Prediction Model for Bronchopulmonary Dysplasia in Preterm Newborns
Abstract
1. Introduction
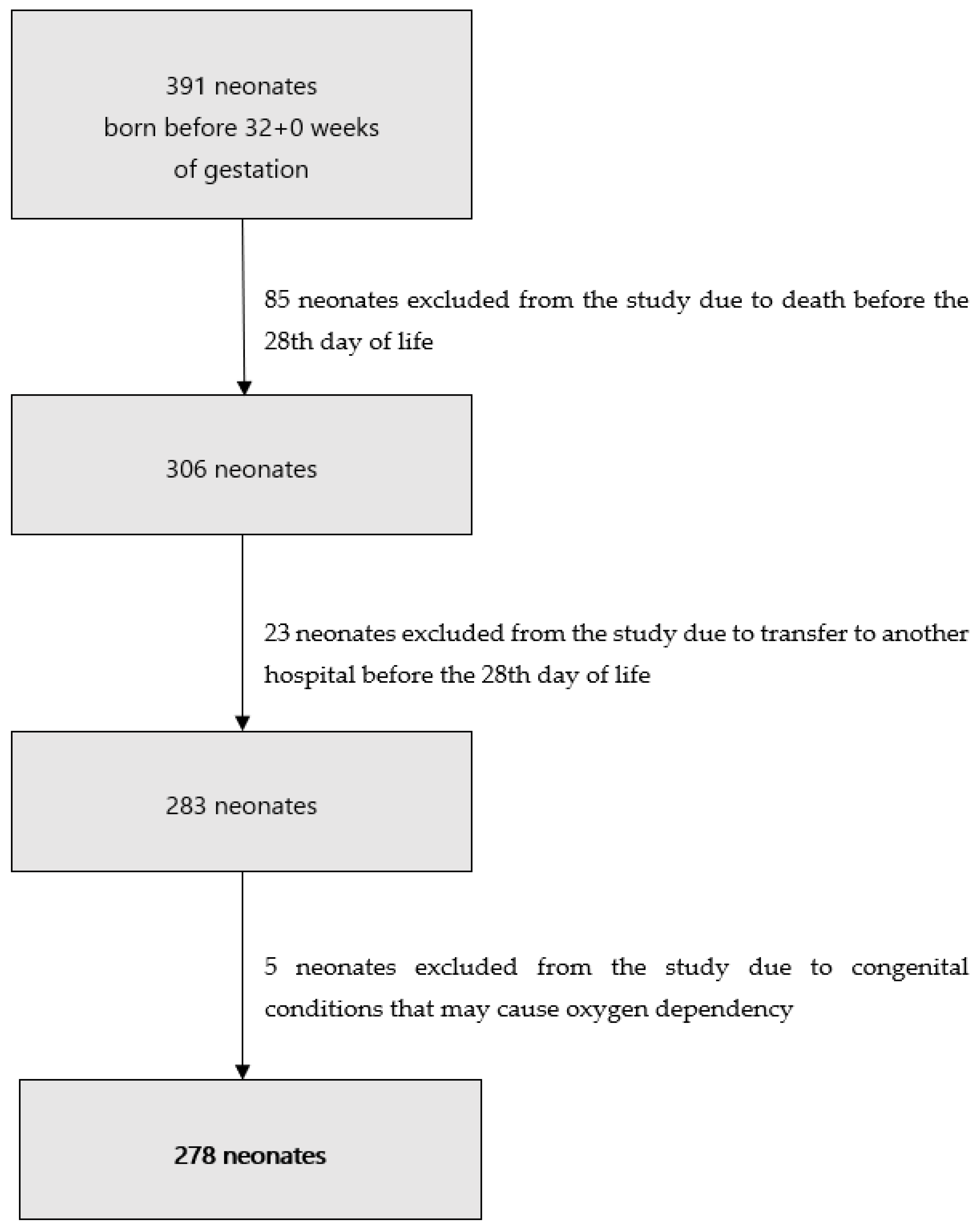
2. Materials and Methods
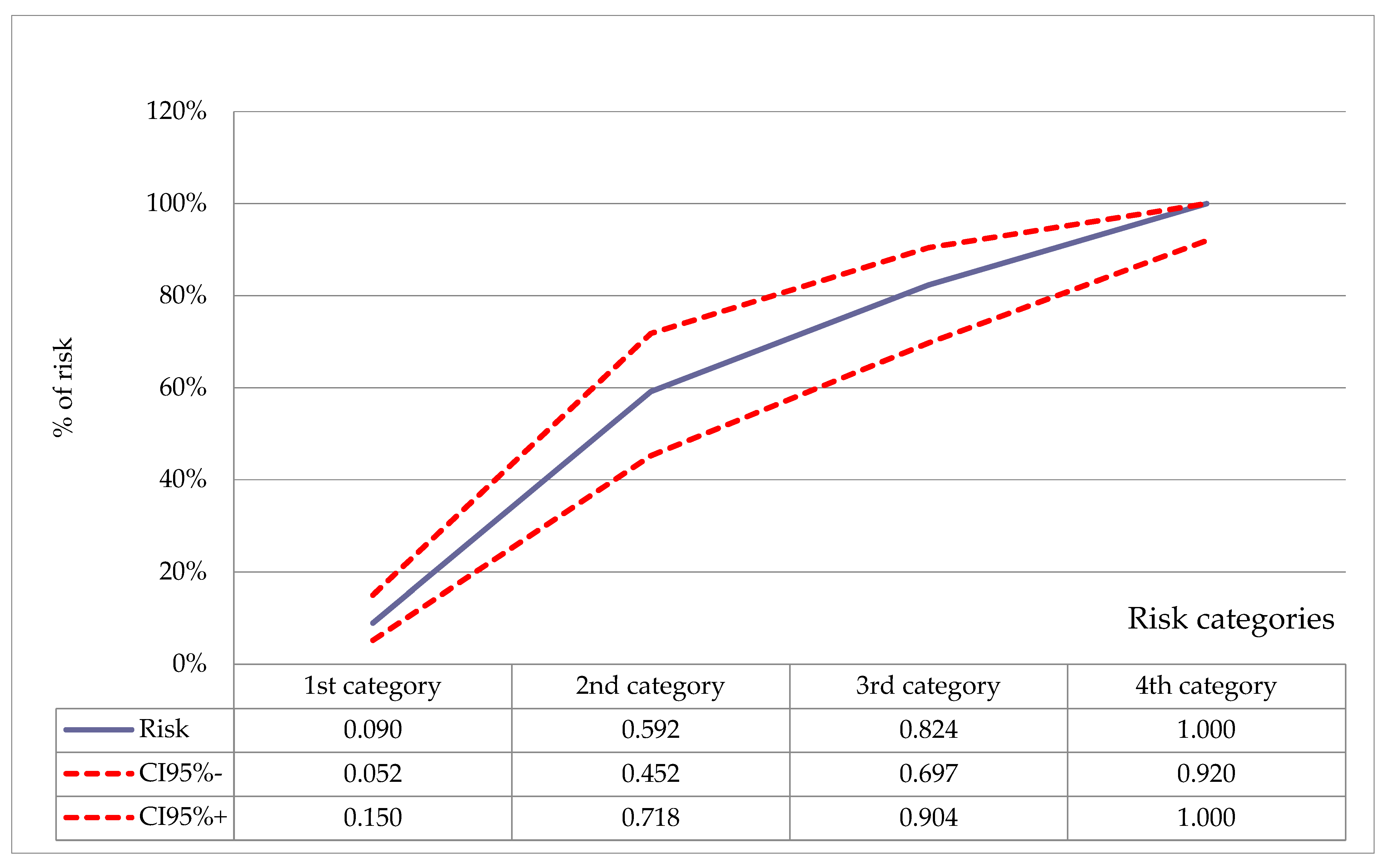
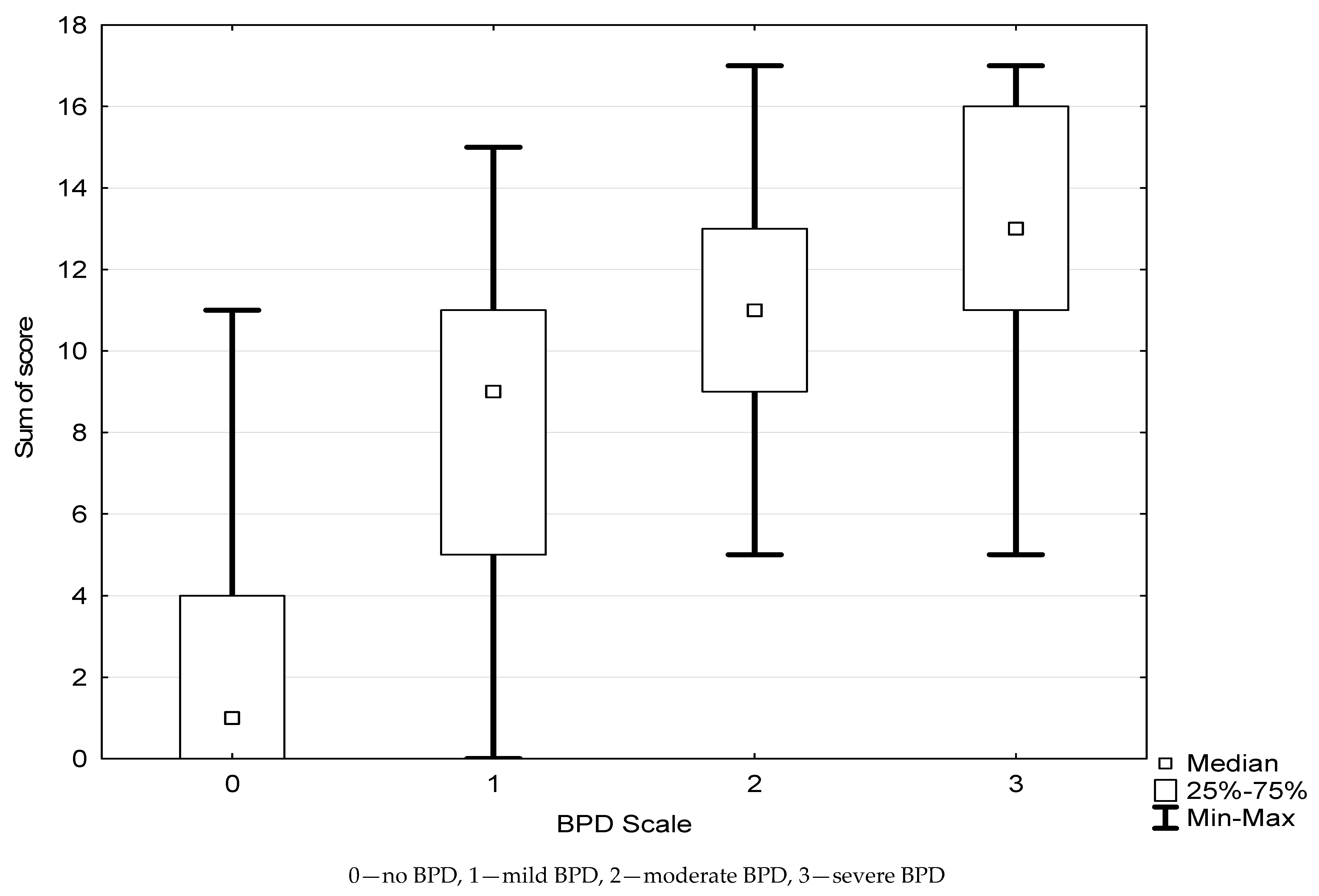
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Howson, E.C.; Kinney, M.; Lawn, J. Born Too Soon, The Global Action Report on Preterm Birth; Howson, C.P., Kinney, M.V., Lawn, J.E., Eds.; World Health Organization: Geneva, Switzerland, 2012; Volume 13. [Google Scholar]
- Johnston, K.M.; Gooch, K.; Korol, E.; Vo, P.; Eyawo, O.; Bradt, P.; Levy, A. The economic burden of prematurity in Canada. BMC Pediatr. 2014, 14. [Google Scholar] [CrossRef]
- Zysman-Colman, Z.; Tremblay, G.M.; Bandeali, S.; Landry, J.S. Bronchopulmonary dysplasia—Trends over three decades. Paediatr. Child Health 2013, 18, 86–90. [Google Scholar] [CrossRef]
- Ancel, P.-Y.; Goffinet, F.; Kuhn, P.; Langer, B.; Matis, J.; Hernandorena, X.; Chabanier, P.; Joly-Pedespan, L.; Lecomte, B.; Vendittelli, F.; et al. Survival and Morbidity of Preterm Children Born at 22 Through 34 Weeks’ Gestation in France in 2011. JAMA Pediatr. 2015, 169, 230–238. [Google Scholar] [CrossRef]
- Stoll, B.J.; Hansen, N.I.; Bell, E.F.; Shankaran, S.; Laptook, A.R.; Walsh, M.C.; Hale, E.C.; Newman, N.S.; Schibler, K.; Carlo, W.A.; et al. Neonatal Outcomes of Extremely Preterm Infants from the NICHD Neonatal Research Network. Pediatrics 2010, 126, 443–456. [Google Scholar] [CrossRef]
- Northway, W.H.; Rosan, R.C.; Porter, D.Y. Pulmonary Disease Following Respirator Therapy of Hyaline-Membrane Disease—Bronchopulmonary Dysplasia. N. Engl. J. Med. 1967, 276, 357–368. [Google Scholar] [CrossRef] [PubMed]
- Jobe, A.H. The new bronchopulmonary dysplasia. Curr. Opin. Pediatr. 2011, 23, 167–172. [Google Scholar] [CrossRef]
- Ehilgendorff, A.; O’Reilly, M.A. Bronchopulmonary Dysplasia Early Changes Leading to Long-Term Consequences. Front. Med. 2015, 2, 2. [Google Scholar] [CrossRef]
- Schmalisch, G.; Wilitzki, S.; Roehr, C.C.; Proquitté, H.; Bührer, C. Development of lung function in very low birth weight infants with or without bronchopulmonary dysplasia: Longitudinal assessment during the first 15 months of corrected age. BMC Pediatr. 2012, 12, 37. [Google Scholar] [CrossRef] [PubMed]
- Henderson-Smart, D.J.; Hutchinson, J.L.; Donoghue, D.A.; Evans, N.J.; Simpson, J.M.; Wright, I. Prenatal predictors of chronic lung disease in very preterm infants. Arch. Dis. Child.-Fetal Neonatal Ed. 2006, 91, F40–F45. [Google Scholar] [CrossRef] [PubMed]
- Lardon-Fernandez, M.; Uberos, J.; Molina-Oya, M.; Narbona-Lopez, E. Epidemiological factors involved in the development of bronchopulmonary dysplasia in very low birth-weight preterm infants. Minerva Pediatr. 2017, 69, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Botet, F.; Figueras-Aloy, J.; Miracle-Echegoyen, X.; Rodríguez-Miguélez, J.M.; Salvia-Roiges, M.; Carbonell-Estrany, X. Trends in survival among extremely-low-birth-weight infants (less than 1000 g) without significant bronchopulmonary dysplasia. BMC Pediatr. 2012, 12, 63. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.K.; Chang, Y.S.; Sung, S.; Ahn, S.Y.; Yoo, H.S.; Park, W.S. Trends in Survival and Incidence of Bronchopulmonary Dysplasia in Extremely Preterm Infants at 23-26 Weeks Gestation. J. Korean Med Sci. 2016, 31, 423–429. [Google Scholar] [CrossRef]
- Onland, W.; Debray, T.P.; Laughon, M.M.; Miedema, M.; Cools, F.; Askie, L.M.; Asselin, J.M.; A Calvert, S.; E Courtney, S.; Dani, C.; et al. Clinical prediction models for bronchopulmonary dysplasia: A systematic review and external validation study. BMC Pediatr. 2013, 13, 207. [Google Scholar] [CrossRef] [PubMed]
- Laughon, M.M.; Langer, J.C.; Bose, C.L.; Smith, P.B.; Ambalavanan, N.; Kathleen, A.; Eunice Kennedy Shriver National Institute of Child Health and Human Development Neonatal Research Network; Stoll, B.J.; Buchter, S.; Laptook, A.R.; et al. Prediction of Bronchopulmonary Dysplasia by Postnatal Age in Extremely Premature Infants. Am. J. Respir. Crit. Care Med. 2011, 183, 1715–1722. [Google Scholar] [CrossRef] [PubMed]
- Hayran, M.; Derin, H.; Ovali, F.; Gursoy, T. A Clinical Scoring System to Predict the Development of Bronchopulmonary Dysplasia. Am. J. Perinatol. 2014, 32, 659–666. [Google Scholar] [CrossRef] [PubMed]
- Nolan, J.P.; Soar, J.; Zideman, D.A.; Biarent, D.; Bossaert, L.L.; Deakin, C.; Koster, R.W.; Wyllie, J.; Böttiger, B.; ERC Guidelines Writing Group. European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation 2010, 81, 1219–1276. [Google Scholar] [CrossRef] [PubMed]
- Sweet, D.G.; Carnielli, V.; Greisen, G.; Hallman, M.; Ozek, E.; Plavka, R.; Saugstad, O.D.; Simeoni, U.; Speer, C.P.; Vento, M.; et al. European Consensus Guidelines on the Management of Neonatal Respiratory Distress Syndrome in Preterm Infants—2013 Update. Neonatology 2013, 103, 353–368. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://emedicine.medscape.com/article/978865-overview (accessed on 20 June 2021).
- A Gole, G.; Ells, A.L.; Katz, X.; Holmstrom, G.; Fielder, A.R.; Capone, A.; Flynn, J.T.; Good, W.G.; Holmes, J.M.; A McNamara, J.; et al. The International Classification of Retinopathy of Prematurity Revisited. Arch. Ophthalmol. 2005, 123, 991–999. [Google Scholar] [CrossRef]
- Bell, M.J.; Ternberg, J.L.; Feigin, R.D.; Keating, J.P.; Marshall, R.; Barton, L.; Brotherton, T. Neonatal Necrotizing Enterocolitis:Therapeutic decisions based upon clinical staging. Ann. Surg. 1978, 187, 1–7. [Google Scholar] [CrossRef]
- Papile, L.-A.; Burstein, J.; Burstein, R.; Koffler, H. Incidence and evolution of subependymal and intraventricular hemorrhage: A study of infants with birth weights less than 1500 gm. J. Pediatr. 1978, 92, 529–534. [Google Scholar] [CrossRef]
- Fenton, T.R. A new growth chart for preterm babies: Babson and Benda’s chart updated with recent data and a new format. BMC Pediatr. 2003, 3, 13. [Google Scholar] [CrossRef] [PubMed]
- Costeloe, K.L.; Hennessy, E.M.; Haider, S.; Stacey, F.; Marlow, N.; Draper, E. Short term outcomes after extreme preterm birth in England: Comparison of two birth cohorts in 1995 and 2006 (the EPICure studies). BMJ 2012, 345, e7976. [Google Scholar] [CrossRef] [PubMed]
- Egreteau, L.; Pauchard, J.-Y.; Semama, D.S.; Matis, J.; Liska, A.; Romeo, B.; Cneude, F.; Hamon, I.; Truffert, P. Chronic oxygen dependency in infants born at less than 32 weeks’ gestation: Incidence and risk factors. Pediatrics 2001, 108, e26. [Google Scholar] [CrossRef]
- Ahn, H.M.; Park, E.A.; Cho, S.J.; Kim, Y.-J.; Park, H.-S. The Association of Histological Chorioamnionitis and Antenatal Steroids on Neonatal Outcome in Preterm Infants Born at Less than Thirty-Four Weeks’ Gestation. Neonatology 2012, 102, 259–264. [Google Scholar] [CrossRef] [PubMed]
- Choi, C.W. Chorioamnionitis: Is a major player in the development of bronchopulmonary dysplasia? Korean J. Pediatr. 2017, 60, 203–207. [Google Scholar] [CrossRef][Green Version]
- Lee, H.J.; Kim, E.-K.; Kim, H.-S.; Choi, C.W.; Kim, B.I.; Choi, J.-H. Chorioamnionitis, respiratory distress syndrome and bronchopulmonary dysplasia in extremely low birth weight infants. J. Perinatol. 2010, 31, 166–170. [Google Scholar] [CrossRef] [PubMed]
- Wemhöner, A.; Jennings, P.; Haller, T.; Rüdiger, M.; Simbruner, G. Effect of exogenous surfactants on viability and DNA synthesis in A549, immortalized mouse type II and isolated rat alveolar type II cells. BMC Pulm. Med. 2011, 11, 11. [Google Scholar] [CrossRef] [PubMed]
- Geary, C.; Caskey, M.; Fonseca, R.; Malloy, M. Decreased Incidence of Bronchopulmonary Dysplasia After Early Management Changes, Including Surfactant and Nasal Continuous Positive Airway Pressure Treatment at Delivery, Lowered Oxygen Saturation Goals, and Early Amino Acid Administration: A Historical Cohort Study. Pediatrics 2008, 121, 89–96. [Google Scholar] [CrossRef]
- Kim, H.-R.; Kim, J.Y.; La Yun, B.; Lee, B.; Choi, C.W.; Kim, B.I. Interstitial pneumonia pattern on day 7 chest radiograph predicts bronchopulmonary dysplasia in preterm infants. BMC Pediatr. 2017, 17, 125. [Google Scholar] [CrossRef]
- Keszler, M.; Sant’Anna, G. Mechanical Ventilation and Bronchopulmonary Dysplasia. Clin. Perinatol. 2015, 42, 781–796. [Google Scholar] [CrossRef]
- Askie, L.M.; Darlow, B.A.; Finer, N.; Schmidt, B.; Stenson, B.; Tarnow-Mordi, W.; Davis, P.G.; Carlo, W.A.; Brocklehurst, P.; Davies, L.C.; et al. Neonatal Oxygenation Prospective Meta-analysis (NeOProM) Collaboration. Association Between Oxygen Saturation Targeting and Death or Disability in Extremely Preterm Infants in the Neonatal Oxygenation Prospective Meta-analysis Collaboration. JAMA 2018, 319, 2190–2201. [Google Scholar] [CrossRef] [PubMed]
- Ambalavanan, N.; Carlo, W.A. Ventilatory strategies in the prevention and management of bronchopulmonary dyspla-sia. Semin. Perinatol. 2006, 30, 192–199. [Google Scholar] [CrossRef] [PubMed]
- Demirel, N.; Bas, A.Y.; Zenciroglu, A. Bronchopulmonary dysplasia in very low birth weight infants. Indian J. Pediatr. 2009, 76, 695–698. [Google Scholar] [CrossRef]
- Potsiurko, S.; Dobryanskyy, D.; Sekretar, L. Patent ductus arteriosus, systemic NT-proBNP concentrations and development of bronchopulmonary dysplasia in very preterm infants: Retrospective data analysis from a randomized controlled trial. BMC Pediatr. 2021, 21, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kalhan, T.G.; Bateman, D.A.; Bowker, R.M.; Hod, E.A.; Kashyap, S. Effect of red blood cell storage time on markers of hemolysis and inflammation in transfused very low birth weight infants. Pediatr. Res. 2017, 82, 964–969. [Google Scholar] [CrossRef]
- Cunningham, K.E.; Okolo, F.C.; Baker, R.; Mollen, K.P.; Good, M. Red blood cell transfusion in premature infants leads to worse necrotizing enterocolitis outcomes. J. Surg. Res. 2017, 213, 158–165. [Google Scholar] [CrossRef]
- Patel, R.M.; Knezevic, A.; Shenvi, N.; Hinkes, M.; Keene, S.; Roback, J.D.; Easley, K.; Josephson, C.D. Association of Red Blood Cell Transfusion, Anemia, and Necrotizing Enterocolitis in Very Low-Birth-Weight Infants. JAMA 2016, 315, 889–897. [Google Scholar] [CrossRef]
- Rayjada, N.; Barton, L.; Chan, L.S.; Plasencia, S.; Biniwale, M.; Bui, K.C. Decrease in Incidence of Bronchopulmonary Dysplasia with Erythropoietin Administration in Preterm Infants: A Retrospective Study. Neonatology 2012, 102, 287–292. [Google Scholar] [CrossRef]
- Ohls, R.K.; Ehrenkranz, R.A.; Wright, L.L.; Lemons, J.A.; Korones, S.B.; Stoll, B.J.; Stark, A.R.; Shankaran, S.; Donovan, E.F.; Close, N.C.; et al. Effects of Early Erythropoietin Therapy on the Transfusion Requirements of Preterm Infants Below 1250 Grams Birth Weight: A Multicenter, Randomized, Controlled Trial. Pediatrics 2001, 108, 934–942. [Google Scholar] [CrossRef] [PubMed]
- Romagnoli, C.; Zecca, E.; Gallini, F.; Girlando, P.; Zuppa, A.A. Do recombinant human erythropoietin and iron supplementation increase the risk of retinopathy of prematurity? Eur. J. Nucl. Med. Mol. Imaging 2000, 159, 627–628. [Google Scholar] [CrossRef]
- Soll, R.F. Early erythropoietin for preventing red blood cell transfusion in preterm and/or low birth weight infants. Neonatology 2012, 102, 127–129. [Google Scholar] [CrossRef]
- Haiden, N.; Schwindt, J.; Cardona, F.; Berger, A.; Klebermass-Schrehof, K.; Wald, M.; Kohlhauser-Vollmuth, C.; Jilma, B.; Pollak, A. Effects of a Combined Therapy of Erythropoietin, Iron, Folate, and Vitamin B12 on the Transfusion Requirements of Extremely Low Birth Weight Infants. Pediatrics 2006, 118, 2004–2013. [Google Scholar] [CrossRef] [PubMed]
- Ohlsson, A.; Aher, S.M. Early erythropoiesis-stimulating agents in preterm or low birth weight infants. Cochrane Database Syst. Rev. 2017, 11, CD004863. [Google Scholar] [CrossRef] [PubMed]
- Sharma, D. Golden hour of neonatal life: Need of the hour. Matern. Health Neonatol. Perinatol. 2017, 3, 16. [Google Scholar] [CrossRef] [PubMed]

| Variable | BPD Group | No-BPD Group | p | OR | 95% CI | |
|---|---|---|---|---|---|---|
| n = 127 | n = 151 | |||||
| Sex | F/M | 64/63 (50%/50%) | 86/65 (57%/43%) | 0.331 | ||
| BPD severity | Mild | 79 (25%) | N/A | |||
| Moderate | 34 (12%) | |||||
| Severe | 13 (5%) | |||||
| data not available | 3 (1%) | |||||
| Gestational age (weeks) | Mean | 27.5 | 30.3 | <0.001 | 1.2 | 1.1–1.2 |
| Median | 27.9 | 30.4 | ||||
| Range | <23.4; 31.6> | <27; 32> | ||||
| Birth weight (grams) | Mean | 1002 | 1394 | <0.001 | 1.01 | 1.0–1.01 |
| Median | 970 | 1385 | ||||
| Range | <510; 1990> | <640; 2200> | ||||
| SGA | 10 (7.8%) | 9 (6%) | 0.726 | |||
| First pregnancy | 77 (61%) | 80 (53%) | 0.246 | |||
| Mean mother’s age (years) | 29.8 (SD 6.3) | 30.7 (SD 5.9) | ||||
| Mother’s arterial hypertension | PIH | 22 (17%) | 23 (15%) | 0.799 | ||
| Hypertension before pregnancy | 8 (26%) | 12 (7.8%) | ||||
| Diabetes mellitus | GDMG1 | 8 (6.3%) | 14 (9.3%) | 0.731 | ||
| GDMG2 | 2 (1.6%) | 3 (2%) | ||||
| DM1 | 3 (2.4%) | 2 (1.3%) | ||||
| Mother’s cervical smear | Physiologic/GBS negative | 38 (31%) | 57 (38%) | 0.772 | ||
| GBS positive | 16 (13%) | 19 (13%) | ||||
| Escherichia coli | 26 (21%) | 28 (19%) | ||||
| Ureaplasma urealitycum | 17 (14%) | 6 (11%) | ||||
| Other, non-physiologic | 27 (22%) | 31 (21%) | ||||
| Factor | BPD/No-PBD Group | p | OR |
|---|---|---|---|
| Gestational age (mean number of weeks) | 27.5/30.3 | <0.001 | 0.9 |
| Surfactant administration (number of children) | 69 (54%)/25 (16.6%) | <0.001 | 4.7 |
| RBC transfusion (number of children) | 108 (85%)/56 (37%) | <0.001 | 3.6 |
| Hemodynamically significant PDA | 33 (26%)/2 (1%) | 0.012 | 8.8 |
| Birth weight (mean in grams) | 1002/1394 | <0.001 | 1.2 |
| Resuscitation at birth | 63 (52%)/34 (23%) | <0.001 | 5.7 |
| Use of T-piece device at birth | 62 (49%)/34 (23%) | <0.001 | 3.8 |
| Premature rupture of membranes (mean in days) | 5.5/2.9 | 0.1 | 1.0 |
| Apgar score ≤7 at the 5th minute | 102 (80%)/107 (71%) | <0.001 | 4.3 |
| Intubation in the delivery room | 28 (22%)/7 (%) | <0.001 | 8.0 |
| Presence of intraventricular hemorrhage | 24 (19%)/9 (6%) | 0.002 | 3.3 |
| Chorionamnionitis | 35 (28%)/20 (13%) | 0.005 | 2.5 |
| Multiple pregnancy | |||
| Twin | 39 (31%)/54 (36%) | 0.193 | 0.7 |
| Triplet | 1 (1%)/11 (7%) | 0.022 | 0.1 |
| Breech presentation | 42 (33%)/33 (22%) | 0.049 | 1.8 |
| Mode of delivery (cesarean section) | 66 (52%)/112 (74%) | <0.001 | 0.4 |
| Late pneumonia | 39 (31%)/13 (9%) | <0.001 | 4.7 |
| Length of stay (mean in days) | 66.1/43 | <0.001 | |
| Late-onset sepsis | 63 (50%)/48 (32%) | 0.004 | 2.1 |
| ROP | |||
| Requiring lasertherapy | 31 (24%)/1 (1%) | <0.001 | 6.9 |
| Not requiring treatment | 19 (15%)/15 (10%) | 0.033 | 2.8 |
| NEC | 26 (20%)/13 (9%) | 0.008 | 2.7 |
| RDS | |||
| Grade 1 or 2 | 86 (68%)/96 (64%) | 0.003 | 2.8 |
| Grade 3 or 4 | 27 (21%)/12 (8%) | <0.001 | 6.9 |
| Parenteral nutrition (days) | 36.7/18.9 | <0.001 | 1.2 |
| Oxygen therapy (days) | 51/20.5 | <0.001 |
| Risk Factor | Number of Patients | p | OR (95% CI) | Score |
|---|---|---|---|---|
| Gestational age | ||||
| >29 weeks + 5 days | 119 | 1 | 0 | |
| 27 weeks + 3 days—29 weeks + 5 days | 106 | <0.001 | 13.9 (4.9–39.8) | 4 |
| ≤27 weeks + 2 | 53 | <0.001 | 46.3 (15.6–137.4) | 8 |
| Surfactant administration | ||||
| No | 183 | 1 | 0 | |
| Yes | 94 | <0.001 | 5.6 (2.2–14.4) | 2 |
| Number of red blood cell transfusions | ||||
| 0 | 115 | 1 | 0 | |
| 1 | 83 | 0.019 | 2.9 (1.2–7) | 1 |
| >1 | 80 | <0.001 | 8.7 (3.1–24.6) | 3 |
| Hemodynamically significant patent ductus arteriosus | ||||
| No | 243 | 1 | 4 | |
| Yes | 35 | 0.007 | 12.0 (2–73.2) | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jassem-Bobowicz, J.M.; Klasa-Mazurkiewicz, D.; Żawrocki, A.; Stefańska, K.; Domżalska-Popadiuk, I.; Kwiatkowski, S.; Preis, K. Prediction Model for Bronchopulmonary Dysplasia in Preterm Newborns. Children 2021, 8, 886. https://doi.org/10.3390/children8100886
Jassem-Bobowicz JM, Klasa-Mazurkiewicz D, Żawrocki A, Stefańska K, Domżalska-Popadiuk I, Kwiatkowski S, Preis K. Prediction Model for Bronchopulmonary Dysplasia in Preterm Newborns. Children. 2021; 8(10):886. https://doi.org/10.3390/children8100886
Chicago/Turabian StyleJassem-Bobowicz, Joanna Maria, Dagmara Klasa-Mazurkiewicz, Anton Żawrocki, Katarzyna Stefańska, Iwona Domżalska-Popadiuk, Sebastian Kwiatkowski, and Krzysztof Preis. 2021. "Prediction Model for Bronchopulmonary Dysplasia in Preterm Newborns" Children 8, no. 10: 886. https://doi.org/10.3390/children8100886
APA StyleJassem-Bobowicz, J. M., Klasa-Mazurkiewicz, D., Żawrocki, A., Stefańska, K., Domżalska-Popadiuk, I., Kwiatkowski, S., & Preis, K. (2021). Prediction Model for Bronchopulmonary Dysplasia in Preterm Newborns. Children, 8(10), 886. https://doi.org/10.3390/children8100886






