Spine Fractures in Children and Adolescents—Frequency, Causes, Diagnostics, Therapy and Outcome—A STROBE-Compliant Retrospective Study at a Level 1 Trauma Centre in Central Europe
Abstract
:1. Introduction
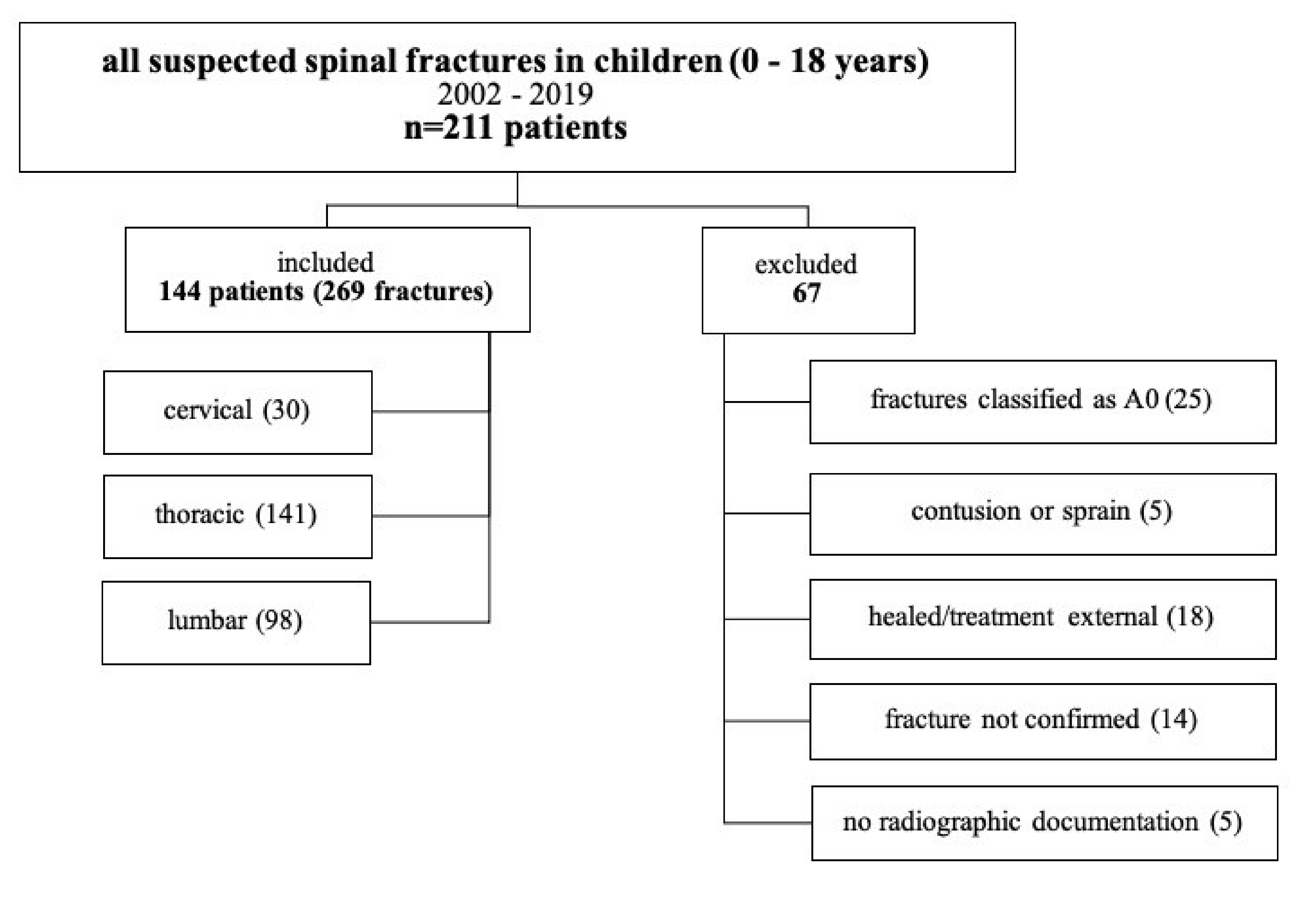
2. Methods
Data Analysis
3. Results
3.1. Injury Mechanisms
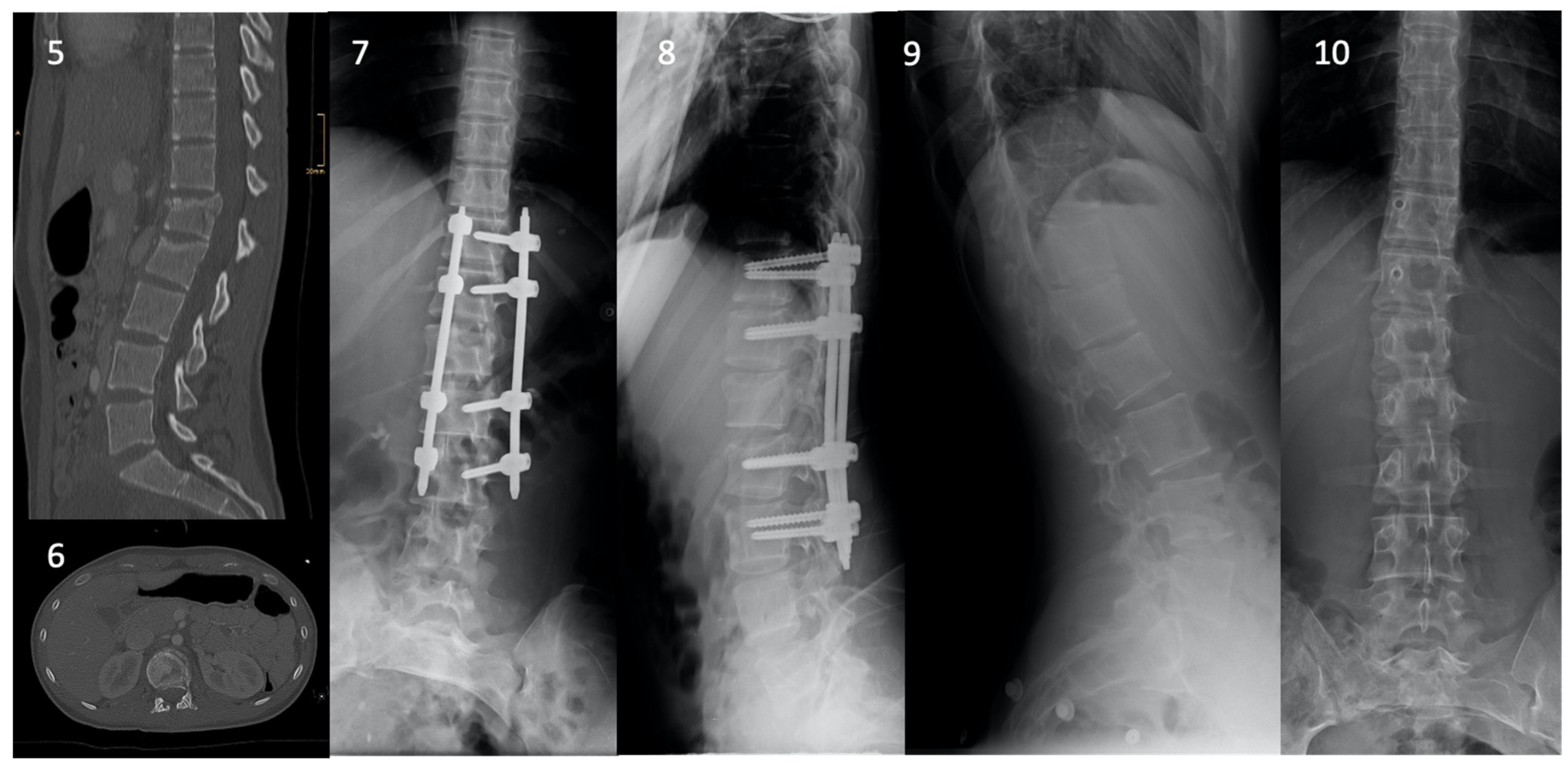
3.2. Fracture Characteristics and Management
3.3. Neurological Deficits and Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Item No | Recommendation | |
| Title and abstract (applied) | 1 | (a) Indicate the study’s design with a commonly used term in the title or the abstract |
| (applied) | (b) Provide in the abstract an informative and balanced summary of what was completed and what was found | |
| Introduction | ||
| Background/rationale (applied) | 2 | Explain the scientific background and rationale for the investigation being reported |
| Objectives (applied) | 3 | State specific objectives, including any prespecified hypotheses |
| Methods | ||
| Study design (applied) | 4 | Present key elements of study design early in the paper |
| Setting (applied) | 5 | Describe the setting, locations, and relevant dates, including periods of recruitment, exposure, follow-up, and data collection |
| Participants (not applicable) | 6 | (a) Cohort study—Give the eligibility criteria, and the sources and methods of selection of participants. Describe methods of follow-up Case-control study—Give the eligibility criteria, and the sources and methods of case ascertainment and control selection. Give the rationale for the choice of cases and controls Cross-sectional study—Give the eligibility criteria, and the sources and methods of selection of participants |
| (not applicable) | (b) Cohort study—For matched studies, give matching criteria and number of exposed and unexposed Case-control study—For matched studies, give matching criteria and the number of controls per case | |
| Variables (applied) | 7 | Clearly define all outcomes, exposures, predictors, potential confounders, and effect modifiers. Give diagnostic criteria, if applicable |
| Data sources/measurement (applied) | 8 * | For each variable of interest, give sources of data and details of methods of assessment (measurement). Describe comparability of assessment methods if there is more than one group |
| Bias | 9 | Describe any efforts to address potential sources of bias |
| Study size (applied) | 10 | Explain how the study size was arrived at |
| Quantitative variables (applied) | 11 | Explain how quantitative variables were handled in the analyses. If applicable, describe which groupings were chosen and why |
| Statistical methods (applied) | 12 | (a) Describe all statistical methods, including those used to control for confounding |
| (not applicable) | (b) Describe any methods used to examine subgroups and interactions | |
| (not applicable) | (c) Explain how missing data were addressed | |
| (not applicable) | (d) Cohort study—If applicable, explain how loss to follow-up was addressed Case-control study—If applicable, explain how matching of cases and controls was addressed Cross-sectional study—If applicable, describe analytical methods taking account of sampling strategy | |
| (not applicable) | (e) Describe any sensitivity analyses | |
| Results | ||
| Participants (applied) | 13 * | (a) Report numbers of individuals at each stage of study—eg numbers potentially eligible, examined for eligibility, confirmed eligible, included in the study, completing follow-up, and analysed |
| (applied) | (b) Give reasons for non-participation at each stage | |
| (applied) | (c) Consider use of a flow diagram | |
| Descriptive data (applied) | 14 * | (a) Give characteristics of study participants (eg demographic, clinical, social) and information on exposures and potential confounders |
| (applied) | (b) Indicate number of participants with missing data for each variable of interest | |
| (applied) | (c) Cohort study—Summarise follow-up time (eg, average and total amount) | |
| Outcome data (not applicable) | 15 * | Cohort study—Report numbers of outcome events or summary measures over time |
| (not applicable) | Case-control study—Report numbers in each exposure category, or summary measures of exposure | |
| (applied) | Cross-sectional study—Report numbers of outcome events or summary measures | |
| Main results (not applicable) | 16 | (a) Give unadjusted estimates and, if applicable, confounder-adjusted estimates and their precision (eg, 95% confidence interval). Make clear which confounders were adjusted for and why they were included |
| (not applicable) | (b) Report category boundaries when continuous variables were categorized | |
| (not applicable) | (c) If relevant, consider translating estimates of relative risk into absolute risk for a meaningful time period | |
| Other analyses (not applicable) | 17 | Report other analyses performed—eg analyses of subgroups and interactions, and sensitivity analyses |
| Discussion | ||
| Key results (applied) | 18 | Summarise key results with reference to study objectives |
| Limitations (applied) | 19 | Discuss limitations of the study, taking into account sources of potential bias or imprecision. Discuss both direction and magnitude of any potential bias |
| Interpretation (applied) | 20 | Give a cautious overall interpretation of results considering objectives, limitations, multiplicity of analyses, results from similar studies, and other relevant evidence |
| Generalisability (applied) | 21 | Discuss the generalisability (external validity) of the study results |
| Other Information | ||
| Funding (not applicable) | 22 | Give the source of funding and the role of the funders for the present study and, if applicable, for the original study on which the present article is based |
| Note: An Explanation and Elaboration article discusses each checklist item and gives the methodological background and published examples of transparent reporting. The STROBE checklist is best used in conjunction with this article (freely available on the Web sites of PLoS Medicine at http://www.plosmedicine.org/, Annals of Internal Medicine at http://www.annals.org/, and Epidemiology at http://www.epidem.com/). Information on the STROBE Initiative is available at www.strobe-statement.org. * Give information separately for cases and controls in case-control studies and, if applicable, for exposed and unexposed groups in cohort and cross-sectional studies. | ||
References
- Cirak, B.; Ziegfeld, S.; Knight, V.M.; Chang, D.; Avellino, A.M.; Paidas, C.N. Spinal injuries in children. J. Pediatr. Surg. 2004, 39, 607–612. [Google Scholar] [CrossRef] [PubMed]
- Akbarnia, B.A. Pediatric spine fractures. Orthop. Clin. N. Am. 1999, 30, 521–536. [Google Scholar] [CrossRef]
- Brown, R.L.; Brunn, M.A.; Garcia, V.F. Cervical spine injuries in children: A review of 103 patients treated consecutively at a level 1 pediatric trauma center. J. Pediatr. Surg. 2001, 36, 1107–1114. [Google Scholar] [CrossRef]
- Kokoska, E.R.; Keller, M.S.; Rallo, M.C.; Weber, T.R. Characteristics of pediatric cervical spine injuries. J. Pediatr. Surg. 2001, 36, 100–105. [Google Scholar] [CrossRef]
- Patel, J.C.; Tepas, J.J., 3rd; Mollitt, D.L.; Pieper, P. Pediatric cervical spine injuries: Defining the disease. J. Pediatr. Surg. 2001, 36, 373–376. [Google Scholar] [CrossRef]
- Platzer, P.; Jaindl, M.; Thalhammer, G.; Dittrich, S.; Kutscha-Lissberg, F.; Vecsei, V.; Gaebler, C. Cervical spine injuries in pediatric patients. J. Trauma 2007, 62, 389–396. [Google Scholar] [CrossRef]
- Jarvers, J.S.; Spiegl, U.; von der Hoh, N.; Josten, C.; Heyde, C.E. Injuries of the thoracolumbar spine in children. Orthopade 2016, 45, 472–483. [Google Scholar] [CrossRef]
- Sayama, C.; Chen, T.; Trost, G.; Jea, A. A review of pediatric lumbar spine trauma. Neurosurg. Focus 2014, 37, E6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ogden, J.A. Spine. In Skeletal Injury in the Child, 3rd ed.; Ogden, J.A., Ed.; Springer: New York, NY, USA, 2000; pp. 708–789. [Google Scholar]
- Rose, S.; Marzi, I. Wirbelsäule. In Kindertraumatologie; Marzi, I., Ed.; Springer: Berlin/Heidelberg, Germany, 2010; Volume 2, pp. 355–384. [Google Scholar]
- Bilston, L.E.; Brown, J. Pediatric spinal injury type and severity are age and mechanism dependent. Spine 2007, 32, 2339–2347. [Google Scholar] [CrossRef] [PubMed]
- Carreon, L.Y.; Glassman, S.D.; Campbell, M.J. Pediatric Spine Fractures: A Review of 137 Hospital Admissions. Clin. Spine Surg. 2004, 17, 477–482. [Google Scholar] [CrossRef] [PubMed]
- Gehweiler, J.; Osborne, R.; Becker, R. The Radiology of Vertebral Trauma; W. B. Saunders Company: Philadelphia, PA, USA, 1980. [Google Scholar]
- Anderson, L.D.; D’Alonzo, R.T. Fractures of the Odontoid Process of the Axis. J. Bone Jt. Surg. 1974, 56, 1663–1674. [Google Scholar] [CrossRef]
- Effendi, B.; Roy, D.; Cornish, B.; Dussault, R.; Laurin, C. Fractures of the ring of the axis. A classification based on the analysis of 131 cases. J. Bone Jt. Surg. 1981, 63, 319–327. [Google Scholar] [CrossRef] [PubMed]
- Vaccaro, A.R.; Oner, C.; Kepler, C.K.; Dvorak, M.; Schnake, K.; Bellabarba, C.; Reinhold, M.; Aarabi, B.; Kandziora, F.; Chapman, J.; et al. AOSpine thoracolumbar spine injury classification system: Fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976) 2013, 38, 2028–2037. [Google Scholar] [CrossRef]
- Frankel, H.L.; Hancock, D.O.; Hyslop, G.; Melzak, J.; Michaelis, L.S.; Ungar, G.H.; Vernon, J.D.S.; Walsh, J.J. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Spinal Cord 1969, 7, 179–192. [Google Scholar] [CrossRef] [Green Version]
- Compagnon, R.; Ferrero, E.; Leroux, J.; Lefevre, Y.; Journeau, P.; Vialle, R.; Glorion, C.; Violas, P.; Chalopin, A.; Odent, T.; et al. Epidemiology of spinal fractures in children: Cross-sectional study. Orthop. Traumatol. Surg. Res. 2020, 106, 1245–1249. [Google Scholar] [CrossRef] [PubMed]
- Dauleac, C.; Beuriat, P.A.; Di Rocco, F.; Szathmari, A.; Mottolese, C. Surgical Management of Pediatric Spine Trauma: 12 Years of Experience. World Neurosurg. 2019, 126, e1494–e1502. [Google Scholar] [CrossRef] [PubMed]
- Reddy, S.P.; Junewick, J.J.; Backstrom, J.W. Distribution of spinal fractures in children: Does age, mechanism of injury, or gender play a significant role? Pediatr. Radiol. 2003, 33, 776–781. [Google Scholar] [CrossRef]
- Poorman, G.W.; Segreto, F.A.; Beaubrun, B.M.; Jalai, C.M.; Horn, S.R.; Bortz, C.A.; Diebo, B.G.; Vira, S.; Bono, O.J.; De La Garza-Ramos, R.; et al. Traumatic Fracture of the Pediatric Cervical Spine: Etiology, Epidemiology, Concurrent Injuries, and an Analysis of Perioperative Outcomes Using the Kids’ Inpatient Database. Int. J. Spine Surg. 2019, 13, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.I.; Lee, N.J.; Cho, S.K. Pediatric Cervical Spine and Spinal Cord Injury: A National Database Study. Spine 2016, 41, 283–292. [Google Scholar] [CrossRef] [PubMed]
- Mahan, S.T.; Mooney, D.P.; Karlin, L.I.; Hresko, M.T. Multiple Level Injuries in Pediatric Spinal Trauma. J. Trauma Acute Care Surg. 2009, 67, 537–542. [Google Scholar] [CrossRef] [PubMed]
- Alas, H.; Pierce, K.E.; Brown, A.; Bortz, C.; Naessig, S.; Ahmad, W.; Moses, M.J.; O’Connell, B.; Maglaras, C.; Diebo, B.G.; et al. Sports-related Cervical Spine Fracture and Spinal Cord Injury: A Review of Nationwide Pediatric Trends. Spine 2021, 46, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Knox, J.B.; Schneider, J.E.; Cage, J.M.; Wimberly, R.L.; Riccio, A.I. Spine trauma in very young children: A retrospective study of 206 patients presenting to a level 1 pediatric trauma center. J. Pediatr. Orthop. 2014, 34, 698–702. [Google Scholar] [CrossRef] [PubMed]
- Puisto, V.; Kääriäinen, S.; Impinen, A.; Parkkila, T.; Vartiainen, E.; Jalanko, T.; Pakarinen, M.P.; Helenius, I. Incidence of Spinal and Spinal Cord Injuries and Their Surgical Treatment in Children and Adolescents: A Population-Based Study. Spine 2010, 35, 104–107. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Vassilyadi, M.; Forbes, J.K.; Moroz, N.W.; Camacho, A.; Moroz, P.J. Traumatic spinal injuries in children at a single level 1 pediatric trauma centre: Report of a 23-year experience. Can. J. Surg. 2016, 59, 205–212. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, S.-H.; Choo, W.-H.; Kim, D.H. Thoracic and Lumbar Anatomy and Surgical Approaches. In Surgery of the Pediatric Spine; Kim, D.H., Betz, R.R., Huhn, S.L., Newton, P.O., Eds.; Thieme: New York, NY, USA; Stuttgart, Germany, 2008; pp. 102–120. [Google Scholar]
- Bogduk, N.; Yoganandan, N. Biomechanics of the cervical spine Part 3: Minor injuries. Clin. Biomech. 2001, 16, 267–275. [Google Scholar] [CrossRef]

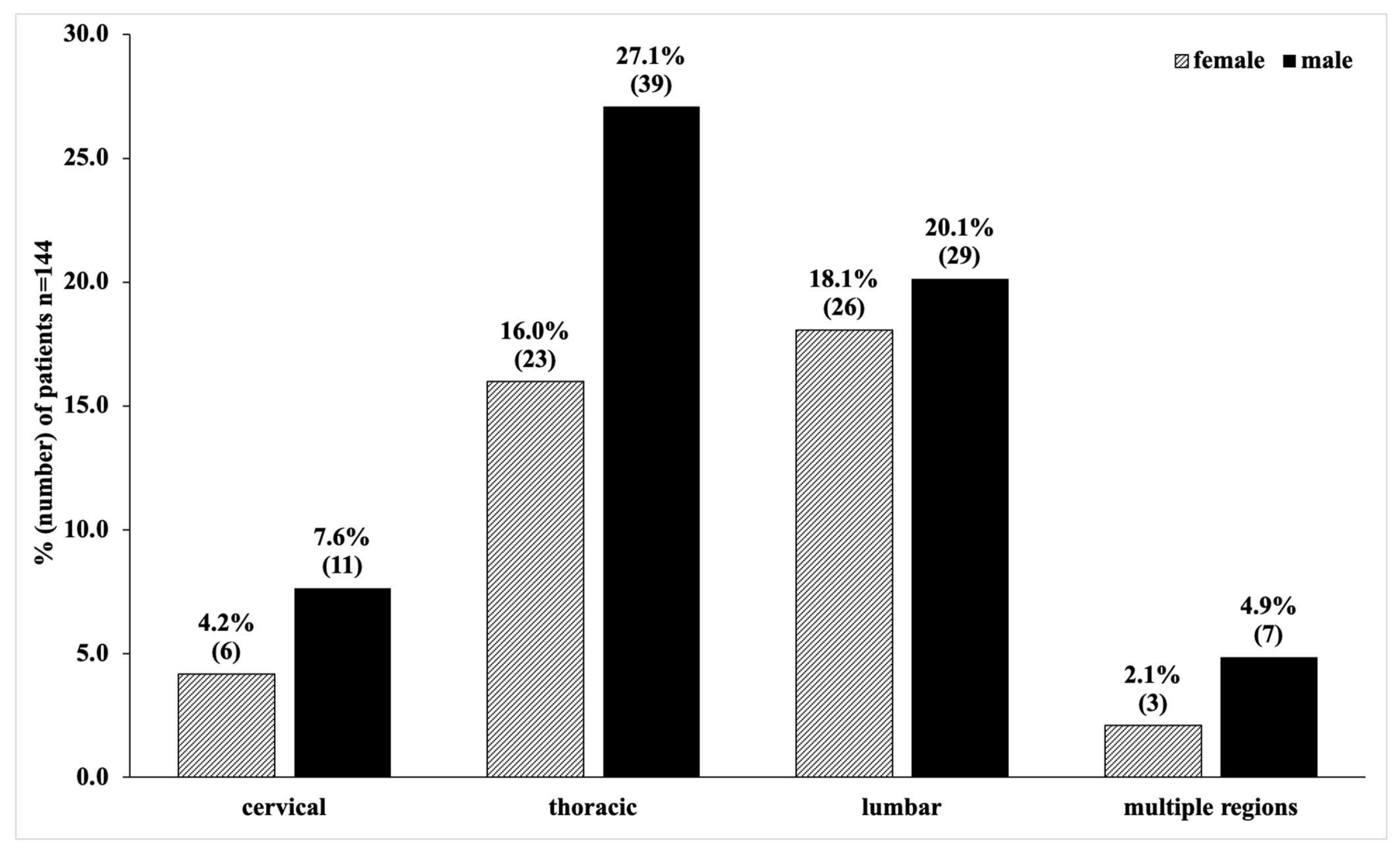

| n = 144 | (%) | Mean Age | Standard Deviation | Age Range | |
|---|---|---|---|---|---|
| (SD) | |||||
| female (f) | 58 | 40.3 | 14.2 | 4.0 | 1–18 |
| male (m) | 86 | 59.7 | 14.7 | 3.5 | 4–18 |
| total | 144 | 100.0 | 14.5 | 3.7 | 1–18 |
| Age Group (Years) | f | (%) | m | (%) | Total | (%) |
|---|---|---|---|---|---|---|
| toddler (0–1) | 2 | 1.4 | 0 | 0 | 2 | 1.4 |
| pre-schooler (2–5) | 2 | 1.4 | 3 | 2.1 | 5 | 3.5 |
| elementary (6–11) | 5 | 3.5 | 9 | 6.3 | 14 | 9.7 |
| high-schooler (12–15) | 22 | 15.3 | 25 | 17.4 | 47 | 32.6 |
| adolescent (16–18) | 27 | 31.3 | 49 | 34 | 76 | 52.8 |
| 2002–2007 | (%) | 2008–2013 | (%) | 2014–2019 | (%) | |
|---|---|---|---|---|---|---|
| Fall | 16 | 11.1 | 24 | 16.7 | 26 | 18.1 |
| Road Incident | 16 | 11.1 | 7 | 4.9 | 7 | 4.9 |
| Sports Incident | 10 | 6.9 | 13 | 9.0 | 20 | 13.9 |
| n = 269 Fractures | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Upper Cervical Spine | Total | Mean Age | (%) | Surg. | Mean Age | (%) | Cons. | Mean Age | (%) |
| Gehweiler Type I | 2 | 2.5 | 0.7 | 0 | - | 0.0 | 2 | 2.5 | 0.7 |
| Gehweiler Type II | 1 | 4 | 0.4 | 0 | - | 0.0 | 1 | 4 | 0.4 |
| Gehweiler Type III | 0 | - | 0.0 | 0 | - | 0.0 | 0 | - | 0.0 |
| Gehweiler Type IV | 0 | - | 0.0 | 0 | - | 0.0 | 0 | - | 0.0 |
| Gehweiler Type V | 0 | - | 0.0 | 0 | - | 0.0 | 0 | - | 0.0 |
| Anderson and D’Alonzo Type I | 0 | - | 0.0 | 0 | - | 0.0 | 0 | - | 0.0 |
| Anderson and D’Alonzo Type II | 0 | - | 0.0 | 0 | - | 0.0 | 0 | - | 0.0 |
| Anderson and D’Alonzo Type III | 2 | 16.5 | 0.7 | 1 | 18 | 0.4 | 1 | 15 | 0.4 |
| Effendi Type I | 1 | 16 | 0.4 | 0 | - | 0.0 | 1 | 16 | 0.4 |
| Effendi Type II | 0 | - | 0.0 | 0 | - | 0.0 | 0 | - | 0.0 |
| Effendi Type III | 0 | - | 0.0 | 0 | - | 0.0 | 0 | - | 0.0 |
| Lower Cervical Spine | Total | Mean Age | (%) | Surg. | Mean Age | (%) | Cons. | Mean Age | (%) |
| A1 | 15 | 16 | 5.6 | 4 | 17.3 | 1.5 | 11 | 15.5 | 4.1 |
| A2 | 3 | 14.7 | 1.1 | 1 | 14.0 | 0.4 | 2 | 16.0 | 0.7 |
| A3 | 3 | 17.3 | 1.1 | 2 | 17 | 0.7 | 1 | 18 | 0.4 |
| A4 | 1 | 15.0 | 0.4 | 1 | 15.0 | 0.4 | 0 | - | 0.0 |
| B1 | 0 | - | 0.0 | 0 | - | 0.0 | 0 | - | 0.0 |
| B2 | 1 | 18.0 | 0.4 | 1 | 18.0 | 0.4 | 0 | - | 0.0 |
| B3 | 0 | - | 0.0 | 0 | - | 0.0 | 0 | - | 0.0 |
| C | 1 | 17.0 | 0.4 | 1 | 17.0 | 0.4 | 0 | 0.0 | |
| Thoracic Spine | Total | Mean Age | (%) | Surg. | Mean Age | (%) | Cons. | Mean Age | (%) |
| A1 | 117 | 14.4 | 43.5 | 0 | - | 0.0 | 117 | 14.4 | 43.5 |
| A2 | 3 | 15.7 | 1.1 | 1 | 15.0 | 0.4 | 2 | 16.0 | 0.7 |
| A3 | 6 | 16.0 | 2.2 | 5 | 16.4 | 1.9 | 1 | 14.0 | 0.4 |
| A4 | 8 | 15.4 | 3.0 | 4 | 15.3 | 1.5 | 4 | 15.5 | 1.5 |
| B1 | 0 | - | 0.0 | 0 | - | 0.0 | 0 | - | 0.0 |
| B2 | 5 | 8.4 | 1.9 | 5 | 8.4 | 1.9 | 0 | - | 0.0 |
| B3 | 1 | 16.0 | 0.4 | 1 | 16.0 | 0.4 | 0 | - | 0.0 |
| C | 1 | 17.0 | 0.4 | 1 | 17.0 | 0.4 | 0 | - | 0.0 |
| Lumbar Spine | Total | Mean Age | (%) | Surg. | Mean Age | (%) | Cons. | Mean Age | (%) |
| A1 | 63 | 14.5 | 23.4 | 1 | 15.0 | 0.4 | 62 | 14.5 | 23.0 |
| A2 | 9 | 13.6 | 3.3 | 3 | 16.0 | 1.1 | 6 | 12.3 | 2.2 |
| A3 | 10 | 15.9 | 3.7 | 7 | 16.1 | 2.6 | 3 | 15.3 | 1.1 |
| A4 | 15 | 15.8 | 5.6 | 12 | 16.5 | 4.5 | 3 | 13.3 | 1.1 |
| B1 | 0 | - | 0.0 | 0 | - | 0.0 | 0 | - | 0.0 |
| B2 | 0 | - | 0.0 | 0 | - | 0.0 | 0 | - | 0.0 |
| B3 | 0 | - | 0.0 | 0 | - | 0.0 | 0 | - | 0.0 |
| C | 1 | 16.0 | 0.4 | 1 | 16.0 | 0.4 | 0 | - | 0.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Payr, S.; Schuller, A.; Dangl, T.; Chocholka, B.; Binder, H.; Tiefenboeck, T.M. Spine Fractures in Children and Adolescents—Frequency, Causes, Diagnostics, Therapy and Outcome—A STROBE-Compliant Retrospective Study at a Level 1 Trauma Centre in Central Europe. Children 2021, 8, 1127. https://doi.org/10.3390/children8121127
Payr S, Schuller A, Dangl T, Chocholka B, Binder H, Tiefenboeck TM. Spine Fractures in Children and Adolescents—Frequency, Causes, Diagnostics, Therapy and Outcome—A STROBE-Compliant Retrospective Study at a Level 1 Trauma Centre in Central Europe. Children. 2021; 8(12):1127. https://doi.org/10.3390/children8121127
Chicago/Turabian StylePayr, Stephan, Andrea Schuller, Theresia Dangl, Britta Chocholka, Harald Binder, and Thomas M. Tiefenboeck. 2021. "Spine Fractures in Children and Adolescents—Frequency, Causes, Diagnostics, Therapy and Outcome—A STROBE-Compliant Retrospective Study at a Level 1 Trauma Centre in Central Europe" Children 8, no. 12: 1127. https://doi.org/10.3390/children8121127
APA StylePayr, S., Schuller, A., Dangl, T., Chocholka, B., Binder, H., & Tiefenboeck, T. M. (2021). Spine Fractures in Children and Adolescents—Frequency, Causes, Diagnostics, Therapy and Outcome—A STROBE-Compliant Retrospective Study at a Level 1 Trauma Centre in Central Europe. Children, 8(12), 1127. https://doi.org/10.3390/children8121127








