Perceived Barriers and Facilitators for Bedtime Routines in Families with Young Children
Abstract
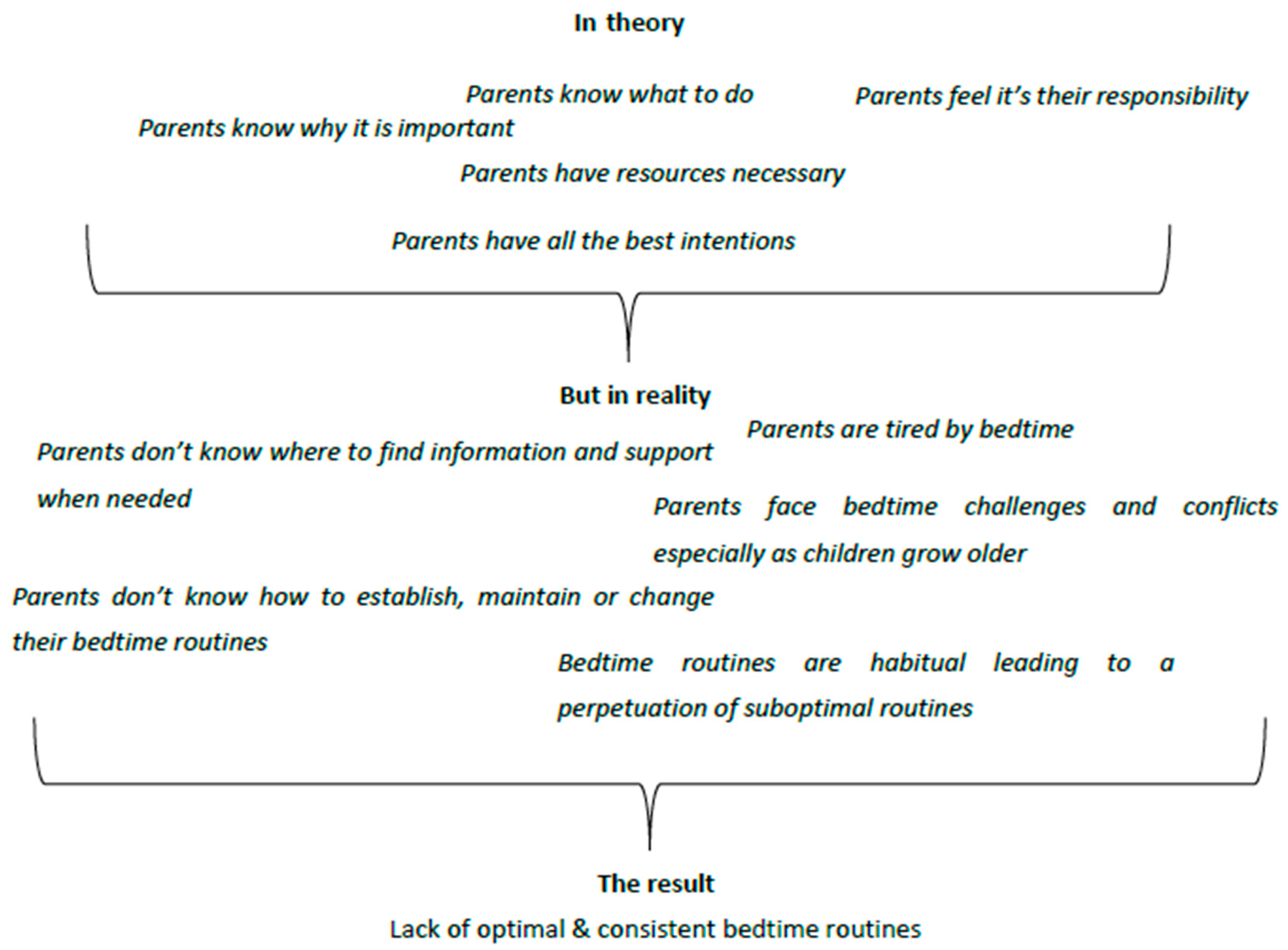
1. Introduction
Objective
2. Participants and Methods
2.1. Participants and Recruitment
2.2. Data Collection
2.3. Data Analysis
3. Results
3.1. Sample Characteristics
3.2. Inter-Rater Reliability
3.3. Barriers and Facilitators by TDF Domain
3.3.1. Knowledge
“Reading that the school asks us to do. Spellings and settling them down in a relaxed environment before bedtime and teaching them that it’s healthy to look after their teeth and that is one of the bedtime routines that, as they get older, that they should be doing.”(QI021)
“No. It would have been good to get some advice, but no one really said anything about routines when the children were born.”(QI012)
“If somebody could have told me how to get my kids to sleep that probably would have been really, really helpful.”(QI005)
3.3.2. Skills
“So when they’re doing their teeth, we have, like, one of their favourite songs will play … so they’ll find a song that’s three and a half minutes long, so they’ve got to brush their teeth while that song is playing, so they’ll dance while they’re brushing their teeth and then once that songs finished, their teeth are done.”(QI004)
3.3.3. Social/Professional Role/Identity
“I suppose what I’m doing as a parent is trying to set them up in good habits for the rest of their lives, because the stuff that they do before they go to bed is the stuff that I do before I go to bed.”(QI025)
3.3.4. Beliefs about Capabilities
“Difficult but it’s something that we’re all used to, and they’ve done since they were younger and it’s something, like I say, that I’ve always been consistent with but yes, it is difficult.”(QI031)
3.3.5. Optimism
“I don’t feel anxious about it really, I think... I haven’t really thought about it really. I don’t know.”(QI005)
3.3.6. Intentions
“Yes, I mean 100 percent, 101 percent really and in terms of that, it’s maintaining and being consistent and that can get tiring but that’s the length that I personally am happy to go to for them.”(QI011)
3.3.7. Beliefs about Consequences
“If you’re brushing your teeth so this will give you a future with nothing a problem with your teeth and everything. But if you do brush correctly, in the correct way.”(QI023)
3.3.8. Reinforcement
“It is a nice feeling, if it’s all smooth and everybody goes to bed happy and so on and you don’t feel like you’re on your last nerve, then, yes, of course it’s a nice feeling, because then you look at these two sleeping angels and think that’s lovely.”(QI005)
3.3.9. Goals
“You’re all busy during the day, the children are at school, you’re at work, so that is a really nice time to talk to the children and find out what’s been going on in their day and yes, they play with each other, it’s their time as well to have a bit of fun with each other.”(QI011)
3.3.10. Emotions
“Calm, quite fine, like I say because we’ve stuck to the same routine. It’s not a chore; it’s a pleasurable thing to do.”(QI008)
3.3.11. Memory, Attention, and Decision Process
“God, yes, it’s hard, well it can be just because I work full time and by the end of the day I’m shattered so, yeah, because they’re busy and they’re five and three.”(QI023)
3.3.12. Environment and Resources
“Well the children have to share a room which makes things more difficult. It would have been nice to be able to have separate rooms for them but that’s not a possibility unfortunately.”(QI012)
3.3.13. Social Influences
“Yes, they always resist, every night they resist at bedtime and obviously at the weekends, I’m a little bit more lenient but no I think they enjoy the bedtime routine.”(QI011)
3.3.14. Behavioural Regulation
“Just in my head and keeping track of how it works well for the children and varying it upon that.”(QI007)
3.4. Overarching Themes
3.5. Barriers and Facilitators
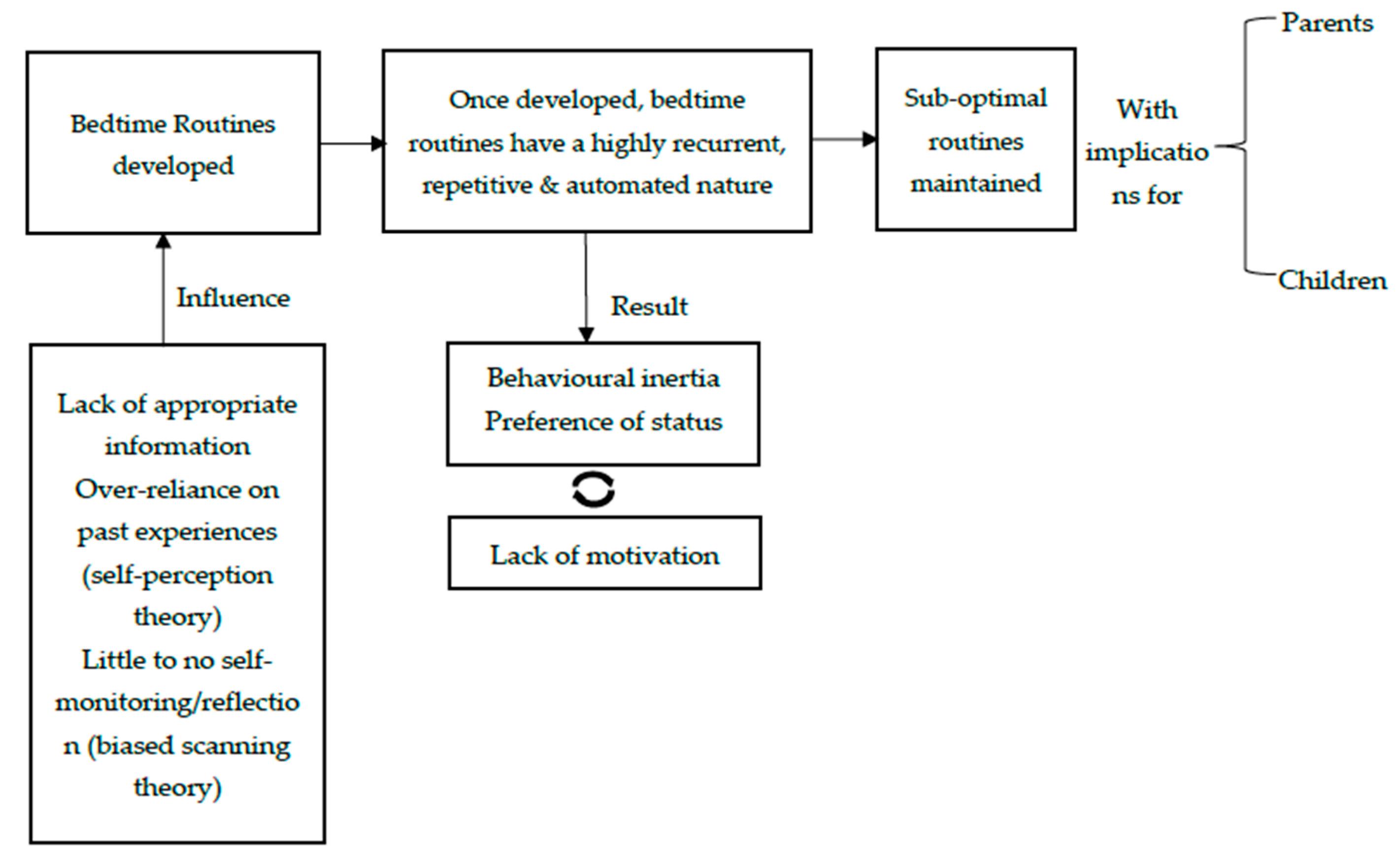
4. Discussion
5. Limitations
6. Implications for Further Research
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Interview Schedule Based on the Theoretical Domains Framework
- 0
- Introduction0.1. Briefly discuss the scope of this interview as an additional source of information in trying to get a better understanding of bedtime routines in families with young children. Discuss overall set up, including time, audio recordings, etc.
- 1
- Bedtime routines overview1.1. Can you describe your typical bedtime routine? What time does it start and end? What does it involve? In what order? Who’s involved?
- 2
- General knowledge and skills2.1. (KNOWLEDGE) How do you think a good bedtime routine looks like? What would be involved?2.2. (KNOWLEDGE) You’ve mentioned X, Y, and Z as things that would be involved in a ‘good’ bedtime routine—why do you think they’re important/why do they matter?2.3. (KNOWLEDGE) Are you aware of guidelines/recommendations relating to bedtime routines?If yes, what do they usually include? If yes, who/how did you come across those guidelines/recommendations? (Hint: midwives, health visitors, internet, etc.)Following reply to Qs.1 and 2.1/2.2/2.3, provide a quick definition of what an optimal bedtime routine should include and use a visual aid to quickly refer to with regards to all four main components (tooth brushing, book reading, diet, and use of electronics).2.4. (SKILLS) What skills do you think you would need in order to be able to do things involved in a good bedtime routine? (point to prompt card)2.5. (SKILLS) Which of these skills do you think you have? Are there ones you could do with improving?2.6. (SOCIAL IDENTITY) Who is responsible for bedtime routines in your view? (Hint: me as parent, parents or others?)2.7. (SOCIAL IDENTITY) Do you think other parents have good bedtime routines? Are they like you?2.8. (SOCIAL INFLUENCES) (If someone’s involved) How do you feel about your partner’s/husband’s/wife’s etc. involvement in your bedtime routines? Do they help or hinder your activities? (If no one’s involved) Do you wish there was someone to help you with your bedtime routines? In what way someone else could be helpful for you during your bedtime routines?2.9. (SOCIAL INFLUENCES) What do your friends/family think about your bedtime routine? Do you care what they think?2.10. (SOCIAL INFLUENCES) What do your kids think about the different bits of this good bedtime routine (Hint: prompt card)? How important is it to you what they think about it?
- 3
- Current situation3.1. (BELIEFS CAPABILITIES) How easy or difficult is it for you to do your bedtime routine every night? Can you manage even when things are difficult?3.2. (BELIEFS CAPABILITIES) How confident are you in completing your bedtime routine every night? (If confidence low) What would make you feel more confident? (If confidence high) What gives you confidence?3.3. (EMOTIONS) How do you feel when you do manage to do all the things involved in your bedtime routine? What about when you don’t? What words describe how you typically feel during your bedtime routines (i.e., stressed, calm, happy, sad)?3.4. (EMOTIONS) How does the way you feel as it’s coming up to bedtime influence whether or not you do the things involved in a good routine?3.5. (MEMORY, ATTENTION & DECISION PROCESS) Are these different things (prompt card) things you do routinely, without thinking? Do they happen at a set time and in the same way every night or do you actively have to remember to do them?3.6. (MEMORY, ATTENTION & DECISION PROCESS) Do your routines change between school days and weekends? If so, how are they different? Do you still complete all of your activities?3.7. (MEMORY, ATTENTION & DECISION PROCESS) When you’re tired or have a lot on your mind, do you try and complete all activities? If not, how do you decide which activities to leave out?3.8. (ENVIRONMENT-RESOURCES) (If employed) Do you believe that your work affects your bedtime routines? If yes, in what way?3.9. (ENVIRONMENT-RESOURCES) Are there things about your home (e.g., where the bedrooms are, need to share rooms, noise, etc.) that make your bedtime routines easier or harder?3.10. (ENVIRONMENT-RESOURCES) Do you have access to the things you need to do the 4 things outlined here (prompt card), e.g., selection of books, toothbrushes, water/milk, etc.? If not, in what way?3.11. (REINFORCEMENT) When you have a good bedtime routine, what happens and how do you feel straight afterwards? What were the immediate benefits?3.12. (REINFORCEMENT) When you have a bad bedtime routine, what happens and how do you feel straight afterwards? What were the immediate consequences?3.13. (GOALS) What is/are your end goal(s) when starting your bedtime routines on a nightly basis?3.14. (GOALS) Compared to other things you need/want to get done, how important is it that you do all the things listed as part of your bedtime routine?3.15. (BEHAVIOUR REGULATION) Do you monitor your bedtime routines in any way? If yes, how do you do it? If not, do you believe that it might be useful to monitor them?3.16. (BEHAVIOUR REGULATION) (If monitor bedtime routines) What do you do when you notice that your bedtime routines are not as good as they used to be? Do you take any actions? If yes, what?
- 4
- Looking ahead4.1. (BELIEFS CONSEQUENCES) Looking ahead in the future, what do you think will happen if you have a good bedtime routine in place? For you, your child, your family or in general? What will happen if you don’t? Do some of these things (prompt card) matter more than other for the future?4.2. (BELIEFS CONSEQUENCES) Do the future benefits outweigh the costs? How?4.3. (OPTIMISM) Looking ahead, how do you feel about your upcoming bedtime routines for the days, weeks, and years to come?4.4. (OPTIMISM) Do you feel that regardless of what happens day to day, things will turn out fine in the end?4.5. (INTENTIONS) Do you want to have a good bedtime routine? If yes, to what extent?4.6. Do you feel ready and able to make any changes that are necessary to your existing bedtime routine?
References
- Fiese, B.H. Routines of daily living and rituals in family life: A glimpse at stability and change during the early child-raising years. Zero Three 2002, 22, 10–13. [Google Scholar]
- Mindell, J.A.; Williamson, A.A. Benefits of a bedtime routine in young children: Sleep, development, and beyond. Sleep Med. Rev. 2018, 40, 93–108. [Google Scholar] [CrossRef] [PubMed]
- Hale, L.; Berger, L.M.; LeBourgeois, M.K.; Brooks-Gunn, J. Social and Demographic Predictors of Preschoolers Bedtime Routines. J. Dev. Behav. Pediatr. 2009, 30, 394–402. [Google Scholar] [CrossRef] [PubMed]
- Kelly, Y.; Kelly, J.; Sacker, A. Time for bed: Associations with cognitive performance in 7-year-old children: A longitudinal population-based study. J. Epidemiol. Community Health 2013, 67, 926–931. [Google Scholar] [CrossRef] [PubMed]
- Kitsaras, G.; Goodwin, M.; Allan, J.; Kelly, M.; Pretty, I. Bedtime routines child wellbeing & development. BMC Public Health 2018, 18, 1–12. [Google Scholar] [CrossRef]
- Levine, R. Caries experience and bedtime consumption of sugar-sweetened food and drinks—A survey of 600 children. Commun. Dent. Health 2001, 18, 228–231. [Google Scholar]
- Goodwin, M.; Patel, D.K.; Vyas, A.; Khan, A.J.; McGrady, M.G.; Boothman, N.; Pretty, I.A. Sugar before bed: A simple dietary risk factor for caries experience. Commun. Dent. Health 2017, 34, 8–13. [Google Scholar]
- High, P.; Hopmann, M.; Lagasse, L.; Linn, H. Evaluation of a Clinic-Based Program to Promote Book Sharing and Bedtime Routines among Low-Income Urban Families with Young Children. Arch. Pediatr. Adolesc. Med. 1998, 152, 459–465. [Google Scholar] [CrossRef]
- Lee, S.; Hale, L.; Chang, A.-M.; Nahmod, N.G.; Master, L.; Berger, L.M.; Buxton, O.M. Longitudinal associations of childhood bedtime and sleep routines with adolescent body mass index. Sleep 2019, 42. [Google Scholar] [CrossRef]
- Mindell, J.A.; Telofski, L.S.; Wiegand, B.; Kurtz, E.S. A Nightly Bedtime Routine: Impact on Sleep in Young Children and Maternal Mood. Sleep 2009, 32, 599–606. [Google Scholar] [CrossRef]
- Michie, S.; Van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, A.C.; Arruda, C.A.M.; Machado, M.M.T.; De Andrade, G.P.; Greaney, M.L. Exploring Brazilian Immigrant Mothers’ Beliefs, Attitudes, and Practices Related to Their Preschool-Age Children’s Sleep and Bedtime Routines: A Qualitative Study Conducted in the United States. Int. J. Environ. Res. Public Health 2018, 15, 1923. [Google Scholar] [CrossRef] [PubMed]
- Albarracin, D.; Wyer, R.S., Jr. The cognitive impact of past behavior: Influences on beliefs, attitudes, and future behavioral decisions. J. Personal. Soc. Psychol. 2000, 79, 5. [Google Scholar] [CrossRef]
- Bentler, P.M.; Speckart, G. Attitudes “cause” behaviors: A structural equation analysis. J. Personal. Soc. Psychol. 1981, 40, 226. [Google Scholar] [CrossRef]
- Ouellette, J.A.; Wood, W. Habit and intention in everyday life: The multiple processes by which past behavior predicts future behavior. Psychol. Bull. 1998, 124, 54. [Google Scholar] [CrossRef]
- Skinner, B.F. Science and Human Behavior (Issue 92904); Simon and Schuster: New York, NY, USA, 1953. [Google Scholar]
- Triandis, H.C. Values, attitudes, and interpersonal behavior. In Nebraska Symposium of Motivation, 1980: Cognitive Processes; Howe, H.E., Jr., Page, M., Eds.; University of Nebraska Press: Lincoln, NE, USA, 1980; Volume 27, pp. 195–259. [Google Scholar]
- Calder, B.J.; Staw, B.M. Self-perception of intrinsic and extrinsic motivation. J. Personal. Soc. Psychol. 1975, 31, 599–605. [Google Scholar] [CrossRef]
- Valkenburg, P.M. Understanding Self-Effects in Social Media. Hum. Commun. Res. 2017, 43, 477–490. [Google Scholar] [CrossRef]
- Cooklin, A.R.; Giallo, R.; Rose, N. Parental fatigue and parenting practices during early childhood: An Australian community survey. Child Care Health Dev. 2011, 38, 654–664. [Google Scholar] [CrossRef]
- Giallo, R.; Seymour, M.; Dunning, M.; Cooklin, A.; Loutzenhiser, L.; McAuslan, P. Factors associated with the course of maternal fatigue across the early postpartum period. J. Reprod. Infant Psychol. 2015, 33, 528–544. [Google Scholar] [CrossRef]
- McQueen, A.; Mander, R. Tiredness and fatigue in the postnatal period. J. Adv. Nurs. 2003, 42, 463–469. [Google Scholar] [CrossRef]
- Jones, T.L.; Prinz, R.J. Potential roles of parental self-efficacy in parent and child adjustment: A review. Clin. Psychol. Rev. 2005, 25, 341–363. [Google Scholar] [CrossRef] [PubMed]
- Madrian, B.C.; Shea, D.F. The power of suggestion: Inertia in 401 (k) participation and savings behavior. Q. J. Econ. 2001, 116, 1149–1187. [Google Scholar] [CrossRef]
- Nicolle, A.; Fleming, S.M.; Bach, D.R.; Driver, J.; Dolan, R.J. A Regret-Induced Status Quo Bias. J. Neurosci. 2011, 31, 3320–3327. [Google Scholar] [CrossRef] [PubMed]
- Samuelson, W.; Zeckhauser, R. Status Quo Bias in Decision Making. J. Risk Uncertain. 1988, 1, 7–59. [Google Scholar] [CrossRef]
- Meltzer, L.J.; Plaufcan, M.R.; Thomas, J.H.; Mindell, J.A. Sleep Problems and Sleep Disorders in Pediatric Primary Care: Treatment Recommendations, Persistence, and Health Care Utilization. J. Clin. Sleep Med. 2014, 10, 421–426. [Google Scholar] [CrossRef]
- Turnbull, K.; Reid, G.J.; Morton, J.B. Behavioral Sleep Problems and their Potential Impact on Developing Executive Function in Children. Sleep 2013, 36, 1077–1084. [Google Scholar] [CrossRef]
- Mindell, J.A.; Sadeh, A.; Kohyama, J.; How, T.H. Parental behaviors and sleep outcomes in infants and toddlers: A cross-cultural comparison. Sleep Med. 2010, 11, 393–399. [Google Scholar] [CrossRef]
- Sadeh, A.; Tikotzky, L.; Scher, A. Parenting and infant sleep. Sleep Med. Rev. 2010, 14, 89–96. [Google Scholar] [CrossRef]
| ID | Consistency | Tooth Brushing | Avoiding Snacks/Food | Use of Electronics | Reading Before | Winding Down |
|---|---|---|---|---|---|---|
| QI001 | X | X | X | X | ||
| QI002 | X | X | X | X | X | X |
| QI003 | X | X | X | |||
| QI004 | X | X | ||||
| QI005 | X | X | X | X | X | |
| QI006 | X | X | X | X | ||
| QI007 | X | X | X | X | X | |
| QI008 | X | X | X | X | X | X |
| QI009 | X | X | X | X | X | X |
| QI010 | X | X | X | X | ||
| QI011 | X | X | X | X | X | |
| QI012 | X | X | X | X | X | |
| QI013 | X | X | X | X | ||
| QI014 | X | X | X | X | X | X |
| QI015 | X | X | X | |||
| QI016 | X | X | ||||
| QI017 | X | X | X | X | X | |
| QI018 | X | X | X | X | ||
| QI019 | X | X | X | X | X | |
| QI020 | X | X | X | X | X | X |
| QI021 | X | X | X | X | X | X |
| QI022 | X | X | X | X | ||
| QI023 | X | X | X | X | X | |
| QI024 | X | X | X | X | X | |
| QI025 | X | X | X | X | X | X |
| QI026 | X | X | X | X | ||
| QI027 | X | X | X | X | X | |
| QI028 | X | X | X | X | X | |
| QI029 | X | X | X | X | ||
| QI030 | X | X | X | X | X | X |
| QI031 | X | X | X | |||
| QI032 | X | X | X | X | X | X |
| Barrier | Facilitator |
|---|---|
‘Knowledge’ and ‘skills development’ were two of the most important barriers identified:
| Beliefs about consequences and the realization from many parents that bedtime routines can have a long-term effect to their children’s overall wellbeing and development was an important facilitator. Awareness of consequences when combined with clearly stated intentions and strong beliefs about the parental role and responsibility can be a powerful combination that can ultimately help parents to achieve and maintain optimal bedtime routines. |
| ‘Social influences’ and ‘intergroup conflicts’—Within the family unit the interactions between parents and children were another important barrier for implementing good bedtime routines. The older the children, the more exposed to peer pressure and outside points of view resulting in higher frequency of arguments and conflicts within the family unit and at bedtime. | Social role was an important facilitator for parents who wanted to provide their children with the best chances in life through, in part, their bedtime routines. Parents expressed deep and strong beliefs about the importance of their role in their children’s overall development and future wellbeing. |
| ‘Tiredness’ or “cognitive overload” was a significant barrier for achieving good bedtime routines especially in families with more than one child or families where the mother, as the one who’s primarily involved in bedtime routines, was working full-time. | Environment and access to resources were both important facilitators for establishing and maintaining optimal bedtime routines since almost all families did not consider them as an issue. Also, all families mentioned that they are able to access all required resources in terms of toothpaste, tooth brushes, books, etc. that form part of an optimal routine. |
| ‘Habituation’ and ‘lack of self-monitoring of routines’ can act as barrier. Most parents reported just doing their bedtime routines as a habit with little thought. Habits are not by definition bad. It depends on what exactly the habit entails. Habits may serve to maintain and perpetuate good routines over time. However, if the bedtime routines of a family are sub-optimal, habituation of that routine with no self-reflection or time to actively think about the routine can result in a vicious cycle with the same, unhelpful and potentially harmful behaviours repeated every night. | Intention is an important facilitator since almost all parents stated clear intentions to be able to have and maintain good bedtime routines for their children and especially as the children are growing older. |
| ‘Lack of motivation’ and ‘negative emotions’ associated with bedtime routines are an important barrier that contribute to parents feeling incapable of achieving optimal routines in a consistent manner or making positive changes to their bedtime routines where required. | Reinforcement at the end of each night, depending how the routine unfolded, can be important facilitator for achieving, and especially for maintaining, good bedtime routines. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kitsaras, G.; Goodwin, M.; Kelly, M.; Pretty, I.; Allan, J. Perceived Barriers and Facilitators for Bedtime Routines in Families with Young Children. Children 2021, 8, 50. https://doi.org/10.3390/children8010050
Kitsaras G, Goodwin M, Kelly M, Pretty I, Allan J. Perceived Barriers and Facilitators for Bedtime Routines in Families with Young Children. Children. 2021; 8(1):50. https://doi.org/10.3390/children8010050
Chicago/Turabian StyleKitsaras, George, Michaela Goodwin, Michael Kelly, Iain Pretty, and Julia Allan. 2021. "Perceived Barriers and Facilitators for Bedtime Routines in Families with Young Children" Children 8, no. 1: 50. https://doi.org/10.3390/children8010050
APA StyleKitsaras, G., Goodwin, M., Kelly, M., Pretty, I., & Allan, J. (2021). Perceived Barriers and Facilitators for Bedtime Routines in Families with Young Children. Children, 8(1), 50. https://doi.org/10.3390/children8010050





