Utility of Laparoscopic Approach of Orchiopexy for Palpable Cryptorchidism: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
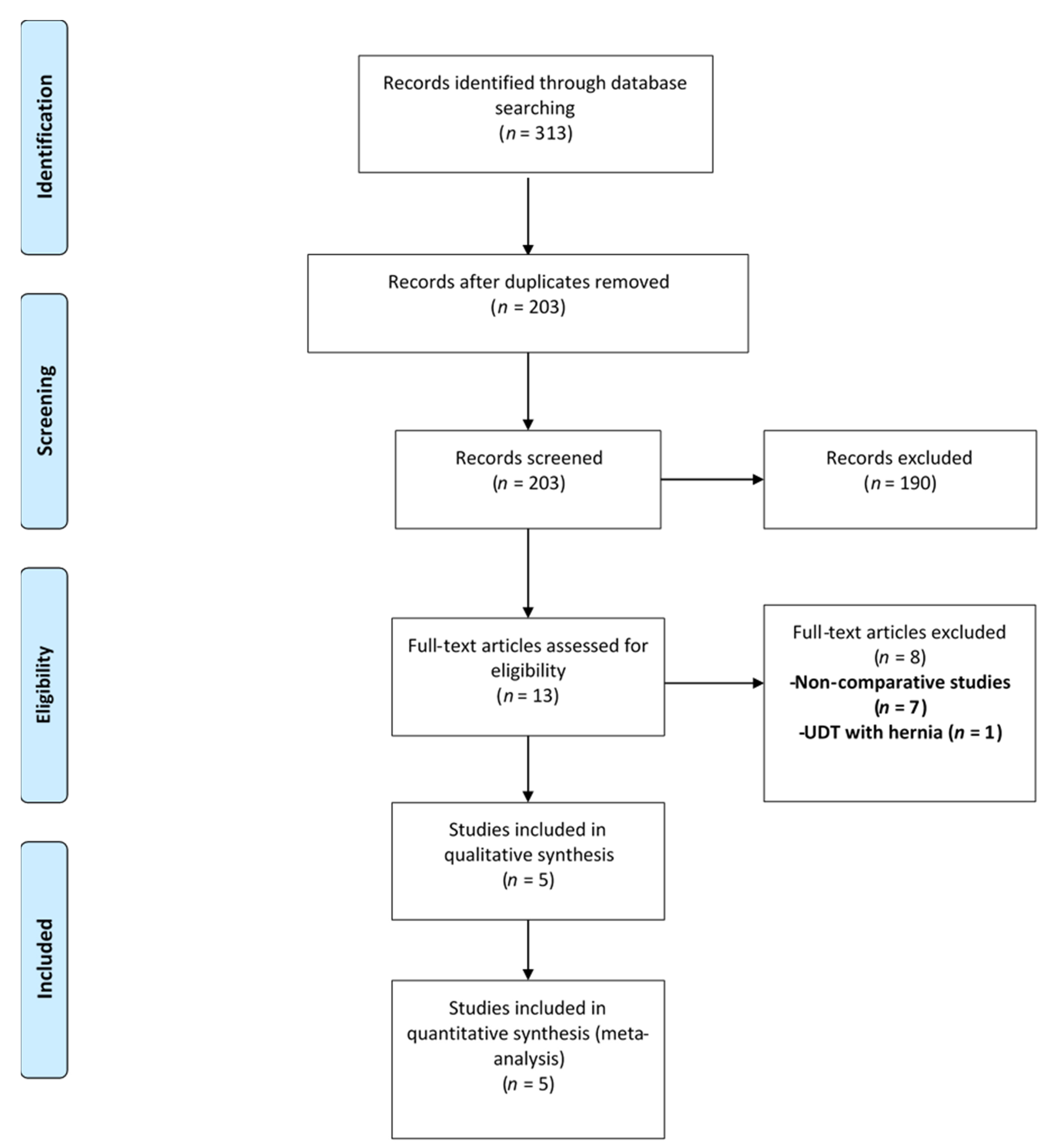
2. Materials and Methods
2.1. Data Source and Search Strategy
2.2. Eligibility Criteria
2.3. Data Synthesis
2.4. Quality Assessment
2.5. Statistical Analysis
3. Results
3.1. Study Characteristics
3.2. Summary of the Included Studies
3.2.1. Escarcega-Fujigaki et al., 2011
3.2.2. Elderwy et al., 2014
3.2.3. Saka et al., 2020
3.2.4. Yang et al., 2020
3.2.5. Gu et al., 2021
3.3. Methodological Quality Assessment
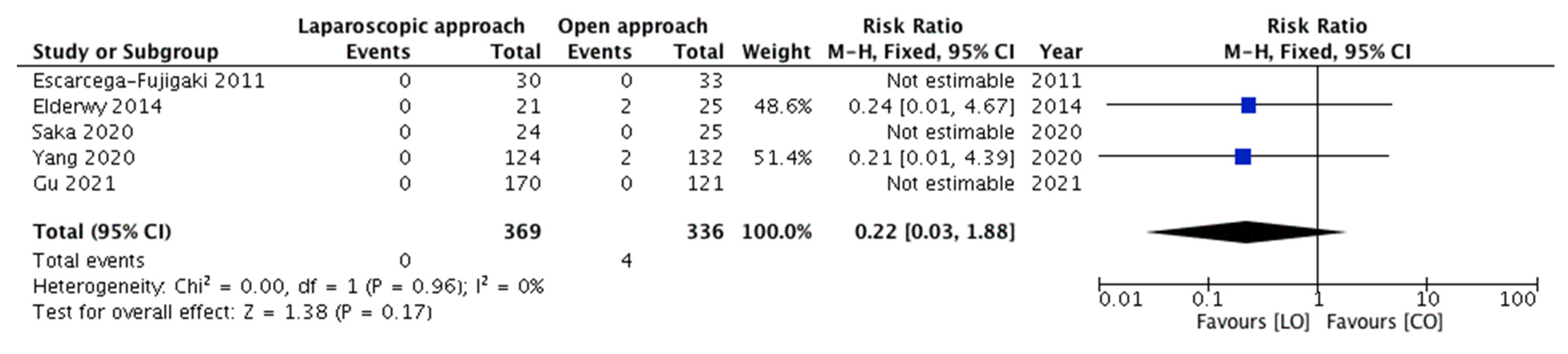
3.3.1. Meta-Analysis of Outcomes—Recurrence of Cryptorchidism and Need for Redo-Orchiopexy
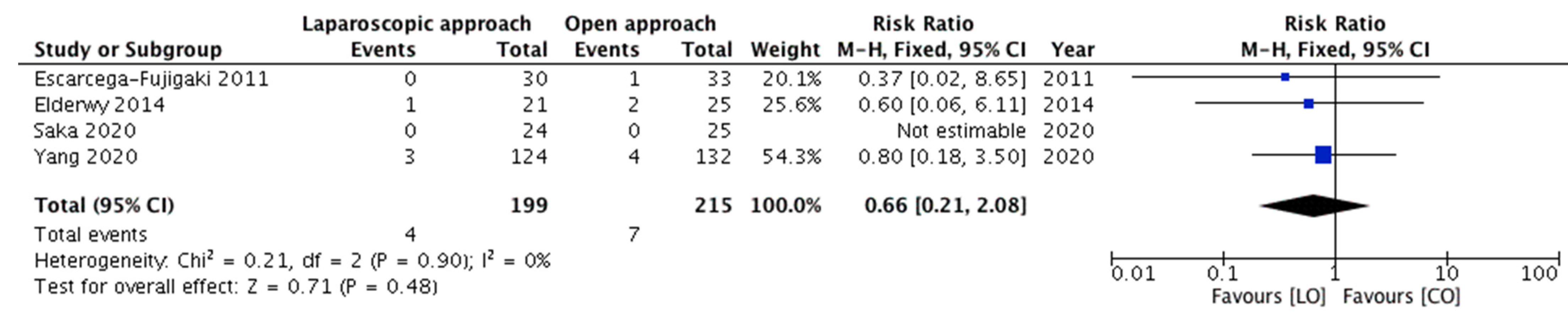
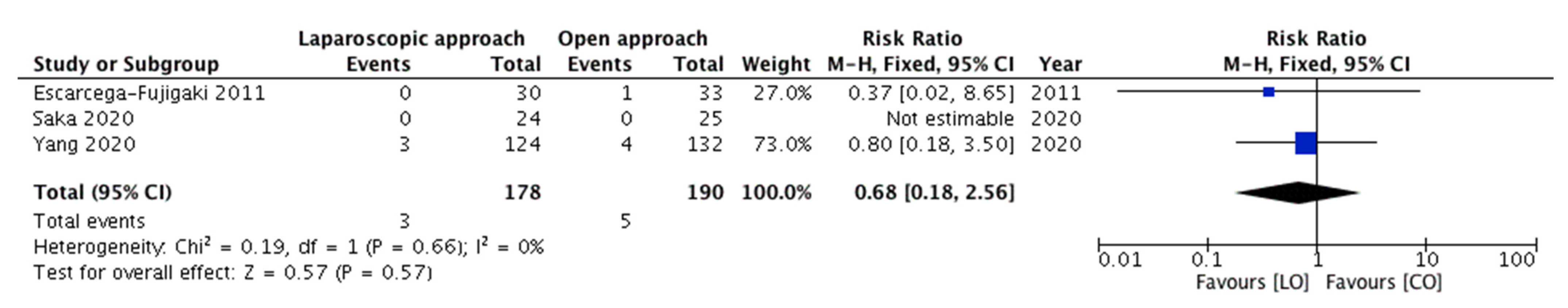
3.3.2. Meta-Analysis of Outcomes—Incidence of Early Postoperative Complications
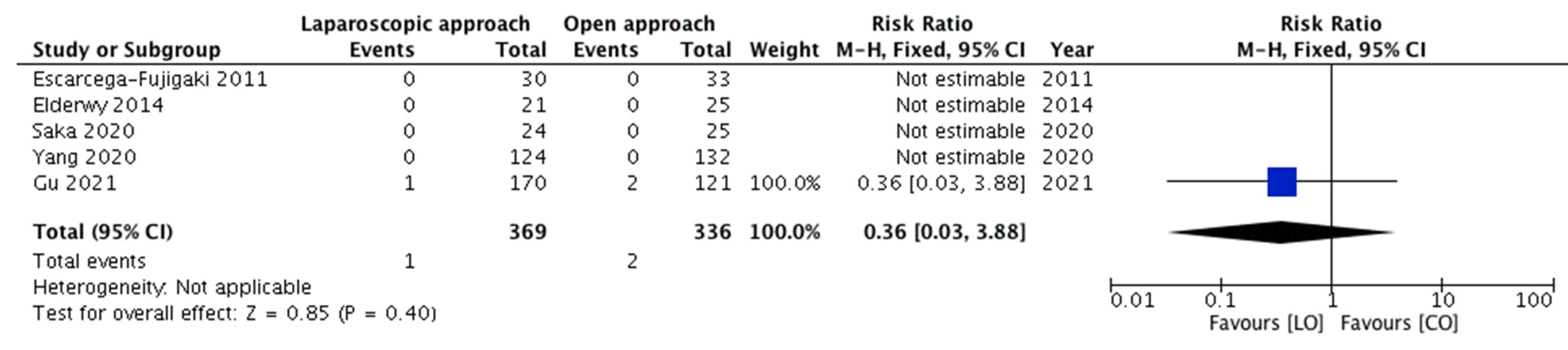
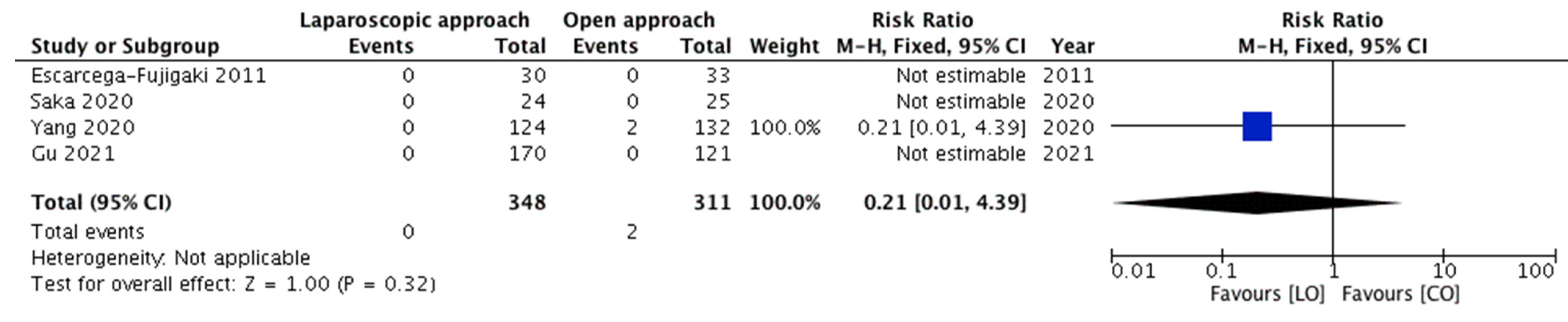
3.3.3. Meta-Analysis of Outcomes—Incidence of Testicular Atrophy (Late Complication)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Database | Studies |
| PubMed | 169 |
| EMBASE | 13 |
| Web of Science | 72 |
| SCOPUS | 59 |
| Total | 313 |
| Duplications | 110 |
| After Duplication Removal | 203 |
References
- Mitsui, T. Effects of the prenatal environment on cryptorchidism: A narrative review. Int. J. Urol. 2021. [Google Scholar] [CrossRef]
- Fawzy, F.; Hussein, A.; Eid, M.M.; El Kashash, A.M.; Salem, H.K. Cryptorchidism and Fertility. Clin. Med. Insights Reprod. Health 2015, 9, 39–43. [Google Scholar] [CrossRef]
- Urry, R.L.; Carrell, D.T.; Starr, N.T.; Snow, B.W.; Middleton, R.G. The incidence of antisperm antibodies in infertility patients with a history of cryptorchidism. J. Urol. 1994, 151, 381–383. [Google Scholar] [CrossRef]
- Hildorf, S.; Clasen-Linde, E.; Cortes, D.; Fossum, M.; Thorup, J. Fertility potential is compromised in 20% to 25% of boys with nonsyndromic cryptorchidism despite orchiopexy within the first year of life. J. Urol. 2020, 203, 832–840. [Google Scholar] [CrossRef]
- Šušnjar, T.; Kuzmić Prusac, I.; Švagelj, I.; Jurišić, A.; Šušnjar, T.; Jurišić, A.; Jukić, M.; Pogorelić, Z. The effect of single and triple testicular biopsy using biopty gun on spermatogenesis in pubertal rats. Animals 2021, 11, 1569. [Google Scholar] [CrossRef]
- Ferguson, L.; Agoulnik, A.I. Testicular cancer and cryptorchidism. Front. Endocrinol. 2013, 4, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pogorelić, Z.; Jurić, I.; Biočić, M.; Furlan, D.; Budimir, D.; Todorić, J.; Milunović, K.P. Management of testicular rupture after blunt trauma in children. Pediatr. Surg. Int. 2011, 27, 885–889. [Google Scholar] [CrossRef] [PubMed]
- Pogorelic, Z.; Neumann, C.; Jukic, M. An unusual presentation of testicular torsion in children: A single—Centre retrospective study. Can. J. Urol. 2019, 26, 10026–10032. [Google Scholar] [PubMed]
- O’Kelly, J.A.; Breen, K.J.; Amoateng, R.; Scanlon, L.; Redmond, E.J.; Kiely, E.A. Assessment of referral patterns for boys with suspected undescended testes and identification of risk factors to aid diagnosis. Surgeon 2021. [Google Scholar] [CrossRef] [PubMed]
- Tseng, C.S.; Chiang, I.N.; Hong, C.H.; Lu, Y.C.; Hong, J.H.; Chang, H.C.; Huang, K.H.; Pu, Y.S. Advantage of early orchiopexy for undescended testis: Analysis of testicular growth percentage ratio in patients with unilateral undescended testicle. Sci. Rep. 2017, 7, 17476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, D.; Lin, T.; Wei, G.; Li, X.; Liu, J.; Hua, Y.; Liu, F. Laparoscopic orchiopexy for treating inguinal canalicular palpable undescended testis. J. Endourol. 2008, 22, 1745–1749. [Google Scholar] [CrossRef] [PubMed]
- Oetzmann von Sochaczewski, C.; Muensterer, O.J. Laparoscopy for abdominal testes: Nationwide analysis of German routine data. J. Laparoendosc. Adv. Surg Tech. A 2021, 31, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Docimo, S.G.; Moore, R.G.; Adams, J.; Kavoussi, L.R. Laparoscopic orchiopexy for the high palpable undescended testis: Preliminary experience. J. Urol. 1995, 154, 1513–1515. [Google Scholar] [CrossRef]
- You, J.; Li, G.; Chen, H.; Wang, J.; Li, S. Laparoscopic orchiopexy of palpable undescended testes experience of a single tertiary institution with over 773 cases. BMC Pediatr. 2020, 20, 124. [Google Scholar] [CrossRef]
- Riquelme, M.; Elizondo, R.A.; Aranda, A. Palpable undescended testes: 15 years of experience and outcome in laparoscopic orchiopexy. J. Endourol. 2015, 29, 978–982. [Google Scholar] [CrossRef] [PubMed]
- Riquelme, M.; Aranda, A.; Rodriguez, C.; Villalvazo, H.; Alvarez, G. Laparoscopic orchiopexy for palpable undescended testes: A five-year experience. J. Laparoendosc. Adv. Surg. Tech. A 2006, 16, 321–324. [Google Scholar] [CrossRef]
- Gu, S.; Wang, Y.; Luo, H. Comparison of laparoscopic orchiopexy and traditional inguinal incision orchiopexy for palpable undescended testes in cryptorchidism. J. Laparoendosc. Adv. Surg. Tech. A 2021, 31, 598–603. [Google Scholar] [CrossRef]
- Elderwy, A.A.; Kurkar, A.; Abdel-Kader, M.S.; Abolyosr, A.; Al-Hazmi, H.; Neel, K.F.; Hammouda, H.M.; Elanany, F.G. Laparoscopic versus open orchiopexy in the management of peeping testis: A multi-institutional prospective randomized study. J. Pediatr. Urol. 2014, 10, 605–609. [Google Scholar] [CrossRef]
- Escarcega-Fujigaki, P.; Rezk, G.H.; Huerta-Murrieta, E.; Lezama-Ramirez, N.; Hernandez-Gomez, S.; Kuri-Cortes, G.; Bañuelos-Montano, A. Orchiopexy-laparoscopy or traditional surgical technique in patients with an undescended palpable testicle. J. Laparoendosc. Adv. Surg. Tech. A 2011, 21, 185–187. [Google Scholar] [CrossRef] [PubMed]
- Saka, R.; Tazuke, Y.; Ueno, T.; Watanabe, M.; Nomura, M.; Masahata, K.; Deguchi, K.; Okuyama, H. Laparoscopy-assisted transscrotal orchidopexy for palpable undescended testis: Initial results. J. Laparoendosc. Adv. Surg. Tech. A 2020, 30, 1131–1136. [Google Scholar] [CrossRef] [PubMed]
- Yang, Z.; Li, S.; Zeng, H.; Yin, J.; Xu, W.; Li, J.; Xie, J.; Liu, C. Laparoscopic orchiopexy versus open orchiopexy for palpable undescended testis in children: A prospective comparison study. J. Laparoendosc. Adv. Surg. Tech. A 2020, 30, 453–457. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [Green Version]
- Downs, S.H.; Black, N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J. Epidemiol. Commu. Health 1998, 52, 377–384. [Google Scholar] [CrossRef] [Green Version]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [Green Version]
- Cochrane Handbook for Systematic Reviews of Interventions (Version 6.2). Cochrane. 2021. Available online: www.training.cochrane.org/handbook (accessed on 27 June 2021).
- Batra, N.V.; DeMarco, R.T.; Bayne, C.E. A narrative review of the history and evidence-base for the timing of orchidopexy for cryptorchidism. J. Pediatr. Urol. 2021, 17, 239–245. [Google Scholar] [CrossRef]
- Zhang, K.; Zhang, Y.; Chao, M. Effect of adjunctive hormonal therapy on testicular descent and spermatogenic function among children with cryptorchidism: A systematic review and meta-analysis. Hormones 2021, 20, 119–129. [Google Scholar] [CrossRef]
- Shehata, S.; Shalaby, R.; Ismail, M.; Abouheba, M.; Elrouby, A. Staged laparoscopic traction-orchiopexy for intraabdominal testis (Shehata technique): Stretching the limits for preservation of testicular vasculature. J. Pediatr. Surg. 2016, 51, 211–215. [Google Scholar] [CrossRef]
- Wang, C.Y.; Wang, Y.; Chen, X.H.; Wei, X.Y.; Chen, F.; Zhong, M. Efficacy of single-stage and two-stage Fowler-Stephens laparoscopic orchidopexy in the treatment of intraabdominal high testis. Asian J. Surg. 2017, 40, 490–494. [Google Scholar] [CrossRef] [PubMed]
- Dawood, W.; Youssif, M.; Badawy, H.; Ghozlan, A.; Orabi, S.; Fahmy, A. Laparoscopic staged management of high intrabdominal testis: A prospective randomized study. J. Pediatr. Surg. 2021. [Google Scholar] [CrossRef]
- Nevešćanin, A.; Vickov, J.; Elezović Baloević, S.; Pogorelić, Z. Laryngeal mask airway versus tracheal intubation for laparoscopic hernia repair in children: Analysis of respiratory complications. J. Laparoendosc. Adv. Surg. Tech. A 2020, 30, 76–80. [Google Scholar] [CrossRef] [PubMed]
- Biliškov, A.N.; Ivančev, B.; Pogorelić, Z. Effects on Recovery of pediatric patients undergoing total intravenous anesthesia with propofol versus ketofol for short—Lasting laparoscopic procedures. Children 2021, 8, 610. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, L.; Cui, X.; Zhou, C.; Zhou, Q.; Zhang, Z. Clinical effect of minimally invasive surgery for inguinal cryptorchidism. BMC Surg. 2021, 21, 21. [Google Scholar]
- Mentessidou, A.; Gargano, T.; Lima, M.; Mirilas, P. Laparoscopic versus open orchiopexy for palpable undescended testes: Systematic review and meta-analysis. J. Ped. Urol. 2021. [Google Scholar] [CrossRef]
- Bramer, W.M.; Rethlefsen, M.L.; Kleijnen, J.; Franco, O.H. Optimal database combinations for literature searches in systematic reviews: A prospective exploratory study. Syst. Rev. 2017, 6, 245. [Google Scholar] [CrossRef]

| Author, Year | Study Design | Sample Size | Mean (SD)/Median (IQR) Age; in Years | Unilateral Cases (%) | Follow-Up Period | |||
|---|---|---|---|---|---|---|---|---|
| LO | CO | LO | CO | LO | CO | |||
| Escarcega-Fujigaki et al., 2011 [19] | Pro | 30 | 33 | Median = 2.3 * | Overall 81% (51/63) were unilateral * | All had follow-up of >6 months § | ||
| Elderwy et al., 2014 [18] | RCT | 21 | 25 | 2 (1.5, 4) | 2.5 (1.5, 4) | All unilateral † | 1–5.5 years (range) | |
| Saka et al., 2020 [20] | Retro | 24 | 25 | 2.5 (0.8–10.3) # | 2.7 (0.8–11.7) # | 63% | 80% | Median follow-up = 1.5 and 1.8 years in both groups |
| Yang et al., 2020 [21] | Pro | 124 | 132 | 2.3 (0.7–11) # | 2.5 (0.8–10) # | 87% | 83% | Mean follow-up of 1 year |
| Gu et al., 2021 [17] | Retro | 170 | 121 | 16.6 (8.4) | 18.4 (15.4) | All unilateral | 0.5–1 years (range) | |
| Author, Year | Mean (SD)/Median (IQR) Operative Duration; Minutes | Cost of Surgery | |
|---|---|---|---|
| LO | CO | ||
| Escarcega-Fujigaki et al., 2011 [19] | 45 # | 38 # | 15% higher cost in LO |
| Elderwy et al., 2014 [18] | 40 (40, 45) | 40 (35, 45) | 25% higher cost in LO |
| Saka et al., 2020 [20] | U/L = 104 (51−143) B/L = 105 (78−130) | U/L = 95 (62−133) B/L = 114 (89−136) | - |
| Yang et al., 2020 [21] | 62.5 (15.2) | 59.0 (13.3) | 19% higher cost in LO |
| Gu et al., 2021 [17] | Age-wise operative durations were compared among the two groups * | - | |
| Methodological Assessment by Author 1 | ||||||
|---|---|---|---|---|---|---|
| Study | Reporting | External Validity | Internal Validity-Bias | Internal Validity-Confounding | Power | Total Scores |
| Escarcega-Fujigaki et al., 2011 [19] | 7 | 3 | 4 | 3 | 0 | 17 |
| Elderwy et al., 2014 [18] | 9 | 1 | 5 | 5 | 0 | 20 |
| Saka et al., 2020 [20] | 9 | 3 | 5 | 3 | 0 | 20 |
| Yang et al., 2020 [21] | 9 | 3 | 5 | 3 | 0 | 20 |
| Gu et al., 2021 [17] | 9 | 3 | 5 | 3 | 0 | 20 |
| Methodological Assessment by Author 2 | ||||||
| Study | Reporting | External Validity | Internal Validity-Bias | Internal Validity-Confounding | Power | Total Scores |
| Escarcega-Fujigaki et al., 2011 [19] | 7 | 3 | 6 | 3 | 0 | 19 |
| Elderwy et al., 2014 [18] | 9 | 0 | 5 | 5 | 0 | 19 |
| Saka et al., 2020 [20] | 9 | 3 | 5 | 3 | 0 | 20 |
| Yang et al., 2020 [21] | 9 | 3 | 5 | 3 | 0 | 20 |
| Gu et al., 2021 [17] | 9 | 3 | 5 | 4 | 0 | 21 |
| Total Scores and Inter-Observer Agreement | ||||||
| Study | Rater 1 | Rater 2 | Mean | Kappa Value | p-Value | |
| Escarcega-Fujigaki et al., 2011 [19] | 17 | 19 | 18 | 0.926 | <0.0001 | |
| Elderwy et al., 2014 [18] | 20 | 19 | 19.5 | |||
| Saka et al., 2020 [20] | 20 | 20 | 20 | |||
| Yang et al., 2020 [21] | 20 | 20 | 20 | |||
| Gu et al., 2021 [17] | 20 | 21 | 20.5 | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Anand, S.; Krishnan, N.; Pogorelić, Z. Utility of Laparoscopic Approach of Orchiopexy for Palpable Cryptorchidism: A Systematic Review and Meta-Analysis. Children 2021, 8, 677. https://doi.org/10.3390/children8080677
Anand S, Krishnan N, Pogorelić Z. Utility of Laparoscopic Approach of Orchiopexy for Palpable Cryptorchidism: A Systematic Review and Meta-Analysis. Children. 2021; 8(8):677. https://doi.org/10.3390/children8080677
Chicago/Turabian StyleAnand, Sachit, Nellai Krishnan, and Zenon Pogorelić. 2021. "Utility of Laparoscopic Approach of Orchiopexy for Palpable Cryptorchidism: A Systematic Review and Meta-Analysis" Children 8, no. 8: 677. https://doi.org/10.3390/children8080677
APA StyleAnand, S., Krishnan, N., & Pogorelić, Z. (2021). Utility of Laparoscopic Approach of Orchiopexy for Palpable Cryptorchidism: A Systematic Review and Meta-Analysis. Children, 8(8), 677. https://doi.org/10.3390/children8080677








