. [Google Scholar] [CrossRef]
- Okada, M.; Kikuchi, E.; Nagasawa, M.; Oshiba, A.; Shimoda, M. An adolescent girl diagnosed with IgA nephropathy following the first dose of the COVID-19 vaccine. CEN Case Rep. 2022, 11, 376–379. [Google Scholar] [CrossRef]
- Niel, O.; Florescu, C. IgA nephropathy presenting as rapidly progressive glomerulonephritis following first dose of COVID-19 vaccine. Pediatr. Nephrol. 2022, 37, 461–462. [Google Scholar] [CrossRef]
- Morisawa, K.; Honda, M. Two patients presenting IgA nephropathy after COVID-19 vaccination during a follow-up for asymptomatic hematuria. Pediatr. Nephrol. 2022, 37, 1695–1696. [Google Scholar] [CrossRef]
- Udagawa, T.; Motoyoshi, Y. Macroscopic hematuria in two children with IgA nephropathy remission following Pfizer COVID-19 vaccination. Pediatr. Nephrol. 2022, 37, 1693–1694. [Google Scholar] [CrossRef]
- Abdel-Qader, D.H.; Alkhatatbeh, I.H.; Hayajneh, W.; Annab, H.; Al Meslamani, A.Z.; Elmusa, R.A. IgA nephropathy in a pediatric patient after receiving the first dose of Pfizer-BioNTech COVID-19 vaccine. Vaccine 2022, 40, 2528–2530. [Google Scholar] [CrossRef] [PubMed]
- Nakazawa, E.; Uchimura, T.; Hirai, Y.; Togashi, H.; Oyama, Y.; Inaba, A.; Shiga, K.; Ito, S. New-onset pediatric nephrotic syndrome following Pfizer-BioNTech SARS-CoV-2 vaccination: A case report and literature review. CEN Case Rep. 2022, 11, 242–246. [Google Scholar] [CrossRef] [PubMed]
- Pella, E.; Sarafidis, P.A.; Alexandrou, M.E.; Stangou, M.; Nikolaidou, C.; Kosmidis, D.; Papagianni, A. De novo Minimal Change Disease in an Adolescent after Pfizer-BioNTech COVID-19 Vaccination: A Case Report. Case Rep. Nephrol. Dial. 2022, 12, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Alhosaini, M.N. A Case of Minimal Change Disease after SARS-CoV-2 Vaccination under the Age of 18. Avicenna J. Clin. Med. 2022, 12, 31–33. [Google Scholar] [CrossRef]
- Jongvilaikasem, P.; Rianthavorn, P. Minimal change disease and acute interstitial nephritis following SARS-CoV-2 BNT162b2 vaccination. Pediatr. Nephrol. 2022, 37, 1419–1421. [Google Scholar] [CrossRef]
- Güngör, T.; Yazılıtaş, F.; Kargın Çakıcı, E.; Karakaya, D.; Bülbül, M. Relapse of Idiopathic Nephrotic Syndrome After SARS-CoV-2 Vaccination: Two Case Reports. J. Paediatr. Child Health 2022, 58, 939–940. [Google Scholar] [CrossRef]
- Choi, J.H.; Kang, K.S.; Han, K.H. Two adolescent cases of acute tubulointerstitial nephritis after second dose of COVID-19 mRNA vaccine. Hum. Vaccin. Immunother. 2022, 18, 2059308. [Google Scholar] [CrossRef]
- Coppo, R. Pediatric IgA Nephropathy in Europe. Kidney Dis. 2019, 5, 182–188. [Google Scholar] [CrossRef]
- Hogg, R.J. Idiopathic immunoglobulin A nephropathy in children and adolescents. Pediatr. Nephrol. 2010, 25, 823–829. [Google Scholar] [CrossRef][Green Version]
- Gutiérrez, E.; Carvaca-Fontán, F.; Luzardo, L.; Morales, E.; Alonso, M.; Praga, M. A personalized update on IgA nephropathy: A new vision and new future challenges. Nephron 2020, 144, 555–571. [Google Scholar] [CrossRef]
- Knoppova, B.; Reily, C.; Maillard, N.; Rizk, D.V.; Moldoveanu, Z.; Mestecky, J.; Raska, M.; Renfrow, M.B.; Julian, B.A.; Novak, J. The origin and activities of IgA1-containing immune complexes in IgA nephropathy. Front. Immunol. 2016, 7, 117. [Google Scholar] [CrossRef] [PubMed]
- Yeo, S.C.; Cheung, C.K.; Barratt, J. New insights into the pathogenesis of IgA nephropathy. Pediatr. Nephrol. 2018, 33, 763–777. [Google Scholar] [CrossRef] [PubMed]
- Lai, K.N. Pathogenesis of IgA nephropathy. Nat. Rev. Nephrol 2012, 8, 275–283. [Google Scholar] [CrossRef] [PubMed]
- Patel, C.; Shah, H.H. Vaccine-associated kidney diseases: A narrative review of the literature. Saudi J. Kidney Dis. Transpl. 2019, 30, 1002–1009. [Google Scholar] [CrossRef] [PubMed]
- Van den Wall Bake, A.W.; Beyer, W.E.; Evers-Schouten, J.H.; Hermans, J.; Daha, M.R.; Masurel, N.; Van Es, L.A. Humoral immune response to influenza vaccination in patients with primary immunoglobulin A nephropathy. An analysis of isotype distribution and size of the influenza-specific antibodies. J. Clin. Investig. 1989, 84, 1070–1075. [Google Scholar] [CrossRef] [PubMed]
- Abramson, M.; Yu, S.M.; Campbell, K.N.; Chung, M.; Salem, F. IgA nephropathy after SARS-CoV-2 vaccination. Kidney Med. 2021, 3, 860–863. [Google Scholar] [CrossRef]
- Zhao, X.; Chen, H.; Wang, H. Glycans of SARS-CoV-2 spike protein in virus infection and antibody production. Front. Mol. Biosci. 2021, 8, 53. [Google Scholar] [CrossRef]
- Wisnewski, A.V.; Luna, J.C.; Redlich, C.A. Human IgG and IgA responses to COVID-19 mRNA vaccines. PLoS ONE 2021, 16, e0249499. [Google Scholar] [CrossRef]
- The Japanese Society for Pediatric Nephrology. The 2020 Japanese Society for Pediatric Nephrology guidelines for pediatric IgA nephropathy. Shindan to Chiryo-sya; The Japanese Society for Pediatric Nephrology: Tokyo, Japan, 2020. [Google Scholar]
- Noone, D.G.; Iijima, K.; Parekh, R. Idiopathic nephrotic syndrome in children. Lancet 2018, 392, 61–74. [Google Scholar] [CrossRef]
- Meyrier, A.; Niaudet, P. Acute kidney injury complicating nephrotic syndrome of minimal change disease. Kidney Int. 2018, 94, 861–869. [Google Scholar] [CrossRef]
- Vivarelli, M.; Massella, L.; Ruggiero, B.; Emma, F. Minimal change disease. Clin. J. Am. Soc. Nephrol. 2017, 12, 332–345. [Google Scholar] [CrossRef] [PubMed]
- Bertelli, R.; Bonanni, A.; Caridi, G.; Canepa, A.; Ghiggeri, G.M. Molecular and cellular mechanisms for proteinuria in minimal change disease. Front. Med. 2018, 5, 170. [Google Scholar] [CrossRef] [PubMed]
- Kimmel, P.L.; Ferreira-Centeno, A.; Farkas-Szallasi, T.; Abraham, A.A.; Garrett, C.T. Viral DNA in microdissected renal biopsy tissue from HIV infected patients with nephrotic syndrome. Kidney Int. 1993, 43, 1347–1352. [Google Scholar] [CrossRef]
- Gupta, A.; Quigg, R.J. Glomerular diseases associated with hepatitis B and C. Adv. Chronic. Kidney Dis. 2015, 22, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Rowley, A.H. Understanding SARS-CoV-2-related multisystem inflammatory syndrome in children. Nat. Rev. Immunol. 2020, 20, 453–454. [Google Scholar] [CrossRef] [PubMed]
- Kari, J. Steroid-sensitive nephrotic syndrome and juvenile idiopathic arthritis. Pediatr. Nephrol. 2002, 11, 975–976. [Google Scholar] [CrossRef]
- Bilginer, Y.; Akpolat, T.; Ozen, S. Renal amyloidosis in children. Pediatr. Nephrol. 2011, 26, 1215–1227. [Google Scholar] [CrossRef]
- Tan, J.; Tang, Y.; Xu, Y.; Yan, S.; Xu, Y.; Tan, L.; Zhong, Z.; Tarun, P.; Qin, W. The clinicopathological characteristics of Henoch-Schönlein purpura nephritis with presentation of nephrotic syndrome. Kidney Blood Press Res. 2019, 44, 754–764. [Google Scholar] [CrossRef]
- Gutiérrez, S.; Dotto, B.; Petiti, J.P.; Paul, A.L.; Dionisio de Cabalier, M.E.; Torres, A.I.; Mukdsi, J.H. Minimal change disease following influenza vaccination and acute renal failure: Just a coincidence? Nefrología 2012, 32, 414–415. [Google Scholar]
- Weijers, J.; Alvarez, C.; Hermans, M.M. Post-vaccinal minimal change disease. Kidney Int. 2021, 100, 459–461. [Google Scholar] [CrossRef]
- Kikuchi, Y.; Imakiire, T.; Hyodo, T.; Higashi, K.; Henmi, N.; Suzuki, S.; Miura, S. Minimal change nephrotic syndrome, lymphadenopathy and hyperimmunoglobulinemia after immunization with a pneumococcal vaccine. Clin. Nephrol. 2002, 58, 68–72. [Google Scholar] [CrossRef] [PubMed]
- Clajus, C.; Spiegel, J.; Bröcker, V.; Chatzikyrkou, C.; Kielstein, J.T. Minimal change nephrotic syndrome in an 82 year old patient following a tetanus-diphteria-poliomyelitis-vaccination. BMC Nephrol. 2009, 10, 21. [Google Scholar] [CrossRef] [PubMed]
- Horinouchi, T.; Nozu, K.; Iijima, K. An updated view of the pathogenesis of steroid-sensitive nephrotic syndrome. Pediatr. Nephrol. 2022, 37, 1957–1965. [Google Scholar] [CrossRef]
- Kaklamanos, A.; Belogiannis, K.; Skendros, P.; Gorgoulis, V.G.; Vlachoyiannopoulos, P.G.; Tzioufas, A.G. COVID-19 Immunobiology: Lessons Learned, New Questions Arise. Front. Immunol. 2021, 12, 719023. [Google Scholar] [CrossRef]
- León-Román, J.; Agraz, I.; Vergara, A.; Ramos, N.; Toapanta, N.; García-Carro, C.; Gabaldón, A.; Bury, R.; Bermejo, S.; Bestard, O. COVID-19 infection and renal injury: Where is the place for acute interstitial nephritis disease? Clin. Kidney J. 2022, 15, 1698–1704. [Google Scholar] [CrossRef]
- Wu, H.H.L.; Li, J.W.C.; Bow, A.; Woywodt, A.; Ponnusamy, A. Acute interstitial nephritis following SARS-CoV-2 vaccination. Clin. Kidney J. 2022, 15, 576–581. [Google Scholar] [CrossRef]
- Storrar, J.; Kudose, S.; Woywodt, A. Have we missed AINything? Acute interstitial nephritis in SARS-CoV-2 infection and vaccination. Clin. Kidney J. 2022, 15, 1643–1652. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Jung, J.; Cho, H.; Lee, J.; Go, H.; Lee, J.H. A child with crescentic glomerulonephritis following SARS-CoV-2 mRNA (Pfizer-BioNTech) vaccination. Pediatr. Nephrol. 2022, 1–4. [Google Scholar] [CrossRef]
- Sakai, T.; Kitagawa, T. Screening system for asymptomatic renal disease in children in Japan. Pediatr. Int. 1990, 32, 677–681. [Google Scholar] [CrossRef]
- Imai, E.; Yamagata, K.; Iseki, K.; Iso, H.; Horio, M.; Mkino, H.; Hishida, A.; Matsuo, S.; Fine, D.M.; Garg, N. Kidney disease screening program in Japan: History, outcome, and perspectives. Clin. J. Am. Soc. Nephrol. 2007, 2, 1360–1366. [Google Scholar] [CrossRef]
- Hicks, D.A. The inequality-adjusted human development index: A constructive proposal. World Dev. 1997, 25, 1283–1298. [Google Scholar] [CrossRef]
- American Academy of Pediatrics. Children and COVID-19 Vaccinations Trends AAP Analysis of Data Posted by the Centers for Disease Control and Prevention as of 29 June 2022. Available online: https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/children-and-covid-19-vaccination-trends/ (accessed on 18 September 2022).
- Australian Government Department of Health and Aged Care. COVID-19 Vaccination Numbers and Statistics. Available online: https://www.health.gov.au/initiatives-and-programs/covid-19-vaccines/numbers-statistics (accessed on 18 September 2022).
- Ionescu, M.D.; Balgradean, M.; Cirstoveanu, C.G.; Balgradean, I.; Popa, L.I.; Pavelescu, C.; Capitanescu, A.; Berghea, E.; Filip, C. Myopericarditis Associated with COVID-19 in a Pediatric Patient with Kidney Failure Receiving Hemodialysis. Pathogens 2021, 10, 486. [Google Scholar] [CrossRef] [PubMed]
| Author(s) & Country of Report | Age (yrs) | Sex | Time to Presentation from Day of Vaccination (Days) | Comorbidities | New- onset or Relapse | Vaccine Brand & Vaccine Dose | Serum Creatinine Since Day of Presentation (mg/dL) | Serum Albumin Since Day of Presentation (g/dL) | Urine Protein-to-Creatinine Ratio Since Day of Presentation (g/g) | Haematuria Since Day of Presentation | Kidney Biopsy | Treatment Received | Clinical Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hanna et al. [17], United States | 13 | M | Within 1 day | TIDM, previous diagnosis of IgA nephropathy | Relapse | Pfizer, 2nd dose | Pre-vaccination: 0.54 Day 2: 1.31 Day 6: 0.66 | Pre-vaccination: 3.4 Day 2: 3.8 Day 6: 3.0 | Pre-vaccination: 1.6 Day 2: 1.07 Day 6: 0.86 | Day 1: Gross haematuria, resolved after 2 days | Not performed | Supportive treatment. Lisinopril 10 mg/day commenced for 5 days. | IgA nephropathy self-resolved within 1 week without other interventions |
| Hanna et al. [17], United States | 17 | M | Within 1 day | Nil | New-onset | Pfizer, 2nd dose | Day 6: 1.78 Day 9: 1.47 Day 22: 1.20 | Day 9: 3.8 | Day 9: 1.75 | Day 1: Gross haematuria, resolved after 4 days | Cellular glomerular crescents and moderate to severe tubulointerstitial scarring suggestive of pre-existing IgA nephropathy | IV pulsed methylprednisolone 1 g daily and oral prednisolone | Improved serum creatinine on follow-up following steroid treatment |
| Horino et al. [18], Japan | 17 | M | 2 days | Nil. But urine dipstick 5 months ago revealed microscopic haematuria | New-onset | Pfizer, 2nd dose | Day 1: 0.70 | Not specified | Day 1: 1.00 Day 7: 1.40 | Day 1: Gross haematuria, >100 RBC/HPF Day 7: Gross haematuria, >100 RBC/HPF | Light microscopy revealed mesangial cell and matrix proliferation, endocapillary hypercellularity and crescents. Immunofluorescence staining revealed predominantly IgA and C3 deposits with weak IgG deposits in the mesangial areas. | Initially treatment was supportive, but with persistence of proteinuria and microhaematuria after 2 months, tonsillectomy and pulsed steroid therapy was commenced | Persistence of proteinuria and microhaematuria after 2 months of supportive treatment. Patient referred for tonsillectomy and commenced on pulsed steroid therapy |
| Okada et al. [19], Japan | 17 | F | 4 days | No cause found for microscopic haematuria when 7 yrs old, followed up in clinic | New-onset | Pfizer, 1st dose | Day 1: 0.58 | Not specified | Day 1: 0.37 Day 10: 0.05 Day 16: 0.07 | 4 months pre-vaccination: 20–29 RBC/HPF 4 days after 1st dose: Gross haematuria | Light microscopy revealed mild mesangial proliferation, no endo-capillary or extra-capillary proliferation, sclerosis, or adhesion was observed. Immunofluorescence analysis revealed diffuse mesangial IgA and C3 deposits. Electron microscopy revealed electron-dense deposits in the mesangial lesions. | Supportive treatment. Patient proceeded to receive 2nd dose of Pfizer vaccine shortly after episode following 1st dose | Spontaneous resolving of proteinuria and gross haematuria, patient followed up until 16 days after 2nd dose of vaccine. |
| Niel et al. [20], Luxembourg | 13 | F | Within 1 day | Nil | New-onset | Pfizer, 1st dose | Day 1: 3.57 Day 11: 1.90 Day 30: 0.86 | Not specified | Day 1: 3.88 | Day 1: Macroscopic haematuria Day 30: Microscopic haematuria persisted | Mesangial and endocapillary proliferation. No constituted crescents were observed, but fibrin deposits were present in the Bowman space of most of the observed glomeruli. No evidence of renal scarring from previous kidney injury could be detected. Diffuse mesangial IgA and C3 deposits on immunofluorescence. Diffuse mesangial deposits on electron microscopy. | Patient commenced on haemodialysis in hospital as kidney function rapidly deteriorated and patient became oliguric. Patient also commenced on three IV methylprednisolone doses followed by oral prednisolone. | Improvements in kidney function following commencement of haemodialysis and steroid course. By 30 days post-vaccination, serum creatinine returned to normal range. Microscopic haematuria and slight proteinuria persisted |
| Morisawa et al. [21], Japan | 16 | M | Within the same day | Followed up in clinic for asymptomatic haematuria. | New-onset | Brand not noted, 2nd dose | Day 6: 1.1 Day 20: 1.26 Day 55: 1.29 Day 90: 1.05 | Not specified | Day 6: 0.28 | Day 1: Gross haematuria Day 3: Gross haematuria resolved | Mild proliferation of mesangial cells and cellular crescents was diagnosed in light microscopy. | Gross haematuria resolved 3 days post-vaccination. However, a rise in serum creatinine and proteinuria is observed afterwards. Patient was commenced on IV pulsed methylprednisolone for 3 consecutive days over two consecutive weeks. Oral prednisolone also prescribed and its dose increased with initial inability to improve serum creatinine. | At follow-up 3 months post-vaccination, significant improvement in serum creatinine has been observed. |
| Morisawa et al. [21], Japan | 13 | F | Within 1 day | Followed up in clinic for asymptomatic haematuria. | New-onset | Brand not noted, 2nd dose | Not specified | Not specified | Day 7: 1.99 | 2 months pre-vaccination: 10–20 RBC/HPF Day 1: Gross haematuria Gross haematuria gradually resolved | Light microscopy found histological picture of IgA nephropathy with mild proliferation of mesangial cells | Supportive treatment | Proteinuria resolved on day 26 post-vaccination spontaneously |
| Udagawa et al. [22], Japan | 15 | F | 1 day | IgA nephropathy. Patient was in remission with multiple-drug therapy that utilized prednisolone, lisinopril, warfarin, and dipyridamole | Relapse | Pfizer, 2nd dose | Not specified | Not specified. | Not specified. Mild proteinuria described, resolved after 3 days | Day 1: Macroscopic haematuria, resolved after 3 days | Not performed | Not specified | Not specified |
| Udagawa et al. [22], Japan | 16 | F | 1.5 days | IgA nephropathy. Following multiple immunosuppressive treatments, including prednisolone, mizoribin, warfarin, and dipyridamole, patient was in remission. | Relapse | Pfizer, 2nd dose | Not specified | Not specified | 15 months pre-vaccination: 0.5–1.0 No excess proteinuria described during acute episode | 15 months pre-vaccination: Intermittent macroscopic haematuria Day 3: Macroscopic haematuria, resolved by Day 6 | Not performed | Supportive treatment | Spontaneously resolved by 5 days following presentation. Serum creatinine did not increase and urinalysis has normalized |
| Abdel-Qader et al. [23] Jordan | 12 | M | Within 1 day | Nil | New-onset | Pfizer, 1st dose | Day 2: 1.77 Day 3: 1.74 Day 4: 1.59 Day 5: 1.39 Day 7: 1.39 4 days post-discharge: 0.87 | Day 2: 4.1 | Day 2: 1.7 Day 7: Trace protein 4 days post-discharge: Trace protein | Day 2: 1920 RBC/µL Day 7: 254 RBC/µL 4 days post-discharge: 992 RBC/µL | Mild increase of mesangial cells and matrix; no thickening of capillary loops, segmental sclerosis, crescent formation or necrosis were seen. Mild interstitial oedema was noted. Many of the tubules showed red cell casts with mild tubular injury and flattening of epithelial cells. Immunofluorescence showed granular mesangial deposits of IgA and C3. | IV pulsed methylprednisolone therapy was commenced. | Follow-up showed improved serum creatinine levels. Patient discharged on oral enalapril 5 mg, prednisolone 5 mg and esomeprazole 20 mg once daily |
| Author(s) & Country of Report | Age (yrs) | Sex | Time to Presentation from Day of Vaccination (Days) | Comorbidities | New- Onset or Relapse | Vaccine Brand & Vaccine Dose | Serum Creatinine Since Day of Presentation (mg/dL) | Serum Albumin Since Day of Presentation (g/dL) | Urine Protein-to-Creatinine Ratio Since Day of Presentation (g/g) | Haematuria Since Day of Presentation | Kidney Biopsy | Treatment Received | Clinical Outcome |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Nakazawa et al. [24], Japan | 15 | M | 1 day | Nil | New-onset | Pfizer, 1st dose | Day 1: 0.64 | Day 1: 1.6 | Day 1: 7.71 | Day 1: Urine sediment showed <1 RBC/HPF | Not performed | Initiated on oral prednisolone 60 mg daily from 21 days post-vaccination | Achieved complete remission on day 12 of treatment. Did not develop complications such as hypertension, AKI or thrombus formation |
| Pella et al. [25], Greece | 18 | M | 11 days | Nil | New-onset | Pfizer, 1st dose | 19 days pre-vaccination: 0.98 Day 5: 0.79 | Day 5: 1.8 Day 12: 1.8 Day 32: 3.2 Day 53: 4.0 Day 85: 4.3 | Day 5: 2.0 Day 12: 10.5 Day 13: 23.4 Day 32: 1.2 Day 53: 0.5 Day 85: 0.2 | Day 12: Urine sediment showed 2–3 RBC/HPF | Light microscopy showed no significant glomerular or tubular abnormalities. Immunofluorescence revealed no positive staining. | Commenced on 150 mg of Irbesartan and 48 mg of methylprednisolone on day 19 since presentation (day 6 of hospitalization). | Discharged on day 25 since presentation (day 12 of hospitalization). Irbesartan was stopped at follow-up review one week after discharge. Patient achieved complete remission of nephrotic syndrome at day 85 since presentation (7 weeks post-discharge). |
| Alhosaini et al. [26], UAE | 16 | M | 7 days | Not specified | New-onset | Pfizer, 2nd dose | Day 1: 0.85 Day 5: 0.85 Day 22: 0.76 | Day 1: 1.7 Day 5: 2.7 Day 22: 3.7 | Day 1: 10.3 Day 5: 2.92 Day 22: 0.06 | Day 1: ‘Moderate’ blood identified on urinalysis | Light microscopy showed normal glomeruli. Immunofluorescence studies were all negative. Electron microscopy showed diffuse foot process effacements. None of the glomeruli had any segmental sclerosis | The patient was commenced on oral prednisone 60 mg daily along with furosemide and olmesartan. | Clinical signs of nephrotic syndrome settled after 1 week since presentation, and proteinuria alongside serum albumin began to show improvement |
| Jongvilaikasem et al. [27], Thailand | 14 | M | 5 days | Nil | New-onset | Pfizer, 1st dose | Day 1: 2.0 Day 5: 9.0 Day 40: 0.53 | Day 1: 2.0 | Day 1: 9.0 Day 40: 0.9 | Nil throughout course of presentation | Light microscopy revealed unremarkable glomeruli. There was negative immunofluorescence staining. Electron microscopy showed diffuse foot process effacement. Diffuse tubular injury and interstitial inflammatory cell infiltration were noted. | Patient received acute haemodialysis for 3 weeks as became anuric with peak serum creatinine of 9.0 mg/dL on day 5 since presentation (10 days post-vaccination). Three daily doses of IV pulsed methylprednisolone were administered, followed by oral prednisolone 60 mg daily. | The patient achieved partial remission on day 40 since presentation, after a 5-week treatment of corticosteroids |
| Güngör et al. [28], Turkey | 17 | F | 19 days | Minimal change disease diagnosed at 1.5 years old, was treated with corticosteroids, levamisole, mycophenolate mofetil and enalapril. The patient discontinued treatment 3.5 years ago and was in remission for 4.5 years | Relapse | Moderna, 2nd dose | Day 1: 0.5 | Day 1: 1.2 | Day 1: 8.7 | Not specified | Not specified | Not specified | Not specified |
| Güngör et al. [28], Turkey | 17.5 | F | 12 days | Diagnosed with idiopathic nephrotic syndrome at 2.5 years old. Patient received corticosteroid treatment for 6 months and had not relapsed on follow-up | Relapse | Brand not noted, 2nd dose | Day 1: 0.48 | Day 1: 2.3 | Day 1: 4.1 | Not specified | Not performed | Patient commenced on oral corticosteroids. At time of case report, the patient is at a steroid reduction phase in which steroid treatment is intended to discontinue at the end of 6 months | Patient achieved remission 2 weeks following commencement of oral corticosteroids |
| Choi et al. [29], Korea | 17 | M | 6 days | Nil | New-onset | Pfizer, 2nd dose | Day 3: 3.0 Day 5: 3.10 Please refer to Figure 3 of this referenced article by Choi et al. for the trend of serum creatinine changes throughout the course of presentation. Exact values not specified in the text by the authors. | Day 5: 0.1 | Day 5: 4.3 | Nil throughout course of presentation | Light microscopy showed glomerulus appearing slightly larger and segmentally hypercellular, involving mesangial cells. Interstitial infiltrates were mainly mononuclear. Focal and moderate interstitial fibrosis and tubular atrophy were noted in approximately 20% of the renal cortices. GBM showed focal wrinkling with partly irregular inner contours. There was negative immunofluorescence staining. Electron microscopy revealed non-significant focal epithelial foot process effacement with no electron-dense deposits. | Supportive treatment | Kidney function gradually improved, with the patient having increased oral intake. He was discharged after 1 week of hospitalization. |
| Choi et al. [29], Korea | 12 | M | 18 days | Nil | New-onset | Pfizer, 2nd dose | Day 1: 2.28 Day 6: 2.25 Please refer to Figure 3 of this referenced article by Choi et al. for the trend of serum creatinine changes throughout the course of presentation. Exact values not specified in the text by the authors. | Day 6: 0.86 | Day 6: 4.4 | Day 1: 1+ blood on urinalysis | Tubules revealed severe necrosis, tubulorrhexis, and loss, with heavy infiltration of neutrophils, eosinophils, and mononuclear cells in the interstitium. GBM thickness was normal with smooth contours. There was negative immunofluorescence staining. No electron dense deposits observed | Commenced on oral steroids on day 10 of hospitalization | The patient had marked improvement in kidney function following commencement of oral steroids. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, H.H.L.; Shenoy, M.; Kalra, P.A.; Chinnadurai, R. Intrinsic Kidney Pathology in Children and Adolescents Following COVID-19 Vaccination: A Systematic Review. Children 2022, 9, 1467. https://doi.org/10.3390/children9101467
Wu HHL, Shenoy M, Kalra PA, Chinnadurai R. Intrinsic Kidney Pathology in Children and Adolescents Following COVID-19 Vaccination: A Systematic Review. Children. 2022; 9(10):1467. https://doi.org/10.3390/children9101467
Chicago/Turabian StyleWu, Henry H. L., Mohan Shenoy, Philip A. Kalra, and Rajkumar Chinnadurai. 2022. "Intrinsic Kidney Pathology in Children and Adolescents Following COVID-19 Vaccination: A Systematic Review" Children 9, no. 10: 1467. https://doi.org/10.3390/children9101467
APA StyleWu, H. H. L., Shenoy, M., Kalra, P. A., & Chinnadurai, R. (2022). Intrinsic Kidney Pathology in Children and Adolescents Following COVID-19 Vaccination: A Systematic Review. Children, 9(10), 1467. https://doi.org/10.3390/children9101467







