Process Evaluation of a School-Based High-Intensity Interval Training Program for Older Adolescents: The Burn 2 Learn Cluster Randomised Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Intervention Description
2.3. Theoretical Basis
2.4. Implementation Framework
2.5. Process Evaluation
2.5.1. Implementation Outcomes
2.5.2. Implementation Determinants
3. Results
3.1. Implementation Outcomes
3.2. Implementation Determinants
4. Discussion
Strengths/Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Janssen, I.; LeBlanc, A.G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 40. [Google Scholar] [CrossRef] [PubMed]
- Lubans, D.; Richards, J.; Hillman, C.; Faulkner, G.; Beauchamp, M.; Nilsson, M.; Kelly, P.; Smith, J.; Raine, L.; Biddle, S. Physical activity for cognitive and mental health in youth: A systematic review of mechanisms. Pediatrics 2016, 138. [Google Scholar] [CrossRef] [PubMed]
- Donnelly, J.E.; Hillman, C.H.; Castelli, D.; Etnier, J.L.; Lee, S.; Tomporowski, P.; Lambourne, K.; Szabo-Reed, A.N. Physical activity, fitness, cognitive function, and academic achievement in children: A systematic review. Med. Sci. Sports Exerc. 2016, 48, 1197. [Google Scholar] [CrossRef] [PubMed]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U.; Group, L.P.A.S.W. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Global trends in insufficient physical activity among adolescents: A pooled analysis of 298 population-based surveys with 1 · 6 million participants. Lancet Child Adolesc. Health 2020, 4, 23–35. [Google Scholar] [CrossRef]
- Dumith, S.C.; Gigante, D.P.; Domingues, M.R.; Kohl III, H.W. Physical activity change during adolescence: A systematic review and a pooled analysis. Int. J. Epidemiol. 2011, 40, 685–698. [Google Scholar] [CrossRef]
- Farooq, M.A.; Parkinson, K.N.; Adamson, A.J.; Pearce, M.S.; Reilly, J.K.; Hughes, A.R.; Janssen, X.; Basterfield, L.; Reilly, J.J. Timing of the decline in physical activity in childhood and adolescence: Gateshead Millennium Cohort Study. Br. J. Sports Med. 2018, 52, 1002–1006. [Google Scholar] [CrossRef]
- Schranz, N.K.; Olds, T.; Boyd, R.; Evans, J.; Gomersall, S.R.; Hardy, L.; Hesketh, K.; Lubans, D.R.; Ridgers, N.D.; Straker, L. Results from Australia’s 2016 report card on physical activity for children and youth. J. Phys. Act. Health 2016, 13, S87–S94. [Google Scholar] [CrossRef]
- World Health Organization. Recommended Population Levels of Physical Activity for Health: 5–17 Years Old; World Health Organization: Geneva, Switzerland, 2010; pp. 15–21. [Google Scholar]
- Raghuveer, G.; Hartz, J.; Lubans, D.R.; Takken, T.; Wiltz, J.L.; Mietus-Snyder, M.; Perak, A.M.; Baker-Smith, C.; Pietris, N.; Edwards, N.M. Cardiorespiratory Fitness in Youth: An Important Marker of Health: A Scientific Statement From the American Heart Association. Circulation 2020, 142, e101–e118. [Google Scholar] [CrossRef]
- Ortega, F.B.; Ruiz, J.R.; Castillo, M.J.; Sjöström, M. Physical fitness in childhood and adolescence: A powerful marker of health. Int. J. Obes. 2008, 32, 1–11. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Comprehensive School Physical Activity Programs: A Guide for Schools; U.S. Department of Health and Human Services: Atlanta, GA, USA, 2013. [Google Scholar]
- Morgan, P.J.; Hansen, V. Classroom teachers’ perceptions of the impact of barriers to teaching physical education on the quality of physical education programs. Res. Q. Exerc. Sport. 2008, 79, 506–516. [Google Scholar] [CrossRef] [PubMed]
- Nathan, N.; Elton, B.; Babic, M.; McCarthy, N.; Sutherland, R.; Presseau, J.; Seward, K.; Hodder, R.; Booth, D.; Yoong, S.L. Barriers and facilitators to the implementation of physical activity policies in schools: A systematic review. Prev. Med. 2018, 107, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Naylor, P.-J.; Nettlefold, L.; Race, D.; Hoy, C.; Ashe, M.C.; Higgins, J.W.; McKay, H.A. Implementation of school based physical activity interventions: A systematic review. Prev. Med. 2015, 72, 95–115. [Google Scholar] [CrossRef] [PubMed]
- Borde, R.; Smith, J.S.; Sutherland, R.; Nathan, N.; Lubans, D.R. Methodological considerations and impact of school-based interventions on objectively measured physical activity in adolescents: A systematic review and meta-analysis. Obes. Rev. 2017, 18, 476–490. [Google Scholar] [CrossRef] [PubMed]
- Love, R.; Adams, J.; van Sluijs, E.M. Are school-based physical activity interventions effective and equitable? A meta-analysis of cluster randomized controlled trials with accelerometer-assessed activity. Obes. Rev. 2019, 20, 859–870. [Google Scholar] [CrossRef] [PubMed]
- Minatto, G.; Barbosa Filho, V.C.; Berria, J.; Petroski, E.L. School-based interventions to improve cardiorespiratory fitness in adolescents: Systematic review with meta-analysis. Sports Med. 2016, 46, 1273–1292. [Google Scholar] [CrossRef]
- Beets, M.W.; Weaver, R.G.; Ioannidis, J.P.; Geraci, M.; Brazendale, K.; Decker, L.; Okely, A.D.; Lubans, D.; van Sluijs, E.; Jago, R. Identification and evaluation of risk of generalizability biases in pilot versus efficacy/effectiveness trials: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 19. [Google Scholar] [CrossRef]
- Kriemler, S.; Meyer, U.; Martin, E.; van Sluijs, E.M.; Andersen, L.B.; Martin, B.W. Effect of school-based interventions on physical activity and fitness in children and adolescents: A review of reviews and systematic update. Br. J. Sports Med. 2011, 45, 923–930. [Google Scholar] [CrossRef]
- Sharma, M. International school-based interventions for preventing obesity in children. Obes. Rev. 2007, 8, 155–167. [Google Scholar] [CrossRef]
- Chambers, D.A.; Glasgow, R.E.; Stange, K.C. The dynamic sustainability framework: Addressing the paradox of sustainment amid ongoing change. Implement. Sci. 2013, 8, 117. [Google Scholar] [CrossRef]
- Wolfenden, L.; Bolsewicz, K.; Grady, A.; McCrabb, S.; Kingsland, M.; Wiggers, J.; Bauman, A.; Wyse, R.; Nathan, N.; Sutherland, R. Optimisation: Defining and exploring a concept to enhance the impact of public health initiatives. Health Res. Syst. 2019, 17, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Hung, T.T.M.; Chiang, V.C.L.; Dawson, A.; Lee, R.L.T. Understanding of factors that enable health promoters in implementing health-promoting schools: A systematic review and narrative synthesis of qualitative evidence. PLoS ONE 2014, 9, e108284. [Google Scholar] [CrossRef] [PubMed]
- Nilsen, P. Making sense of implementation theories, models and frameworks. Implement. Sci. 2015, 10, 53. [Google Scholar] [CrossRef]
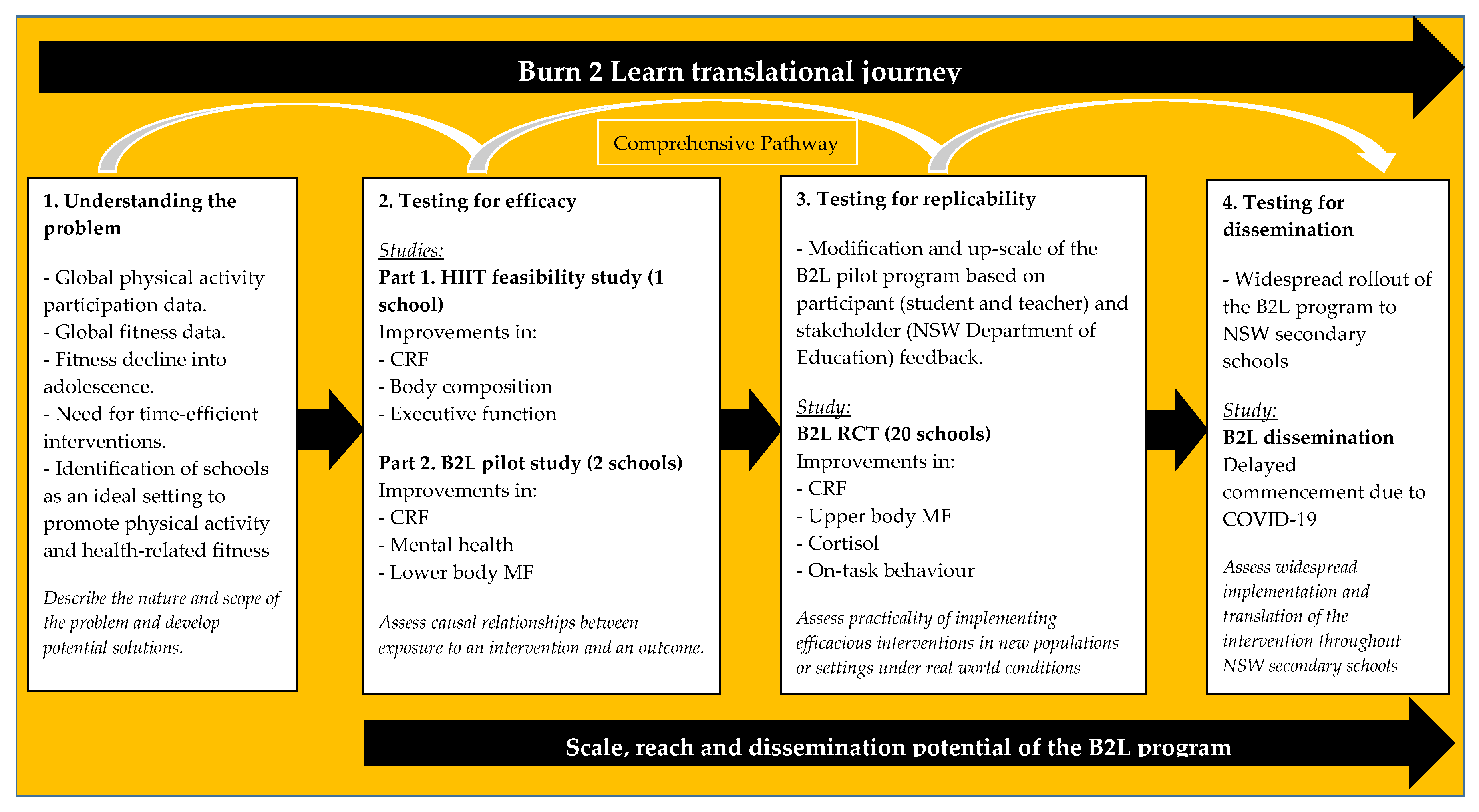
- Kennedy, S.G.; McKay, H.A.; Naylor, P.J.; Lubans, D.R. Implementation and Scale-Up of School-Based Physical Activity Interventions. In The Routledge Handbook of Youth Physical Activity; Routledge: New York, NY, USA; Abingdon, UK, 2020; pp. 438–460. [Google Scholar]
- McKay, H.; Naylor, P.J.; Lau, E.; Gray, S.M.; Wolfenden, L.; Milat, A.; Bauman, A.; Race, D.; Nettlefold, L.; Sims-Gould, J. Implementation and scale-up of physical activity and behavioural nutrition interventions: An evaluation roadmap. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 102. [Google Scholar] [CrossRef]
- Martins, J.; Marques, A.; Sarmento, H.; Carreiro da Costa, F. Adolescents’ perspectives on the barriers and facilitators of physical activity: A systematic review of qualitative studies. Health Educ. Res. 2015, 30, 742–755. [Google Scholar] [CrossRef] [PubMed]
- Weston, K.; Barker, A.R.; Bond, B.; Costigan, S.; Ingul, C.; Williams, C. The BASES Expert Statement on the Role of High-intensity Interval Exercise for Health and Fitness Promotion in Young People. Sport Exerc. Sci. 2020, 8–9. [Google Scholar]
- Logan, G.R.; Harris, N.; Duncan, S.; Schofield, G. A review of adolescent high-intensity interval training. Sports Med. 2014, 44, 1071–1085. [Google Scholar] [CrossRef]
- Costigan, S.A.; Eather, N.; Plotnikoff, R.; Taaffe, D.R.; Lubans, D.R. High-intensity interval training for improving health-related fitness in adolescents: A systematic review and meta-analysis. Br. J. Sports Med. 2015, 49, 1253–1261. [Google Scholar] [CrossRef]
- Leahy, A.A.; Mavilidi, M.F.; Smith, J.J.; Hillman, C.H.; Eather, N.; Barker, D.; Lubans, D.R. Review of High-Intensity Interval Training for Cognitive and Mental Health in Youth. Med. Sci. Sports Exerc. 2020. [Google Scholar] [CrossRef]
- Barkley, J.E.; Epstein, L.H.; Roemmich, J.N. Reinforcing value of interval and continuous physical activity in children. Phys. Behav. 2009, 98, 31–36. [Google Scholar] [CrossRef]
- Bond, B.; Weston, K.L.; Williams, C.A.; Barker, A.R. Perspectives on high-intensity interval exercise for health promotion in children and adolescents. Open Access J. Sports Med. 2017, 8, 243–265. [Google Scholar] [CrossRef] [PubMed]
- Biddle, S.J.H.; Batterham, A.M. High-intensity interval exercise training for public health: A big HIT or shall we HIT it on the head? Int. J. Behav. Nutr. Phys. Act. 2015, 12, 95. [Google Scholar] [CrossRef] [PubMed]
- Malik, A.A.; Williams, C.; Weston, K.; Barker, A.R. Perceptual responses to high-and moderate-intensity interval exercise in adolescents. Med. Sci. Sports Exerc. 2017. [Google Scholar] [CrossRef] [PubMed]
- Leahy, A.A.; Eather, N.; Smith, J.J.; Hillman, C.; Morgan, P.J.; Nilsson, M.; Lonsdale, C.; Plotnikoff, R.C.; Noetel, M.; Holliday, E. School-based physical activity intervention for older adolescents: Rationale and study protocol for the Burn 2 Learn cluster randomised controlled trial. BMJ Open 2019, 9, e026029. [Google Scholar] [CrossRef] [PubMed]
- Leahy, A.A.; Eather, N.; Smith, J.J.; Hillman, C.H.; Morgan, P.J.; Plotnikoff, R.C.; Nilsson, M.; Costigan, S.A.; Noetel, M.; Lubans, D.R. Feasibility and preliminary efficacy of a teacher-facilitated high-intensity interval training intervention for older adolescents. Pediatr. Exerc. Sci. 2019, 31, 107–117. [Google Scholar] [CrossRef] [PubMed]
- Leahy, A.A.; Michels, M.F.; Eather, N.; Hillman, C.H.; Shigeta, T.T.; Lubans, D.R.; Smith, J.J. Feasibility of test administration and preliminary findings for cognitive control in the Burn 2 learn pilot randomised controlled trial. J. Sports Sci. 2020, 38, 1708–1716. [Google Scholar] [CrossRef]
- Lubans, D.R.; Smith, J.J.; Eather, N.; Leahy, A.A.; Morgan, P.J.; Lonsdale, C.; Plotnikoff, R.C.; Nilsson, M.; Kennedy, S.G.; Holliday, E.G.; et al. Time-efficient intervention to improve older adolescents’ cardiorespiratory fitness: Findings from the ‘Burn 2 Learn’ cluster randomized controlled trial. Br. J. Sports Med. 2020, in press. [Google Scholar]
- Taylor, K.L.; Weston, M.; Batterham, A.M. Evaluating intervention fidelity: An example from a high-intensity interval training study. PLoS ONE 2015, 10, e0125166. [Google Scholar] [CrossRef]
- Costigan, S.A.; Eather, N.; Plotnikoff, R.; Taaffe, D.R.; Pollock, E.; Kennedy, S.G.; Lubans, D.R. Preliminary efficacy and feasibility of embedding high intensity interval training into the school day: A pilot randomized controlled trial. Prev. Med. Rep. 2015, 2, 973–979. [Google Scholar] [CrossRef]
- Milat, A.J.; King, L.; Bauman, A.E.; Redman, S. The concept of scalability: Increasing the scale and potential adoption of health promotion interventions into policy and practice. Health Promot. Int. 2013, 28, 285–298. [Google Scholar] [CrossRef]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Mavilidi, M.F.; Mason, C.; Leahy, A.A.; Kennedy, S.G.; Eather, N.; Hillman, C.H.; Morgan, P.J.; Lonsdale, C.; Wade, L.; Riley, N. Effect of a Time-Efficient Physical Activity Intervention on Senior School Students’ On-Task Behaviour and Subjective Vitality: The ‘Burn 2 Learn’Cluster Randomised Controlled Trial. Educ. Psychol. Rev. 2020, 1–25. [Google Scholar]
- Costigan, S.A.; Eather, N.; Plotnikoff, R.C.; Hillman, C.H.; Lubans, D.R. High-intensity interval training on cognitive and mental health in adolescents. Med. Sci. Sports Exerc. 2016, 48, 1985–1993. [Google Scholar] [CrossRef] [PubMed]
- Milat, A.J.; Bauman, A.E.; Redman, S.; Curac, N. Public health research outputs from efficacy to dissemination: A bibliometric analysis. BMC Public Health 2011, 11, 934. [Google Scholar] [CrossRef]
- Nutbeam, D.; Bauman, A.E. Evaluation in a Nutshell: A Practical Guide to the Evaluation of Health Promotion Programs; McGraw-Hill: New York, NY, USA, 2006. [Google Scholar]
- Deci, E.L.; Ryan, R.M. Intrinsic Motivation and Self-Determination in Human Behavior; Plenum Press: New York, NY, USA, 1985. [Google Scholar]
- Lubans, D.R.; Lonsdale, C.; Cohen, K.; Eather, N.; Beauchamp, M.R.; Morgan, P.J.; Sylvester, B.D.; Smith, J.J. Framework for the design and delivery of organized physical activity sessions for children and adolescents: Rationale and description of the ‘SAAFE’ teaching principles. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 24. [Google Scholar] [CrossRef]
- Sutherland, R.; Reeves, P.; Campbell, E.; Lubans, D.R.; Morgan, P.J.; Nathan, N.; Wolfenden, L.; Okely, A.D.; Gillham, K.; Davies, L. Cost effectiveness of a multi-component school-based physical activity intervention targeting adolescents: The ‘Physical Activity 4 Everyone’cluster randomized trial. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 94. [Google Scholar] [CrossRef]
- Lau, E.Y.; Wandersman, A.H.; Pate, R.R. Factors influencing implementation of youth physical activity interventions: An expert perspective. Transl. J. Am. Coll. Sports Med. 2016, 1, 60–70. [Google Scholar]
- Dyrstad, S.M.; Kvalø, S.E.; Alstveit, M.; Skage, I. Physically active academic lessons: Acceptance, barriers and facilitators for implementation. BMC Public Health 2018, 18, 1–11. [Google Scholar] [CrossRef]
- Kohl, R.; Cooley, L. Scaling up—A Conceptual and Operational Framework; Management Systems International: Washington, DC, USA, 2003; pp. 1–31. [Google Scholar]
- Milat, A.J.; King, L.; Newson, R.; Wolfenden, L.; Rissel, C.; Bauman, A.; Redman, S. Increasing the scale and adoption of population health interventions: Experiences and perspectives of policy makers, practitioners, and researchers. Health Res. Syst. 2014, 12, 18. [Google Scholar] [CrossRef]
- Bopp, M.; Saunders, R.P.; Lattimore, D. The tug-of-war: Fidelity versus adaptation throughout the health promotion program life cycle. J. Prim. Prev. 2013, 34, 193–207. [Google Scholar] [CrossRef]
- Hills, A.P.; Dengel, D.R.; Lubans, D.R. Supporting public health priorities: Recommendations for physical education and physical activity promotion in schools. Prog. Cardiovasc. Dis. 2015, 57, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Beets, M.W.; Okely, A.; Weaver, R.G.; Webster, C.; Lubans, D.; Brusseau, T.; Carson, R.; Cliff, D.P. The theory of expanded, extended, and enhanced opportunities for youth physical activity promotion. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Su, Y.-L.; Reeve, J. A meta-analysis of the effectiveness of intervention programs designed to support autonomy. Educ. Psychol. Rev. 2011, 23, 159–188. [Google Scholar] [CrossRef]
- Silins, H.; Mulford, B. Schools as learning organisations. J. Educ. Adm. 2002. [Google Scholar] [CrossRef]
- Chandler, J.; Brazendale, K.; Beets, M.; Mealing, B. Classification of physical activity intensities using a wrist-worn accelerometer in 8–12-year-old children. Pediatr. Obes. 2016, 11, 120–127. [Google Scholar] [CrossRef]
- Brazendale, K.; Beets, M.W.; Weaver, R.G.; Pate, R.R.; Turner-McGrievy, G.M.; Kaczynski, A.T.; Chandler, J.L.; Bohnert, A.; von Hippel, P.T. Understanding differences between summer vs. school obesogenic behaviors of children: The structured days hypothesis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 100. [Google Scholar] [CrossRef]
- Eather, N.; Beauchamp, M.R.; Rhodes, R.E.; Diallo, T.M.; Smith, J.J.; Jung, M.E.; Plotnikoff, R.C.; Noetel, M.; Harris, N.; Graham, E. Development and Evaluation of the High-Intensity Interval Training Self-Efficacy Questionnaire. J. Sport Exerc. Psychol. 2020, 42, 114–122. [Google Scholar] [CrossRef]
- Luszczynska, A.; Cao, D.S.; Mallach, N.; Pietron, K.; Mazurkiewicz, M.; Schwarzer, R. Intentions, planning, and self-efficacy predict physical activity in Chinese and Polish adolescents: Two moderated mediation analyses. International Journal of Clinical and Health Psychology. Int. J. Clin. Health Psychol. 2010, 10, 265–278. [Google Scholar]
- Sharma, M. School-based interventions for childhood and adolescent obesity. Obes. Rev. 2006, 7, 261–269. [Google Scholar] [CrossRef]
- Durlak, J.A.; DuPre, E.P. Implementation matters: A review of research on the influence of implementation on program outcomes and the factors affecting implementation. Am. J. Commun. Psychol. 2008, 41, 327. [Google Scholar] [CrossRef]

| McKay and Colleagues’ [27] Definition | Operationalisation within B2L | ||
|---|---|---|---|
| Outcomes | Dose delivered | Intended units of each intervention component delivered to participants by the delivery team | (a) Number of B2L sessions delivered by teachers, throughout the three phases of delivery. (b) Student-reported session participation (c) Proportion of students completing self-directed sessions during the school holidays |
| Reach | Proportion of the intended priority audience (i.e., participants) who participate in the intervention | Proportion of students from classes involved in the intervention that consented to participating | |
| Fidelity | The extent to which an intervention is implemented as it was prescribed in the intervention protocol—by the delivery team | (a) Session quality (as delivered by teachers) was assessed by members of the research team, utilising the SAAFE observation checklist (see Supplementary Figure S2). (b) Session intensity was also assessed throughout the intervention, using HR monitors. | |
| Sustainability | Whether an intervention continues to be delivered | (a) Teachers’ intention to deliver the B2L program to future student cohorts (b) Students’ intention to participate in HIIT | |
| Determinants | Context | Aspects of the larger social, political and economic environment that may influence intervention implementation | Impact of the NSW Department of Education professional learning requirements and endorsements on implementation |
| Acceptability | Perceptions among the delivery team that a given intervention is agreeable, palatable, or satisfactory | Teachers’ perceptions of the: (a) Quality of program resources (b) Acceptability of intervention delivery time | |
| Adaptability | Extent to which an intervention can be adapted, tailored, refined, or reinvented to meet local needs | Teachers’ perceptions of the adaptability of the program dependent on school/class characteristics | |
| Compatibility | Extent to which an intervention fits with the mission, priorities and values of organisations or settings | Teachers’ perceptions of increases in students’ on-task behaviour, academic performance and mental health | |
| Culture | Organisations’ norms, values and basic assumptions around selected health outcomes | (a) School executives and teacher support of the B2L program (b) Teacher provided with recognition for delivering the program | |
| Dose (satisfaction) | Delivery team’s satisfaction with an intervention and with interactions with the support system | (a) Teachers’ overall program satisfaction (b) Students’ overall program satisfaction (c) Interactions with external change agents | |
| Complexity | Perceptions among the delivery team that a given intervention is relatively difficult to understand and use; number of different intervention components | Teachers’ perceptions of program implementation | |
| Self-efficacy | Delivery team’s belief in its ability to execute courses of action to achieve implementation goals | Teachers’ perceptions of implementation capability | |
| Characteristics | B2L Intervention Schools (n = 10) | Control Schools (n = 10) | |
|---|---|---|---|
| Student | Socioeconomic status, mean (SD) %; range a Low Medium High | 81 (24.3) 169 (50.8) 83 (24.9) | 48 (14.5) 170 (51.4) 113 (34.1) |
| Indigenous decent, n (%) b Yes No | 24 (7.2) 311 (92.8) | 37 (11.2) 294 (88.8) | |
| Cultural background, n (%) b Australian European African Asian Middle Eastern Other | 239 (71.3) 39 (11.6) 3 (0.9) 21 (6.3) 4 (1.2) 29 (8.7) | 230 (69.5) 28 (8.5) 3 (0.9) 18 (5.4) 3 (0.9) 49 (14.8) | |
| School | Student enrolments Total enrolments, N Female enrolments, n (%) Male enrolments, n (%) Enrolments per school, mean (SD); range Female enrolments per school, mean (SD); range Male enrolments per school, mean (SD); range | 9634 5524 (57) 4210 (43) 963 (329); 588–1575 552 (316); 289–1322 421 (259); 0–1019 | 9675 4623 (48) 5052 (52) 966 (306); 600–1426 462 (137); 294–694 505 (171); 306–732 |
| Selective schools, n (%) Academic, n (%) Performing Arts, n (%) | 2 (20) 1 (10) 1 (10) | 1 (10) 1 (10) 0 (0) | |
| School location, n (%) Major Cities Inner Regional | 9 (90) 1 (10) | 10 (100) 0 (0) | |
| School type, n (%) 7–12 K-12 11–12 10–12 | 8 (80) 1 (10) 0 (0) 1 (10) | 8 (80) 0 (0) 2 (20) 0 (0) | |
| School Index of Community Socio-Educational Advantage (ISCEA) c ISCEA Mean (SD); Range d ISCEA Percentile Mean (SD) e; Range | 998 (86); 871–1120 47 (34); 5–90 | 1020 (83); 929–1153 54 (33); 15–96 | |
| Dose delivered | Teacher reported B2L sessions/week, mean (SD) Teacher reported B2L sessions/week, range Proportion of teachers delivering sessions during each Phase, % (n) | Phase 1 2.0 (0.8) 0–3 90 (19) | Phase 2 1.7 (0.6) 0–3 95 (20) | Phase 3 0.6 (0.7) 0–2 50 (10) | |
| Total number of teacher reported B2L sessions delivered/week), mean (SD) Typical length of teacher reported B2L sessions, n (%) 4 min 8 min 12 min 16 min Student reported participation in B2L sessions/week, mean (SD) Students completing B2L session in the school holidays, n (%) Never <1/week 1/week 2/week 3/week More than 3/week | 25.9 (5.2) 4 (19.0) 12 (57.1) 4 (19.0) 1 (4.8) 3.2 (0.9) 154 (57.7) 43 (16.1) 26 (9.7) 30 (11.2) 9 (3.4) 5 (1.9) | ||||
| Reach | Consent rates from intervention schools, mean % (SD) | 79.0 (18.2) | |||
| Fidelity | Session Quality | Adherence to SAAFE delivery principles, mean (SD) Supportive (/4) Active (/4) Autonomous (/4) Fair (/4) Enjoyable (/4) Session total (/20) | Observation 1 3.5 (0.7) 3.1 (0.8) 2.5 (0.9) 3.3 (0.8) 2.8 (1.1) 15.1 (3.2) | Observation 2 3.5 (0.7) 3.3 (0.7) 2.9 (1.1) 3.5 (0.6) 3.2 (0.9) 16.3 (2.7) | Overall 3.5 (0.6) 3.3 (0.7) 2.8 (0.9) 3.4 (0.6) 3.1 (0.8) 16.0 (2.6) |
| Session Intensity | Average HR during sessions, mean beats per minute (SD) Average HR during sessions, mean % of HRmax (SD) Number of students achieving Average HR ≥ 85% HRmax, n (% whole cohort) Peak HR during sessions, mean beats per minute (SD) Peak HR during sessions, mean % of HRmax (SD) Number of students achieving Peak HR ≥ 85% HRmax, n (% whole cohort) | 143.1 (21.8) 70 (11) 56 (17) 167.6 (20.4) 82 (10) 170 (50) | |||
| Sustainability | Intention to deliver to future cohorts of students (Yes, %) Student intention to participate in HIIT in the future (Yes, %) | 81.8 69.6 | |||
| Determinant | Evaluation Questionnaire Item | Mean (SD) | Qualitative Comments from Teachers a/Students b |
|---|---|---|---|
| Context c | (a) Implementation facilitated to satisfy professional learning requirements | 2.0 (0.8) | NC |
| (b) Implementation facilitated due to endorsement by the NSW Department of Education | 2.6 (0.8) | NC | |
| Acceptability c | (a) Quality and acceptable design of resources | 3.1 (0.6) | (1) Great resources with support cards and music! (2) The resources provided for the B2L program were very useful. (3) I enjoyed the B2L program and believe the resources were great. |
| (b) Acceptability of intervention delivery time | 2.3 (0.6) | (1) Sometimes the time including transition, etc. took a little longer than I had hoped. (2) Around assessment periods it was harder to implement and find time to complete. | |
| Adaptability c | Adaptation to school characteristics | 3.4 (0.6) | NC |
| Compatibility (Appropriateness) c | Perceived improvements in student: | ||
| (a) On-task behaviour | 3.2 (0.6) | (1) Each student who participated enjoyed the sessions and were more alert and could concentrate more in class after the session. (2) Benefit to students. | |
| (b) Academic performance | 3.3 (0.7) | (1) Each student who participated enjoyed the sessions and were more alert and could concentrate more in class after the session. (2) Benefit to students. | |
| (c) Mental health | 3.6 (0.5) | (1) Benefit to students. | |
| Culture c | (a) Teachers at school supportive of B2L | 3.4 (0.6) | NC |
| (b) School executives supportive of B2L | 3.3 (0.7) | NC | |
| (c) Incentives and recognition for implementing B2L | 2.3 (0.7) | NC | |
| Dose (Satisfaction) | (a) Teacher satisfaction, mean (SD) c | 3.3 (0.5) | (1) B2L was a great success. (2) I enjoyed the B2L program. (3) Personally, I enjoyed the program and definitely support the reasoning behind the implementation of physical activity in senior years. |
| (b) Student satisfaction, mean (SD) d, | 3.8 (0.9) | (1) Everything, it was all heaps good. (2) It was very enjoyable and great to do with friends. (3) Encouraged me to exercise as it was a part of class and I had time to participate | |
| (c) Research team support, mean (SD) c | 3.6 (0.5) | (1) The knowledge and support provided by the University were excellent. (2) I liked that the University were in touch constantly. (3) The support when the uni attended was beneficial. | |
| Complexity c | Ease of implementation | 3.0 (0.7) | (1) Easy to implement on a weekly basis. (2) The program was easy to implement. |
| Self-efficacy c | Teacher confidence to implement B2L | 3.5 (0.6) | (1) Great program I was really excited to implement. |
| Determinant | Evaluation Questionnaire item | SD (n, %) | D (n, %) | A (n, %) | SA (n, %) | |||
|---|---|---|---|---|---|---|---|---|
| Teacher | Context a | (a) Implementation facilitated to satisfy professional learning requirements (b) Implementation facilitated due to endorsement by the NSW Department of Education | 6 (29) 1 (5) | 9 (43) 9 (43) | 6 (29) 8 (38) | 0 (0) 3 (14) | ||
| Acceptability a | (a) Quality and acceptable design of resources (b) Acceptability of intervention delivery time | 0 (0) 1 (9) | 2 (10) 6 (55) | 14 (67) 4 (36) | 5 (24) 0 (0) | |||
| Adaptability a | Adaptation to school characteristics | 0 (0) | 1 (5) | 10 (48) | 10 (48) | |||
| Compatibility (Appropriateness) a | Perceived improvements in student: (a) On-task behaviour (b) Academic performance (c) Mental health | 0 (0) 0 (0) 0 (0) | 2 (10) 2 (10) 0 (0) | 13 (62) 10 (48) 9 (45) | 6 (29) 9 (43) 11 (55) | |||
| Culture a | (a) Teachers at school supportive of B2L (b) School executives supportive of B2L (c) Incentives and recognition for implementing B2L | 0 (0) 1 (5) 2 (10) | 1 (5) 0 (0) 11 (52) | 11 (52) 11 (52) 7 (33) | 9 (43) 9 (43) 1 (5) | |||
| Dose (Satisfaction) | (a) Teacher satisfaction, mean (SD) a | 0 (0) | 0 (0) | 14 (67) | 7 (33) | |||
| (b) Research team support, mean (SD) a | 0 (0) | 0 (0) | 8 (38) | 13 (62) | ||||
| Complexity a | Ease of implementation | 0 (0) | 5 (24) | 10 (48) | 6 (29) | |||
| Self-efficacy a | Teacher confidence to implement B2L | 0 (0) | 1 (5) | 9 (43) | 11 (52) | |||
| Student | Dose (Satisfaction) b | P | F | Av | G | E | ||
| Student satisfaction, mean (SD) b | 7 (3) | 15 (6) | 50 (19) | 137 (51) | 58 (22) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kennedy, S.G.; Leahy, A.A.; Smith, J.J.; Eather, N.; Hillman, C.H.; Morgan, P.J.; Plotnikoff, R.C.; Boyer, J.; Lubans, D.R. Process Evaluation of a School-Based High-Intensity Interval Training Program for Older Adolescents: The Burn 2 Learn Cluster Randomised Controlled Trial. Children 2020, 7, 299. https://doi.org/10.3390/children7120299
Kennedy SG, Leahy AA, Smith JJ, Eather N, Hillman CH, Morgan PJ, Plotnikoff RC, Boyer J, Lubans DR. Process Evaluation of a School-Based High-Intensity Interval Training Program for Older Adolescents: The Burn 2 Learn Cluster Randomised Controlled Trial. Children. 2020; 7(12):299. https://doi.org/10.3390/children7120299
Chicago/Turabian StyleKennedy, Sarah G., Angus A. Leahy, Jordan J. Smith, Narelle Eather, Charles H. Hillman, Philip J. Morgan, Ronald C. Plotnikoff, James Boyer, and David R. Lubans. 2020. "Process Evaluation of a School-Based High-Intensity Interval Training Program for Older Adolescents: The Burn 2 Learn Cluster Randomised Controlled Trial" Children 7, no. 12: 299. https://doi.org/10.3390/children7120299
APA StyleKennedy, S. G., Leahy, A. A., Smith, J. J., Eather, N., Hillman, C. H., Morgan, P. J., Plotnikoff, R. C., Boyer, J., & Lubans, D. R. (2020). Process Evaluation of a School-Based High-Intensity Interval Training Program for Older Adolescents: The Burn 2 Learn Cluster Randomised Controlled Trial. Children, 7(12), 299. https://doi.org/10.3390/children7120299





