Analysis of Clinical Outcome and Predictors of Mortality in Pediatric Trauma Population: Evidence from a 10 Year Analysis in a Single Center
Abstract
:1. Introduction
2. Methods
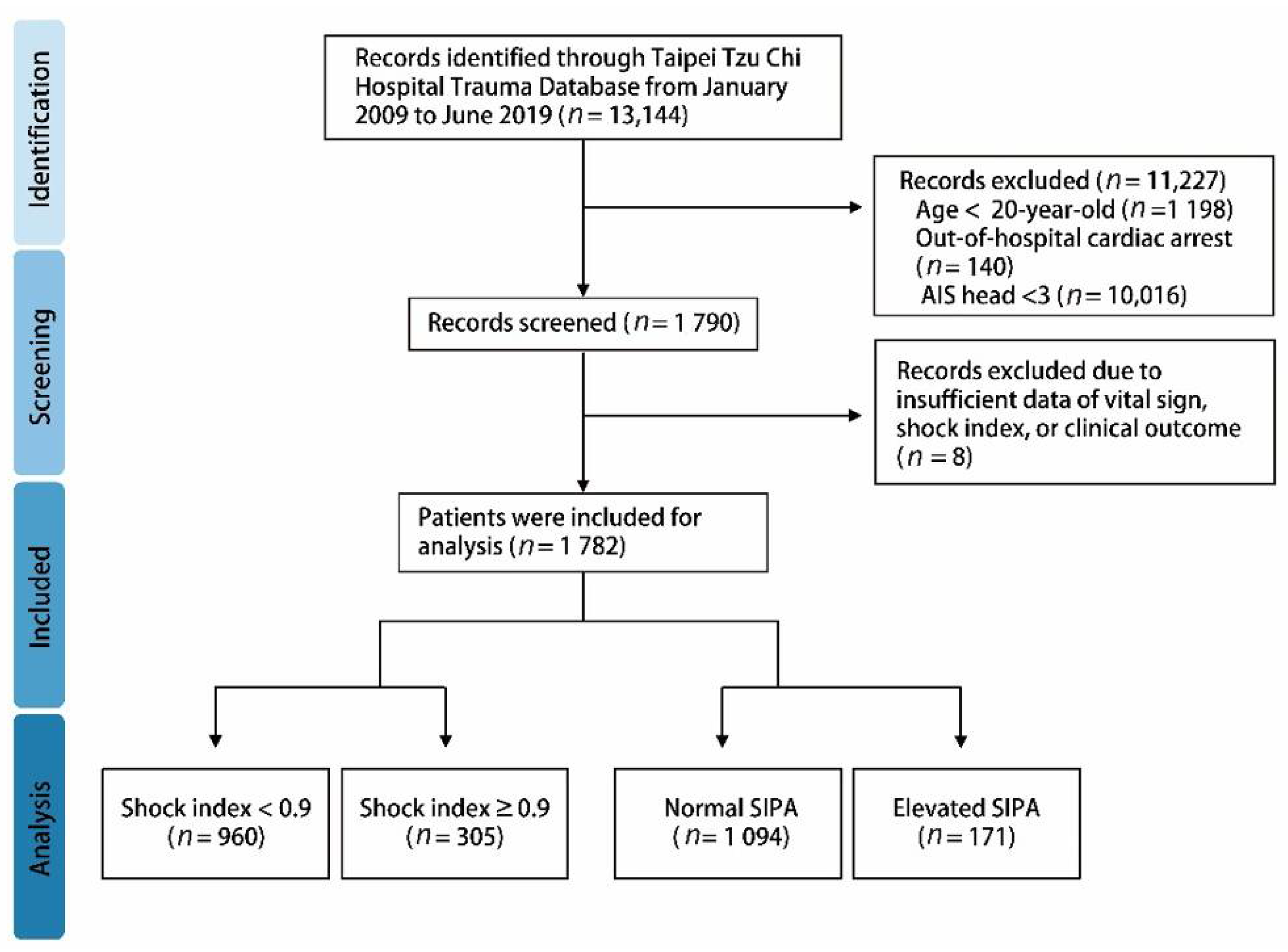
2.1. Study Design and Inclusion Criteria
2.2. Shock Index and Pediatric Age-Adjusted Shock Index
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Injuries and Violence: The Facts 2014; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Bruijns, S.R.; Guly, H.R.; Bouamra, O.; Lecky, F.; Lee, W.A. The value of traditional vital signs, shock index, and age-based markers in predicting trauma mortality. J. Trauma Acute Care Surg. 2013, 74, 1432–1437. [Google Scholar] [CrossRef] [PubMed]
- Ott, R.; Krämer, R.; Martus, P.; Bussenius-Kammerer, M.; Carbon, R.; Rupprecht, H. Prognostic value of trauma scores in pediatric patients with multiple injuries. J. Trauma 2000, 49, 729–736. [Google Scholar] [CrossRef] [PubMed]
- Eichelberger, M.R.; Gotschall, C.S.; Sacco, W.J.; Bowman, L.M.; Mangubat, E.A.; Lowenstein, A.D. A comparison of the trauma score, the revised trauma score, and the pediatric trauma score. Ann. Emerg. Med. 1989, 18, 1053–1058. [Google Scholar] [CrossRef]
- Nordin, A.; Coleman, A.; Shi, J.; Wheeler, K.; Xiang, H.; Acker, S.; Bensard, D.; Kenney, B. Validation of the age-adjusted shock index using pediatric trauma quality improvement program data. J. Pediatric Surg. 2018, 53, 130–135. [Google Scholar] [CrossRef] [PubMed]
- Acker, S.N.; Ross, J.T.; Partrick, D.A.; Tong, S.; Bensard, D.D. Pediatric specific shock index accurately identifies severely injured children. J. Pediatric Surg. 2015, 50, 331–334. [Google Scholar] [CrossRef] [PubMed]
- Linnaus, M.E.; Notrica, D.M.; Langlais, C.S.; St. Peter, S.D.; Leys, C.M.; Ostlie, D.J.; Maxson, R.T.; Ponsky, T.; Tuggle, D.W.; Eubanks, J.W.; et al. Prospective validation of the shock index pediatric-adjusted (SIPA) in blunt liver and spleen trauma: An ATOMAC+ study. J. Pediatric Surg. 2017, 52, 340–344. [Google Scholar] [CrossRef] [PubMed]
- Koch, E.; Lovett, S.; Nghiem, T.; Riggs, R.A.; Rech, M.A. Shock index in the emergency department: Utility and limitations. Open Access Emerg. Med. OAEM 2019, 11, 179–199. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, M.-Y.; Chen, Y.-L.; Yiang, G.-T.; Li, C.-J.; Lin, A.S.-C. Clinical Outcome and Management for Geriatric Traumatic Injury: Analysis of 2688 Cases in the Emergency Department of a Teaching Hospital in Taiwan. J. Clin. Med. 2018, 7, 255. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Birkhahn, R.H.; Gaeta, T.J.; Terry, D.; Bove, J.J.; Tloczkowski, J. Shock index in diagnosing early acute hypovolemia. Am. J. Emerg. Med. 2005, 23, 323–326. [Google Scholar] [CrossRef] [PubMed]
- Vandromme, M.J.; Griffin, R.L.; Kerby, J.D.; McGwin, G., Jr.; Rue, L.W., III; Weinberg, J.A. Identifying Risk for Massive Transfusion in the Relatively Normotensive Patient: Utility of the Prehospital Shock Index. J. Trauma Acute Care Surg. 2011, 70, 384–390. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DeMuro, J.P.; Simmons, S.; Jax, J.; Gianelli, S.M. Application of the shock index to the prediction of need for hemostasis intervention. Am. J. Emerg. Med. 2013, 31, 1260–1263. [Google Scholar] [CrossRef]
- Acker, S.N.; Bredbeck, B.; Partrick, D.A.; Kulungowski, A.M.; Barnett, C.C.; Bensard, D.D. Shock index, pediatric age-adjusted (SIPA) is more accurate than age-adjusted hypotension for trauma team activation. Surgery 2017, 161, 803–807. [Google Scholar] [CrossRef] [PubMed]




| Age | Heart Rate | Systolic Blood Pressure | Shock Index Cutoff Value |
|---|---|---|---|
| ≤3 years | 70–110 | 90–110 | 1.2 |
| 4–6 years | 65–110 | 90–110 | 1.2 |
| 7–12 years | 60–100 | 100–120 | 1.0 |
| >12 years | 55–90 | 100–135 | 0.9 |
| Characteristics | All Pediatric Population |
|---|---|
| N = 1265 | |
| Age (years), mean ± SD | 14.27 ± 5.51 |
| Male, n (%) | 912(72.1%) |
| Underlying diseases, n (%) | 70(5.5%) |
| Vital sign | |
| SBP, mean ± SD | 126.73 ± 23.48 |
| DBP, mean ± SD | 75.33 ± 13.67 |
| RR, mean ± SD | 19.17 ± 2.58 |
| HR, mean ± SD | 93.56 ± 19.57 |
| Triage | |
| I | 96(7.6%) |
| II | 698(55.2%) |
| III | 467(36.9%) |
| IV + V | 4(0.3%) |
| Consciousness level | |
| 15 | 1152(91.1%) |
| 8–15 | 88(7.0%) |
| ≤8 | 24(1.9%) |
| Injury site | |
| Home | 160(12.6%) |
| Street | 760(60.1%) |
| Public site | 268(21.2%) |
| Others | 77(6.1%) |
| Mechanism | |
| Motor Vehicle Collision | 672(53.1%) |
| Fall | 387(30.6%) |
| Crushing injury | 76(6.0%) |
| Sharp object | 55(4.3%) |
| Others | 75(5.9%) |
| Injured area | |
| Head and neck | 251(18.8%) |
| Face | 199(15.7%) |
| Thorax | 82(6.5%) |
| Abdomen | 91(7.2%) |
| Extremity | 920(72.7%) |
| Activation of trauma team | 58(4.6%) |
| Trauma scores | |
| Shock index | 0.77 ± 0.24 |
| Shock index ≥ 0.9 | 305(24.1%) |
| SIPA | 0.86 ± 0.34 |
| Elevated SIPA | 171(13.5%) |
| ISS, (mean; SD) | 6.51 ± 5.80 |
| ISS ≥ 16, (%) | 78(6.2%) |
| RTS, (mean; SD) | 7.70 ± 0.63 |
| NISS, (mean; SD) | 7.36 ± 6.89 |
| TRISS, (mean; SD) | 0.98 ± 0.10 |
| Clinical outcome | |
| LOS days, (median; IQR) | 5.0 (3.0–9.0) |
| ICU Admission, (%) | 177(14.0%) |
| ICU Readmission, (%) | 2(0.2%) |
| ICU days, (median; IQR) | 4.0 (2.0–6.0) |
| Need for surgery (%) | 867(68.5%) |
| Reoperation (%) | 49(3.9%) |
| Death, (%) | 7(0.6%) |
| Characteristics | SI < 0.9 | SI ≥ 0.9 | p-Value | Normal SIPA | Elevated SIPA | p-Value |
|---|---|---|---|---|---|---|
| N = 960 | N = 305 | N = 1094 | N = 171 | |||
| Age (years), mean ± SD | 15.91 ± 4.04 | 9.09 ± 6.27 | <0.001 | 14.63 ± 5.22 | 11.97 ± 6.69 | <0.001 |
| Male, n (%) | 727(75.73%) | 185(60.66%) | <0.001 | 808(73.86%) | 104(60.82%) | <0.001 |
| Underlying diseases, n (%) | 58(6.04%) | 12(3.93%) | 0.161 | 63(5.76%) | 7(4.09%) | 0.376 |
| Vital sign | ||||||
| SBP, mean ± SD | 133.69 ± 20.63 | 104.83 ± 17.78 | <0.001 | 130.67 ± 21.64 | 101.53 ± 18.74 | <0.001 |
| DBP, mean ± SD | 78.07 ± 12.24 | 66.70 ± 14.33 | <0.001 | 77.01 ± 12.87 | 64.54 ± 13.69 | <0.001 |
| RR, mean ± SD | 18.78 ± 2.0 | 20.39 ± 3.61 | <0.001 | 19.01 ± 2.23 | 20.17 ± 4.06 | <0.001 |
| HR, mean ± SD | 87.19 ± 14.53 | 113.62 ± 19.85 | <0.001 | 90.05 ± 16.83 | 116.06 ± 20.90 | <0.001 |
| Injury site | ||||||
| Home | 72(7.50%) | 88(28.85%) | <0.001 | 125(11.43%) | 35(20.47%) | <0.001 |
| Street | 631(65.73%) | 129(42.30%) | <0.001 | 666(60.88%) | 94(54.97%) | 0.143 |
| Public site | 86(8.96%) | 29(9.51%) | 0.771 | 104(9.51%) | 11(6.43%) | 0.194 |
| Others | 165(17.19%) | 56(18.36%) | 0.638 | 191(17.46%) | 30(17.54%) | 0.978 |
| ISS, (mean; SD) | 6.33 ± 5.28 | 7.10 ± 7.20 | 0.084 | 6.22 ± 5.08 | 8.39 ± 8.98 | 0.002 |
| ISS ≥ 16, (%) | 46(4.79%) | 32(10.49%) | <0.001 | 52(4.75%) | 26(15.20%) | <0.001 |
| RTS, (mean; SD) | 7.75 ± 0.52 | 7.53 ± 0.87 | <0.001 | 7.74 ± 0.55 | 7.42 ± 0.94 | <0.001 |
| NISS, (mean; SD) | 7.17 ± 6.32 | 7.97 ± 8.42 | 0.126 | 7.04 ± 6.08 | 9.40 ± 10.49 | 0.005 |
| TRISS, (mean; SD) | 0.98 ± 0.09 | 0.97 ± 0.13 | 0.091 | 0.98 ± 0.09 | 0.97 ± 0.12 | 0.152 |
| LOS days, (median; IQR) | 5.0 (3.0–9.0) | 3.0 (2.0–7.0) | <0.001 | 5.0(3.0–9.0) | 4.0(2.0–10.0) | 0.204 |
| ICU admission, (%) | 137(14.27%) | 40(13.11%) | 0.612 | 162(14.81%) | 15(8.77%) | 0.034 |
| ICU readmission, (%) | 2(0.21%) | 0(0.00%) | 1.000 | 2(0.18%) | 0(0.00%) | 1.000 |
| ICU days, (median; IQR) | 4.0 (3.0–6.0) | 3.5 (2.0–6.0) | 0.556 | 4.0(2.0–6.0) | 3.0(2.0–5.0) | 0.411 |
| Need for surgery (%) | 664(69.17%) | 203(66.56%) | 0.363 | 753(68.83%) | 114(66.67%) | 0.571 |
| Reoperation (%) | 35(3.65%) | 14(4.59%) | 0.457 | 44(4.02%) | 5(2.92%) | 0.489 |
| Death, (%) | 4(0.42%) | 3(0.98%) | 0.369 | 4(0.37%) | 3(1.75%) | 0.056 |
| Characteristics | Crude OR of Mortality | Crude OR of ICU Admission | Crude OR of Need for Surgery | ||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Age | 1.245 | 0.943–1.644 | 0.121 | 1.000 | 0.971–1.029 | 0.987 | 1.022 | 1.001–1.044 | 0.040 |
| Male | 0.967 | 0.187–5.008 | 0.968 | 1.082 | 0.756–1.550 | 0.666 | 0.928 | 0.711–1.211 | 0.584 |
| Underlying diseases, n (%) | 13.332 | 2.925–60.777 | <0.001 | 1.156 | 0.595–2.246 | 0.669 | 0.765 | 0.464–1.261 | 0.294 |
| Vital sign | |||||||||
| SBP | 0.985 | 0.953–1.018 | 0.355 | 0.999 | 0.992–1.006 | 0.716 | 1.003 | 0.998–1.009 | 0.190 |
| DBP | 0.937 | 0.885–0.991 | 0.023 | 0.992 | 0.980–1.003 | 0.153 | 1.002 | 0.993–1.010 | 0.732 |
| RR | 0.850 | 0.617–1.170 | 0.319 | 1.026 | 0.968–1.088 | 0.384 | 1.023 | 0.976–1.073 | 0.338 |
| HR | 1.006 | 0.971–1.043 | 0.726 | 0.998 | 0.989–1.006 | 0.565 | 1.003 | 0.997–1.009 | 0.309 |
| Shock index | 7.991 | 1.033–61.838 | 0.047 | 0.853 | 0.434–1.674 | 0.644 | 0.945 | 0.577–1.545 | 0.820 |
| Shock index > 0.9 | 2.375 | 0.529–10.668 | 0.259 | 0.907 | 0.621–1.324 | 0.612 | 0.887 | 0.674–1.167 | 0.393 |
| Elevated SIPA | 4.867 | 1.080–21.937 | 0.039 | 0.553 | 0.317–0.964 | 0.038 | 0.906 | 0.643–1.276 | 0.571 |
| ISS | 1.135 | 1.084–1.189 | <0.001 | 0.996 | 0.968–1.025 | 0.785 | 0.987 | 0.967–1.006 | 0.180 |
| ISS ≥ 16 | 98.833 | 11.741–831.938 | <0.001 | 0.791 | 0.388–1.615 | 0.520 | 0.719 | 0.448–1.153 | 0.171 |
| RTS | 0.521 | 0.395–0.689 | <0.001 | 1.028 | 0.788–1.341 | 0.840 | 1.173 | 0.980–1.405 | 0.083 |
| NISS | 1.107 | 1.069–1.145 | <0.001 | 1.002 | 0.979–1.024 | 0.896 | 0.993 | 0.977–1.010 | 0.425 |
| TRISS | 0.016 | 0.002–0.106 | <0.001 | 3.741 | 0.303–46.183 | 0.304 | 1.173 | 0.360–3.823 | 0.791 |
| Activation of trauma team | 56.839 | 10.778–299.750 | <0.001 | 1.136 | 0.548–2.355 | 0.732 | 0.548 | 0.322–0.933 | 0.027 |
| LOS days | 1.004 | 0.972–1.037 | 0.803 | 1.035 | 1.021–1.049 | <0.001 | 0.995 | 0.986–1.004 | 0.272 |
| Characteristics | Age ≤ 8 year | 8 ≤ Age < 12 year | 12 ≤ Age < 16 year | 16 ≤ Age < 20 year | p-Value |
|---|---|---|---|---|---|
| N = 236 | N = 165 | N = 237 | N = 627 | ||
| Age (years), mean ± SD | 4.69 ± 2.38 | 10.65 ± 1.11 | 14.74 ± 1.16 | 18.65 ± 1.03 | |
| Male, n (%) | 150(36.4%) | 113(31.5%) | 183(22.9%) | 466(25.7%) | 0.003 |
| Underlying diseases, n (%) | 9(3.8%) | 10(6.1%) | 13(5.5%) | 38(6.1%) | 0.624 |
| Vital sign | |||||
| SBP, mean ± SD | 108.82 ± 19.87 | 120.5 ± 18.30 | 131.50 ± 21.56 | 133.29 ± 22.80 | <0.001 |
| DBP, mean ± SD | 69.36 ± 15.90 | 74.52 ± 11.33 | 75.59 ± 12.35 | 77.69 ± 13.11 | <0.001 |
| RR, mean ± SD | 20.78 ± 3.83 | 18.99 ± 2.05 | 18.73 ± 1.85 | 18.76 ± 2.08 | <0.001 |
| HR, mean ± SD | 109.40 ± 21.23 | 93.45 ± 15.53 | 88.93 ± 16.31 | 89.38 ± 17.91 | <0.001 |
| Injury site | |||||
| Home | 92(39.0%) | 28(17.0%) | 16(6.8%) | 24(3.8%) | <0.001 |
| Street | 64(27.1%) | 51(30.9%) | 129(54.7%) | 516(82.3%) | <0.001 |
| Public site | 26(11.0%) | 25(15.2%) | 41(17.4%) | 23(3.7%) | <0.001 |
| Others | 51(21.6%) | 61(37.0%) | 50(20.8%) | 59(9.4%) | <0.001 |
| ISS, (mean; SD) | 5.34 ± 3.40 | 4.90 ± 2.89 | 6.70 ± 6.71 | 7.31 ± 6.54 | <0.001 |
| ISS ≥ 16, (%) | 12(5.1%) | 5(3.0%) | 16(6.8%) | 45(7.2%) | 0.210 |
| RTS, (mean; SD) | 7.59 ± 0.83 | 7.80 ± 0.20 | 7.70 ± 0.55 | 7.70 ± 0.64 | <0.001 |
| NISS, (mean; SD) | 5.88 ± 3.98 | 5.67 ± 3.39 | 7.72 ± 8.05 | 8.24 ± 7.75 | <0.001 |
| TRISS, (mean; SD) | 0.97 ± 0.15 | 1.00 ± 0.00 | 0.98 ± 0.10 | 0.98 ± 0.09 | <0.001 |
| Shock index | 1.04 ± 0.27 | 0.79 ± 0.17 | 0.69 ± 0.17 | 0.69 ± 0.19 | <0.001 |
| Shock index > 0.9 | 167(70.8%) | 44(26.7%) | 29(12.3%) | 65(10.4%) | <0.001 |
| Elevated SIPA | 53(22.5%) | 24(14.5%) | 29(12.3%) | 65(10.4%) | <0.001 |
| LOS days, (median; IQR) | 3(2–5) | 3(2–5) | 5(3–8) | 6(4–11) | <0.001 |
| ICU admission, (%) | 33(14.0%) | 20(12.1%) | 36(15.3%) | 88(14.0%) | 0.858 |
| ICU readmission, (%) | 0(0.0%) | 0(0.0%) | 0(0.0%) | 2(0.3%) | 0.564 |
| ICU days, (median; IQR) | 4(2–6) | 4(3–5.75) | 4(3–7) | 3(2–6) | 0.303 |
| Need for surgery (%) | 148(62.7%) | 114(69.1%) | 165(69.9%) | 440(70.2%) | 0.200 |
| Reoperation (%) | 13(5.5%) | 6(3.6%) | 10(4.2%) | 20(3.2%) | 0.461 |
| Death, (%) | 0(0.0%) | 0(0.0%) | 3(1.3%) | 4(0.6%) | 0.212 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, Y.-C.; Hsieh, T.-H.; Liu, C.-Y.; Chang, C.-Y.; Hou, Y.-T.; Lin, P.-C.; Chen, Y.-L.; Chien, D.-S.; Yiang, G.-T.; Wu, M.-Y. Analysis of Clinical Outcome and Predictors of Mortality in Pediatric Trauma Population: Evidence from a 10 Year Analysis in a Single Center. Children 2021, 8, 688. https://doi.org/10.3390/children8080688
Yang Y-C, Hsieh T-H, Liu C-Y, Chang C-Y, Hou Y-T, Lin P-C, Chen Y-L, Chien D-S, Yiang G-T, Wu M-Y. Analysis of Clinical Outcome and Predictors of Mortality in Pediatric Trauma Population: Evidence from a 10 Year Analysis in a Single Center. Children. 2021; 8(8):688. https://doi.org/10.3390/children8080688
Chicago/Turabian StyleYang, Ya-Chih, Tsung-Han Hsieh, Chi-Yuan Liu, Chun-Yu Chang, Yueh-Tseng Hou, Po-Chen Lin, Yu-Long Chen, Da-Sen Chien, Giou-Teng Yiang, and Meng-Yu Wu. 2021. "Analysis of Clinical Outcome and Predictors of Mortality in Pediatric Trauma Population: Evidence from a 10 Year Analysis in a Single Center" Children 8, no. 8: 688. https://doi.org/10.3390/children8080688
APA StyleYang, Y.-C., Hsieh, T.-H., Liu, C.-Y., Chang, C.-Y., Hou, Y.-T., Lin, P.-C., Chen, Y.-L., Chien, D.-S., Yiang, G.-T., & Wu, M.-Y. (2021). Analysis of Clinical Outcome and Predictors of Mortality in Pediatric Trauma Population: Evidence from a 10 Year Analysis in a Single Center. Children, 8(8), 688. https://doi.org/10.3390/children8080688







