Maternal Age, the Disparity across Regions and Their Correlation to Sudden Infant Death Syndrome in Taiwan: A Nationwide Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
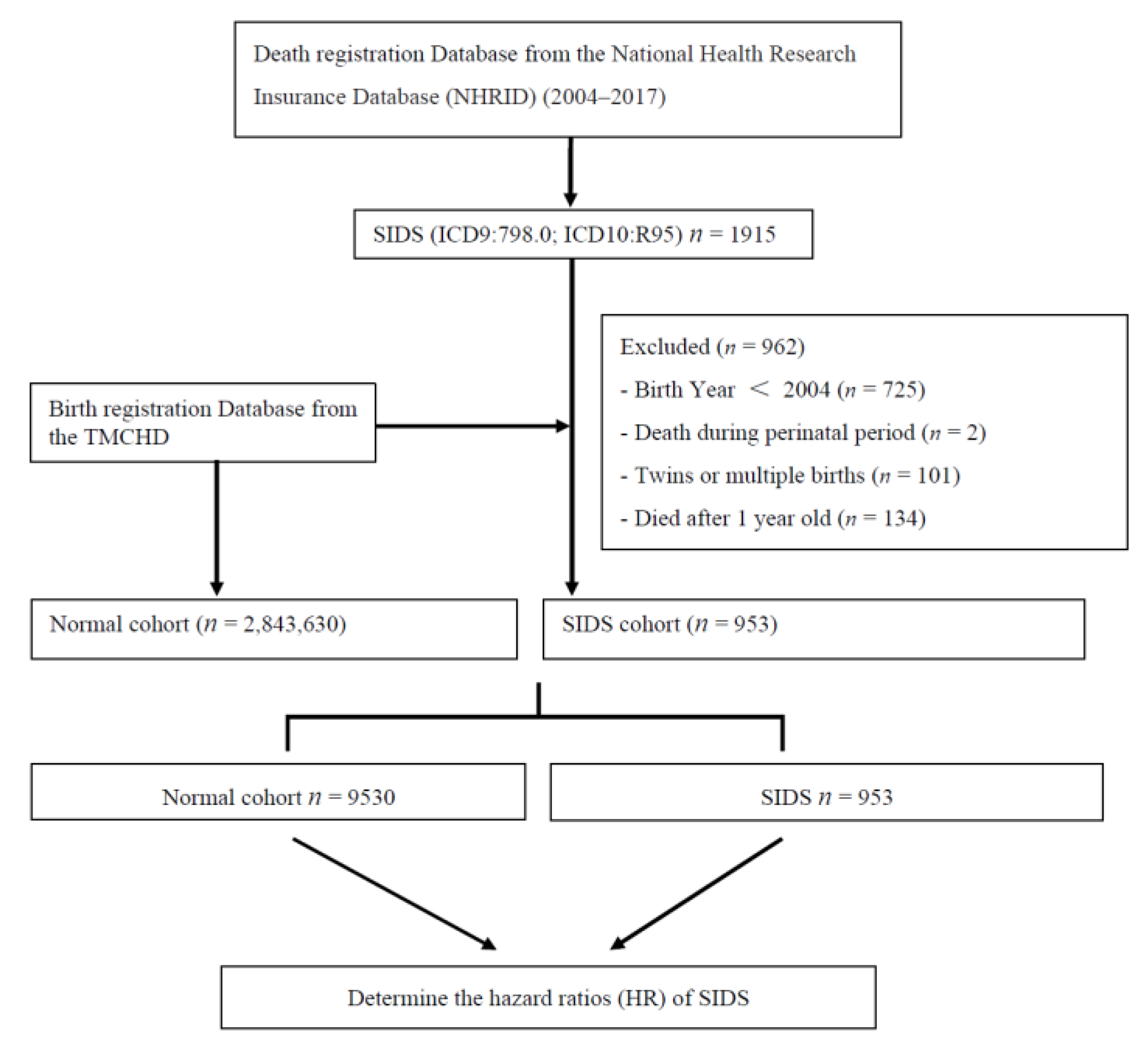
2.2. Study Population
2.3. Survival Data
2.4. Statistical Analysis
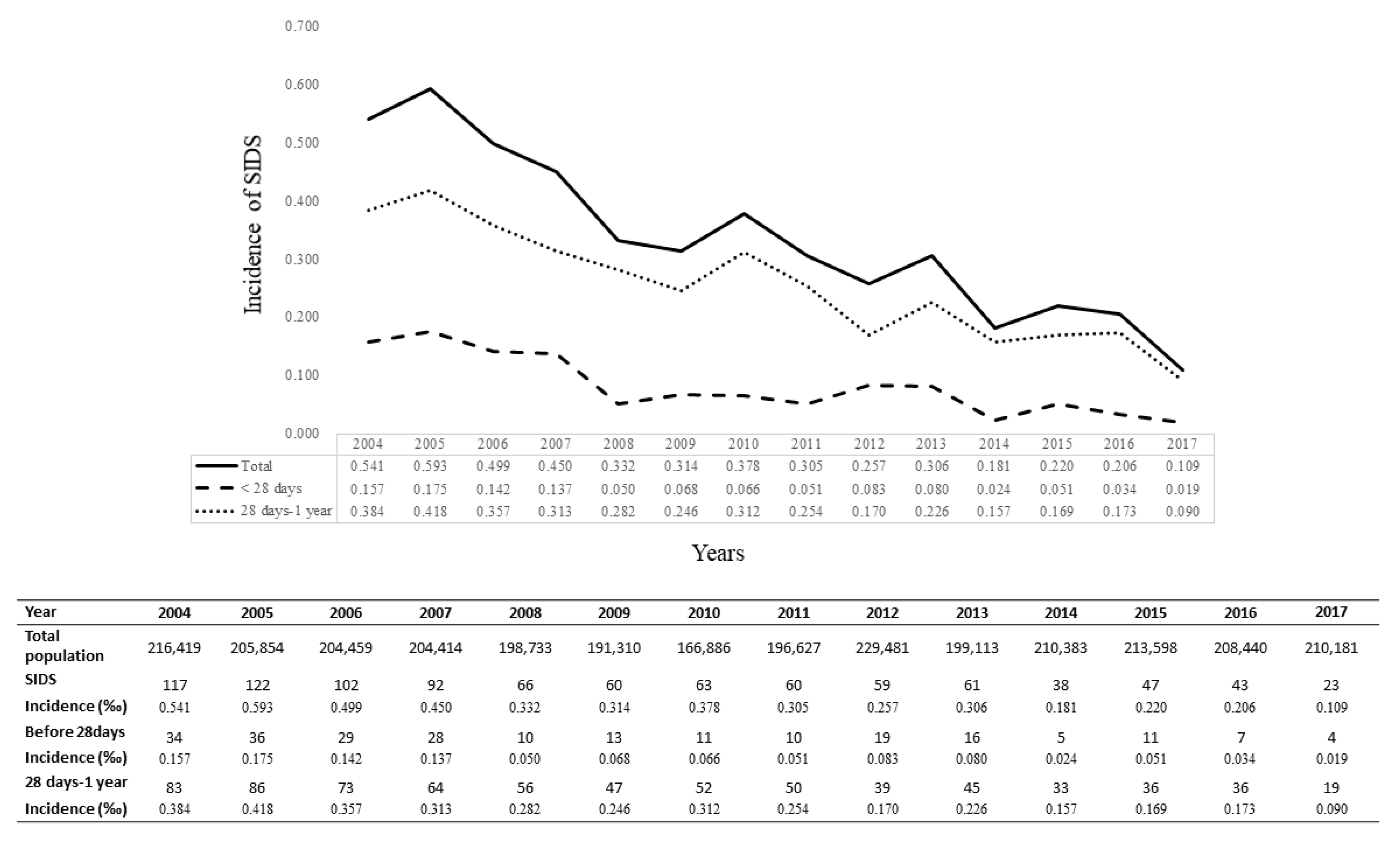
3. Results
3.1. Prediction for the Occurrence of SIDS
3.2. Comparison of the Differences between Two Groups using 20 Years of Maternal Age as the Reference in the Total Study Population
3.3. Proportion of Survival between the Maternal Age ≥20 and <20 Years Cohorts
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Goldberg, N.; Rodriguez-Prado, Y.; Tillery, R.; Chua, C. Sudden infant death syndrome: A review. Pediatr. Ann. 2018, 47, e118–e123. [Google Scholar] [CrossRef]
- Hakeem, G.F.; Oddy, L.; Holcroft, C.A.; Abenhaim, H.A. Incidence and determinants of sudden infant death syndrome: A population-based study on 37 million births. World J. Pediatr. 2015, 11, 41–47. [Google Scholar] [CrossRef]
- Kinney, H.C.; Thach, B.T. The sudden infant death syndrome. N. Engl. J. Med. 2009, 361, 795–805. [Google Scholar] [CrossRef]
- Li, D.K.; Petitti, D.B.; Willinger, M.; McMahon, R.; Odouli, R.; Vu, H.; Hoffman, H.J. Infant sleeping position and the risk of sudden infant death syndrome in California, 1997–2000. Am. J. Epidemiol. 2003, 157, 446–455. [Google Scholar] [CrossRef]
- Hwang, M.J.; Cheong, H.K.; Kim, J.H. Ambient air pollution and sudden infant death syndrome in Korea: A time-stratified case-crossover study. Int. J. Environ. Res. Public Health 2019, 16, 3273. [Google Scholar] [CrossRef] [PubMed]
- Jhun, I.; Mata, D.A.; Nordio, F.; Lee, M.; Schwartz, J.; Zanobetti, A. Ambient temperature and sudden infant death syndrome in the United States. Epidemiology 2017, 28, 728–734. [Google Scholar] [CrossRef]
- Anderson, T.M.; Lavista Ferres, J.M.; Ren, S.Y.; Moon, R.Y.; Goldstein, R.D.; Ramirez, J.M.; Mitchell, E.A. Maternal smoking before and during pregnancy and the risk of sudden unexpected infant death. Pediatrics 2019, 143, e20183325. [Google Scholar] [CrossRef]
- Horne, R.S.C. Sudden infant death syndrome: Current perspectives. Intern. Med. J. 2019, 49, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Vennemann, M.M.; Findeisen, M.; Butterfass-Bahloul, T.; Jorch, G.; Brinkmann, B.; Köpcke, W.; Bajanowski, T.; Mitchell, E.A.; GeSID Group. Modifiable risk factors for SIDS in Germany: Results of GeSID. Acta Paediatr. 2005, 94, 655–660. [Google Scholar] [CrossRef]
- Moon, R.Y.; Task Force on Sudden Infant Death Syndrome. SIDS and other sleep-related infant deaths: Evidence base for 2016 updated recommendations for a safe infant sleeping environment. Pediatrics 2016, 138, e20162940. [Google Scholar] [CrossRef] [PubMed]
- Babson, S.G.; Clarke, N.G. Relationship between infant death and maternal age. Comparison of sudden infant death incidence with other causes of infant mortality. J. Pediatr. 1983, 103, 391–393. [Google Scholar] [CrossRef]
- Pinho, A.P.; Aerts, D.; Nunes, M.L. Risk factors for sudden infant death syndrome in a developing country. Rev. Saude Publica. 2008, 42, 396–401. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Huang, C.C.; Lin, Y.C.; Huang, Y.T.; Huang, K.H. Comparison of medical issues in antenatal and perinatal periods in early youth, adolescent, and young adult mothers in Taiwan: A 10-year nationwide study. BMC Pregnancy Childbirth 2014, 14, 260. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.P.W.; Twynstra, J.; Gilliland, J.A.; Cook, J.L.; Seabrook, J.A. Risk factors and birth outcomes associated with teenage pregnancy: A Canadian sample. J. Pediatr. Adolesc. Gynecol. 2020, 33, 153–159. [Google Scholar] [CrossRef]
- Mahavarkar, S.H.; Madhu, C.K.; Mule, V.D. A comparative study of teenage pregnancy. J. Obstet. Gynaecol. 2008, 28, 604–607. [Google Scholar] [CrossRef] [PubMed]
- Caraballo, M.; Shimasaki, S.; Johnston, K.; Tung, G.; Albright, K.; Halbower, A.C. Knowledge, attitudes, and risk for sudden unexpected infant death in children of adolescent mothers: A qualitative study. J. Pediatr. 2016, 174, 78–83.e2. [Google Scholar] [CrossRef]
- Kreng, V.B.; Yang, C.T. The equality of resource allocation in health care under the National Health Insurance System in Taiwan. Health Policy 2011, 100, 203–210. [Google Scholar] [CrossRef]
- Hu, J.L.; Chang, M.C.; Chung, H.J. Projecting the target quantity of medical staff in Taiwan’s administrative regions by the theory of carrying capacity. Int. J. Environ. Res. Public Health 2020, 17, 2998. [Google Scholar] [CrossRef]
- Ely, D.M.; Hoyert, D.L. Differences between rural and urban areas in mortality rates for the leading causes of infant death: United States, 2013–2015. NCHS Data Brief 2018, 300, 1–8. [Google Scholar]
- Womack, L.S.; Rossen, L.M.; Hirai, A.H. Urban-rural infant mortality disparities by race and ethnicity and cause of death. Am. J. Prev. Med. 2020, 58, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Mohamoud, Y.A.; Kirby, R.S.; Ehrenthal, D.B. Poverty, urban-rural classification and term infant mortality: A population-based multilevel analysis. BMC Pregnancy Childbirth 2019, 19, 40. [Google Scholar] [CrossRef]
- Wu, T.Y.; Majeed, A.; Kuo, K.N. An overview of the healthcare system in Taiwan. Lond. J. Prim. Care 2010, 3, 115–119. [Google Scholar] [CrossRef]
- Lu, W.L.; Shen, P.C.; Lee, C.H.; Su, Y.T.; Chen, L.M. High risk of early cataracts in young type 1 diabetes group: A nationwide cohort study. Int. J. Endocrinol. 2020, 2020, 8160256. [Google Scholar] [CrossRef]
- Hsieh, C.Y.; Su, C.C.; Shao, S.C.; Sung, S.F.; Lin, S.J.; Kao Yang, Y.H.; Lai, E.C. Taiwan’s National Health Insurance Research Database: Past and future. Clin. Epidemiol. 2019, 11, 349–358. [Google Scholar] [CrossRef]
- Hsu, S.T.; Hsieh, C.J.; Chen, H.W.; Jeng, S.F.; Wu, H.C.; Chen, M.H.; Chen, C.Y.; Chou, H.C.; Tsao, P.N.; Chen, P.C.; et al. Nationwide birth weight and gestational age-specific neonatal mortality rate in Taiwan. Pediatr. Neonatol. 2015, 56, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Health Promotion Administration, Ministry of Health and Welfare in Taiwan. Reporting. Available online: http://www.hpa.gov.tw/English/ClassPrint.aspx?No=201502020008 (accessed on 5 May 2021).
- Li, C.Y.; Chen, L.H.; Chiou, M.J.; Liang, F.W.; Lu, T.H. Set-up and future applications of the Taiwan Maternal and Child Health Database (TMCHD). Taiwan J. Public Health 2016, 35, 221–233. [Google Scholar]
- Leftwich, H.K.; Alves, M.V. Adolescent pregnancy. Pediatr. Clin. N. Am. 2017, 64, 381–388. [Google Scholar] [CrossRef]
- Chu, T.B.; Liu, T.C.; Chen, C.S.; Tsai, Y.W.; Chiu, W.T. Household out-of-pocket medical expenditures and National Health Insurance in Taiwan: Income and regional inequality. BMC Health Serv. Res. 2005, 5, 60. [Google Scholar] [CrossRef]
- Malloy, M.H. Prematurity and sudden infant death syndrome: United States 2005–2007. J. Perinatol. 2013, 33, 470–475. [Google Scholar] [CrossRef] [PubMed]
- Reidpath, D.D.; Allotey, P. Infant mortality rate as an indicator of population health. J. Epidemiol. Community Health 2003, 57, 344–346. [Google Scholar] [CrossRef]
- Thakrar, A.P.; Forrest, A.D.; Maltenfort, M.G.; Forrest, C.B. Child mortality in the US and 19 OECD comparator nations: A 50-year time-trend analysis. Health Aff. 2018, 37, 140–149. [Google Scholar] [CrossRef]
- Liang, F.W.; Chou, H.C.; Chiou, S.T.; Chen, L.H.; Wu, M.H.; Lue, H.C.; Chiang, T.L.; Lu, T.H. Trends in birth weight-specific and -adjusted infant mortality rates in Taiwan between 2004 and 2011. Pediatr. Neonatol. 2018, 59, 267–273. [Google Scholar] [CrossRef]
- Liang, F.W.; Lu, T.H.; Wu, M.H.; Lue, H.C.; Chiang, T.L.; Huang, Y.L.; Chen, L.H. International ranking of infant mortality rates: Taiwan compared with European countries. Pediatr. Neonatol. 2016, 57, 326–332. [Google Scholar] [CrossRef][Green Version]
- Department of Statistics, Ministry of Health and Welfare. The Collaboration Center for Health Information Application, Ministry of Health and Welfare. 2021. Available online: https://dep.mohw.gov.tw/dos/cp-1720-7287-113.html (accessed on 20 May 2021).
- Tzeng, I.S.; Chen, K.H.; Lee, Y.L.; Yang, W.S. Trends and age-period-cohort effects of fertility rate: Analysis of 26,224 married women in Taiwan. Int. J. Environ. Res. Public Health 2019, 16, 4952. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.W.; Tsai, C.Y.; Sung, F.C.; Lee, Y.Y.; Lu, T.H.; Li, C.Y.; Ko, M.C. Adverse birth outcomes among pregnancies of teen mothers: Age-specific analysis of national data in Taiwan. Child. Care Health Dev. 2010, 36, 232–240. [Google Scholar] [CrossRef]
- Wang, R.H.; Wang, H.H.; Hsu, M.T. Factors associated with adolescent pregnancy- a sample of Taiwanese female adolescents. Public Health Nurs. 2003, 20, 33–41. [Google Scholar] [CrossRef] [PubMed]
- Xavier, C.; Benoit, A.; Brown, H.K. Teenage pregnancy and mental health beyond the postpartum period: A systematic review. J. Epidemiol. Community Health 2018, 72, 451–457. [Google Scholar] [CrossRef]
- Cunnington, A.J. What’s so bad about teenage pregnancy? J. Fam. Plann. Reprod. Health Care 2001, 27, 36–41. [Google Scholar] [CrossRef]
- Vargas, G.; Borus, J.; Charlton, B.M. Teenage pregnancy prevention: The role of young men. Curr. Opin. Pediatr. 2017, 29, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Stanger-Hall, K.F.; Hall, D.W. Abstinence-only education and teen pregnancy rates: Why we need comprehensive sex education in the U.S. PLoS ONE 2011, 6, e24658. [Google Scholar] [CrossRef]
- Kong, F.; Wang, A.; He, J.; Xiong, L.; Xie, D.; Su, J.; Liu, Z. Trend of unintentional suffocation death for infants under 1 year of age from 2009 to 2018 in Hunan, China: A cross-sectional study. BMJ Open 2020, 10, e038666. [Google Scholar] [CrossRef]
- Hsin, Y.C.; Chang, Y.C.; Lee, E.P.; Chiu, C.H.; Chou, I.J.; Hsia, S.H.; Lin, K.L.; Lee, J.; Huang, J.L.; Wang, C.J.; et al. Prevention, Protection Against Child Abuse, Neglect (PCHAN) Study Group. Risk factors for child maltreatment by the utilization of medical service and socioeconomic environment in Taiwan. Medicine 2018, 97, e13728. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatrics; Hymel, K.P.; Committee on Child Abuse and Neglect; National Association of Medical Examiners. Distinguishing sudden infant death syndrome from child abuse fatalities. Pediatrics 2006, 118, 421–427. [Google Scholar] [CrossRef] [PubMed]
- Howard, L.M.; Hannam, S. Sudden infant death syndrome and psychiatric disorders. Br. J. Psychiatry 2003, 182, 379–380. [Google Scholar] [CrossRef]
- Howard, L.M.; Kirkwood, G.; Latinovic, R. Sudden infant death syndrome and maternal depression. J. Clin. Psychiatry 2007, 68, 1279–1283. [Google Scholar] [CrossRef] [PubMed]
- Chou, W.J. Maternal mental health and child development in Asian immigrant mothers in Taiwan. J. Formos. Med. Assoc. 2010, 109, 293–302. [Google Scholar] [CrossRef][Green Version]
- Shu, B.C.; Lung, F.W.; Chen, C.H. Mental health of female foreign spouses in transnational marriages in southern Taiwan. BMC Psychiatry 2011, 11, 4. [Google Scholar] [CrossRef]
- Foss, G.F.; Chantal, A.W.; Hendrickson, S. Maternal depression and anxiety and infant development: A comparison of foreign-born and native-born mothers. Public Health Nurs. 2004, 21, 237–246. [Google Scholar] [CrossRef]
- Lee, C.H. Sudden Infant Death Syndrome in Taiwan: A comparative epidemiological survey on cases with and without forensic autopsy. Master’s Thesis, Graduate Institute of Forensic Medicine, College of Medicine, National Taiwan University, Taipei, Taiwan, 2012. (In Chinese) [Google Scholar] [CrossRef]
- Chang, Y.C.; Huang, J.L.; Hsia, S.H.; Lin, K.L.; Lee, E.P.; Chou, I.J.; Hsin, Y.C.; Lo, F.S.; Wu, C.T.; Chiu, C.H.; et al. Prevention, Protection Against Child Abuse, Neglect (PCHAN) Study Group. Child protection medical service demonstration centers in approaching child abuse and neglect in Taiwan. Medicine 2016, 95, e5218. [Google Scholar] [CrossRef] [PubMed]

| Normal Cohort n = 9530 | SIDS Cohort n = 953 | p-Value | |
|---|---|---|---|
| Gestational age | 37.34 ± 3.31 | 37.34 ± 3.31 | >0.9999 |
| Infant sex | 0.0013 | ||
| Boy | 4911 (51.53%) | 543 (56.98%) | |
| Girl | 4619 (48.47%) | 410 (43.02%) | |
| Birth weight | 2913.5 ± 658.04 | 2842.78 ± 638.06 | 0.0015 |
| Native citizen (mother) | 8744 (91.75%) | 913 (95.8%) | <0.0001 |
| Age of father | 33.84 ± 5.49 | 32.8 ± 6.10 | <0.0001 |
| Age of mother | 30.73 ± 5.03 | 28.18 ± 5.87 | <0.0001 |
| Region (in Taiwan) | 0.0039 | ||
| Northern | 2869 (30.1%) | 249 (26.13%) | |
| North Central | 1761 (18.48%) | 213 (22.35%) | |
| Central | 1908 (20.02%) | 181 (18.99%) | |
| South Central | 1238 (12.99%) | 123 (12.91%) | |
| Southern | 1409 (14.78%) | 138 (14.48%) | |
| Eastern | 345 (3.62%) | 49 (5.14%) | |
| Mode of delivery | 0.0056 | ||
| Vagina | 5813 (61%) | 625 (65.58%) | |
| Cesarean section | 3717 (39%) | 328 (34.42%) | |
| Apgar score (1 min) | 8.07 ± 1.34 | 7.66 ± 1.96 | <0.0001 |
| Apgar score (5 min) | 9.84 ± 1.27 | 9.2 ± 2.72 | <0.0001 |
| Maternal and obstetric risk factors | |||
| Anemia | 79 (0.83%) | 6 (0.63%) | 0.5129 |
| Hypertensive disorder | 186 (1.95%) | 15 (1.57%) | 0.4175 |
| Premature rupture of membranes | 285 (2.99%) | 10 (1.05%) | 0.0006 |
| Fetal distress | 142 (1.49%) | 28 (2.94%) | 0.0007 |
| Crude HR (95% CI) | p | Adjusted HR (95% CI) | p | |
|---|---|---|---|---|
| Maternal age (<20 vs. ≥20 years) | 4.22 (3.38–5.27) | <0.0001 | 2.81 (1.43–5.50) | <0.01 |
| Gender | 1.23 (1.08–1.40) | <0.01 | 1.20 (0.93–1.56) | 0.166 |
| Birth weight | 1.00 (1.00–1.00) | <0.01 | 1.00 (1.00–1.00) | 0.083 |
| Paternal age | 0.97 (0.95–0.98) | <0.0001 | 0.96 (0.94–0.99) | <0.01 |
| Native citizen (mother) | 1.99 (1.45–2.74) | <0.0001 | 1.78 (0.90–3.50) | 0.095 |
| Region (in Taiwan) | ||||
| Northern | 0.62 (0.46–0.84) | <0.01 | 0.42 (0.20–0.88) | <0.05 |
| North Central | 0.86 (0.63–1.17) | 0.326 | 0.42 (0.20–0.89) | <0.05 |
| Central | 0.68 (0.50–0.93) | <0.05 | 0.37 (0.18–0.80) | <0.05 |
| South Central | 0.71 (0.51–0.99) | <0.05 | 0.37 (0.17–0.82) | <0.05 |
| Southern | 0.70 (0.51–0.97) | <0.05 | 0.35 (0.16–0.77) | <0.01 |
| Eastern | REF. | REF. | ||
| Gestational age | 1.00 (0.98–1.02) | 0.868 | 1.11 (1.01–1.21) | <0.05 |
| Mode of delivery | 1.21 (1.06–1.38) | <0.01 | 1.18 (0.88–1.58) | 0.262 |
| Apgar score (1 min) | 0.85 (0.82–0.88) | <0.0001 | 0.73 (0.55–0.96) | <0.05 |
| Apgar score (5 min) | 0.85 (0.81–0.88) | <0.0001 | 0.97 (0.76–1.24) | 0.832 |
| Maternal and obstetric risk factors | ||||
| Anemia | 0.76 (0.34–1.70) | 0.505 | 1.12 (0.16–8.11) | 0.910 |
| Hypertensive disorder | 0.82 (0.49–1.36) | 0.434 | 1.35 (0.49–3.70) | 0.557 |
| Premature rupture of membranes | 0.36 (0.19–0.66) | <0.05 | 0.43 (0.13–1.36) | 0.150 |
| Fetal distress | 1.98 (1.36–2.88) | <0.05 | 0.61 (0.14–2.58) | 0.502 |
| Age < 20 Years Cohort (n = 267) | Age ≥ 20 Years Cohort (n = 10,216) | p | |
|---|---|---|---|
| Cases of SIDS | 85 (31.84%) | 868 (8.50%) | <0.0001 |
| Birth weight | 2679.94 ± 734.43 | 2913.01 ± 653.35 | <0.0001 |
| Native citizen (mother) | 252 (94.38%) | 9405 (92.06%) | 0.1647 |
| Paternal age | 25.19 ± 5.26 | 33.88 ± 5.45 | <0.0001 |
| Maternal age | 18.15 ± 1.31 | 30.82 ± 4.82 | <0.0001 |
| Region (in Taiwan) | <0.0001 | ||
| Northern | 47 (17.60%) | 3071 (30.06%) | |
| North Central | 59 (22.10%) | 1915 (18.75%) | |
| Central | 56 (20.97%) | 2033 (19.90%) | |
| South Central | 43 (16.10%) | 1318 (12.90%) | |
| Southern | 42 (15.73%) | 1505 (14.73%) | |
| Eastern | 20 (7.49%) | 374 (3.66%) | |
| Gestational age | 36.56 ± 4.43 | 37.36 ± 3.27 | 0.0001 |
| Mode of delivery | <0.0001 | ||
| Vagina | 218 (81.65%) | 6220 (60.88%) | |
| Cesarean section | 49 (18.35%) | 3996 (39.12%) | |
| Apgar score (1 min) | 7.57 ± 1.92 | 8.04 ± 1.39 | <0.0001 |
| Apgar score (5 min) | 9.12 ± 2.86 | 9.79 ± 1.42 | 0.0002 |
| Maternal and obstetric risk factors | |||
| Anemia | 7 (2.62%) | 78 (0.76%) | 0.0008 |
| Hypertensive disorder | 3 (1.12%) | 198 (1.94%) | 0.3380 |
| Premature rupture of membranes | 6 (2.25%) | 289 (2.83%) | 0.5704 |
| Fetal distress | 3 (1.12%) | 167 (1.63%) | 0.5139 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, L.-Y.; Chen, W.-J.; Yang, Y.-N.; Wu, C.-Y.; Wu, P.-L.; Tey, S.-L.; Yang, S.-N.; Liu, H.-K. Maternal Age, the Disparity across Regions and Their Correlation to Sudden Infant Death Syndrome in Taiwan: A Nationwide Cohort Study. Children 2021, 8, 771. https://doi.org/10.3390/children8090771
Huang L-Y, Chen W-J, Yang Y-N, Wu C-Y, Wu P-L, Tey S-L, Yang S-N, Liu H-K. Maternal Age, the Disparity across Regions and Their Correlation to Sudden Infant Death Syndrome in Taiwan: A Nationwide Cohort Study. Children. 2021; 8(9):771. https://doi.org/10.3390/children8090771
Chicago/Turabian StyleHuang, Lin-Yi, Wan-Ju Chen, Yung-Ning Yang, Chien-Yi Wu, Pei-Ling Wu, Shu-Leei Tey, San-Nan Yang, and Hsien-Kuan Liu. 2021. "Maternal Age, the Disparity across Regions and Their Correlation to Sudden Infant Death Syndrome in Taiwan: A Nationwide Cohort Study" Children 8, no. 9: 771. https://doi.org/10.3390/children8090771
APA StyleHuang, L.-Y., Chen, W.-J., Yang, Y.-N., Wu, C.-Y., Wu, P.-L., Tey, S.-L., Yang, S.-N., & Liu, H.-K. (2021). Maternal Age, the Disparity across Regions and Their Correlation to Sudden Infant Death Syndrome in Taiwan: A Nationwide Cohort Study. Children, 8(9), 771. https://doi.org/10.3390/children8090771






