The Impact of Sex on Arterial Ischemic Stroke in Young Patients: From Stroke Occurrence to Poststroke Consequences
Abstract
1. Introduction
2. Methods
3. Sex Distribution in Different Populations of Young Patients with AIS
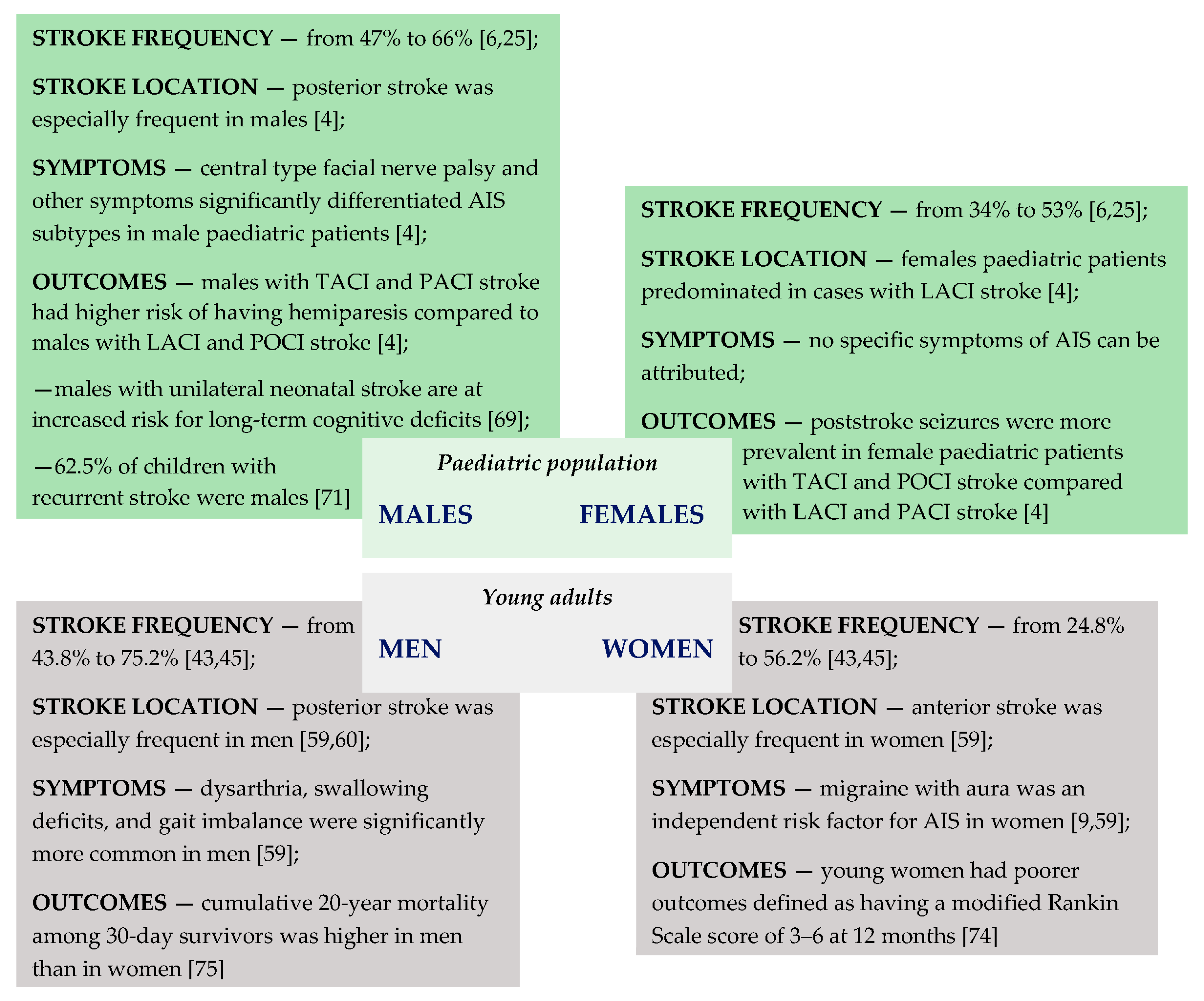
3.1. Paediatric Population
3.2. Young Adults
4. Clinical Presentation of AIS According to Patients’ Sex
4.1. Symptoms of AIS in Paediatric Population
4.2. Symptoms of AIS in Young Adults
5. Poststroke Outcome According to Sex
5.1. Poststroke Outcome in Paediatric Population
5.2. Poststroke Outcome in Young Adults
6. The Role of Hormones in AIS
7. Genetic Risk Factors for AIS According to Sex
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Sarecka-Hujar, B.; Kopyta, I. Poststroke epilepsy: Current perspectives on diagnosis and treatment. Neuropsychiatr. Dis. Treat. 2018, 15, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Numis, A.L.; Fox, C.K. Arterial Ischemic Stroke in Children: Risk Factors and Etiologies. Curr. Neurol. Neurosci. Rep. 2014, 14, 1–9. [Google Scholar] [CrossRef] [PubMed]
- George, M.G. Risk Factors for Ischemic Stroke in Younger Adults. Stroke 2020, 51, 729–735. [Google Scholar] [CrossRef] [PubMed]
- Kopyta, I.; Dobrucka-Głowacka, A.; Cebula, A.; Sarecka-Hujar, B. Does the Occurrence of Particular Symptoms and Outcomes of Arterial Ischemic Stroke Depend on Sex in Pediatric Patients? A Pilot Study. Brain Sci. 2020, 10, 881. [Google Scholar] [CrossRef] [PubMed]
- Sultan, S.; Schupf, N.; Dowling, M.; DeVeber, G.; Kirton, A.; Elkind, M.S. Predictors of Cholesterol and Lipoprotein(a) Testing in Children with Arterial Ischemic Stroke. J. Stroke Cerebrovasc. Dis. 2014, 23, 2405–2413. [Google Scholar] [CrossRef]
- Herak, D.C.; Krleza, J.L.; Antolic, M.R.; Horvat, I.; Djuranovic, V.; Topic, R.Z.; Zadro, R. Association of Polymorphisms in Coagulation Factor Genes and Enzymes of Homocysteine Metabolism with Arterial Ischemic Stroke in Children. Clin. Appl. Thromb. 2017, 23, 1042–1051. [Google Scholar] [CrossRef]
- Lopez-Espejo, M.; Hernandez-Chavez, M.; Huete, I. Risk factors for in-hospital and follow-up mortality after childhood arterial ischemic stroke. J. Neurol. 2019, 266, 1526–1532. [Google Scholar] [CrossRef]
- Roy-O’Reilley, R.; McCullough, L.D. Age and Sex Are Critical Factors in Ischemic Stroke Pathology. Endocrinology 2018, 159, 3120–3131. [Google Scholar] [CrossRef]
- Abanoz, Y.; Abanoz, Y.G.; Gündüz, A.; Uludüz, D.; Ince, B.; Yavuz, B.; Göksan, B. Migraine as a risk factor for young patients with ischemic stroke: A case–control study. Neurol. Sci. 2017, 38, 611–617. [Google Scholar] [CrossRef]
- Felling, R.J.; Sun, L.R.; Maxwell, E.C.; Goldenberg, N.; Bernard, T. Pediatric arterial ischemic stroke: Epidemiology, risk factors, and management. Blood Cells Mol. Dis. 2017, 67, 23–33. [Google Scholar] [CrossRef] [PubMed]
- Golomb, M.R.; Fullerton, H.J.; Nowak-Gottl, U.; DeVeber, G. Male Predominance in Childhood Ischemic Stroke. Stroke 2009, 40, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Fullerton, H.J.; Wu, Y.W.; Zhao, S.; Johnston, S.C. Risk of stroke in children: Ethnic and gender disparities. Neurology 2003, 61, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Agrawal, N.; Johnston, S.C.; Wu, Y.W.; Sidney, S.; Fullerton, H.J. Imaging Data Reveal a Higher Pediatric Stroke Inci-dence Than Prior US Estimates. Stroke 2009, 40, 3415–3421. [Google Scholar] [CrossRef] [PubMed]
- Mallick, A.A.; Ganesan, V.; Kirkham, F.J.; Fallon, P.; Hedderly, T.; McShane, T.; Parker, A.P.; Wassmer, E.; Wraige, E.; Amin, S.; et al. Childhood arterial ischaemic stroke incidence, presenting features, and risk factors: A prospective pop-ulation-based study. Lancet Neurol. 2014, 13, 35–43. [Google Scholar] [CrossRef]
- National Center for Injury Prevention and Control, CDC. 10 Leading Causes of Death by Age-Group. 2018. Available online: https://www.cdc.gov/injury/wisqars/pdf/leading_causes_of_death_by_age_group_2018-508.pdf (accessed on 2 February 2021).
- Krishnamurthi, R.V.; DeVeber, G.; Feigin, V.L.; Barker-Collo, S.; Fullerton, H.J.; Mackay, M.T.; O’Callahan, F.; Lindsay, M.P.; Kolk, A.; Lo, W.; et al. Stroke Prevalence, Mortality and Disability-Adjusted Life Years in Children and Youth Aged 0-19 Years: Data from the Global and Regional Burden of Stroke 2013. Neuroepidemiology 2015, 45, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Deveber, G.A.; Kirton, A.; Booth, F.A.; Yager, J.Y.; Wirrell, E.C.; Wood, E.; Shevell, M.; Surmava, A.-M.; McCusker, P.; Massicotte, M.P.; et al. Epidemiology and Outcomes of Arterial Ischemic Stroke in Children: The Canadian Pediatric Ischemic Stroke Registry. Pediatr. Neurol. 2017, 69, 58–70. [Google Scholar] [CrossRef] [PubMed]
- State of New Jersey, Department of Labor & Workforce Development. Population Estimates by Single-Year of Age and Sex: April 2010 to July 1, 2019. Available online: https://www.nj.gov/labor/lpa/dmograph/est/est_index.html (accessed on 6 February 2021).
- Naeye, R.L.; Burt, L.S.; Wright, D.L.; A Blanc, W.; Tatter, D. Neonatal mortality, the male disadvantage. Pediatry 1971, 48, 902–906. [Google Scholar]
- Aubenque, M. Indice de masculinite a la naissance: Apercu retrospectif et commentaires [The sex ratio at birth: A ret-rospective review and commentary]. J. Soc. Stat. Paris. 1989, 130, 80–102. (In French) [Google Scholar]
- Bohmer, M.; Niederstadt, T.; Heindel, W.; Wildgruber, M.; Sträter, R.; Hanning, U.; Kemmling, A.; Sporns, P.B. Impact of arterial ischemic stroke standardized classification and diagnostic evaluation classification on further course of ar-teriopathy and recurrence of childhood stroke. Stroke 2019, 50, 83–87. [Google Scholar] [CrossRef]
- Steinlin, M.; Bigi, S.; Stojanovski, B.; Gajera, J.; Regényi, M.; El-Koussy, M.; Mackay, M.T. Swiss NeuroPediatric Stroke Registry. Focal Cerebral Arteriopathy: Do Steroids Improve Outcome? Stroke 2017, 48, 2375–2382. [Google Scholar] [CrossRef]
- Per, H.; Unal, E.; Poyrazoğlu, H.G.; Ozdemir, M.A.; Donmez, H.; Gümüş, H.; Üzüm, K.; Canpolat, M.; Akyildiz, B.N.; Coşkun, A.; et al. Childhood Stroke: Results of 130 Children from a Reference Center in Central Anatolia, Turkey. Pediatr. Neurol. 2014, 50, 595–600. [Google Scholar] [CrossRef]
- Rambaud, T.; Legris, N.; Bejot, Y.; Bellesme, C.; Lapergue, B.; Jouvent, E.; Pico, F.; Smadja, D.; Zuber, M.; Crozier, S.; et al. Acute ischemic stroke in adolescents. Neurol. 2020, 94, e158–e169. [Google Scholar] [CrossRef]
- Nowak-Göttl, U.; Sträter, R.; Kosch, A.; Von Eckardstein, A.; Schobess, R.; Luigs, P.; Nabel, P.; Vielhaber, H.; Kurnik, K.; Junker, R.; et al. The plasminogen activator inhibitor (PAI)-1 promoter 4G/4G genotype is not associated with ischemic stroke in a population of German children. Eur. J. Haematol. 2001, 66, 57–62. [Google Scholar] [CrossRef]
- Masri, A.; Al-Ammouri, I. Clinical presentation, etiology, and outcome of stroke in children: A hospital-based study. Brain Dev. 2016, 38, 204–208. [Google Scholar] [CrossRef]
- Gelfand, A.A.; Croen, L.A.; Torres, A.R.; Wu, Y.W. Genetic Risk Factors for Perinatal Arterial Ischemic Stroke. Pediatr. Neurol. 2013, 48, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Golomb, M.R.; Dick, P.T.; MacGregor, D.L.; Curtis, R.; Sofronas, M.; DeVeber, G.A. Neonatal arterial ischemic stroke and cerebral sinovenous thrombosis are more commonly diagnosed in boys. J. Child Neurol. 2004, 19, 493–497. [Google Scholar] [CrossRef]
- Salih, M.A.; Abdel-Gader, A.G.; Al-Jarallah, A.A.; Kentab, A.Y.; Alorainy, I.A.; Hassan, H.H.; Al-Nasser, M.N. Perinatal stroke in Saudi children. Clinical features and risk factors. Saudi Med. J. 2006, 27, S35–S40. [Google Scholar] [PubMed]
- Sträter, R.; Becker, S.; von Eckardstein, A.; Heinecke, A.; Gutsche, S.; Junker, R.; Kurnik, K.; Schobess, R.; Nowak-Göttl, U. Prospective assessment of risk factors for recurrent stroke during childhood—A 5-year follow-up study. Lancet 2002, 360, 1540–1545. [Google Scholar] [CrossRef]
- Sebire, G.; Tabarki, B.; Saunders, D.E.; Leroy, I.; Liesner, R.; Saint-Martin, C.; Husson, B.; Williams, A.N.; Wade, A.; Kirkham, F.J. Cerebral venous sinus thrombosis in children: Risk factors, presentation, diagnosis and outcome. Brain 2005, 128, 477–489. [Google Scholar] [CrossRef] [PubMed]
- Kenet, G.; Sadetzki, S.; Murad, H.; Martinowitz, U.; Rosenberg, N.; Gitel, S.; Rechavi, G.; Inbal, A. Factor V Leiden and Antiphospholipid Antibodies Are Significant Risk Factors for Ischemic Stroke in Children. Stroke 2000, 31, 1283–1288. [Google Scholar] [CrossRef] [PubMed]
- Kenet, G.; Kirkham, F.; Niederstadt, T.; Heinecke, A.; Saunders, D.; Stoll, M.; Brenner, B.; Bidlingmaier, C.; Heller, C.; Knöfler, R.; et al. Risk factors for recurrent venous thromboembolism in the European collaborative paediatric database on cerebral venous thrombosis: A multicentre cohort study. Lancet Neurol. 2007, 6, 595–603. [Google Scholar] [CrossRef]
- Bonduel, M.; Sciuccati, G.; Hepner, M.; Pieroni, G.; Torres, A.F.; Frontroth, J.P.; Tenembaum, S. Arterial Ischemic Stroke and Cerebral Venous Thrombosis in Children: A 12-Year Argentinean Registry. Acta Haematol. 2006, 115, 180–185. [Google Scholar] [CrossRef] [PubMed]
- Ozyurek, E.; Balta, G.; Degerliyurt, A.; Parlak, H.; Aysun, S.; Gürgey, A. Significance of Factor V, Prothrombin, MTHFR, and PAI-1 Genotypes in Childhood Cerebral Thrombosis. Clin. Appl. Thromb. 2007, 13, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Hills, N.K.; Johnston, S.C.; Sidney, S.; Zielinski, B.A.; Fullerton, H.J. Recent trauma and acute infection as risk factors for childhood arterial ischemic stroke. Ann. Neurol. 2012, 72, 850–858. [Google Scholar] [CrossRef] [PubMed]
- Helmuth, I.G.; Mølbak, K.; Uldall, P.V.; Poulsen, A. Post-varicella Arterial Ischemic Stroke in Denmark 2010 to 2016. Pediatr. Neurol. 2018, 80, 42–50. [Google Scholar] [CrossRef]
- Fullerton, H.J.; Luna, J.M.; Wintermark, M.; Hills, N.K.; Tokarz, R.; Li, Y.; Glaser, C.; DeVeber, G.A.; Lipkin, W.I.; Elkind, M.S.V. Parvovirus B19 Infection in Children with Arterial Ischemic Stroke. Stroke 2017, 48, 2875–2877. [Google Scholar] [CrossRef] [PubMed]
- Amlie-Lefond, C.; Bernard, T.J.; Sébire, G.; Friedman, N.R.; Heyer, G.L.; Lerner, N.B.; de Veber, G.; Fullerton, H.J. Pre-dictors of Cerebral Arteriopathy in Children with Arterial Ischemic Stroke: Results of the International Pediatric Stroke Study. Circulation 2009, 119, 1417–1423. [Google Scholar] [CrossRef] [PubMed]
- Szaflarski, J.; Allendorfer, J.; Byars, A.; Vannest, J.; Dietz, A.; Hernando, K.; Holland, S. Age at stroke determines post-stroke language lateralization. Restor. Neurol. Neurosci. 2014, 32, 733–742. [Google Scholar] [CrossRef]
- Kissela, B.M.; Khoury, J.C.; Alwell, K.; Moomaw, C.J.; Woo, D.; Adeoye, O.; Flaherty, M.L.; Khatri, P.; Ferioli, S.; Rosa, F.D.L.R.L.; et al. Age at stroke: Temporal trends in stroke incidence in a large, biracial population. Neurology 2012, 79, 1781–1787. [Google Scholar] [CrossRef]
- Bergman, E.-M.; Henriksson, K.M.; Åsberg, S.; Farahmand, B.; Terént, A. National registry-based case-control study: Comorbidity and stroke in young adults. Acta Neurol. Scand. 2015, 131, 394–399. [Google Scholar] [CrossRef]
- Martínez-Sánchez, P.; Fuentes, B.; Fernández-Domínguez, J.; Ortega-Casarrubios, M.D.L. Ángeles; Aguilar-Amar, M.J.; Abenza-Abildúa, M.J.; Idrovo-Freire, L.; Diez-Tejedor, E.; Gimeno, B.E.F. Young Women Have Poorer Outcomes than Men after Stroke. Cerebrovasc. Dis. 2011, 31, 455–463. [Google Scholar] [CrossRef]
- Spengos, K.; Vemmos, K. Risk factors, etiology, and outcome of first-ever ischemic stroke in young adults aged 15 to 45—The Athens young stroke registry. Eur. J. Neurol. 2010, 17, 1358–1364. [Google Scholar] [CrossRef]
- Kwon, S.U.; Kim, J.S.; Lee, J.H.; Lee, M.C. Ischemic stroke in Korean young adults. Acta Neurol. Scand. 2000, 101, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Tang, M.; Yao, M.; Zhu, Y.; Peng, B.; Zhou, L.; Ni, J. Sex differences of ischemic stroke in young adults—A single-center Chinese cohort study. J. Stroke Cerebrovasc. Dis. 2020, 29, 105087. [Google Scholar] [CrossRef]
- Aigner, A.; Grittner, U.; Rolfs, A.; Norrving, B.; Siegerink, B.; Busch, M.A. Contribution of Established Stroke Risk Factors to the Burden of Stroke in Young Adults. Stroke 2017, 48, 1744–1751. [Google Scholar] [CrossRef] [PubMed]
- Putaala, J.; Metso, A.J.; Metso, T.M.; Konkola, N.; Kraemer, Y.; Haapaniemi, E.; Kaste, M.; Tatlisumak, T. Analysis of 1008 Consecutive Patients Aged 15 to 49 With First-Ever Ischemic Stroke. Stroke 2009, 40, 1195–1203. [Google Scholar] [CrossRef]
- Arntz, R.M.; Broek, S.M.V.D.; Van Uden, I.W.; Ghafoorian, M.; Platel, B.; Rutten-Jacobs, L.C.; Maaijwee, N.A.; Schaapsmeerders, P.; Schoonderwaldt, H.C.; Van Dijk, E.J.; et al. Accelerated development of cerebral small vessel disease in young stroke patients. Neurology 2016, 87, 1212–1219. [Google Scholar] [CrossRef] [PubMed]
- Ekker, M.S.; Verhoeven, J.I.; Vaartjes, I.; Jolink, W.M.T.; Klijn, C.J.M.; De Leeuw, F.-E. Association of Stroke Among Adults Aged 18 to 49 Years with Long-term Mortality. JAMA 2019, 321, 2113–2123. [Google Scholar] [CrossRef]
- Leppert, M.H.; Ho, P.M.; Burke, J.; Madsen, T.E.; Kleindorfer, D.; Sillau, S.; Daugherty, S.; Bradley, C.J.; Poisson, S.N. Young Women Had More Strokes Than Young Men in a Large, United States Claims Sample. Stroke 2020, 51, 3352–3355. [Google Scholar] [CrossRef]
- Onwuchekwa, A.; Asekomeh, E.; Onwuchekwa, R. Stroke in young Nigerian adults. J. Vasc. Nurs. 2009, 27, 98–102. [Google Scholar] [CrossRef]
- Wu, T.Y.; Kumar, A.; Wong, E.H. Young ischaemic stroke in South Auckland: A hospital-based study. New Zealand Med J. 2012, 125, 47–56. [Google Scholar] [PubMed]
- Lasek-Bal, A.; Kopyta, I.; Warsz-Wianecka, A.; Puz, P.; Łabuz-Roszak, B.; Zaręba, K. Risk factor profile in patients with stroke at a young age. Neurol. Res. 2018, 40, 595–601. [Google Scholar] [CrossRef]
- Tuckuviene, R.; Christensen, A.; Helgestad, J.; Johnsen, S.; Kristensen, S. Paediatric arterial ischaemic stroke and cerebral sinovenous thrombosis in Denmark 1994–2006: A nationwide population-based study. Acta Paediatr. 2010, 100, 543–549. [Google Scholar] [CrossRef]
- Carey, S.; Wrogemann, J.; Booth, F.A.; Rafay, M.F. Epidemiology, Clinical Presentation, and Prognosis of Posterior Circulation Ischemic Stroke in Children. Pediatr. Neurol. 2017, 74, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Colsch, R.; Lindseth, G. Unique Stroke Symptoms in Women: A Review. J. Neurosci. Nurs. 2018, 50, 336–342. [Google Scholar] [CrossRef]
- Labiche, L.A.; Chan, W.; Saldin, K.R.; Morgenstern, L.B. Sex and acute stroke presentation. Ann. Emerg. Med. 2002, 40, 453–460. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.; Ibrahim, A. Gender differences in risk factors, clinical presentation, and outcome of stroke: A secondary analysis of previous hospital-based study in Qatar. Libyan J. Med Sci. 2018, 2, 51. [Google Scholar] [CrossRef]
- Von Sarnowski, B.; Schminke, U.; Grittner, U.; Tanislav, C.; Böttcher, T.; Hennerici, M.G.; Tatlisumak, T.; Putaala, J.; Kaps, M.; Fazekas, F.; et al. Posterior versus Anterior Circulation Stroke in Young Adults: A Comparative Study of Stroke Aetiologies and Risk Factors in Stroke among Young Fabry Patients (sifap1). Cerebrovasc. Dis. 2017, 43, 152–160. [Google Scholar] [CrossRef]
- Kuruvilla, A.; Bhattacharya, P.; Rajamani, K.; Chaturvedi, S. Factors Associated With Misdiagnosis of Acute Stroke in Young Adults. J. Stroke Cerebrovasc. Dis. 2011, 20, 523–527. [Google Scholar] [CrossRef]
- Breitweg, I.; Von Stülpnagel, C.; Pieper, T.; Lidzba, K.; Holthausen, H.; Staudt, M.; Kluger, G. Early seizures predict the development of epilepsy in children and adolescents with stroke. Eur. J. Paediatr. Neurol. 2017, 21, 465–467. [Google Scholar] [CrossRef]
- Lee, E.H.; Yum, M.-S.; Ko, T.-S. Risk Factors and Clinical Outcomes of Childhood Ischemic Stroke in a Single Korean Tertiary Care Center. J. Child Neurol. 2011, 27, 485–491. [Google Scholar] [CrossRef]
- Roivainen, R.; Haapaniemi, E.; Putaala, J.; Kaste, M.; Tatlisumak, T. Young adult ischaemic stroke related acute symptomatic and late seizures: Risk factors. Eur. J. Neurol. 2013, 20, 1247–1255. [Google Scholar] [CrossRef]
- Chen, T.-C.; Chen, Y.-Y.; Cheng, P.-Y.; Lai, C.-H. The incidence rate of post-stroke epilepsy: A 5-year follow-up study in Taiwan. Epilepsy Res. 2012, 102, 188–194. [Google Scholar] [CrossRef] [PubMed]
- De Schryver, E.L.; Kappelle, L.J.; Jennekens-Schinkel, A.; Boudewyn Peters, A.C. Prognosis of ischemic stroke in childhood: A long-term follow-up study. Dev. Med. Child. Neurol. 2000, 42, 313–318. [Google Scholar] [CrossRef] [PubMed]
- Morais, N.M.M.; Ranzan, J.; Riesgo, R.S. Predictors of Epilepsy in Children with Cerebrovascular Disease. J. Child Neurol. 2012, 28, 1387–1391. [Google Scholar] [CrossRef] [PubMed]
- Kopyta, I.; Sarecka-Hujar, B.; Skrzypek, M. Post-stroke epilepsy in Polish paediatric patients. Dev. Med. Child Neurol. 2015, 57, 821–828. [Google Scholar] [CrossRef] [PubMed]
- Westmacott, R.; MacGregor, D.; Askalan, R.; DeVeber, G. Late Emergence of Cognitive Deficits After Unilateral Neonatal Stroke. Stroke 2009, 40, 2012–2019. [Google Scholar] [CrossRef] [PubMed]
- Öztürk, Ş.; Ege, F.; Ekmekci, H. Language Disorders due to Posterior System Strokes—An Ignored Dysfunction. Arch. Neuropsychiatry 2014, 51, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Fullerton, H.J.; Wintermark, M.; Hills, N.K.; Dowling, M.M.; Tan, M.; Rafay, M.F.; Elkind, M.S.V.; Barkovich, A.J.; DeVeber, G.A.; Plumb, P.A.; et al. Risk of Recurrent Arterial Ischemic Stroke in Childhood. Stroke 2016, 47, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Uohara, M.Y.; Beslow, L.A.; Billinghurst, L.; Jones, B.M.; Kessler, S.K.; Licht, D.J.; Ichord, R.N. Incidence of Recurrence in Posterior Circulation Childhood Arterial Ischemic Stroke. JAMA Neurol. 2017, 74, 316–323. [Google Scholar] [CrossRef]
- Rafay, M.F.; Shapiro, K.A.; Surmava, A.-M.; DeVeber, G.A.; Kirton, A.; Fullerton, H.J.; Amlie-Lefond, C.; Weschke, B.; Dlamini, N.; Carpenter, J.L.; et al. Spectrum of cerebral arteriopathies in children with arterial ischemic stroke. Neurol. 2020, 94, e2479–e2490. [Google Scholar] [CrossRef]
- Geng, C.; Lin, Y.; Tang, Q.; Tang, Y.; Wang, X.; Zhou, J.-S.; Yang, J.; Zheng, D.; Zhang, Y.-D. Sex differences in clinical characteristics and 1-year outcomes of young ischemic stroke patients in East China. Ther. Clin. Risk Manag. 2018, 15, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Rutten-Jacobs, L.C.A.; Arntz, R.M.; Maaijwee, N.A.M.; Schoonderwaldt, H.C.; Dorresteijn, L.D.; Van Dijk, E.J.; De Leeuw, F.-E. Long-term Mortality After Stroke Among Adults Aged 18 to 50 Years. JAMA 2013, 309, 1136–1144. [Google Scholar] [CrossRef]
- Lutski, M.; Zucker, I.; Shohat, T.; Tanne, D. Characteristics and Outcomes of Young Patients with First-Ever Ischemic Stroke Compared to Older Patients: The National Acute Stroke ISraeli Registry. Front. Neurol. 2017, 8, 421. [Google Scholar] [CrossRef] [PubMed]
- Arntz, R.; Rutten-Jacobs, L.; Maaijwee, N.; Schoonderwaldt, H.; Dorresteijn, L.; Van Dijk, E.; De Leeuw, F.-E. Post-Stroke Epilepsy in Young Adults: A Long-Term Follow-Up Study. PLoS ONE 2013, 8, e55498. [Google Scholar] [CrossRef] [PubMed]
- Naess, H.; Nyland, H.I.; Thomassen, L.; Aarseth, J.; Myhr, K.-M. Long-term outcome of cerebral infarction in young adults. Acta Neurol. Scand. 2004, 110, 107–112. [Google Scholar] [CrossRef] [PubMed]
- Naess, H.; Nyland, H.I.; Thomassen, L.; Aarseth, J.; Myhr, K.-M. Mild depression in young adults with cerebral infarction at long-term follow-up: A population-based study. Eur. J. Neurol. 2005, 12, 194–198. [Google Scholar] [CrossRef] [PubMed]
- Lim, T.S.; Lee, J.S.; Yoon, J.H.; Moon, S.Y.; Joo, I.S.; Huh, K.; Hong, J.M. Cigarette smoking is an independent risk factor for post-stroke delirium. BMC Neurol. 2017, 17, 56. [Google Scholar] [CrossRef]
- Simpkins, J.W.; Rajakumar, G.; Zhang, Y.-Q.; Simpkins, C.E.; Greenwald, D.; Yu, C.J.; Bodor, N.; Day, A.L. Estrogens may reduce mortality and ischemic damage caused by middle cerebral artery occlusion in the female rat. J. Neurosurg. 1997, 87, 724–730. [Google Scholar] [CrossRef] [PubMed]
- Castelló-Ruiz, M.; Torregrosa, G.; Burguete, M.C.; Miranda, F.J.; Centeno, J.M.; López-Morales, M.A.; Gasull, T.; Alborch, E. The selective estrogen receptor modulator, bazedoxifene, reduces ischemic brain damage in male rat. Neurosci. Lett. 2014, 575, 53–57. [Google Scholar] [CrossRef]
- Manwani, B.; McCullough, L.D. Sexual Dimorphism in Ischemic Stroke: Lessons from the Laboratory. Women’s Health 2011, 7, 319–339. [Google Scholar] [CrossRef]
- Ritzel, R.M.; Capozzi, L.A.; McCullough, L.D. Sex, stroke, and inflammation: The potential for estrogen-mediated immunoprotection in stroke. Horm. Behav. 2013, 63, 238–253. [Google Scholar] [CrossRef]
- Liu, F.; McCullough, L.D. Interactions between age, sex, and hormones in experimental ischemic stroke. Neurochem. Int. 2012, 61, 1255–1265. [Google Scholar] [CrossRef]
- Ahnstedt, H.; McCullough, L.D.; Cipolla, M.J. The Importance of Considering Sex Differences in Translational Stroke Research. Transl. Stroke Res. 2016, 7, 261–273. [Google Scholar] [CrossRef]
- Normann, S.; De Veber, G.; Fobker, M.; Langer, C.; Kenet, G.; Bernard, T.J.; Fiedler, B.; Sträter, R.; Goldenberg, N.A.; Nowak-Göttl, U. Role of endogenous testosterone concentration in pediatric stroke. Ann. Neurol. 2009, 66, 754–758. [Google Scholar] [CrossRef]
- Zak, I.; Sarecka-Hujar, B.; Kopyta, I.; Emich-Widera, E.; Marszal, E.; Wendorff, J.; Jachowicz-Jeszka, J. The T Allele of the 677C>T Polymorphism ofMethylenetetrahydrofolate ReductaseGene is Associated with an Increased Risk of Ischemic Stroke in Polish Children. J. Child Neurol. 2009, 24, 1262–1267. [Google Scholar] [CrossRef] [PubMed]
- Coen Herak, D.; Čeri, A.; Grzunov, A.; Krleza, J.L.; Radic Antolic, M.; Horvat, I.; Đuranović, V.; Barisic, N.; Zrinski Topić, R.; Zadro, R. Gender specific effect of the fxiii-a val34leu polymorphism on the risk for childhood and perinatal arterial ischemic stroke. In Proceedings of the 2nd International Factor XIII Workshop, Heviz, Hungary, 28 September–2 October 2016. [Google Scholar]
- Sarecka-Hujar, B.; Zak, I.; Emich-Widera, E.; Kopyta, I.; Pilarska, E.; Pienczk-Reclawowicz, K. Association analysis of the E-selectin 98G > T polymorphism and the risk of childhood ischemic stroke. Cell Biochem. Funct. 2010, 28, 591–596. [Google Scholar] [CrossRef]
- Gromadzka, G.; Baranska-Gieruszczak, M.; Sarzynska-Dlugosz, I.; Ciesielska, A.; Czlonkowska, A. The APOE pol-ymorphism and 1-year outcome in ischemic stroke: Genotype-gender interaction. Acta Neurol. Scand. 2007, 116, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Martiskainen, M.; Oksala, N.; Pohjasvaara, T.; Kaste, M.; Oksala, A.; Karhunen, P.J.; Erkinjuntti, T. Βeta-fibrinogen gene promoter A −455 allele associated with poor longterm survival among 55–71 years old Caucasian women in Finnish stroke cohort. BMC Neurol. 2014, 14, 137. [Google Scholar] [CrossRef] [PubMed]
- Joly, B.; Menard, A.-L.; Ozkul-Wermester, O.; Triquenot-Bagan, A.; Guegan-Massardier, E.; Borg, J.-Y.; Le Cam-Duchez, V. Involvement of Arg306 mutation in factor V gene in two young men with ischemic stroke. Blood Coagul. Fibrinolysis 2014, 25, 916–917. [Google Scholar] [CrossRef] [PubMed]

| Study | Type of the Study | Population | Number of Cases | Age at Time of AIS | Females n (%) | Males n (%) |
|---|---|---|---|---|---|---|
| Kopyta et al. [4] | Retrospective | Patients hospitalized in the Department of Pediatric Neurology of the Medical University of Silesia in Katowice (Poland) | 89 | From 1 month to 18 years old | 37 (42) | 52 (58) |
| Sultan et al. [5] | Cross-sectional analysis | Patients from the International Pediatric Stroke Study (IPSS) registry | 1652 | From 28 days of age to 18 years old | 679 (41.1) | 973 (58.9) |
| Coen Herak et al. [6] | Retrospective | Patients admitted to the Department of Neuropediatrics, Children’s Hospital Zagreb, and the Department of Pediatric Neurology, University Hospital Centre Zagreb (Croatia) | 73 | Below 18 years old | 25 (34) | 48 (66) |
| Lopez-Espejo et al. [7] | Single centre-prospective observational study | Patients admitted to the Pontifical Catholic University of Chile’s Clinical Hospital (Chile) | 119 | Between 30 days and 18 years old | 45 (37.8) | 74 (62.2) |
| deVeber et al. [17] | Prospective, national population-based study | Patients registered in the Canadian Pediatric Ischemic Stroke Registry diagnosed with AIS in any of the 16 Canadian acute care paediatric hospitals (Canada) | 933 | From birth to 28 days and from 29 days to 18 years | 420 (45) | 513 (55) |
| Bohmer et al. [21] | Retrospective | Patients admitted to the Department of Pediatrics, University Hospital of Muenster (Germany) | 86 | >29 days and <18 years old | 42 (49) | 44 (51) |
| Steinlin et al. [22] | Retrospective | Patient cohorts with FCA from Switzerland and Australia | 73 | From 1 month to 18 years old | 36 (49.3) | 37 (50.7) |
| Per et al. [23] | Retrospective | Patients diagnosed at Erciyes University Children’s Hospital in Central Anatolia (Turkey) | 130 | From 1 month to 16 years old | 62 (47.7) | 68 (52.3) |
| Rambaud et al. [24] | Retrospective cohort study | Patients with a first-ever ischemic stroke hospitalized in 10 French academic centres (France) | 60 | 10–18 years old | 28 (47) | 32 (53) |
| Nowak-Göttl et al. [25] | Prospective multicentre study | Patients recruited from different geographic areas of Germany | 198 | from 6 months to 16 years old | 105 (53) | 93 (47) |
| Masri and Al-Ammouri [26] | Retrospective | Patients from the Child Neurology Clinic at Jordan University Hospital (Jordan) | 24 | 1 month to 13 years (median: 5 years) | 12 (50) | 12 (50) |
| Total, n | 3437 | 1491 | 1946 |
| Study | Type of the Study | Population | Number of Cases | Age at Time of AIS | Females n (%) | Males n (%) |
|---|---|---|---|---|---|---|
| Bergman et al. [42] | Retrospective, nationwide cohort study | Cohort was based on three registries: the Swedish Stroke Register, the Swedish National Patient Register and the National Board of Health and Welfare, and the Population Register (Sweden) | 2599 | 15–44 | 1088 (41.9) | 1511 (58.1) |
| Martínez-Sánchez et al. [43] | Retrospective | Patients admitted at the Stroke Center, Department of Neurology, Hospital Universitario La Paz, Madrid (Spain) | 310/38 * | 15–50/ 15–30 * | 128 (42.3)/ 18 (47.4) * | 182 (58.7)/ 20 (52.6) * |
| Spengos and Vemmos [44] | Prospective, cooperative observational study | Patients admitted to the Departments of Neurology and Clinical Therapeutics of the Athens University Medical School (Greece) | 253/48 * | 15–45/ 15–30 * | 110 (43.5)/ 27 (56.2) * | 143 (56.5)/ 21 (43.8) * |
| Kwon et al. [45] | Retrospective | Patients admitted to the Department of Neurology, University of Ulsan, Asan Medical Center, Seoul (South Korea) | 149 | 15–44 | 37 (24.8) | 112 (75.2) |
| Tang et al. [46] | Retrospective cohort study | Young adults with ischemic stroke consecutively admitted to the Peking Union Medical College Hospital (China) | 411 | 18–50 | 129 (31.4) | 282 (68.6) |
| Aigner et al. [47] | Nationwide case–control study | Patients with first-ever stroke from Germany | 2009 | 18–55 | 762 (37.9) | 1247 (62.1) |
| Putaala et al. [48] | Retrospective | Patients aged 15 to 49 admitted to Helsinki University Central Hospital (Finland) | 1008 | 15–49 | 380 (37.7) | 628 (62.3) |
| Arntz et al. [49] | Prospective cohort study | Patients recruited in the Follow-Up of Transient Ischemic Attack and Stroke Patients and Unelucidated Risk Factor Evaluation (FUTURE) study and admitted to the Radboud University Nijmegen Medical Centre (Netherlands) | 337 | 18–50 | 240 (54.6) | 153 (45.4) |
| Ekker et al. [50] | Registry-based cohort study | Cohort was based on two registries: the Dutch nationwide hospital registry and the National Cause of Death Registry (Netherlands) | 8444 | 18–49 | 4593 (54.4) | 3851 (45.6) |
| Leppert et al. [51] | Retrospective cohort study | Randomly selected sample of a large commercial health insurance database, PharMetrics | 5218 | 15–54 | 2651 (50.8) | 2567 (49.2) |
| Onwuchekwa et al. [52] | Retrospective, descriptive study | Patients admitted to the University of Port Harcourt Teaching Hospital, Port Harcourt, Rivers State (Nigeria) | 54 | 18–45 | 26 (48.1) | 28 (51.9) |
| Wu et al. [53] | Retrospective | Patients in a hospital-based population in South Auckland (New Zealand) | 131 | 15–45 | 66 (50.4) | 65 (49.6) |
| Lasek-Bal et al. [54] | Retrospective | Patients hospitalized in the Department of Neurology and Department of Child Neurology/Division of Pediatrics and Developmental Age Neurology in Katowice (Poland) | 141 | 1–51 | 67 (47.5) | 74 (52.5) |
| Total, n | 21,064/86 * | 10,277/45 * | 10,843/41 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sarecka-Hujar, B.; Kopyta, I. The Impact of Sex on Arterial Ischemic Stroke in Young Patients: From Stroke Occurrence to Poststroke Consequences. Children 2021, 8, 238. https://doi.org/10.3390/children8030238
Sarecka-Hujar B, Kopyta I. The Impact of Sex on Arterial Ischemic Stroke in Young Patients: From Stroke Occurrence to Poststroke Consequences. Children. 2021; 8(3):238. https://doi.org/10.3390/children8030238
Chicago/Turabian StyleSarecka-Hujar, Beata, and Ilona Kopyta. 2021. "The Impact of Sex on Arterial Ischemic Stroke in Young Patients: From Stroke Occurrence to Poststroke Consequences" Children 8, no. 3: 238. https://doi.org/10.3390/children8030238
APA StyleSarecka-Hujar, B., & Kopyta, I. (2021). The Impact of Sex on Arterial Ischemic Stroke in Young Patients: From Stroke Occurrence to Poststroke Consequences. Children, 8(3), 238. https://doi.org/10.3390/children8030238







