Infants of Mothers with Cocaine Use: Review of Clinical and Medico-Legal Aspects
Abstract
1. Introduction
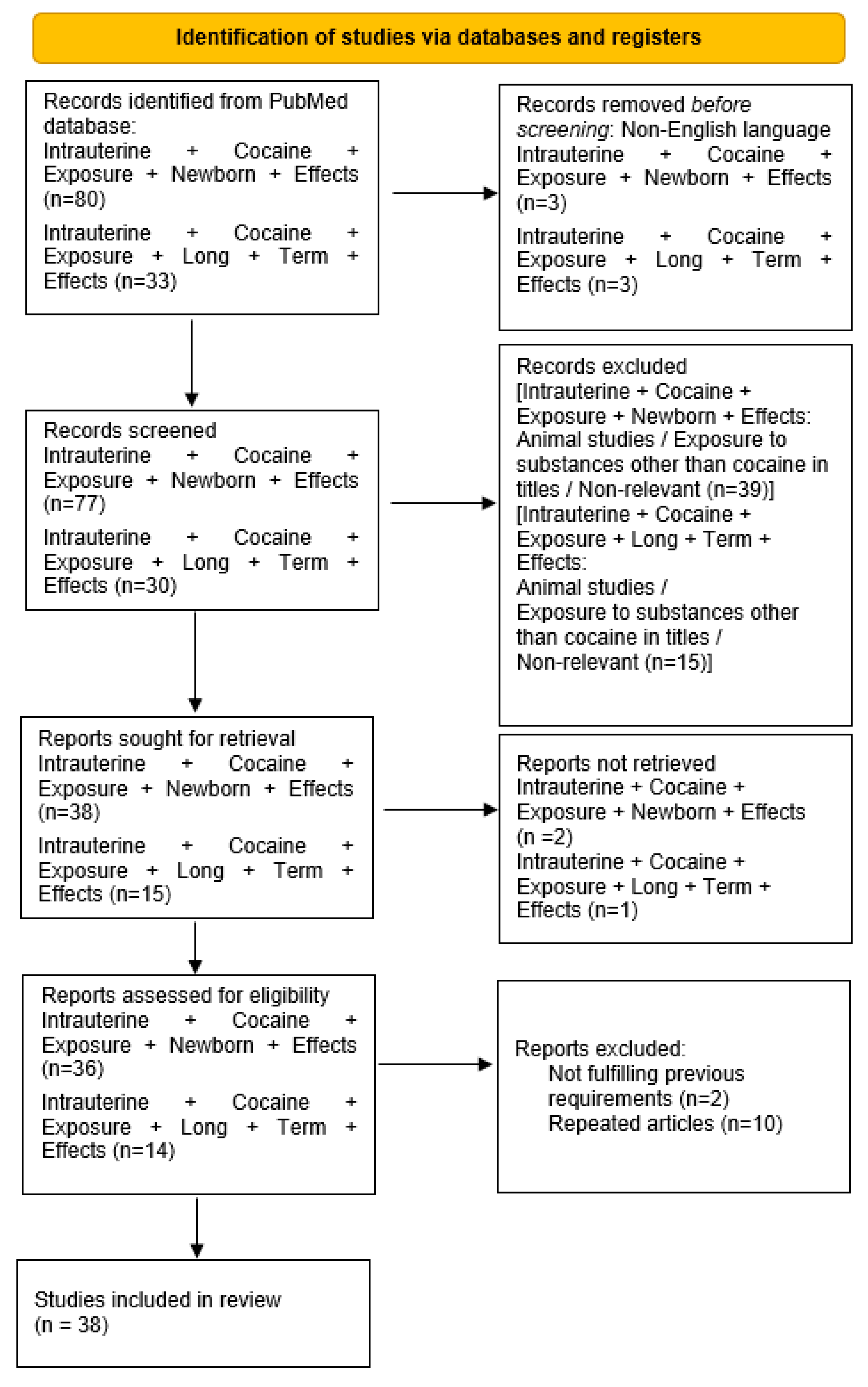
2. Material and Methods
2.1. Inclusion Criteria
2.2. Exclusion Criteria
3. Results
3.1. Birth Timing, Foetal Consequences and Infant Measurements
3.2. Neurological and Neurobehavioural Consequences
3.3. Cardiac and Respiratory Consequences
3.4. Other Consequences
3.5. Long-Term Effects
4. Discussion
5. Limitations and Scope for Further Research
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Centers for Disease Control and Prevention. National Center of Health Statistic. Illicit Drug Use. Available online: https://www.cdc.gov/nchs/fastats/drug-use-illicit.htm (accessed on 1 September 2021).
- Bhuvaneswar, C.G.; Chang, G.; Epstein, L.A.; Stern, T.A. Cocaine and Opioid Use During Pregnancy: Prevalence and Management: (Rounds in the General Hospital). Prim. Care Companion J. Clin. Psychiatry 2008, 10, 59–65. [Google Scholar] [CrossRef]
- Wendell, A.D. Overview and Epidemiology of Substance Abuse in Pregnancy. Clin. Obstet. Gynecol. 2013, 56, 91–96. [Google Scholar] [CrossRef]
- World Health Organization. Guidelines for the Identification and Management of Substance Use and Substance Use Disorders in Pregnancy. November 2014. Available online: https://www.who.int/publications/i/item/9789241548731 (accessed on 1 September 2021).
- Lester, B.M.; Andreozzi, L.; Appiah, L. Substance use during pregnancy: Time for policy to catch up with research. Harm Reduct. J. 2004, 1, 5. [Google Scholar] [CrossRef] [PubMed]
- Forray, A. Substance use during pregnancy. F1000Research 2016, 5, 887. [Google Scholar] [CrossRef] [PubMed]
- Ornoy, A.; Ergaz, Z. Alcohol Abuse in Pregnant Women: Effects on the Fetus and Newborn, Mode of Action and Maternal Treatment. Int. J. Environ. Res. Public Health 2010, 7, 364–379. [Google Scholar] [CrossRef] [PubMed]
- The American College of Obstetricians and Gynecologists. Opioid Use and Opioid Use Disorder in Pregnancy. Available online: https://www.acog.org/-/media/project/acog/acogorg/clinical/files/committee-opinion/articles/2017/08/opioid-use-and-opioid-use-disorder-in-pregnancy.pdf (accessed on 1 September 2021).
- Gouin, K.; Murphy, K.; Shah, P.S. Effects of cocaine use during pregnancy on low birthweight and preterm birth: Systematic review and metaanalyses. Am. J. Obstet. Gynecol. 2011, 204, 340.e1–340.e12. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Sehgal, S.; Ewing, C.; Waring, P.; Findlay, R.; Bean, X.; Taeusch, H.W. Morbidity of low-birthweight infants with intrauterine cocaine exposure. J. Natl. Med. Assoc. 1993, 85, 20–24. [Google Scholar]
- Singer, L.; Arendt, R.; Minnes, S. Neurodevelopmental Effects of Cocaine. Clin. Perinatol. 1993, 20, 245–262. [Google Scholar] [CrossRef]
- Van de Bor, M.; Walther, J.; Ebrahimi, M. Decreased Cardiac Output in Infants of Mothers Who Abused Cocaine. Pediatrics 1990, 85, 30–32. [Google Scholar] [CrossRef]
- Bandstra, E.S.; Morrow, C.E.; Anthony, J.C.; Churchill, S.S.; Chitwood, D.C.; Steele, B.W.; Ofir, A.Y.; Xue, L. Intrauterine Growth of Full-Term Infants: Impact of Prenatal Cocaine Exposure. Pediatrics 2001, 108, 1309–1319. [Google Scholar] [CrossRef]
- Chasnoff, I.J.; Griffith, D.R.; MacGregor, S.; Dirkes, K.; Burns, K.A. Temporal patterns of Cocaine use in Pregnancy: Perinatal Outcome. JAMA 1989, 261, 1741–1744. [Google Scholar] [CrossRef]
- Chasnoff, I.J. Cocaine, Pregnancy, and the Neonate. Women Health 1989, 15, 23–35. [Google Scholar] [CrossRef]
- Cherukuri, R.; Minkoff, H.; Feldman, J.; Parekh, A.; Glass, L. A cohort study of alkaloidal cocaine (“crack”) in pregnancy. Obstet. Gynecol. 1988, 72, 147–151. [Google Scholar]
- Bateman, D.A.; Ng, S.K.; Hansen, C.A.; Heagarty, M.C. The effects of intrauterine cocaine exposure in newborns. Am. J. Public Health 1993, 83, 190–193. [Google Scholar] [CrossRef][Green Version]
- Bateman, D.A.; Chiriboga, C.A. Dose-Response Effect of Cocaine on Newborn Head Circumference. Pediatrics 2000, 106, e33. [Google Scholar] [CrossRef]
- Van de Bor, M.; Walther, F.J.; Sims, M.E. Increased Cerebral Blood Flow Velocity in Infants of Mothers who abuse Cocaine. Pediatrics 1990, 85, 733–736. [Google Scholar] [CrossRef] [PubMed]
- Lester, B.M.; Corwin, M.J.; Sepkoski, C.; Seifer, R.; Peucker, M.; McLaughlin, S.; Golub, H.L. Neurobehavioral Syndromes in Cocaine-exposed Newborn Infants. Child Dev. 1991, 62, 694–705. [Google Scholar] [CrossRef] [PubMed]
- Hadeed, J.A.; Siegel, S.R. Maternal Cocaine Use During Pregnancy: Effect on the Newborn Infant. Pediatrics 1989, 84, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Chiriboga, C.A.; Brust, J.C.M.; Bateman, D.; Hauser, W.A. Dose–Response Effect of Fetal Cocaine Exposure on Newborn Neurologic Function. Pediatrics 1999, 103, 79–85. [Google Scholar] [CrossRef]
- Sallee Floyd, R.; Katikaneni, L.P.; McArthur, P.D.; Ibrahim, H.M.; Nesbitt, L.; Sethuraman, G. Head Growth in Cocaine-Exposed Infants: Relationship to Neonate Hair Level. J. Dev. Behav. Pediatrics 1995, 16, 77–81. [Google Scholar]
- Richardson, G.A.; Hamel, S.C.; Goldschmidt, L.; Day, N.L. Growth of Infants Prenatally Exposed to Cocaine/Crack: Comparison of a Prenatal Care and a No Prenatal Care Sample. Pediatrics 1999, 104, e18. [Google Scholar] [CrossRef]
- Hand, I.L.; Noble, L.; McVeigh, T.J.; Kim, M.; Yoon, J.J. The Effects of Intrauterine Cocaine Exposure on the Respiratory Status of the Very Low Birth Weight Infant. J. Perinatol. 2001, 21, 372–375. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Weathers, W.T.; Crane, M.M.; Sauvain, K.J.; Blackhurst, D.W. Cocaine Use in Women from a defined Population: Prevalence at Delivery and Effects on Growth in Infants. Pediatrics 1993, 91, 350–354. [Google Scholar] [CrossRef] [PubMed]
- McLenan, D.A.; Ajayi, O.A.; Bs, M.; Rydman, R.J.; Pildes, R.S. Evaluation of the relationship between cocaine and intraventricular hemorrhage. J. Natl. Med. Assoc. 1994, 86, 7. [Google Scholar]
- Avants, B.B.; Hurt, H.; Giannetta, J.M.; Epstein, C.L.; Shera, D.M.; Rao, H.; Wang, J.; Gee, J.C. Effects of Heavy in Utero Cocaine Exposure on Adolescent Caudate Morphology. Pediatr. Neurol. 2007, 37, 275–279. [Google Scholar] [CrossRef] [PubMed]
- Chiriboga, C.A.; Bateman, D.A.; Brust, J.C.M.; Allen Hauser, W. Neurologic findings in neonates with intrauterine cocaine exposure. Pediatr. Neurol. 1993, 9, 115–119. [Google Scholar] [CrossRef]
- Beltran, R.S.; Coker, S.B. Transient dystonia of infancy, a result of intrauterine cocaine exposure? Pediatr. Neurol. 1995, 12, 354–356. [Google Scholar] [CrossRef]
- LeBlanc, P.E.; Parekh, A.J.; Glass, L. Effects of Intrauterine Exposure to Alkaloidal Cocaine (‘Crack’). Am. J. Dis. Child. 1987, 141, 937–938. [Google Scholar]
- Chiriboga, C.A. Neurological Correlates of Fetal Cocaine Exposure. Ann. N. Y. Acad. Sci. 1998, 846, 109–125. [Google Scholar] [CrossRef]
- Karmel, B.Z.; Gardner, J.M. Prenatal Cocaine Exposure Effects on Arousal-Modu1ated Attention during the Neonatal Period. Dev. Psychobiol. 1996, 29, 463–480. [Google Scholar] [CrossRef]
- Swanson, M.W.; Streissguth, A.P.; Sampson, P.D.; Carmichael Olson, H. Prenatal Cocaine and Neuromotor outcome at four months: Effect of duration of exposure. Dev. Behav. Pediatrics 1999, 20, 325–334. [Google Scholar] [CrossRef]
- Chasnoff, I.J.; Hunt, C.E.; Kletter, R.; Kaplan, D. Prenatal cocaine exposure is associated with respiratory pattern abnormalities. Am. J. Dis. Child. 1989, 143, 583–587. [Google Scholar] [PubMed]
- Beeram, M.R.; Abedin, M.; Young, M.; Leftridge, C.; Dhanireddy, R. Effect of intrauterine cocaine exposure on respiratory distress syndrome in very low birthweight infants. J. Natl. Med. Assoc. 1994, 86, 370–372. [Google Scholar]
- Mehta, S.K.; Super, D.M.; Salvator, A.; Singer, L.; Connuck, D.; Fradley, L.G.; Harcar-Sevcik, R.A.; Kaufman, E.S. Heart rate variability in cocaine-exposed newborn infants. Am. Heart J. 2001, 142, 828–832. [Google Scholar] [CrossRef][Green Version]
- Mehta, S.K.; Super, D.M.; Connuck, D.; Kirchner, H.L.; Salvator, A.; Singer, L.; Fradley, L.G.; Kaufman, E.S. Autonomic alterations in cocaine-exposed infants. Am. Heart J. 2002, 144, 1109–1115. [Google Scholar] [CrossRef][Green Version]
- Mehta, S.K.; Super, D.M.; Salvator, A.; Singer, L.; Connuck, D.; Fradley, L.G.; Harcar-Sevcik, R.A.; Thomas, J.D.; Sun, J.P. Diastolic filling abnormalities by color kinesis in newborns exposed to intrauterine cocaine. J. Am. Soc. Echocardiogr. 2002, 15, 447–453. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Mehta, S.K.; Super, D.M.; Connuck, D.; Kirchner, H.L.; Salvator, A.; Singer, L.; Fradley, L.G.; Thomas, J.D.; Sun, J.P. Diastolic alterations in infants exposed to intrauterine cocaine: A follow-up study by color kinesis. J. Am. Soc. Echocardiogr. 2002, 15, 1361–1366. [Google Scholar] [CrossRef] [PubMed]
- Mitra, S.C. Effect of cocaine on fetal kidney and bladder function. J. Matern.-Fetal Med. 1999, 8, 262–269. [Google Scholar] [CrossRef]
- Hoyme, H.E.; Jones, K.L.; Dixon, S.D.; Jewtt, T.; Hanson, J.W.; Robinson, L.K.; Msall, M.E.; Allanson, J.E. Prenatal Cocaine Exposure and Fetal Vascular Disruption. Pediatrics 1998, 85, 743–747. [Google Scholar] [CrossRef]
- The’, T.G.; Young, M.; Rosser, S. In-Utero cocaine exposure and neonatal intestinal perforation: A case report. J. Natl. Med. Assoc. 1995, 87, 889–891. [Google Scholar]
- Doberczak, T.M.; Shanzer, S.; Senie, R.T.; Kandall, S.R. Neonatal neurologic and electroencephalographic effects of intrauterine cocaine exposure. J. Pediatr. 1988, 113, 354–358. [Google Scholar] [CrossRef]
- Meyer, K.D.; Zhang, L. Short- and long-term adverse effects of cocaine abuse during pregnancy on the heart development. Ther. Adv. Cardiovasc. Dis. 2009, 3, 7–16. [Google Scholar] [CrossRef]
- Beeghly, M.; Rose-Jacobs, R.; Martin, B.M.; Cabral, H.J.; Heeren, T.C.; Frank, D.A. Level of intrauterine cocaine exposure and neuropsychological test scores in preadolescence: Subtle effects on auditory attention and narrative memory. Neurotoxicol. Teratol. 2014, 45, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Giacoia, G.P. Cocaine in the cradle: A hidden epidemic. South. Med. J. 1990, 83, 947–951. [Google Scholar] [CrossRef] [PubMed]
- Presidenza del Consiglio dei Ministri. Relazione Annuale al Parlamento sul Fenomeno delle Tossicodipendenze in Italia Anno 2020 (dati 2019). Available online: https://www.iss.it/documents/20126/0/relazione-annuale-al-parlamento-2020-dati-2019.pdf/c5dd54ae-5e24-381d-7367-4ac427c2fc4b?t=1611899971308 (accessed on 1 September 2021).
- Kampschmidt, E.D. Prosecuting Women for Drug Use during Pregnancy: The Criminal Justice System Should Step Out and the Affordable Care Act Should Step Up. Health Matrix 2012, 23, 487–513. [Google Scholar]
- The American College of Obstetricians and Gynecologists. Opposition to Criminalization of Individuals during Pregnancy and the Postpartum Period. Available online: https://www.acog.org/clinical-information/policy-and-position-statements/statements-of-policy/2020/opposition-criminalization-of-individuals-pregnancy-and-postpartum-period (accessed on 1 September 2021).
- Bracchi, S. La soggettività giuridica del feto nel diritto penale. Famiglia Persone Successioni 2012, 11, 742–748. [Google Scholar]
- The American College of Obstetricians and Gynecologists. Substance Use Disorder in Pregnancy. Available online: https://www.acog.org/advocacy/policy-priorities/substance-use-disorder-in-pregnancy (accessed on 17 December 2021).
- Legge 22 Dicembre 2017, n. 219. Norme in Materia di Consenso Informato e di Disposizioni Anticipate di Trattamento. Available online: https://www.gazzettaufficiale.it/eli/id/2018/1/16/18G00006/sg (accessed on 17 December 2021).
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2013. [Google Scholar]
- Brancato, A.; Cannizzaro, C. Mothering under the influence: How perinatal drugs of abuse alter the mother-infant interaction. Rev. Neurosci. 2018, 29, 283–294. [Google Scholar] [CrossRef]
- American Society of Addiction Medicine. Substance Use, Misuse, and Use Disorders during and Following Pregnancy, with an Emphasis on Opioids. Available online: https://www.asam.org/advocacy/find-a-policy-statement/view-policy-statement/public-policy-statements/2017/01/19/substance-use-misuse-and-use-disorders-during-and-following-pregnancy-with-an-emphasis-on-opioids (accessed on 1 September 2021).
| Study | Study Design and Population | Prenatal Cocaine Exposure Assessment | Results |
|---|---|---|---|
| Sehgal et al. [11] | Case–control study 158 low-birthweight infants (500–2500 g) with a history of cocaine exposure admitted to neonatal intensive care units vs. 536 low-birthweight infants with no history of cocaine exposure | Drug-exposed infants identified either through a positive history or positive urine toxicology of the infant or mother | Low birthweight and increased incidence of necrotising enterocolitis in infants with intrauterine cocaine exposure |
| Singer et al. [12] | Review (methodological approach not described) | – | The way and degree to which foetal cocaine exposure leads to negative long-term effects on infant neurodevelopmental competence have not been established |
| Van de Bor et al. [13] | Case–control study 15 full-term newborns with a maternal history of cocaine use during pregnancy vs. 22 healthy full-term newborns admitted during the same period | Maternal history and mother’s and/or infant’s first urine samples after birth | On day 1 of life, infants exposed to cocaine had lower cardiac output, lower stroke volume, and higher arterial blood pressure. On day 2, cardiac output, stroke volume, and mean arterial blood pressure were similar |
| Bandstra et al. [14] | Case–control study 253 infants exposed prenatally to cocaine vs. 223 non-cocaine-exposed infants | Maternal interview and maternal and infant urine and meconium testing for cocaine metabolite (benzoylecgonine) | Growth deficits related to cocaine, symmetrical and partially mediated by gestational age |
| Chasnoff et al. [15] | Case–control study 75 cocaine-using women (Group 1: 23 women using cocaine in the first trimester; Group 2: 52 women using cocaine throughout pregnancy) vs. 40 women with no history or evidence of substance abuse | Maternal history and urine analysis using enzyme-multiplied immunoassay followed by gas chromatography/mass spectrometry | Group 2: increased rate of preterm delivery, low birthweight, intrauterine growth retardation; Group 1: rates of these complications similar to the drug-free group; mean birthweight, length and head circumference for term infants reduced in Group 2 infants; cocaine-exposed infants’ impairment of orientation, motor and state regulation behaviours measured using the Neonatal Behavioral Assessment Scale |
| Chasnoff et al. [16] | Case–control study 70 infants born to cocaine-using women vs. 70 drug-free infants | History and urine samples | High incidence of pregnancy complications in cocaine-addicted women; increased rate of intrauterine growth retardation, prematurity, microcephaly, and perinatal morbidity in infants born to cocaine-using women |
| Cherukuri et al. [17] | Case–control study 55 crack-using women vs. 55 parturients negative for drug use | Maternal and newborn urine testing | Higher risk of growth retardation and head circumference below the 10th percentile for gestational age in crack-exposed infants; transient abnormal neurobehavioural signs in 38% of crack-exposed infants |
| Bateman et al. [18] | Case–control study 361 cocaine-exposed infants vs. 387 infants not known to be exposed to cocaine | Maternal history or infant urine assay | Intrauterine cocaine exposure related to foetal growth retardation and shortened gestation |
| Bateman et al. [19] | Observational study 240 newborn infants (gestational age of >36 weeks) with exposure to cocaine. Cocaine exposure categorised into three levels: no exposure, low exposure and high exposure | Cocaine exposure assessed by maternal radioimmunoassay of hair (RIAH), additional maternal information from interviews and medical records, urine analysis of infants born to RIAH cocaine-positive mothers | Asymmetric intrauterine growth retardation, with head circumference disproportionately smaller than would be predicted from birthweight in infants with high intrauterine exposure to cocaine |
| Van de Bor et al. [20] | Case–control study 20 full-term newborn infants whose mothers had a history of cocaine use vs. 18 healthy full-term newborn infants whose mothers denied drug use | Maternal history, maternal and infant urine testing | On day 1 of life, cocaine-exposed infants had significantly higher peak systolic, end diastolic, and mean flow velocities in the pericallosal, internal carotid, and basilar arteries and mean arterial blood pressures. On day 2, cerebral flow velocities and mean arterial blood pressure were similar |
| Lester et al. [21] | Case–control study 80 cocaine-exposed infants vs. 80 controls | Data collected from the medical chart and based on urine tests (when available) or anamnesis | Lower birthweight, shorter length, and smaller head circumference in cases. Both direct and indirect effects (secondary to low birthweight) of cocaine on cries |
| Hadeed et al. [22] | Cohort study 56 newborn infants of mothers who used cocaine | Maternal history, maternal and infant urine samples | Growth retardation and microcephaly in newborns exposed to cocaine |
| Chiriboga et al. [23] | Case–control study 104 cocaine-exposed infants vs. 136 non-cocaine-exposed infants | Maternal radioimmunoassay of hair, additional maternal information from medical records, urine toxicology of a subset of infants and women | Dose–response relationship between cocaine exposure and adverse neonatal effects; higher rates of foetal head growth impairment and abnormalities of muscle tone, movements and posture in newborns with higher levels of prenatal cocaine exposure |
| Sallee et al. [24] | Cross-sectional study 34 infants born to mothers urine-positive for cocaine vs. 33 infants born to urine-negative mothers | Interview, maternal and urine testing, neonatal radioimmunoassay of hair | Head growth abnormalities associated with the levels of cocaine exposure |
| Richardson et al. [25] | Case–control study 295 women with prenatal care vs. 98 without prenatal care | Interview at the end of each trimester about use of cocaine, crack, alcohol, tobacco and other drugs | Growth retardation in cocaine/crack-exposed newborns |
| Hand et al. [26] | Retrospective cohort study 48 infants exposed to cocaine and 101 infants negative for drug exposure with birthweights of 750–1500 g and gestational age of <34 weeks | Maternal history and/or urine testing, infant urine testing | Short-term effects on the need for surfactant replacement therapy and initial intubation of exposed newborns with respiratory distress syndrome; no overall effect on the development of bronchopulmonary dysplasia |
| Weathers et al. [27] | Cohort study 137 infants with cocaine exposure during pregnancy | History or urine drug testing | Expected growth levels could be achieved by 1 year of age in cocaine-exposed children |
| McLenan et al. [28] | Observational study Cocaine-exposed preterm newborns examined by head ultrasound in their first week of life | Analysis of neonates’ first voided urine and/or maternal urine toxicology or history of drug use | No effect on the prevalence or severity of intraventricular haemorrhage in preterm infants exposed to cocaine |
| Avants et al. [29] | Case–control study 25 adolescents exposed to cocaine during pregnancy vs. 24 matched controls | Maternal urine testing at delivery | Dopaminergic system negatively affected by cocaine exposure during pregnancy |
| Chiriboga et al. [30] | Case–control study 14 prenatally cocaine-exposed infants vs. 16 unexposed infants | Maternal history, infant urine toxicology | Tone and movement abnormalities in newborn infants exposed to cocaine |
| Beltran et al. [31] | Case series 4 newborns positive for cocaine exposure | Maternal history and/or urine toxicology | Transient dystonic reactions initiated at 3 h to 3 months of age and continuing for months |
| Le Blanc et al. [32] | Observational study 38 children born to crack-using mothers | Maternal history, infant urine analysis | Mild and short-lived signs of central nervous system disfunction in less than half of the infants |
| Chiriboga [33] | Review (methodological approach not described) | – | Absence of evidence of detrimental long-term cocaine effects; no cognitive deficits related to foetal cocaine exposure, except as mediated through cocaine effects on head growth; abnormalities in neurological and neuropsychological function, self-limited and restricted to early infancy and childhood |
| Karmel et al. [34] | Observational study 180 infants with prenatal cocaine exposure | Maternal report, maternal or infant urine toxicology and/or meconium toxicology | Lack of appropriate arousal-modulated attention related to cocaine exposure in utero |
| Swanson et al. [35] | Case–control study 120 cocaine-exposed infants vs. 186 non-cocaine-exposed infants at 4 months | Maternal self-reports and (in most women) verification by maternal radioimmunoassay of hair | Adverse effects on infant motor development after the neonatal period related to the timing and duration of uterine cocaine exposure |
| Chasnoff et al. [36] | Case–control study 32 full-term and preterm 2-week-old cocaine-exposed infants vs. 18 heroin/methadone-exposed children 17 of 32 women used cocaine in the first trimester; 15 used cocaine throughout pregnancy | Urine screening | Higher incidence of cardiorespiratory pattern abnormalities in infants with intrauterine exposure to cocaine than in controls |
| Beeram et al. [37] | Case–control study 40 cocaine-exposed infants vs. 29 non-cocaine-exposed infants | Maternal or urine drug testing | Incidence of respiratory distress syndrome not influenced by intrauterine cocaine in very low-birthweight infants (<1500 g) |
| Mehta et al. [38] | Case–control study 68 infants with intrauterine cocaine exposure vs. 77 infants exposed to other drugs vs. 72 infants negative for drug exposure | Toxicological analysis of maternal urine, infant urine and meconium testing | Decreased heart rate variability associated with cocaine exposure |
| Mehta et al. [39] | Case–control study 71 cocaine-exposed infants (2–6 months old) vs. 89 newborns exposed to other drugs vs. 77 normal controls | Interview, questionnaire, toxicological analysis of maternal urine, infant urine and meconium testing | Lower heart rate variability in the first 72 h of life in cocaine-exposed infants with remission at 2–6 months of age; rebounding levels of vagal tone in infants exposed to light cocaine use; similar reduced response in heavy cocaine exposure |
| Mehta et al. [40] | Case–control study 82 newborns exposed to cocaine vs. 108 infants exposed to other drugs vs. 87 controls | Questionnaire, toxicological analysis of maternal urine, infant urine and meconium testing | Greater global and segmental fractional area changes and asynchrony during diastole in infants with intrauterine cocaine exposure |
| Mehta et al. [41] | Case–control study 56 2–6-month-old infants exposed to cocaine vs. 72 infants exposed to other drugs vs. 60 controls | Maternal self-report, maternal urine toxicological analysis, infant urine and meconium testing | At 2–6 months of age, infants exposed to cocaine recovered from left ventricular diastolic segmental alterations seen in the first 48 h of life; differences in heavily cocaine-exposed group |
| Mitra [42] | Case–control study Foetal hourly urine production and bladder cycle length in 36 pregnant women with cocaine abuse vs. 59 controls | Maternal history and urine drug screening for cocaine only on the day of the study | Reduced foetal urine output and bladder cycle in cases |
| Hoyme et al. [43] | Case series 10 infants with prenatal exposure to cocaine and other drugs | – | Congenital limb reduction and/or intestinal atresia or infarction in nine cases; limitations due to exposure to other substances |
| The’ et al. [44] | Case report | Maternal history and maternal and infant urine testing | Intestinal perforation in a preterm infant; mother with alcohol and cocaine abuse |
| Doberczak et al. [45] | Observational study 39 infants with intrauterine cocaine exposure | Maternal history and maternal/neonatal urine toxicologic assays | Transient and self-limited cocaine-related neonatal clinical neurological dysfunction |
| Meyer et al. [46] | Review (methodological approach not described) | – | Immediate and long-term cardiac consequences in animal model; human study incomplete but suggesting potential negative effects of cocaine exposure during development |
| Beeghly et al. [47] | Cohort study 137 preadolescents from low-income urban environments | History in medical record or neonatal or maternal urine toxicological screening, meconium assay | Association between cocaine exposure and simple sustained auditory attention test results; results not dose-dependent; other biological and environmental aspects suspected to influence neuropsychological functioning |
| Giacoia [48] | Review (methodological approach not described) | – | Microcephaly, growth retardation, brain infarcts, congenital malformations and withdrawal symptoms lasting for several weeks associated to cocaine exposure |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cestonaro, C.; Menozzi, L.; Terranova, C. Infants of Mothers with Cocaine Use: Review of Clinical and Medico-Legal Aspects. Children 2022, 9, 67. https://doi.org/10.3390/children9010067
Cestonaro C, Menozzi L, Terranova C. Infants of Mothers with Cocaine Use: Review of Clinical and Medico-Legal Aspects. Children. 2022; 9(1):67. https://doi.org/10.3390/children9010067
Chicago/Turabian StyleCestonaro, Clara, Lorenzo Menozzi, and Claudio Terranova. 2022. "Infants of Mothers with Cocaine Use: Review of Clinical and Medico-Legal Aspects" Children 9, no. 1: 67. https://doi.org/10.3390/children9010067
APA StyleCestonaro, C., Menozzi, L., & Terranova, C. (2022). Infants of Mothers with Cocaine Use: Review of Clinical and Medico-Legal Aspects. Children, 9(1), 67. https://doi.org/10.3390/children9010067






