The Profile, Health Seeking Behavior, Referral Patterns, and Outcome of Outborn Neonates Admitted to a District and Regional Hospital in the Upper West Region of Ghana: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
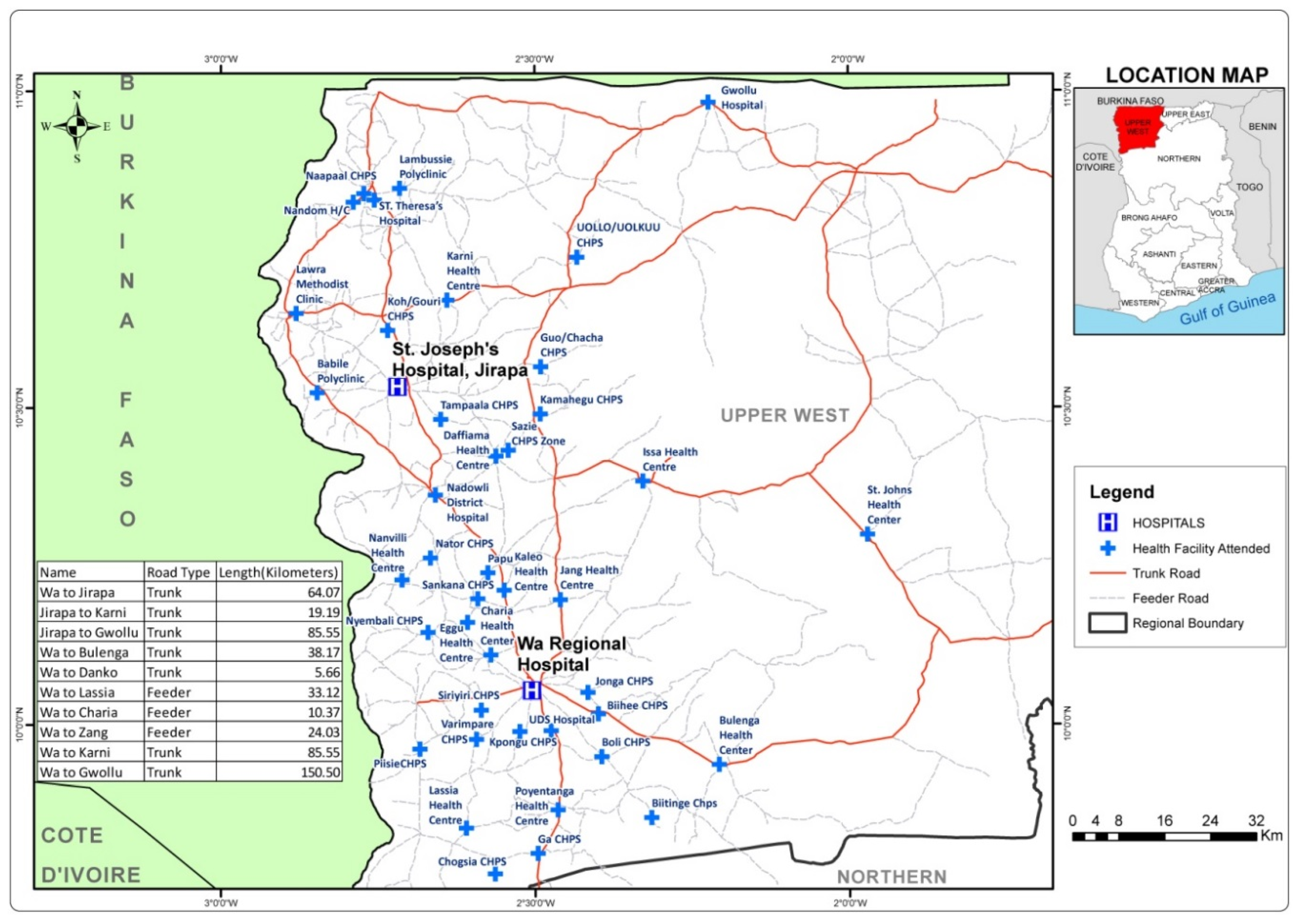
2.1. Study Area
2.2. Study Design
2.3. Sampling and Sample Size
2.4. Study Population
2.5. Data Collection
2.6. Data Analysis
2.7. Ethical Clearance
3. Results
3.1. Characteristics of Patients and Caregivers
3.2. Danger Signs and Home Treatments
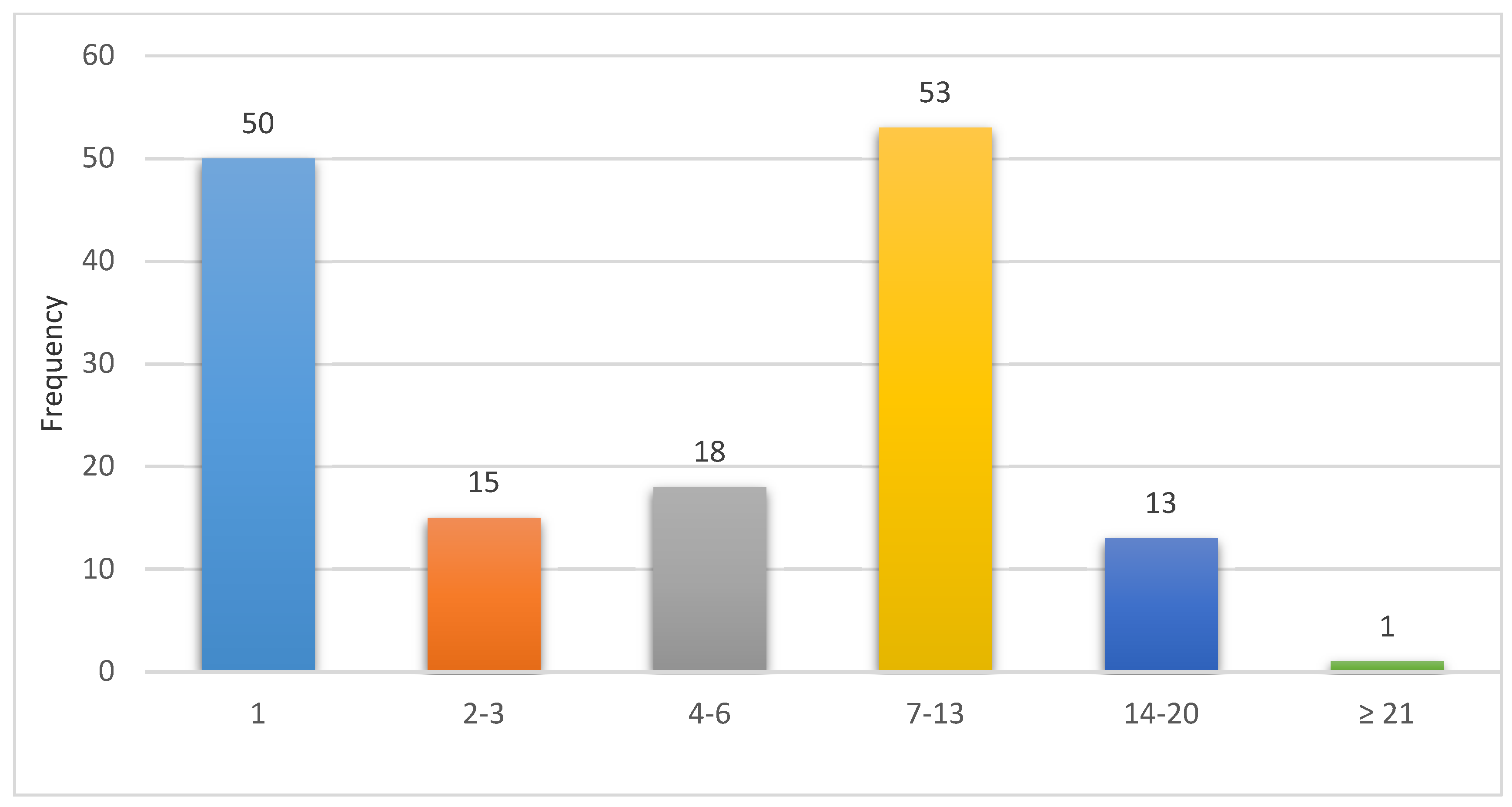
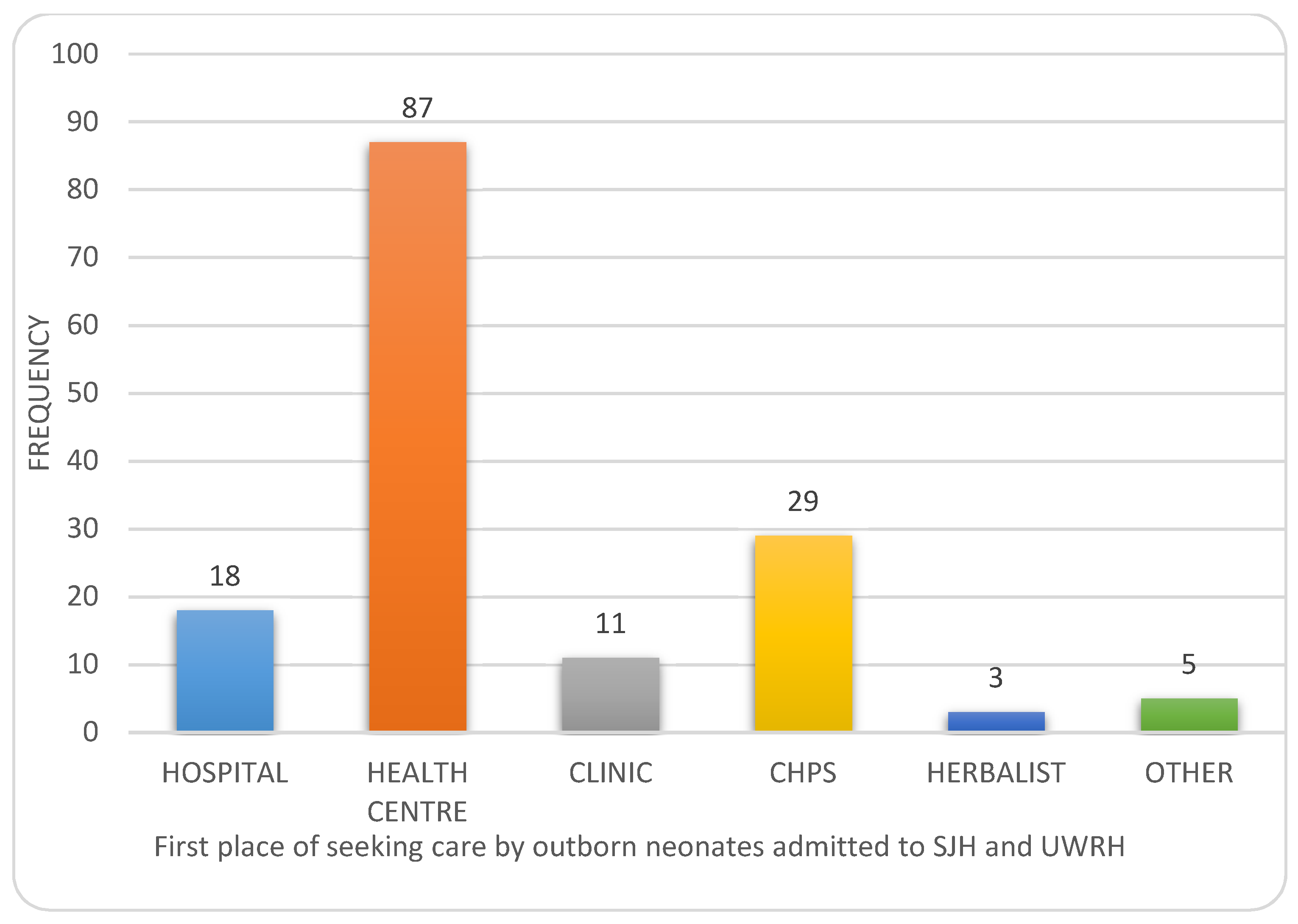
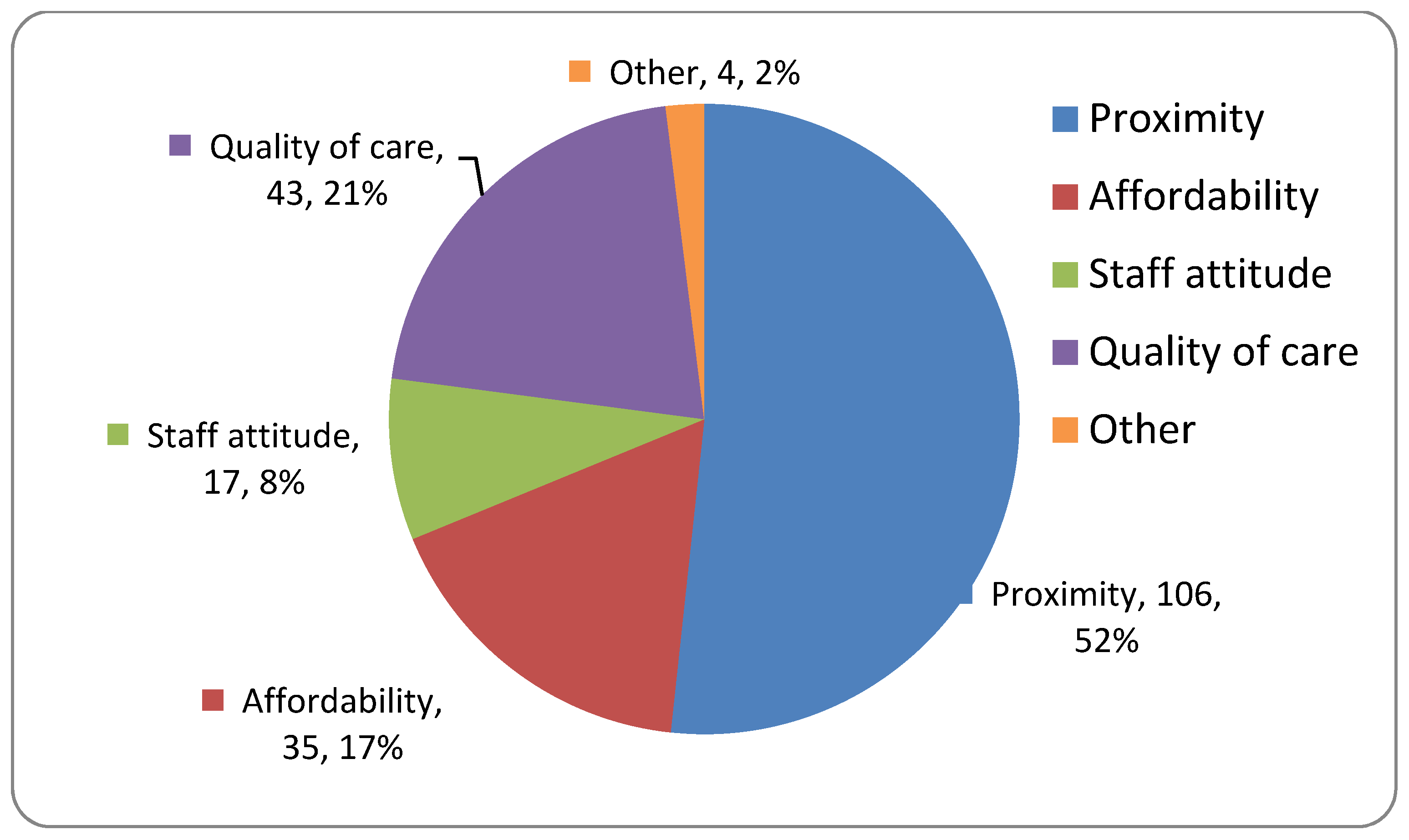
3.3. Health Facilities Attended and Treatments Given
3.4. Difficulties Experienced
3.5. Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lawn, J.E.; Cousens, S.; Zupan, J. 4 million neonatal deaths: When? Where? Why? Lancet 2005, 365, 891–900. [Google Scholar] [CrossRef]
- Ghana Statistical Service (GSS); Ghana Health Service(GHS); ICF International. Ghana Demographic and Health Survey 2014; GSS, GHS, and ICF International: Rockville, MD, USA, 2015. [Google Scholar]
- Thaddeus, S.; Maine, D. Too far to walk: Maternal mortality in context. Soc. Sci. Med. 1994, 38, 1091–1110. [Google Scholar] [CrossRef]
- Lawn, J.; Mongi, P.; Cousens, S. Africa’s Newborns–Counting Them and Making Them Count. 2006. Available online: https://www.who.int/pmnch/media/publications/aonsection_I.pdf (accessed on 17 February 2019).
- Lawn, J.E.; Blencowe, H.; Oza, S.; You, D.; Lee, A.C.; Waiswa, P.; Lalli, M.; Bhutta, Z.; Barros, A.J.; Christian, P.; et al. Every Newborn: Progress, priorities, and potential beyond survival. Lancet 2014, 384, 189–205. [Google Scholar] [CrossRef]
- Akter, T.; Dawson, A.; Sibbritt, D. Changes in neonatal mortality and newborn health-care practices: Descriptive data from the Bangladesh Demographic and Health Surveys 2011 and 2014. WHO South East Asia J. Public Health 2018, 7, 43. [Google Scholar] [CrossRef] [PubMed]
- Herbert, H.K.; Lee, A.C.; Chandran, A.; Rudan, I.; Baqui, A.H. Care Seeking for Neonatal Illness in Low- and Middle-Income Countries: A Systematic Review. PLoS Med. 2012, 9, e1001183. [Google Scholar] [CrossRef] [PubMed]
- Berhe, M.; Medhaniye, A.A.; Kahsay, G.; Birhane, E.; Abay, M. Essential neonatal care utilization and associated factors among mothers in public health facilities of Aksum Town, North Ethiopia, 2016. PLoS ONE 2017, 12, e0175902. [Google Scholar] [CrossRef]
- Srivastava, N.M.; Awasthi, S.; Agarwal, G.G. Care-seeking behavior and out-of-pocket expenditure for sick newborns among urban poor in Lucknow, northern India: A prospective follow-up study. BMC Health Serv. Res. 2009, 9, 61. [Google Scholar] [CrossRef]
- Wambui, W.M.; Kimani, S.; Odhiambo, E. Determinants of Health Seeking Behavior among Caregivers of Infants Admitted with Acute Childhood Illnesses at Kenyatta National Hospital, Nairobi, Kenya. Int. J. Pediatr. 2018, 2018, 1–11. [Google Scholar] [CrossRef]
- Chowdhury, S.K.; Billah, S.M.; Arifeen, S.E.; Hoque, D.M.E. Care-seeking practices for sick neonates: Findings from cross-sectional survey in 14 rural sub-districts of Bangladesh. PLoS ONE 2018, 13, e0204902. [Google Scholar] [CrossRef]
- Shah, R.; Mullany, L.C.; Darmstadt, G.L.; Talukder, R.R.; Rahman, S.M.; Mannan, I.; Arifeen, S.E.; Baqui, A.H. Determinants and pattern of care seeking for preterm newborns in a rural Bangladeshi cohort. BMC Health Serv. Res. 2014, 14, 417. [Google Scholar] [CrossRef]
- World Health Organization. Standards for Improving Quality of Maternal and Newborn Care in Health Facilities; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Kozuki, N.; Guenther, T.; Vaz, L.; Moran, A.; Soofi, S.B.; Kayemba, C.N.; Peterson, S.S.; Bhutta, Z.A.; Khanal, S.; Tielsch, J.M.; et al. A systematic review of community-to-facility neonatal referral completion rates in Africa and Asia. BMC Public Health 2015, 15, 989. [Google Scholar] [CrossRef] [PubMed]
- Ismail, S.A.; McCullough, A.; Guo, S.; Sharkey, A.; Harma, S.; Rutter, P. Gender-related differences in care-seeking behaviour for newborns: A systematic review of the evidence in South Asia. BMJ Glob. Health 2019, 4, e001309. [Google Scholar] [CrossRef] [PubMed]
- Hedstrom, A.; Ryman, T.; Otai, C.; Nyonyintono, J.; McAdams, R.M.; Lester, D.; Batra, M. Demographics, clinical characteristics and neonatal outcomes in a rural Ugandan NICU. BMC Pregnancy Childbirth 2014, 14, 327. [Google Scholar] [CrossRef] [PubMed]
- O’Leary, M.; Edmond, K.; Floyd, S.; Newton, S.; Thomas, G. A cohort study of low birth weight and health outcomes in the first year of life, Ghana. Bull. World Health Organ. 2017, 95, 574–583. [Google Scholar] [CrossRef] [PubMed]
- Ravikumar, S.; Harikrishnan, E.; Elayaraja, K.; Aravind Sunderavel, K. Morbidity and mortality profile of neonates in a tertiary care centre in Tamil Nadu: A study from South India. Int. J. Contemp. Pediatr. 2018, 5, 377–382. [Google Scholar]
- Gibbs, L.; Tooke, L.; Harrison, M. Short-Term Outcomes of Inborn V. Outborn Very-Lowbirth- Weight Neonates South African. South Afr. Med. J. 2017, 107, 900–903. Available online: https://www.ajol.info/index.php/samj/article/view/165816 (accessed on 11 September 2019). [CrossRef]
- Fahmy, N.; Ramy, N.; El Houchi, S.; Abdel Khalek, K.; Alsharany, W.; Tosson, A. Outborns or inborns: Clinical audit of the two intensive care units of Cairo University Hospital. Egypt Pediatr. Assoc. Gaz. 2017, 65, 10–14. [Google Scholar] [CrossRef]
- Ekwochi, U.; Ndu, I.; Nwokoye, I.; Ezenwosu, O.; Amadi, O.; Osuorah, D. Pattern of morbidity and mortality of newborns admitted into the sick and special care baby unit of Enugu State University Teaching Hospital, Enugu state. Niger J. Clin. Pract. 2014, 17, 346. [Google Scholar] [CrossRef]
- Nalwadda, C.K.; Waiswa, P.; Guwatudde, D.; Kerber, K.; Peterson, S.; Kiguli, J. ‘As soon as the umbilical cord gets off, the child ceases to be called a newborn’: Sociocultural beliefs and newborn referral in rural Uganda. Glob. Health Action 2015, 8, 24386. [Google Scholar] [CrossRef][Green Version]
- Syed, U.; Khadka, N.; Khan, A.; Wall, S. Care-seeking practices in South Asia: Using formative research to design program interventions to save newborn lives. J. Perinatol. 2008, 28, S9–S13. [Google Scholar] [CrossRef]
- Warren, C.; Daly, P.; Toure, L.; Mong, P. Postnatal Care. In Opportunities for Africa’s Newborns, Partnership for Maternal Newborn & Child Health; World Health Organization—WHO, Ed.; World Health Organisation: Geneva, Switzerland, 2006; pp. 79–90. Available online: https://www.who.int/pmnch/media/publications/oanfullreport.pdf (accessed on 24 June 2019).
- Lama, T.P.; Khatry, S.K.; Katz, J.; LeClerq, S.C.; Mullany, L.C. Illness recognition, decision-making, and care-seeking for maternal and newborn complications: A qualitative study in Sarlahi District, Nepal. J. Health Popul. Nutr. 2017, 36, 45. [Google Scholar] [CrossRef] [PubMed]
- Awasthi, S.; Verma, T.; Agarwal, M. Danger signs of neonatal illnesses: Perceptions of caregivers and health workers in northern India. Bull. World Health Organ. 2006, 84, 819–826. [Google Scholar] [CrossRef] [PubMed]
- Hasbaoui BEl Karboubi, L.; Benjelloun, B.S. Newborn Haemorrhagic Disorders. Pan Afr Med J. 2017, 28, 123. Available online: https://www.ajol.info/index.php/pamj/article/view/167169 (accessed on 24 June 2019).
- Chou, V.B.; Walker, N.; Bhutta, Z.A.; Paul, V.K.; Blencowe, H.; Lawn, J.E.; Das, J.K.; Bahl, R.; Salam, R.A.; Rizvi, A.; et al. Can available interventions end preventable deaths in mothers, newborn babies, and stillbirths, and at what cost? Lancet 2014, 384, 347–370. [Google Scholar] [CrossRef]
- Bazzano, A.N.; Kirkwood, B.R.; Tawiah-Agyemang, C.; Owusu-Agyei, S.; Adongo, P.B. Beyond symptom recognition: Care-seeking for ill newborns in rural Ghana. Trop. Med. Int. Health 2008, 13, 123–128. [Google Scholar] [CrossRef] [PubMed]
- Sarrassat, S.; Meda, N.; Badolo, H.; Ouedraogo, M.; Somé, H.; Cousens, S. Distance to care, care seeking and child mortality in rural Burkina Faso: Findings from a population-based cross-sectional survey. Trop. Med. Int. Health 2019, 24, 31–42. [Google Scholar] [CrossRef] [PubMed]
- Shamba, D.; Tancred, T.; Hanson, C.; Wachira, J.; Manzi, F. Delayed illness recognition and multiple referrals: A qualitative study exploring care-seeking trajectories contributing to maternal and newborn illnesses and death in southern Tanzania. BMC Health Serv. Res. 2019, 19, 225. [Google Scholar] [CrossRef] [PubMed]
- Sumankuuro, J.; Crockett, J.; Wang, S. Perceived barriers to maternal and newborn health services delivery: A qualitative study of health workers and community members in low and middle-income settings. BMJ Open 2018, 8, e021223. [Google Scholar] [CrossRef]
- Bhutta, Z.; Soofi, S. Community-based newborn care: Are we there yet? Lancet 2008, 372, 1124–1126. [Google Scholar] [CrossRef]
- Hatch, J. The role of the neonatal nurse practitioner in the community hospital level I nursery. Neonatal Netw. 2012, 31, 141–147. [Google Scholar] [CrossRef]
- Awoonor-Williams, J.K.; Bailey, P.E.; Yeji, F.; Adongo, A.E.; Baffoe, P.; Williams, A.; Mercer, S. Conducting an audit to improve the facilitation of emergency maternal and newborn referral in northern Ghana. Glob. Public Health 2015, 10, 1118–1133. [Google Scholar] [CrossRef] [PubMed]
- Vidyasagar, D. Regionalization of Perinatal Care: Its Relevance to India and Other Developing Countries. J. Neonatol. 2005, 19, 293–303. [Google Scholar] [CrossRef]
- Neogi, S.B.; Malhotra, S.; Zodpey, S.; Mohan, P. Does facility-based newborn care improve neonatal outcomes? A review of evidence. Indian Pediatr. 2012, 49, 651–658. [Google Scholar] [CrossRef] [PubMed]
- Waiswa, P.; Pariyo, G.; Kallander, K.; Akuze, J.; Namazzi, G.; Ekirapa-Kiracho, E.; Kerber, K.; Sengendo, H.; Aliganyira, P.; Lawn, J.E.; et al. Effect of the Uganda Newborn Study on care-seeking and care practices: A cluster-randomised controlled trial. Glob. Health Action 2015, 8, 24584. [Google Scholar] [CrossRef] [PubMed]
- Gul, S.; Khalil, R.; Yousafzai, M.T.; Shoukat, F. Newborn care knowledge and practices among mothers attending pediatric outpatient clinic of a hospital in Karachi, Pakistan. Int. J. Health Sci. 2014, 8, 167–175. [Google Scholar] [CrossRef]
- Engmann, C.M.; Hodgson, A.; Aborigo, R.; Adongo, P.L.; Moyer, C.A. Addressing the continuum of maternal and newborn care in Ghana: Implications for policy and practice. Health Policy Plan. 2016, 31, 1355–1363. [Google Scholar] [CrossRef]
- Prost, A.; Colbourn, T.; Seward, N.; Azad, K.; Coomarasamy, A.; Copas, A.; Houweling, T.A.; Fottrell, E.; Kuddus, A.; Lewycka, S.; et al. Women’s groups practising participatory learning and action to improve maternal and newborn health in low-resource settings: A systematic review and meta-analysis. Lancet 2013, 381, 1736–1746. [Google Scholar] [CrossRef]
- Morrison, J.; Tamang, S.; Mesko, N.; Osrin, D.; Shrestha, B.; Manandhar, M.; Manandhar, D.; Standing, H.; Costello, A. Women’s health groups to improve perinatal care in rural Nepal. BMC Pregnancy Childbirth 2005, 5, 6. [Google Scholar] [CrossRef]
- Ghana Health Service. Ghana National Newborn Health Strategy and Action Plan 2019–2023; Ministry of Health: Accra, Ghana, 2019.
- Dong, Y.; Speer, C.P. Late-onset neonatal sepsis: Recent developments. Arch. Dis. Child Fetal Neonatal Ed. 2015, 100, F257–F263. [Google Scholar] [CrossRef]
- Lawn, J.; Kerber, K.; Enweronu-Laryea, C.; Massee Bateman, O. Newborn survival in low resource settings-are we delivering? BJOG An Int. J. Obs. Gynaecol. 2009, 116, 49–59. [Google Scholar] [CrossRef]
| Frequency | Percent (%) | |
|---|---|---|
| MATERNAL CHARACTERISTICS | ||
| Maternal Age (years) | ||
| <20 | 19 | 12.4 |
| 20–35 | 115 | 75.2 |
| >35 | 19 | 12.4 |
| Educational Status | ||
| None | 14 | 9.2 |
| Primary | 27 | 17.6 |
| JHS | 20 | 13.1 |
| SHS | 55 | 35.9 |
| Tertiary | 37 | 24.2 |
| Marital Status | ||
| Married | 118 | 77.1 |
| Divorced | 2 | 1.3 |
| Cohabitation | 2 | 1.3 |
| Single/Never married | 31 | 20.3 |
| Religion | ||
| Christian | 77 | 50.3 |
| Moslem | 74 | 48.4 |
| Traditionalist | 2 | 1.3 |
| NEONATAL CHARACTERISTICS | ||
| Age (days) | ||
| ≤1 | 30 | 19.6 |
| 2–3 | 19 | 12.4 |
| 4–6 | 20 | 13.1 |
| 7–14 | 61 | 39.9 |
| ≥15 | 23 | 15.0 |
| Sex | ||
| Male | 88 | 57.5 |
| Female | 65 | 42.5 |
| Birth weight (grams) | ||
| <1000 | 0 | 0.0 |
| 1000–1499 | 1 | 0.7 |
| 1500–1999 | 8 | 5.2 |
| 2000–2499 | 12 | 7.8 |
| ≥2500 | 132 | 86.3 |
| Gestational age | ||
| <37 weeks | 26 | 17.0 |
| ≥37 weeks | 127 | 83.0 |
| Place of admission | ||
| Upper West R. Hospital | 140 | 91.5 |
| St. Joseph’s Hospital | 13 | 8.5 |
| Reasons for the Referral | Frequency | Percentage (%) | |
|---|---|---|---|
| 1 | Fever | 67 | 44.1 |
| 2 | Breathing abnormalities | 35 | 23.5 |
| 3 | Excessive crying | 27 | 17.8 |
| 4 | Poor feeding | 24 | 15.8 |
| 5 | Abdominal Distension | 17 | 11.2 |
| 6 | Jaundice | 16 | 10.5 |
| 7 | Bleeding | 13 | 8.6 |
| 8 | Vomiting | 12 | 7.9 |
| 9 | Skin lesions | 10 | 6.6 |
| 10 | Prematurity | 8 | 5.2 |
| 11 | Eye discharge | 8 | 5.2 |
| 12 | Discharging/weak cord | 7 | 4.6 |
| 13 | Low birth weight | 7 | 4.6 |
| 14 | Cough | 5 | 3.3 |
| 15 | Febrile convulsion | 4 | 2.6 |
| 16 | Deformity/malformation | 4 | 2.6 |
| 17 | Impetigo | 3 | 2.0 |
| 18 | Congenital malformations | 3 | 2.0 |
| 19 | Inability to pass or difficulty to passing stool | 3 | 2.0 |
| 20 | Diarrhea | 2 | 1.3 |
| 21 | Hypoglycemia | 2 | 1.3 |
| 22 | Hypothermia | 2 | 1.3 |
| 23 | Altered sensorium | 1 | 0.7 |
| 24 | Non-febrile convulsion | 1 | 0.7 |
| * Others | 9 | 5.9 |
| Treatment (Multiple Response) | Frequency | Percentage |
|---|---|---|
| Home treatments | ||
| Medicine to drink | ||
| Herbal medicine | 7 | 4.5 |
| Paracetamol syrup | 21 | 13.5 |
| Teedar (paracetamol + diphenhydramine) syrup | 3 | 1.9 |
| Application of agents to cord | ||
| Breast milk | 2 | 1.3 |
| Applied toothpaste to cord | 1 | 0.6 |
| Used powder | 3 | 1.9 |
| Used cow dung | 3 | 1.9 |
| Shea butter | 2 | 1.3 |
| Palm kernel oil | 1 | 0.6 |
| Other Herbal applications | ||
| Herbal enema | 5 | 3.2 |
| Herbal baths | 6 | 3.8 |
| Herbal lotions/creams | 2 | 1.3 |
| Substances applied to eyes | ||
| Salt water | 4 | 2.6 |
| Breast milk | 1 | 0.6 |
| No home therapy | ||
| Did nothing | 93 | 60.8 |
| Treatment at referring health facility prior to referral to neonatal unit | ||
| Antibiotics were given | 2 | 1.3 |
| Cord was dressed | 4 | 2.6 |
| Paracetamol syrup was given | 9 | 5.9 |
| Salvon was given to baby | 1 | 0.7 |
| Tepid sponging | 1 | 0.7 |
| Baby was detained, medication given and referred afterwards | 30 | 19.6 |
| Nothing was done | 2 | 1.3 |
| Not applicable | 6 | 3.9 |
| Referral note was given | 94 | 61.4 |
| Other | 4 | 2.6 |
| Duration of Illness Before Seeking Care | SEX | ||
|---|---|---|---|
| Male | Female | Total | |
| <24 h | 0 (0) | 1 (11.1%) | 1 (8.3) |
| 1st week | 2 (66.7%) | 3 (33.3%) | 5 (41.7) |
| 2nd week | 1 (33.3%) | 5 (55.6%) | 6 (50.0) |
| Characteristics | OR (95% CI) | p-Values | AOR * (95% CI) | p-Values |
|---|---|---|---|---|
| Birth weight | ||||
| Low birth weight | 0.2 (0.1–0.4) | 0.000 | 0.2 (0.1–0.4) | 0.000 |
| Normal or macrosomia | - | |||
| Home based remedy administration | ||||
| Home remedy administered | 8.5 (2.8–25.3) | 0.000 | 9.0 (2.9–27.5) | 0.000 |
| Home remedy not administered | - | |||
| Neonate fever | ||||
| No Fever | 6.5 (2.5–16.6) | 0.000 | 6.7 (2.6–17.6) | 0.000 |
| Had Fever | - | |||
| Breathing pattern | ||||
| Normal breathing | 6.6 (2.0–20.8) | 0.002 | 6.5 (2.0–21.1) | 0.002 |
| Abnormal breathing | - | |||
| Went to postnatal clinic/health center | ||||
| Less than three times | - | |||
| More than four times | 2.4 (1.0–5.6) | 0.050 | 2.7 (1.1–7.1) | 0.040 |
| Maternal Age | ||||
| 20 years and below | - | |||
| 21–30 years | 1.8 (0.7–4.8) | 0.2 | 2.5 (0.7–9.0) | 0.151 |
| More than 30 years | 2.9 (0.7–3.6) | 0.06 | 4.4 (1.0–4.7) | 0.045 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tette, E.M.A.; Nuertey, B.D.; Azusong, E.A.; Gandau, N.B. The Profile, Health Seeking Behavior, Referral Patterns, and Outcome of Outborn Neonates Admitted to a District and Regional Hospital in the Upper West Region of Ghana: A Cross-Sectional Study. Children 2020, 7, 15. https://doi.org/10.3390/children7020015
Tette EMA, Nuertey BD, Azusong EA, Gandau NB. The Profile, Health Seeking Behavior, Referral Patterns, and Outcome of Outborn Neonates Admitted to a District and Regional Hospital in the Upper West Region of Ghana: A Cross-Sectional Study. Children. 2020; 7(2):15. https://doi.org/10.3390/children7020015
Chicago/Turabian StyleTette, Edem M. A., Benjamin Demah Nuertey, Emmanuel A. Azusong, and Naa Barnabas Gandau. 2020. "The Profile, Health Seeking Behavior, Referral Patterns, and Outcome of Outborn Neonates Admitted to a District and Regional Hospital in the Upper West Region of Ghana: A Cross-Sectional Study" Children 7, no. 2: 15. https://doi.org/10.3390/children7020015
APA StyleTette, E. M. A., Nuertey, B. D., Azusong, E. A., & Gandau, N. B. (2020). The Profile, Health Seeking Behavior, Referral Patterns, and Outcome of Outborn Neonates Admitted to a District and Regional Hospital in the Upper West Region of Ghana: A Cross-Sectional Study. Children, 7(2), 15. https://doi.org/10.3390/children7020015





