Distribution of Cardiometabolic Risk Factors in School-Aged Children with Excess Body Weight in the Al Ain City, United Arab Emirates: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Subjects
2.3. Anthropometric Measurements
2.4. Clinical Variables
2.5. Definition of Risk Factors
2.6. Statistical Analysis
2.7. Ethical Considerations
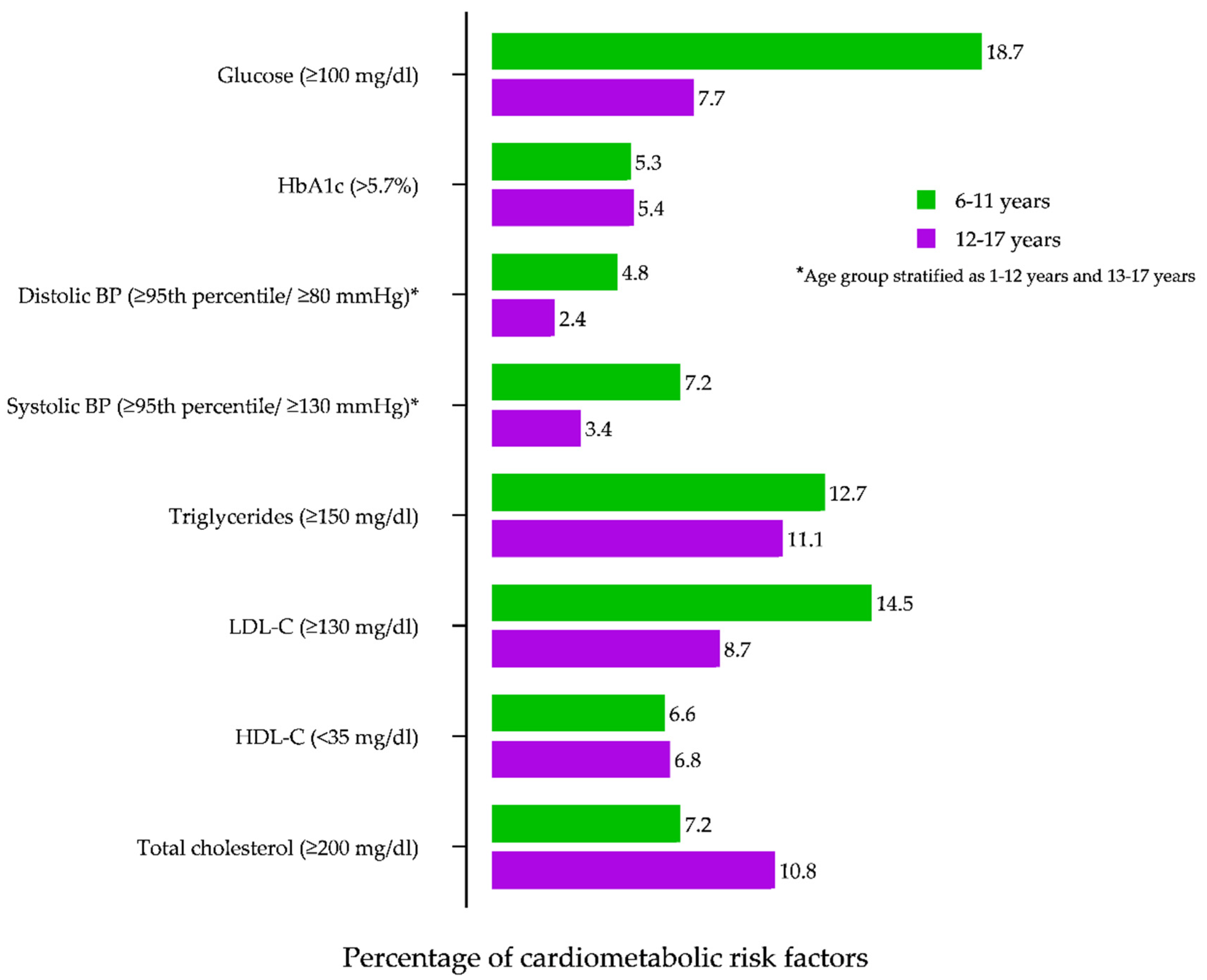
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alderman, H.; Behrman, J.R.; Glewwe, P.; Fernald, L.; Walker, S. Evidence of impact of interventions on growth and development during early and middle childhood. Child Adolesc. Health Dev. 2017, 8, 1790. [Google Scholar]
- Seo, Y.G.; Choi, M.K.; Kang, J.H.; Lee, H.J.; Jang, H.B.; Park, S.I.; Ju, Y.S.; Park, K.H. Cardiovascular disease risk factor clustering in children and adolescents: A prospective cohort study. Arch. Dis. Child. 2018, 103, 968–973. [Google Scholar] [CrossRef] [PubMed]
- Jin, B.; Lin, H.; Yuan, J.; Dong, G.; Huang, K.; Wu, W.; Chen, X.; Zhang, L.; Wang, J.; Liang, X.; et al. Abdominal adiposity and total body fat as predictors of cardiometabolic health in children and adolescents with obesity. Front. Endocrinol. 2020, 11, 579. [Google Scholar] [CrossRef] [PubMed]
- Al-Shorman, A.; AlKhatib, B.; Al-Domi, H. The association between fat mass and subclinical atherosclerosis in healthy schoolchildren. Clin. Nutr. ESPEN 2020, 37, 87–92. [Google Scholar] [CrossRef]
- Bendor, C.D.; Bardugo, A.; Pinhas-Hamiel, O.; Afek, A.; Twig, G. Cardiovascular morbidity, diabetes and cancer risk among children and adolescents with severe obesity. Cardiovasc. Diabetol. 2020, 19, 79. [Google Scholar] [CrossRef]
- Faienza, M.F.; Chiarito, M.; Molina-Molina, E.; Shanmugam, H.; Lammert, F.; Krawczyk, M.; D’Amato, G.; Portincasa, P. Childhood obesity, cardiovascular and liver health: A growing epidemic with age. World J. Pediatr. 2020, 16, 438–445. [Google Scholar] [CrossRef]
- Skinner, A.C.; Perrin, E.M.; Moss, L.A.; Skelton, J.A. Cardiometabolic risks and severity of obesity in children and young adults. N. Engl. J. Med. 2015, 373, 1307–1317. [Google Scholar] [CrossRef]
- Abduelkarem, A.R.; Sharif, S.I.; Bankessli, F.G.; Kamal, S.A.; Kulhasan, N.M.; Hamrouni, A.M. Obesity and its associated risk factors among school-aged children in Sharjah, UAE. PLoS ONE 2020, 15, e0234244. [Google Scholar] [CrossRef]
- Abdulle, A.; Al-Junaibi, A.; Nagelkerke, N. High blood pressure and its association with body weight among children and adolescents in the United Arab Emirates. PLoS ONE 2014, 9, e85129. [Google Scholar] [CrossRef]
- Kuczmarski, R.J.; Ogden, C.L.; Grummer-Strawn, L.M.; Flegal, K.M.; Guo, S.S.; Wei, R. CDC growth charts: United States. Adv. Data 2000, 314, 1–27. [Google Scholar]
- O’Donnell, A.; Buffini, M.; Kehoe, L.; Nugent, A.; Kearney, J.; Walton, J.; Flynn, A.; McNulty, B. The prevalence of overweight and obesity in Irish children between 1990 and 2019. Public Health Nutr. 2020, 23, 2512–2520. [Google Scholar] [CrossRef]
- Aryeetey, R.; Lartey, A.; Marquis, G.S.; Nti, H.; Colecraft, E.; Brown, P. Prevalence and predictors of overweight and obesity among school-aged children in urban Ghana. BMC Obes. 2017, 4, 38. [Google Scholar] [CrossRef]
- Al-Lahham, S.; Jaradat, N.; Altamimi, M.; Anabtawi, O.; Irshid, A.; AlQub, M.; Dwikat, M.; Nafaa, F.; Badran, L.; Mohareb, R.; et al. Prevalence of underweight, overweight and obesity among Palestinian school-age children and the associated risk factors: A cross sectional study. BMC Pediatr. 2019, 19, 483. [Google Scholar] [CrossRef]
- Azmatulla, S.; Garg, R. A comparison study on the prevalence of obesity and its associated factors among school children. Int. J. Health Clin. Res. 2021, 4, 21–24. Available online: https://ijhcr.com/index.php/ijhcr/article/view/693 (accessed on 26 July 2021).
- Sakaki, J.R.; Li, J.; Melough, M.M.; Ha, K.; Tamimi, R.M.; Chavarro, J.E.; Chen, M.H.; Chun, O.K. Orange juice intake and anthropometric changes in children and adolescents. Public Health Nutr. 2020, 24, 4482–4489. [Google Scholar] [CrossRef] [PubMed]
- Kavey, R.E.W.; Daniels, S.R.; Lauer, R.M.; Atkins, D.L.; Hayman, L.L.; Taubert, K. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Circulation 2003, 107, 1562–1566. [Google Scholar] [CrossRef] [PubMed]
- Lau, D.C.; Douketis, J.D.; Morrison, K.M.; Hramiak, I.M.; Sharma, A.M.; Ur, E. 2006 Canadian clinical practice guidelines on the management and prevention of obesity in adults and children [summary]. CMAJ 2007, 176, S1–S13. [Google Scholar] [CrossRef] [PubMed]
- Hayman, L.L.; Williams, C.L.; Daniels, S.R.; Steinberger, J.; Paridon, S.; Dennison, B.A.; McCrindle, B.W. Cardiovascular health promotion in the schools: A statement for health and education professionals and child health advocates from the Committee on Atherosclerosis, Hypertension, and Obesity in Youth (AHOY) of the Council on Cardiovascular Disease in the Young, American Heart Association. Circulation 2004, 110, 2266–2275. [Google Scholar] [PubMed]
- Daniels, S.R. Guidelines for Screening, Prevention, Diagnosis and Treatment of Dyslipidemia in Children and Adolescents. [Updated 2020 Jan 18]. In Endotext [Internet]; Feingold, K.R., Anawalt, B., Boyce, A., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000. Available online: https://www.ncbi.nlm.nih.gov/books/NBK395579/ (accessed on 21 July 2021).
- Spagnolo, A.; Giussani, M.; Ambruzzi, A.M.; Bianchetti, M.; Maringhini, S.; Matteucci, M.C.; Menghetti, E.; Salice, P.; Simionato, L.; Strambi, M.; et al. Focus on prevention, diagnosis and treatment of hypertension in children and adolescents. Ital. J. Pediatrics 2013, 39, 20. [Google Scholar] [CrossRef] [PubMed]
- Flynn, J.T.; Kaelber, D.C.; Baker-Smith, C.M.; Blowey, D.; Carroll, A.E.; Daniels, S.R.; de Ferranti, S.D.; Dionne, J.M.; Falkner, B.; Flinn, S.K.; et al. Clinical practice guideline for screening and management of high blood pressure in children and adolescents. Pediatrics 2017, 140, e20171904. [Google Scholar] [CrossRef]
- Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: Summary report. Pediatrics 2011, 128, S213–S256. [CrossRef]
- Kuczmarski, R.J.; Ogden, C.L.; Guo, S.S.; Grummer-Strawn, L.M.; Flegal, K.M.; Mei, Z.; Wei, R.; Curtin, L.R.; Roche, A.F.; Johnson, C.L. CDC Growth Charts for the United States: Methods and development. Vital Health Stat. 2002, 246, 1–190. [Google Scholar]
- Kabiri, L.S.; Hernandez, D.C.; Mitchell, K. Reliability, validity, and diagnostic value of a pediatric bioelectrical impedance analysis scale. Child Obes. 2015, 11, 650–655. [Google Scholar] [CrossRef]
- Fitch, K.V.; Stanley, T.L.; Looby, S.E.; Rope, A.M.; Grinspoon, S.K. Relationship between neck circumference and cardiometabolic parameters in HIV-infected and non-HIV-infected adults. Diabetes Care 2011, 34, 1026–1031. [Google Scholar] [CrossRef] [PubMed]
- Furtado, J.M.; Almeida, S.M.; Mascarenhas, P.; Ferraz, M.E.; Ferreira, J.C.; Vilanova, M.; Monteiro, M.P.; Ferraz, F.P. Anthropometric features as predictors of atherogenic dyslipidemia and cardiovascular risk in a large population of school-aged children. PLoS ONE 2018, 13, e0197922. [Google Scholar]
- Mameli, C.; Krakauer, N.Y.; Krakauer, J.C.; Bosetti, A.; Ferrari, C.M.; Moiana, N.; Schneider, L.; Borsani, B.; Genoni, T.; Zuccotti, G. The association between a body shape index and cardiovascular risk in overweight and obese children and adolescents. PLoS ONE 2018, 13, e0190426. [Google Scholar] [CrossRef]
- da Costa Teixeira, F.; Pereira, F.E.; Pereira, A.F.; Ribeiro, B.G. Overweight or obesity and abdominal obesity and their association with cardiometabolic risk factors in Brazilian schoolchildren: A cross-sectional study. Nutrition 2020, 78, 110780. [Google Scholar] [CrossRef] [PubMed]
- Kelly, A.S.; Barlow, S.E.; Rao, G.; Inge, T.H.; Hayman, L.L.; Steinberger, J.; Urbina, E.M.; Ewing, L.J.; Daniels, S.R. Severe obesity in children and adolescents: Identification, associated health risks, and treatment approaches: A scientific statement from the American Heart Association. Circulation 2013, 128, 1689–1712. [Google Scholar] [CrossRef]
- Barlow, S.E. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: Summary report. Pediatrics 2007, 120, S164–S192. [Google Scholar] [CrossRef]
- De Ferranti, S.D.; Steinberger, J.; Ameduri, R.; Baker, A.; Gooding, H.; Kelly, A.S.; Mietus-Snyder, M.; Mitsnefes, M.M.; Peterson, A.L.; St-Pierre, J.; et al. Cardiovascular risk reduction in high-risk pediatric patients: A scientific statement from the American Heart Association. Circulation 2019, 139, e603–e634. [Google Scholar] [CrossRef] [PubMed]
- Chedjou-Nono, E.; Sap, S.; Choukem, S.P.; Tetanye, I.N.; Nebongo, D.; Ndombo, O.K. Cardiometabolic profile of obese children in a sub-Saharan African setting: A cross-sectional study. BMC Pediatrics 2017, 17, 129. [Google Scholar] [CrossRef]
- Fraporti, M.I.; Adami, F.S.; Rosolen, M.D. Cardiovascular risk factors in children. Rev. Port. Cardiol. 2017, 36, 699–705. [Google Scholar] [CrossRef]
- Wang, J.; Zhu, Y.; Jing, J.; Chen, Y.; Mai, J.; Wong, S.H.; O’Reilly, J.; Ma, L. Relationship of BMI to the incidence of hypertension: A 4 years’ cohort study among children in Guangzhou, 2007-2011. BMC Public Health 2015, 15, 782. [Google Scholar] [CrossRef]
- Mokha, J.S.; Srinivasan, S.R.; Dasmahapatra, P.; Fernandez, C.; Chen, W.; Xu, J.; Berenson, G.S. Utility of waist-to-height ratio in assessing the status of central obesity and related cardiometabolic risk profile among normal weight and overweight/obese children: The Bogalusa heart study. BMC Pediatrics 2010, 10, 73. [Google Scholar] [CrossRef] [PubMed]
- Castro-Piñero, J.; Delgado-Alfonso, A.; Gracia-Marco, L.; Gómez-Martínez, S.; Esteban-Cornejo, I.; Veiga, O.L.; Marcos, A.; Segura-Jiménez, V. Neck circumference and clustered cardiovascular risk factors in children and adolescents: Cross-sectional study. BMJ Open 2017, 7, e016048. [Google Scholar] [CrossRef] [PubMed]
- Lambert, M.; Delvin, E.E.; Levy, E.; O’Loughlin, J.; Paradis, G.; Barnett, T.; McGrath, J.J. Prevalence of cardiometabolic risk factors by weight status in a population-based sample of Quebec children and adolescents. Can. J. Cardiol. 2008, 24, 575–583. [Google Scholar] [CrossRef][Green Version]
- Valerio, G.; Balsamo, A.; Baroni, M.G.; Brufani, C.; Forziato, C.; Grugni, G.; Licenziati, M.R.; Maffeis, C.; Del Giudice, E.M.; Morandi, A.; et al. Childhood obesity classification systems and cardiometabolic risk factors: A comparison of the Italian, World Health Organization and International Obesity Task Force references. Ital. J. Pediatrics 2017, 43, 19. [Google Scholar] [CrossRef] [PubMed]
- Brzeziński, M.; Metelska, P.; Myśliwiec, M.; Szlagatys-Sidorkiewicz, A. Lipid disorders in children living with overweight and obesity-large cohort study from Poland. Lipids Health Dis. 2020, 19, 47. [Google Scholar] [CrossRef] [PubMed]
- Ahmadi, N.; Seyed Mahmood, S.A.D.R.; Mohammadi, M.R.; Mirzaei, M.; Mehrparvar, A.H.; Ardekani, S.M.Y.; Sarebanhassanabadi, M.; Nilforoshan, N.; Mostafavi, S.A. Prevalence of abdominal obesity and metabolic syndrome in children and adolescents: A community based cross-sectional study. Iran J. Public Health 2020, 49, 360–368. [Google Scholar] [CrossRef]
- Magnussen, C.G.; Smith, K.J.; Juonala, M. What the long term cohort studies that began in childhood have taught us about the origins of coronary heart disease. Curr. Cardiovasc. Risk Rep. 2014, 8, 373. [Google Scholar] [CrossRef]
- McCrindle, B.W. Pathogenesis and management of dyslipidemia in obese children. In Pediatric Obesity; Humana Press: Cham, Germany, 2018; pp. 419–449. [Google Scholar]
- Aburawi, E.H.; Al Hamad, S.; Yasin, J.; Almekhaini, L.A.; Souid, A.K. Dyslipidemia, subclinical inflammation, hepatic cholestasis and endothelial dysfunction in schoolchildren with excess fat: A study from the United Arab Emirates. PLoS ONE 2019, 14, e0210316. [Google Scholar] [CrossRef] [PubMed]
- Lobstein, T.; Jackson-Leach, R. Planning for the worst: Estimates of obesity and comorbidities in school-age children in 2025. Pediatric Obes. 2016, 11, 321–325. [Google Scholar] [CrossRef] [PubMed]
| Variable | Age (Years) | No. Of Participants Evaluated | Definition of Abnormal Values |
|---|---|---|---|
| Total cholesterol | 6–17 | 966 | ≥200 mg/dL |
| HDL cholesterol | 6–17 | 966 | <35 mg/dL |
| LDL cholesterol | 6–17 | 966 | ≥130 mg/dL |
| Triglycerides | 6–17 | 966 | ≥150 mg/dL |
| Systolic BP | 1–12 | 588 | ≥95th percentile |
| 13–17 | 378 | ≥130 mmHg | |
| Diastolic BP | 1–12 | 588 | ≥95th percentile |
| 13–17 | 378 | ≥80 mmHg | |
| Glycated hemoglobin | 11–17 | 811 | >5.7% |
| Glucose | 11–17 | 811 | ≥100 mg/dL |
| Characteristics | Boys (n = 490, 50.7%) | Girls (n = 476, 49.3%) | p-Value * |
|---|---|---|---|
| Age, %, 95% CI | 0.809 | ||
| 6–11 years | 26.7 (22.8–30.9) | 26.1 (22.1–30.2) | |
| 12–17 years | 73.2 (69.1–77.1) | 73.9 (69.7–77.8) | |
| Schooling | 0.127 | ||
| 2–5 grades | 14.9 (11.9–18.3) | 19.7 (16.2–23.6) | |
| 6–9 grades | 45.7 (41.2–50.2) | 42 (37.5–46.6) | |
| 10 or above grade | 39.4 (35.0–43.8) | 38.2 (33.8–42.7) | |
| BMI category † | |||
| ≤10 years old | 0.160 | ||
| Overweight | 10.7 (5.9–17.2) | 13.7 (8.2–21.0) | |
| Obese | 6.1 (2.6–11.6) | 12.1 (6.9–19.1) | |
| 11–17 years old | 0.122 | ||
| Overweight | 14.5 (11.0–18.5) | 10.2 (7.2–13.8) | |
| Obese | 11.7 (8.5–15.4) | 9.7 (6.7–13.2) | |
| Clinical parameters (mean ± SD) | |||
| Pulse rate, beats/min | 84.0 ± 12.9 | 86.8 ± 11.8 | <0.001 |
| Blood pressure, mmHg | 113.2 ± 71.1 | 111.8 ± 72.1 | 0.293 |
| Waist circumference, cm | 70.4 ± 17.3 | 64.0 ± 13.2 | <0.001 |
| Waist/height ratio, % | 0.47 ± 0.10 | 0.44 ± 0.09 | <0.001 |
| Neck circumference, cm | 32.2 ± 6.5 | 31.0 ± 8.9 | 0.116 |
| Body fat mass, kg | 46.0 ± 27.5 | 36.4 ± 6.4 | <0.001 |
| Body fat mass, % | 12.7 ± 11.2 | 14.5 ± 10.3 | 0.115 |
| Lipid profile, mg/dL | |||
| Total cholesterol | 164.9 ± 43.4 | 153.7 ± 26.6 | 0.474 |
| Low-density lipoprotein cholesterol | 98.8 ± 23.6 | 101.0 ± 28.7 | 0.001 |
| High-density lipoprotein cholesterol | 50.2 ± 15.0 | 52.3 ±12.8 | <0.001 |
| Triglycerides | 100.5 ± 131.5 | 90.4 ± 68.5 | 0.017 |
| Apolipoprotein A, g/L | 1.5 ± 2.6 | 1.5 ± 0.3 | 0.419 |
| Apolipoprotein B, g/L | 2.1 ± 8.42 | 0.81 ± 0.29 | 0.257 |
| Lipoprotein (a), mg/dL | 59.9 ± 48.1 | 49.0 ± 45.2 | 0.480 |
| Inflammatory/endothelial function biomarkers | |||
| Interleukin 6 (g/L) | 4.1 ± 2.6 | 3.8 ± 2.1 | 0.503 |
| Intercellular adhesion molecule 1 (ICMA) ng/mL | 252.3 ± 88.2 | 263.5 ± 79.1 | 0.355 |
| Vascular cell adhesion molecule 1 (VCAM-1), ng/mL | 593.7 ± 142.3 | 586.7 ± 128.0 | 0.470 |
| Tumor necrosis factor alpha (TNF alpha), g/mL | 7.9 ± 2.4 | 5.8 ± 2.4 | 0.778 |
| Adiponectin µg/ml | 7.9 ± 4.0 | 7.2 ± 3.3 | 0.572 |
| C-reactive protein, g/L | 1.6 ± 2.4 | 1.6 ± 2.5 | 0.192 |
| Metabolic parameters | |||
| Glucose | 91.6 ± 21.9 | 90.0 ± 20.4 | 0.012 |
| Glycated hemoglobin (HbA1c), % | 5.2 ± 0.4 | 5.1 ± 0.4 | 0.097 |
| Gamma-glutamyl transferase measured in U/L | 24.2 ± 10.7 | 20.0 ± 6.6 | <0.001 |
| Risk Factor, % (95% CI) | Normal Weight (n = 748) | Excess Body Weight (n = 218) | p-Value |
|---|---|---|---|
| Total cholesterol (≥200 mg/dL) | n = 50 (6.6) | n = 22 (10.1) | 0.499 |
| Boys | 3.2 (2.0–4.7) | 4.1 (1.9–7.7) | |
| Girls | 3.4 (2.2–5.0) | 5.9 (3.2–9.9) | |
| HDL cholesterol (<35 mg/dL) | n = 38 (5) | n = 55 (25.2) | 0.039 |
| Boys | 3.3 (2.1–4.9) | 7.3 (4.2–11.6) | |
| Girls | 1.7 (0.9–2.9) | 1.8 (0.5–4.6) | |
| LDL cholesterol (≥130 mg/dL) | n = 66 (8.8) | n = 25 (11.5) | 0.263 |
| Boys | 5.0 (3.6–6.9) | 6.4 (3.5–10.5) | |
| Girls | 4.9 (3.5–6.7) | 5.0 (2.5–8.8) | |
| Triglycerides (≥150 mg/dL) | n = 47 (6.2) | n = 31 (14.2) | <0.001 |
| Boys | 3.3 (2.1–4.9) | 7.3 (4.2–11.6) | |
| Girls | 2.9 (1.8–4.4) | 6.8 (3.9–11.0) | |
| Systolic BP Age: <13 years (≥95th percentile) | n = 15 (6.8) | n = 6 (2.8) | 0.777 |
| Boys | 1.4 (0.7–2.6) | 1.3 (0.2–3.9) | |
| Girls | 0.5 (0.1–1.3) | 1.3 (0.2–3.9) | |
| Age: 13–17 years (≥ 130 mmHg) | n = 6 (3.7) | n = 10 (6.2) | 0.015 |
| Boys | 0.8 (0.3–1.7) | 3.2 (1.3–6.5) | |
| Girls | 0 | 2.7 (1.0–5.9) | |
| Diastolic BP Age: <13 years (≥95th percentile) | n = 15 (6.8) | n = 4 (1.9) | 0.686 |
| Boys | 1.3 (0.6–2.4) | 1.3 (0.2–3.9) | |
| Girls | 0.6 (0.2–1.5) | 0.4 (0.1–2.5) | |
| Age: 13–17 years (≥80 mmHg) | n = 6 (3.7) | n = 6 (2.7) | 0.287 |
| Boys | 0.8 (0.3–1.7) | 2.3 (0.7–5.2) | |
| Girls | 0 | 0.4 (0.1–2.5) | |
| Glycated hemoglobin (>5.7%) Age: 11–17 years | n = 44 (5.8) | n = 11 (5) | 0.536 |
| Boys | 3.3 (2.1–4.9) | 3.6 (1.6–7.1) | |
| Girls | 2.5 (1.5–3.9) | 1.3 (0.2–3.9) | |
| Glucose (≥100 mg/dL) Age: 11–17 years | n = 98 (13.1) | n = 31 (14.2) | 0.766 |
| Boys | 6.4 (4.7–8.4) | 10 (6.4–14.8) | |
| Girls | 6.6 (5.0–8.7) | 4.1 (1.9–7.7) |
| Variable | Boys | Girls | ||
|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Total cholesterol (≥200 mg/dL) | ||||
| Normal weight | 1 | – | 1 | – |
| Excess weight | 1.24 (0.56–2.77) | 0.590 | 2.06 (1.01–4.21) | 0.046 |
| HDL cholesterol (<35 mg/dL) | ||||
| Normal weight | 1 | – | 1 | – |
| Excess weight | 2.20 (1.12–4.31) | 0.021 | 1.11 (0.35–3.51) | 0.854 |
| LDL cholesterol (≥130 mg/dL) | ||||
| Normal weight | 1 | – | 1 | – |
| Excess weight | 1.58 (0.80–3.11) | 0.186 | 1.11 (0.54–2.27) | 0.767 |
| Triglycerides (≥150 mg/dL) | ||||
| Normal weight | 1 | – | 1 | – |
| Excess weight | 2.08 (1.06–4.10) | 0.033 | 2.74 (1.36–5.52) | 0.005 |
| Systolic BP (≥95th percentile) | ||||
| Normal weight | 1 | – | 1 | – |
| Excess weight | 1.39 (0.55–3.52) | 0.485 | 6.45 (1.83–22.72) | 0.004 |
| Diastolic BP (≥95th percentile) | ||||
| Normal weight | 1 | – | 1 | – |
| Excess weight | 1..23 (0.46–3.26) | 0.673 | 1.73 (0.38–7.77) | 0.472 |
| Glycated hemoglobin (>5.7%) | ||||
| Normal weight | 1 | – | 1 | – |
| Excess weight | 0.83 (0.37–1.86) | 0.655 | 0.67 (0.22–2.01) | 0.478 |
| Glucose (≥100 mg/dL) | ||||
| Normal weight | 1 | – | 1 | - |
| Excess weight | 1.30 (0.78–2.17) | 0.313 | 0.83 (0.46–1.49) | 0.545 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bhagavathula, A.S.; Al-Hamad, S.; Yasin, J.; Aburawi, E.H. Distribution of Cardiometabolic Risk Factors in School-Aged Children with Excess Body Weight in the Al Ain City, United Arab Emirates: A Cross-Sectional Study. Children 2021, 8, 884. https://doi.org/10.3390/children8100884
Bhagavathula AS, Al-Hamad S, Yasin J, Aburawi EH. Distribution of Cardiometabolic Risk Factors in School-Aged Children with Excess Body Weight in the Al Ain City, United Arab Emirates: A Cross-Sectional Study. Children. 2021; 8(10):884. https://doi.org/10.3390/children8100884
Chicago/Turabian StyleBhagavathula, Akshaya Srikanth, Sania Al-Hamad, Javed Yasin, and Elhadi H. Aburawi. 2021. "Distribution of Cardiometabolic Risk Factors in School-Aged Children with Excess Body Weight in the Al Ain City, United Arab Emirates: A Cross-Sectional Study" Children 8, no. 10: 884. https://doi.org/10.3390/children8100884
APA StyleBhagavathula, A. S., Al-Hamad, S., Yasin, J., & Aburawi, E. H. (2021). Distribution of Cardiometabolic Risk Factors in School-Aged Children with Excess Body Weight in the Al Ain City, United Arab Emirates: A Cross-Sectional Study. Children, 8(10), 884. https://doi.org/10.3390/children8100884








