Consequences of Low Sleep Duration in Anthropometric and Body Composition Parameters of Chilean Preschoolers
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design
2.2. Sleep Information from Parent’s Questionnaire
2.3. Anthropometric and Body Composition Measurement
2.4. Muscle Strength Measurement
2.5. Statistical Analyses
3. Results
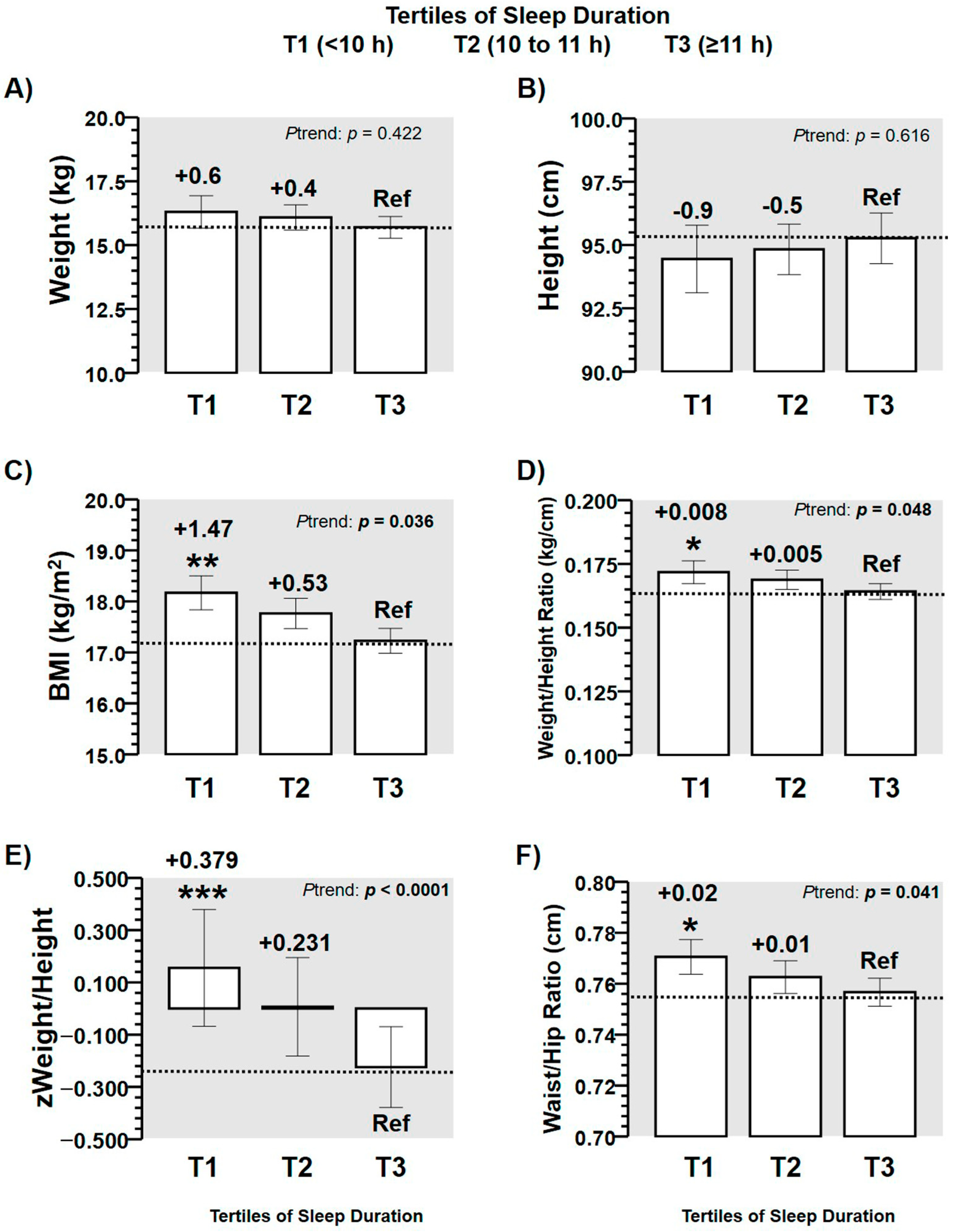
3.1. Anthropometric Outcomes by Tertiles of Sleep Duration
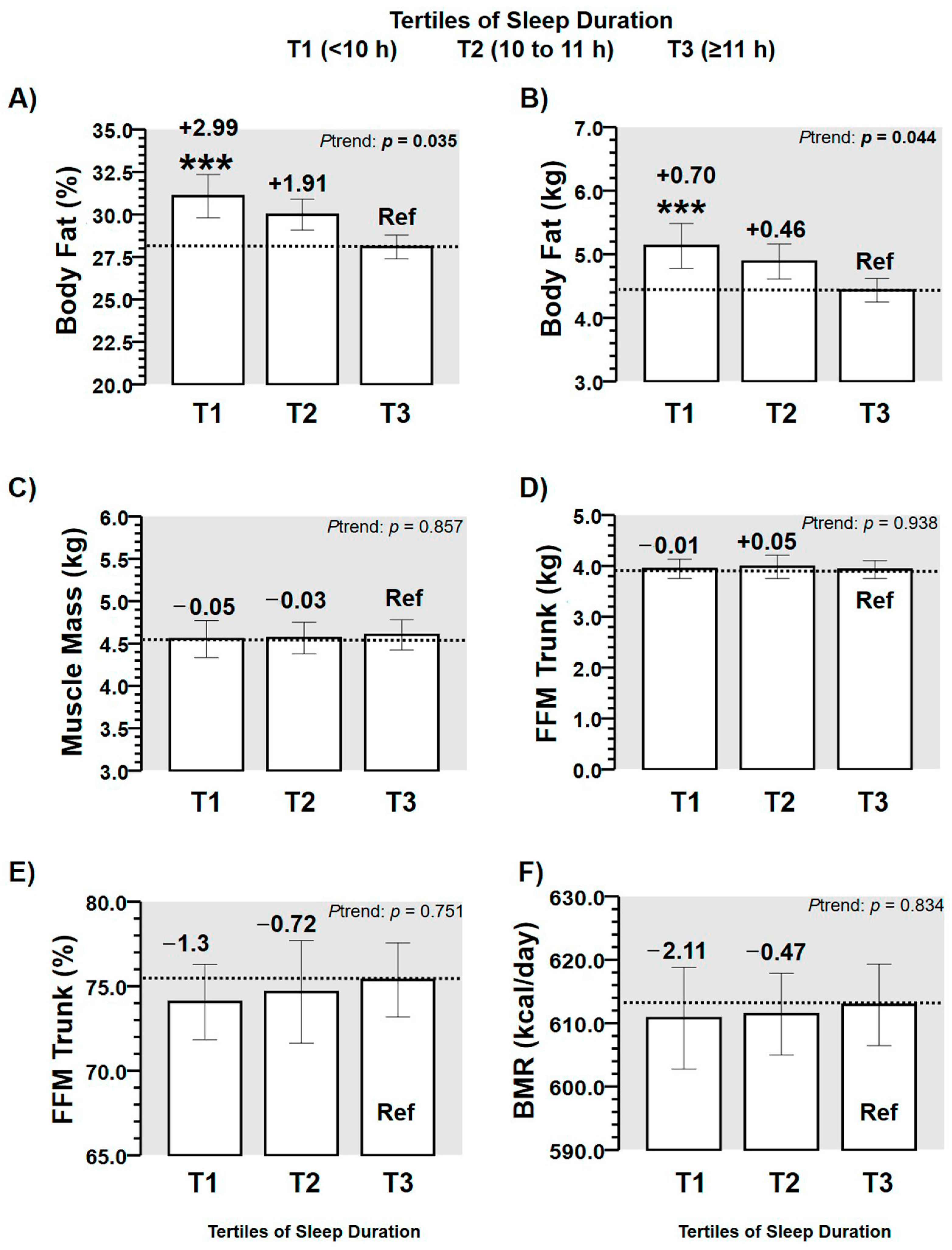
3.2. Body Composition Outcomes by Tertiles of Sleep Duration
3.3. Odds Ratios for Suffering More Altered Anthropometric Markers of Adiposity
3.4. Odds Ratios for Suffering from More Altered Body Composition Markers of Adiposity
3.5. Association of the Sleep Time with Z-Weight/Height Ratio and Body Fat Percentage
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Becerra, S.; Roldán, W.; Aguirre, M. Adaptación del cuestionario de crianza parental (pcri-m) en Canto Grande. Pensam. Psicológico 2010, 4, 135–150. [Google Scholar]
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 2014, 311, 806–814. [Google Scholar] [CrossRef] [Green Version]
- MINEDUC. Nutritional Map. Scholarships; National Board of School Aid and Scholarships, Ed.; Ministry of Education: Santiago, Chile, 2017; pp. 1–29. [Google Scholar]
- Albala, C.; Vio, F.; Kain, J.; Uauy, R. Nutrition transition in Chile: Determinants and consequences. Public Health Nutr. 2006, 5, 123–128. [Google Scholar] [CrossRef]
- Kenney, E.L.; Gortmaker, S.L. United States adolescents’ television, computer, videogame, smartphone, and tablet use: Associations with sugary drinks, sleep, physical activity, and obesity. J. Pediatrics 2017, 182, 144–149. [Google Scholar] [CrossRef] [Green Version]
- Álvarez, C.; Lucia, A.; Ramírez-Campillo, R.; Martínez-Salazar, C.; Delgado-Floody, P.; Cadore, E.L.; Alonso-Martínez, A.M.; Izquierdo, M. Low sleep time is associated with higher levels of blood pressure and fat mass in Amerindian schoolchildren. Am. J. Hum. Biol. 2019, 31, e23303. [Google Scholar] [CrossRef]
- Bayer, O.; Rosario, A.S.; Wabitsch, M.; von Kries, R. Sleep duration and obesity in children: Is the association dependent on age and choice of the outcome parameter? Sleep 2009, 32, 1183–1189. [Google Scholar] [CrossRef] [Green Version]
- Van Cauter, E.; Knutson, K.L. Sleep and the epidemic of obesity in children and adults. Eur. J. Endocrinol. 2008, 159, S59–S66. [Google Scholar] [CrossRef] [Green Version]
- Kar, S.; Khandelwal, B. Fast foods and physical inactivity are risk factors for obesity and hypertension among adolescent school children in east district of Sikkim, India. J. Nat. Sci. Biol. Med. 2015, 6, 356. [Google Scholar] [CrossRef] [Green Version]
- Li, L.; Fu, J.; Yu, X.T.; Li, G.; Xu, L.; Yin, J.; Cheng, H.; Hou, D.; Zhao, X.; Gao, S. Sleep duration and Cardiometabolic risk among Chinese school-aged children: Do Adipokines play a mediating role? Sleep 2017, 40, zsx042. [Google Scholar] [CrossRef]
- Paruthi, S.; Brooks, L.J.; D’Ambrosio, C.; Hall, W.A.; Kotagal, S.; Lloyd, R.M.; Malow, B.A.; Maski, K.; Nichols, C.; Quan, S.F. Consensus Statement of the American Academy of Sleep Medicine on the Recommended Amount of Sleep for Healthy Children: Methodology and Discussion. J. Clin. Sleep Med. 2016, 12, 1549–1561. [Google Scholar] [CrossRef]
- Lee, S.; Arslanian, S. Cardiorespiratory fitness and abdominal adiposity in youth. Eur. J. Clin. Nutr. 2007, 61, 561–565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Alvarez, C.; Flores-Opazo, M.; Mancilla, R.; Martínez-Salazar, C.; Mangiamarchi, P.; Sade-Calles, F.; Ramírez-Campillo, R. Gender differences in blood pressure and body composition in schoolchildren ascendants from Amerindian and European. Ethn. Health 2019, 1–12. [Google Scholar] [CrossRef]
- Schreck, C.J.; Fisher, B.S. Specifying the influence of family and peers on violent victimization: Extending routine activities and lifestyles theories. J. Interpers. Violence 2004, 19, 1021–1041. [Google Scholar] [CrossRef]
- Moliner-Urdiales, D.; Ruiz, J.R.; Vicente-Rodriguez, G.; Ortega, F.B.; Rey-Lopez, J.P.; España-Romero, V.; Casajús, J.A.; Molnar, D.; Widhalm, K.; Dallongeville, J. Associations of muscular and cardiorespiratory fitness with total and central body fat in adolescents: The HELENA study. Br. J. Sports Med. 2011, 45, 101–108. [Google Scholar] [CrossRef] [Green Version]
- Silva, D.A.S.; Lang, J.J.; Barnes, J.D.; Tomkinson, G.R.; Tremblay, M.S. Cardiorespiratory fitness in children: Evidence for criterion-referenced cut-points. PLoS ONE 2018, 13, e0201048. [Google Scholar] [CrossRef]
- Neubauer, S. The failing heart—An engine out of fuel. N. Engl. J. Med. 2007, 356, 1140–1151. [Google Scholar] [CrossRef] [Green Version]
- Svensson, V.; Jacobsson, J.A.; Fredriksson, R.; Danielsson, P.; Sobko, T.; Schiöth, H.B.; Marcus, C. Associations between severity of obesity in childhood and adolescence, obesity onset and parental BMI: A longitudinal cohort study. Int. J. Obes. 2011, 35, 46–52. [Google Scholar] [CrossRef] [Green Version]
- Garcia-Hermoso, A.; Oriol-Granado, X.; Correa-Bautista, J.E.; Ramírez-Vélez, R. Asociación entre la victimización por bullying y la condición física en niños y adolescentes. Int. J. Clin. Health Psychol. 2019, 19, 134–140. [Google Scholar] [CrossRef]
- Zhang, M.; Li, F.; Ma, X.F.; Li, W.T.; Jiang, R.R.; Han, R.L.; Li, G.X.; Yan-Bin, W.; Li, Z.Y.; Tian, Y.D.; et al. Identification of differentially expressed genes and pathways between intramuscular and abdominal fat-derived preadipocyte differentiation of chickens in vitro. BMC Genom. 2019, 20, 15. [Google Scholar] [CrossRef] [Green Version]
- Cole, T.J.; Lobstein, T. Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatric Obes. 2012, 7, 284–294. [Google Scholar] [CrossRef]
- Minsal. Norma Técnica para la Supervisión de Niños y Niñas de 0 a 9 Años en la Atención Primaria de Salud: Programa Nacional de Salud de la Infancia. Santiago. 2014, pp. 1–398. Available online: https://www.minsal.cl/sites/default/files/files/2014_Norma%20T%c3%a9cnica%20para%20la%20supervisi%c3%b3n%20de%20ni%c3%b1os%20y%20ni%c3%b1as%20de%200%20a%209%20en%20APS_web(1).pdf (accessed on 20 December 2020).
- Garcia-Hermoso, A.; Cofre-Bolados, C.; Andrade-Schnettler, R.; Ceballos-Ceballos, R.; Fernández-Vergara, O.; Vegas-Heredia, E.D.; Ramírez-Vélez, R.; Izquierdo, M. Normative Reference Values for Handgrip Strength in Chilean Children at 8–12 Years Old Using the Empirical Distribution and the Lambda, Mu, and Sigma Statistical Methods. J. Strength Cond. Res. 2018, 35, 260–266. [Google Scholar] [CrossRef]
- Wang, J.; Adab, P.; Liu, W.; Chen, Y.; Li, B.; Lin, R.; Liu, W.; Cheng, K.K.; Pallan, M. Prevalence of adiposity and its association with sleep duration, quality, and timing among 9–12-year-old children in Guangzhou, China. J. Epidemiol. 2017, 27, 531–537. [Google Scholar] [CrossRef]
- Garaulet, M.; Ortega, F.; Ruiz, J.; Rey-Lopez, J.; Beghin, L.; Manios, Y.; Cuenca-Garcia, M.; Plada, M.; Diethelm, K.; Kafatos, A. Short sleep duration is associated with increased obesity markers in European adolescents: Effect of physical activity and dietary habits. The HELENA study. Int. J. Obes. 2011, 35, 1308–1317. [Google Scholar] [CrossRef] [Green Version]
- Vargas, J.E.; Vásquez, S.M.; Villar, J.C.; Herrera, V.M. Relación entre los atributos del sueño y el cambio en la presión arterial. Análisis de la cohorte CHICAMOCHA. Rev. Colomb. Cardiol. 2019, 26, 198–204. [Google Scholar] [CrossRef]
- Carson, V.; Tremblay, M.S.; Chaput, J.-P.; Chastin, S.F. Associations between sleep duration, sedentary time, physical activity, and health indicators among Canadian children and youth using compositional analyses. Appl. Physiol. Nutr. Metab. 2016, 41, S294–S302. [Google Scholar] [CrossRef] [Green Version]
- Baird, J.; Hill, C.M.; Harvey, N.C.; Crozier, S.; Robinson, S.M.; Godfrey, K.M.; Cooper, C.; Inskip, H.; Group, S.S. Duration of sleep at 3 years of age is associated with fat and fat-free mass at 4 years of age: The Southampton Women's Survey. J. Sleep Res. 2016, 25, 412–418. [Google Scholar] [CrossRef] [Green Version]
- Esteban, R.F.C.; Caycho-Rodríguez, T.; Arias, S.A.S.; Guerra, R.M.R.; Vilchez, C.C.; Orci, K.C.; Rivera, J.P. Efectividad de intervención basada en modelo de Nola Pender en promoción de estilos de vida saludables de universitarios peruanos. Rev. Cuba. Enfermería 2019, 35, 1–10. [Google Scholar]
- Rudnicka, A.R.; Nightingale, C.M.; Donin, A.S.; Sattar, N.; Cook, D.G.; Whincup, P.H.; Owen, C.G. Sleep duration and risk of type 2 diabetes. Pediatrics 2017, 140, e20170338. [Google Scholar] [CrossRef] [Green Version]
- Edvardsson, K.; Ivarsson, A.; Eurenius, E.; Garvare, R.; Nyström, M.E.; Small, R.; Mogren, I. Giving offspring a healthy start: parents' experiences of health promotion and lifestyle change during pregnancy and early parenthood. BMC Public Health 2011, 11, 936. [Google Scholar] [CrossRef] [Green Version]
- West, F.; Sanders, M.R.; Cleghorn, G.J.; Davies, P.S. Randomised clinical trial of a family-based lifestyle intervention for childhood obesity involving parents as the exclusive agents of change. Behav. Res. Ther. 2010, 48, 1170–1179. [Google Scholar] [CrossRef]
- Katzmarzyk, P.; Janssen, I.; Ardern, C. Physical inactivity, excess adiposity and premature mortality. Obes. Rev. 2003, 4, 257–290. [Google Scholar] [CrossRef] [PubMed]
- García Rodríguez, K. Influencia de los factores psicológicos y familiares en el mantenimiento de la obesidad infantil. Rev. Mex. Trastor. Aliment. 2018, 9, 221–237. [Google Scholar] [CrossRef]
- Chaput, J.-P.; Colley, R.C.; Aubert, S.; Carson, V.; Janssen, I.; Roberts, K.C.; Tremblay, M.S. Proportion of preschool-aged children meeting the Canadian 24-Hour Movement Guidelines and associations with adiposity: Results from the Canadian Health Measures Survey. BMC Public Health 2017, 17, 829. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Outcomes | Tertiles of Sleep Time | |||
|---|---|---|---|---|
| T1 (< 10 h) Mean (95% CI) | T2 (10 to 11 h) Mean (95% CI) | T3 (≥ 11 h) Mean (95% CI) | p-Trend | |
| (n = ) | 34 | 35 | 30 | |
| Parent´s information | ||||
| Mother Age (years) | 32.0 (27.3, 36.6) | 32.5 (29.8, 35.1) | 32.1 (29.8, 34.5) | p = 0.955 |
| Father Age (years) | 33.1 (27.8, 38.4) | 36.3 (32.4, 40.3) | 34.3 (31.8, 36.9) | p = 0.797 |
| Familiar mean income (Chilean pesos $) | ||||
| <350,000 | 9 (40.9%) | 8 (36.4%) | 5 (22.7%) | p = 0.719 |
| 350,000–500,000 | 1 (5.6%) | 9 (50.0%) | 8 (44.4%) | |
| 500,000–1,000,000 | 3 (14.3%) | 9 (42.9%) | 9 (42.9%) | |
| >1,000,000 | 6 (31.6%) | 7 (36.8%) | 6 (31.6%) | |
| Mother Education | ||||
| Primary/secondary | 10 (52.6%) | 12 (34.3%) | 10 (33.3%) | p = 0.214 |
| Technical/University | 8 (42.1%) | 21 (60%) | 20 (66.7%) | |
| Father Education | ||||
| Primary/secondary | 10 (52.6%) | 12 (34.3%) | 12 (40.0%) | p = 0.090 |
| Technical/University | 6 (31.6%) | 18 (51.4%) | 18 (60%) | |
| Prevalence of active’s play with children at home | ||||
| Yes, n = / (%) | 18 (94.7%) | 31 (88.6%) | 25 (83.3%) | p = 0.454 |
| No, n = / (%) | 1 (5.3%) | 4 (11.4%) | 5 (16.7%) | |
| Prevalence for Mother´s or Father’s play more with children at home | ||||
| Mother, n = / (%) | 15 (78.9%) | 24 (68.6%) | 26 (86.7%) | p = 0.244 |
| Father, n = / (%) | 4 (21.1%) | 11 (31.4% | 4 (13.3%) | |
| Preschoolers information | ||||
| Sex, Girls | 11 (57.9%) | 22 (62.9%) | 18 (60.0%) | |
| Age (years) | 3.0 (2.7, 3.2) | 3.1 (2.9, 3.3) | 3.2 (2.9, 3.4) | p = 0.292 |
| Anthropometric | ||||
| Body Fat, kg/HGS, kg Ratio | 0.561 (4.059, 0.662) | 0.555 (0.430, 0.670) | 0.601 (0.498, 0.701) | p = 0.590 |
| Body Fat, %/HGS, kg Ratio | 0.713 (0.576, 0.850) | 0.652 (0.535, 0.769) | 0.664 (0.558, 0.770) | p = 0.646 |
| Muscle Mass, kg/Body Fat, kg Ratio | 0.944 (0.807, 1.081) | 0.989 (0.833, 1.095) | 1.061 (0.982, 1.140) | p = 0.132 |
| Nutritional status | ||||
| Normal weight, n = / (%) | 5 (26.3%) | 13 (37.1%) | 15 (50.0%) | p = 0.716 |
| Overweight, n = / (%) | 7 (37.8%) | 12 (34.3%) | 12 (40.0%) | |
| Obese, n = / (%) | 7 (37.8%) | 10 (28.6%) | 3 (10.0%) | |
| Muscle strength, kg | ||||
| HGS-ra (kg) | 2.9 (2.1, 3.6) | 2.6 (2.1, 3.1) | 3.0 (2.3, 3.6) | p = 0.696 |
| HGS-la (kg) | 2.8 (2.1, 3.4) | 2.5 (2.0, 3.0) | 2.6 (2.3, 2.9) | p = 0.760 |
| Mean HGS (kg) | 2.8 (2.2, 3.4) | 2.5 (2.0, 3.0) | 2.6 (2.1, 3.2) | p = 0.789 |
| Z Weight/Height Ratio | Body Fat % | |||||
|---|---|---|---|---|---|---|
| Predicted % by R2 | β (95% CI) | p-Value | Predicted % by R2 | β (95% CI) | p-Value | |
| Model 1, Sleep time | 0.008 (0.8%) | −0.092 (−0.345, 0.141) | p = 0.406 | 0.028 (2.8%) | −0.168 (−2.157, 0.273) | p < 0.0001 |
| Model 2, Sleep time, age | 0.203 (20.3%) | −0.154 (−0.393, 0.051) | p < 0.0001 | 0.029 (2.9%) | −0.164 (−2.152, 0.317) | p < 0.0001 |
| Model 3, Sleep time, age, gender | 0.220 (22.0%) | −0.154 (−0.392, 0.049) | p < 0.0001 | 0.072 (7.2%) | −0.163 (−2.129, 0.301) | p < 0.0001 |
| Model 4, Sleep time, age, gender, handgrip strength | 0.288 (28.8%) | −0.134 (−0.362, 0.064) | p < 0.0001 | 0.083 (8.3%) | −0.155 (−2.088, 0.350) | p < 0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alvarez, C.; Paredes-Arévalo, L.; Obando, I.; Leal, M.; Avila, Y.; Sadarangani, K.P.; Delgado-Floody, P.; Alonso-Martínez, A.M.; Izquierdo, M. Consequences of Low Sleep Duration in Anthropometric and Body Composition Parameters of Chilean Preschoolers. Children 2021, 8, 8. https://doi.org/10.3390/children8010008
Alvarez C, Paredes-Arévalo L, Obando I, Leal M, Avila Y, Sadarangani KP, Delgado-Floody P, Alonso-Martínez AM, Izquierdo M. Consequences of Low Sleep Duration in Anthropometric and Body Composition Parameters of Chilean Preschoolers. Children. 2021; 8(1):8. https://doi.org/10.3390/children8010008
Chicago/Turabian StyleAlvarez, Cristian, Lorena Paredes-Arévalo, Isabel Obando, Marlys Leal, Yennifer Avila, Kabir P. Sadarangani, Pedro Delgado-Floody, Alicia M. Alonso-Martínez, and Mikel Izquierdo. 2021. "Consequences of Low Sleep Duration in Anthropometric and Body Composition Parameters of Chilean Preschoolers" Children 8, no. 1: 8. https://doi.org/10.3390/children8010008
APA StyleAlvarez, C., Paredes-Arévalo, L., Obando, I., Leal, M., Avila, Y., Sadarangani, K. P., Delgado-Floody, P., Alonso-Martínez, A. M., & Izquierdo, M. (2021). Consequences of Low Sleep Duration in Anthropometric and Body Composition Parameters of Chilean Preschoolers. Children, 8(1), 8. https://doi.org/10.3390/children8010008