A Validation and Cost-Analysis Study of a Targeted School-Based Dental Check-Up Intervention: Children’s Dental Program
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Target Population
2.2. Sample Size
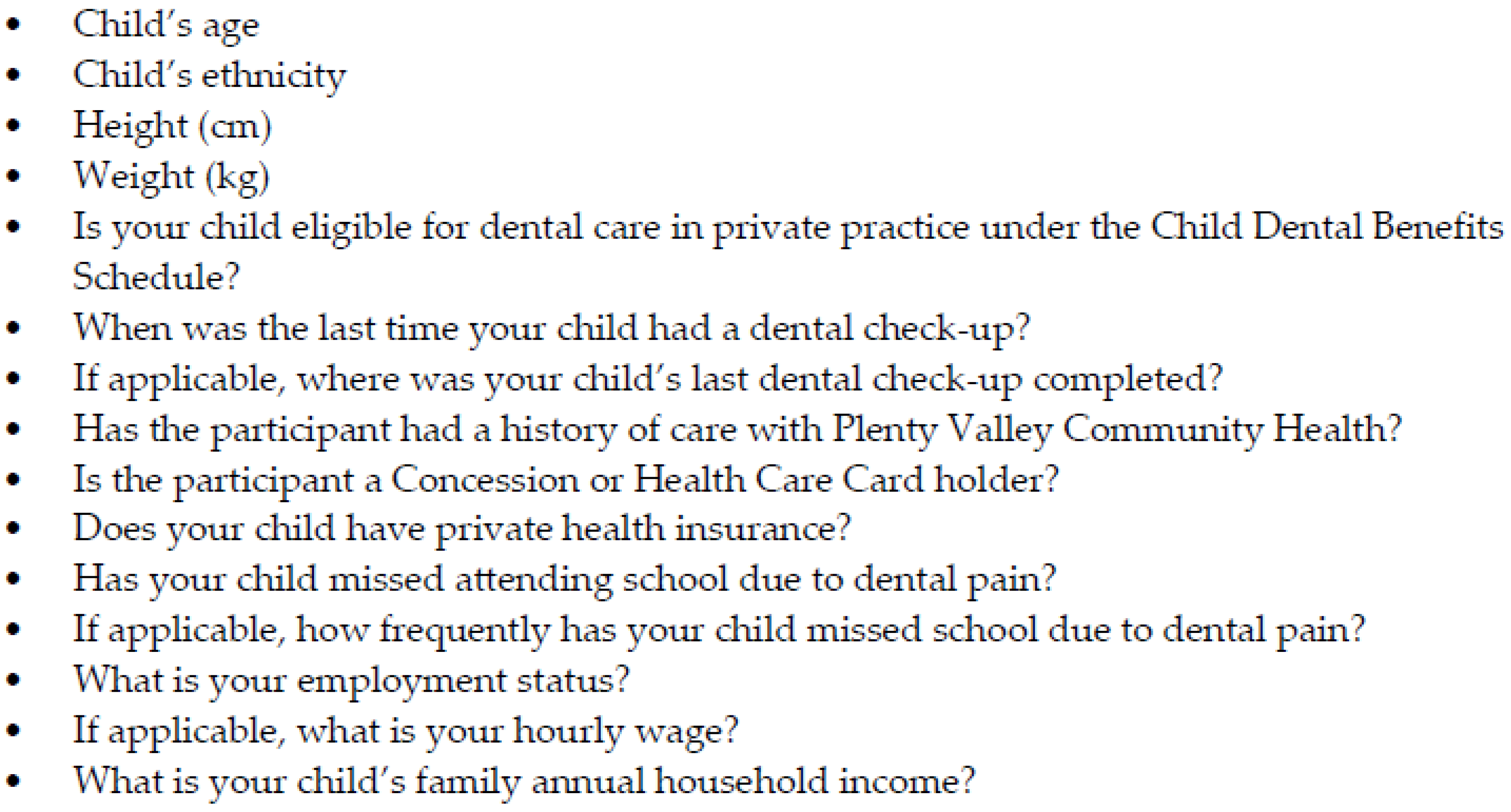
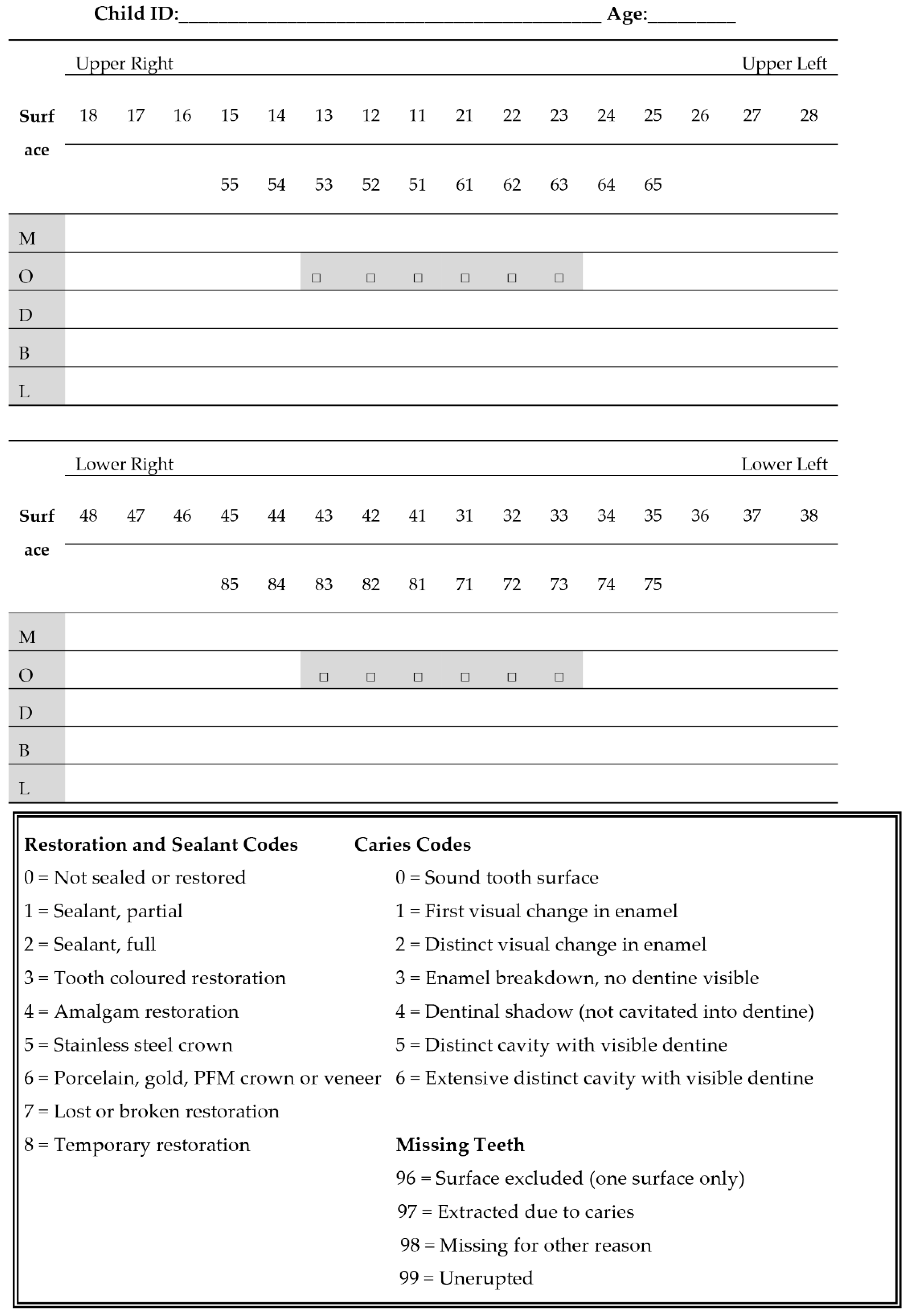
2.3. Training and Calibration
2.4. The Intervention
2.5. Standard Care
2.6. Data Collection
- Previous history of the last dental visit,
- Household income,
- Card-holder status (eligibility for subsidised publicly funded healthcare),
- Eligibility for the CDBS, and
- Cultural background classified using the Australian Standard Classification of Cultural and Ethnic Groups (ASCCEG) [21].
- Date of birth,
- Sex,
- Principle place of residence classified using the SEIFA index [18],
- Dental referral/treatment required after a dental check-up,
- Whether the child received any restorations or extractions for dental caries,
- The status if the child’s dental treatment plan was completed,
- Dental treatment time,
- Number of dental visits,
- The number and type of dental treatment services provided according to the Australian Schedule of Dental Services and Glossary [25], and
- The prevalence of untreated and treated dental caries (in units of teeth).
2.7. Cost-Analysis
2.8. Data Analysis
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| EQ-5D-Y | |
|---|---|
| Describing your health TODAY | |
| Under each heading, please tick the ONE box that best describes your health TODAY | |
| Mobility (walking about) | |
| I have no problems walking about | □ |
| I have some problems walking about | □ |
| I have a lot of problems walking about | □ |
| Looking after myself | |
| I have no problems washing or dressing myself | □ |
| I have some problems washing or dressing myself | □ |
| I have a lot of problems washing or dressing myself | □ |
| Doing usual activities (for example, going to school, hobbies, sports, playing, doing things with family or friends) | |
| I have no problems doing my usual activities | □ |
| I have some problems doing my usual activities | □ |
| I have a lot of problems doing my usual activities | □ |
| Having pain or discomfort | |
| I have no pain or discomfort | □ |
| I have some pain or discomfort | □ |
| I have a lot of pain or discomfort | □ |
| Feeling worried, sad or unhappy | |
| I am not worried, sad or unhappy | □ |
| I am a bit worried, sad or unhappy | □ |
| I am very worried, sad or unhappy | □ |
| Weight Category | Percentile Range |
|---|---|
| Below a healthy weight | Less than the 5th percentile |
| Healthy Weight | 5th percentile to less than the 85th percentile |
| Above a healthy weight | 85th to less than the 95th percentile |
| Well above a healthy weight | Equal to or greater than the 95th percentile |
References
- Peres, M.A.; Macpherson, L.M.D.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- Do, L.; Spencer, J.E. Oral Health of Australian Children: The National Child Oral Health Study 2012–14; University of Adelaide Press: Adelaide, Australia, 2016. [Google Scholar] [CrossRef]
- Nguyen, T.M.N. Is the Current Model of Public Dental Care Promoting the Oral Health of Young Children in Australia? Australian Healthcare and Hospitals Association, Deeble Institute: Canberra, Australia, 2017; Available online: https://ahha.asn.au/publication/health-policy-issue-briefs/deeble-institute-issues-brief-no-20-current-model-public (accessed on 13 October 2020).
- Australian Government, Department of Health. Report on the Fourth Review of the Dental Benefits Act 2008; Australian Government: Canberra, Australia, 2019. Available online: https://www1.health.gov.au/internet/main/publishing.nsf/Content/Dental_Report_on_the_Review_of_the_Dental_Benefits_Act_2008 (accessed on 13 October 2020).
- Arora, A.; Khattri, S.; Ismail, N.; Kumbargere Nagraj, S.; Prashanti, E. School dental screening programmes for oral health. Cochrane Database Syst. Rev. 2019, 8, CD012595. [Google Scholar] [CrossRef] [PubMed]
- Joury, E.; Bernabe, E.; Sabbah, W.; Nakhleh, K.; Gurusamy, K. Systematic review and meta-analysis of randomised controlled trials on the effectiveness of school-based dental screening versus no screening on improving oral health in children. J. Dent. 2017, 58, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.M.N.; Hsueh, Y.-S.; Morgan, M.; Mariño, R.; Koshy, S. Economic Evaluation of a Pilot Targeted School-Based Dental Check-up Program. JDR Clin. Trans. Res. 2017, 2, 214–222. [Google Scholar] [CrossRef]
- Milsom, K.; Blinkhorn, A.; Worthington, H.; Threlfall, A.; Buchanan, K.; Kearney-Mitchell, P.; Tickle, M. The effectiveness of school dental screening: A cluster-randomized control trial. J. Dent. Res. 2006, 85, 924–928. [Google Scholar] [CrossRef]
- Wainwright, P.; Thomas, J.; Jones, M. Health promotion and the role of the school nurse: A systematic review. J. Adv. Nurs. 2000, 32, 1083–1091. [Google Scholar] [CrossRef]
- Lineberry, M.J.; Ickes, M.J. The role and impact of nurses in American elementary schools: A systematic review of the research. J. Sch. Nurs. 2015, 31, 22–33. [Google Scholar] [CrossRef]
- Greyson, D.; Vriesema-Magnuson, C.; Bettinger, J.A. Impact of school vaccination mandates on pediatric vaccination coverage: A systematic review. CMAJ Open 2019, 7, e524–e536. [Google Scholar] [CrossRef]
- Fisher-Owens, S.A.; Gansky, S.A.; Platt, L.J.; Weintraub, J.A.; Soobader, M.-J.; Bramlett, M.D.; Newacheck, P.W. Influences on children’s oral health: A conceptual model. Pediatrics 2007, 120, e510–e520. [Google Scholar] [CrossRef]
- Nguyen, T.M.N.; Morgan, M.; Koshy, S.; Mathew, S.; Lew, S. Revisiting the value of school dental check-up programs. Health Care 2015, 50, 70. [Google Scholar]
- Armfield, J.M.; Spencer, A.J.; Stewart, J.F. Dental fear in Australia: Who’s afraid of the dentist? Aus. Dent. J. 2006, 51, 78–85. [Google Scholar] [CrossRef]
- Rebelo, M.A.B.; Rebelo Vieira, J.M.; Pereira, J.V.; Quadros, L.N.; Vettore, M.V. Does oral health influence school performance and school attendance? A systematic review and meta-analysis. Int. J. Clin. Pediatr. Dent. 2019, 29, 138–148. [Google Scholar] [CrossRef] [PubMed]
- Ruff, R.R.; Senthi, S.; Susser, S.R.; Tsutsui, A. Oral health, academic performance, and school absenteeism in children and adolescents: A systematic review and meta-analysis. J. Am. Dent. Assoc. 2019, 150, 111–121. [Google Scholar] [CrossRef] [PubMed]
- Hooley, M.; Skouteris, H.; Boganin, C.; Satur, J.; Kilpatrick, N. Body mass index and dental caries in children and adolescents: A systematic review of literature published 2004 to 2011. Syst. Rev. 2012, 21, 57. [Google Scholar] [CrossRef] [PubMed]
- Australian Bureau of Statistics. Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2011; Australian Bureau of Statistics: Canberra, Australia, 2013. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/DetailsPage/2033.0.55.0012011 (accessed on 13 October 2020).
- Lemeshow, S. Adequacy of Sample Size in Health Studies; John Wiley & Sons Limited: West Sussex, UK, 1990. [Google Scholar]
- International Caries Detection and Assessment System (ICDAS) Coordinating Committee. Criteria Manual: International Caries Detection and Assessment System (ICDAS II). Available online: https://iccms-web.com/uploads/asset/5ccb149905404942610729.pdf (accessed on 13 October 2020).
- Australian Bureau of Statistics. Australian Standard Classification of Cultural and Ethnic Groups. Available online: https://www.abs.gov.au/ausstats/abs@.nsf/mf/1249.0 (accessed on 13 October 2020).
- EuroQol Group. EQ-5D-Y User Guide. Available online: https://euroqol.org/wp-content/uploads/2019/10/EQ-5D-Y-User-Guide.pdf (accessed on 13 October 2020).
- Kreimeier, S.; Greiner, W. EQ-5D-Y as a Health-Related Quality of Life Instrument for Children and Adolescents: The Instrument’s Characteristics, Development, Current Use, and Challenges of Developing Its Value Set. Value Health 2019, 22, 31–37. [Google Scholar] [CrossRef]
- NSW Health. Healthy Weight Calculator for Children and Teenagers. Available online: https://pro.healthykids.nsw.gov.au/calculator (accessed on 13 October 2020).
- Australian Dental Association. The Australian Schedule of Dental Services and Glossary: Twelfth Edition. Available online: https://www.ada.org.au/Dental-Professionals/Publications/Schedule-and-Glossary/The-Australian-Schedule-of-Dental-Services-and-(1)/Australian_Schedule_and_Dental_Glossary_2015_FA2_W.aspx (accessed on 13 October 2020).
- Australian Tax Office. Cents per Kilometre Method. Available online: https://www.ato.gov.au/Business/Income-and-deductions-for-business/Deductions/Deductions-for-motor-vehicle-expenses/Cents-per-kilometre-method (accessed on 13 October 2020).
- Fair Work Commission. National Minimum Wage Order 2016. Available online: https://www.fwc.gov.au/awards-agreements/minimum-wages-conditions/annual-wage-reviews/annual-wage-review-2015-16/national (accessed on 13 October 2020).
- Australian Government, Department of Health. The Child Dental Benefits Schedule. Available online: https://www1.health.gov.au/internet/main/publishing.nsf/Content/childdental (accessed on 13 October 2020).
- Harris, R.; Nicoll, A.D.; Adair, P.M.; Pine, C.M. Risk factors for dental caries in young children: A systematic review of the literature. Community Dent. Health 2004, 21, 71–85. [Google Scholar] [PubMed]
- Bergstrom, E.K.; Lingstrom, P.; Hakeberg, M.; Gahnberg, L.; Skold, U.M. Caries and costs: An evaluation of a school-based fluoride varnish programme for adolescents in a Swedish region. Community Dent. Health 2016, 33, 138–144. [Google Scholar] [CrossRef]
- Sköld, U. Approximal caries increment in relation to baseline approximal caries prevalence among adolescents in Sweden with and without a school-based fluoride varnish programme. Community Dent. Health 2016, 33, 281–285. [Google Scholar] [CrossRef]
- Griffin, S.; Naavaal, S.; Scherrer, C.; Griffin, P.M.; Harris, K.; Chattopadhyay, S. School-based dental sealant programs prevent cavities and are cost-effective. Health Aff. (Millwood) 2016, 35, 2233–2240. [Google Scholar] [CrossRef]
- Griffin, S.O.; Naavaal, S.; Scherrer, C.; Patel, M.; Chattopadhyay, S. Evaluation of School-Based Dental Sealant Programs: An Updated Community Guide Systematic Economic Review. Am. J. Prev. Med. 2017, 52, 407–415. [Google Scholar] [CrossRef] [PubMed]
- Neidell, M.; Shearer, B.; Lamster, I.B. Cost-Effectiveness Analysis of Dental Sealants versus Fluoride Varnish in a School-Based Setting. Caries Res. 2016, 50, 78–82. [Google Scholar] [CrossRef]
- Marinho, V.; Worthington, H.; Walsh, T.; Clarkson, J. Fluoride varnishes for preventing dental caries in children and adolescents. Cochrane Database Syst. Rev. 2013, 11, CD002279. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, T.M.N.; Tonmukayakul, U.; Warren, E.; Cartwright, S.; Liew, D. A Markov cost-effective analysis of biannual fluoride varnish for preventing dental caries in permanent teeth over a 70-year time horizon. Health Promot. J. Austr. 2020, 31, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Rogers, J.; Delany, C.; Wright, C.; Roberts-Thomson, K.; Morgan, M. What factors are associated with dental general anaesthetics for Australian children and what are the policy implications? A qualitative study. BMC Oral Health 2018, 18, 174. [Google Scholar] [CrossRef] [PubMed]
- Newhouse, J. Consumer-Directed Health Plans and the RAND Health Insurance Experiment. Health Aff. 2004, 23, 107–113. [Google Scholar] [CrossRef] [PubMed]
- Lamont, T.; Worthington, H.V.; Clarkson, J.E.; Beirne, P.V. Routine scale and polish for periodontal health in adults. Cochrane Database Syst. Rev. 2018, 27, CD004625. [Google Scholar] [CrossRef]
| Demographics and Social History | Standard Care (n = 163) n (%) | Intervention (n = 168) n (%) | p-Value |
|---|---|---|---|
| Mean Age (SD) (y) | 7.3 (2.8) | 6.2 (2.8) | 0.001 * |
| Sex | |||
| Female | 92 (56%) | 78 (46%) | Reference |
| Male | 71 (44%) | 90 (54%) | 0.068 |
| Cultural Background (ASCCEG Classification) | |||
| Not Stated | 5 (3%) | 9 (5%) | - |
| Multiracial | 22 (13%) | 15 (9%) | - |
| Oceanian | 60 (37%) | 20 (12%) | - |
| Southern and Eastern European | 14 (9%) | 9 (5%) | - |
| North-West European | 12 (7%) | 3 (2%) | - |
| North-East Asian | 2 (1%) | 8 (4%) | - |
| South-East Asian | 5 (3%) | 9 (5%) | - |
| Southern and Central Asian | 27 (17%) | 46 (27%) | - |
| North African and Middle Eastern | 16 (10%) | 44 (26%) | - |
| Sub-Saharan African | 0 (0%) | 5 (3%) | - |
| Principal Place of Residence (SEIFA Classification) | |||
| 1–5 | 47 (29%) | 153 (91%) | Reference |
| 6–10 | 116 (71%) | 15 (9%) | 0.001 * |
| Household Income | |||
| Not Stated | 24 (14%) | 36 (21%) | - |
| <$50,000 | 71 (44%) | 77 (46%) | Reference |
| ≥$50,000 | 68 (42%) | 55 (33%) | 0.231 |
| Card-holder Status | |||
| Yes | 88 (54%) | 77 (46%) | Reference |
| No | 75 (46%) | 91 (54%) | 0.138 |
| CDBS Eligibility | |||
| Yes | 84 (52%) | 87 (52%) | Reference |
| No | 79 (48%) | 81 (48%) | 0.962 |
| Has Private Health Insurance | |||
| Yes | 34 (21%) | 27 (16%) | Reference |
| No | 129 (79%) | 141 (84%) | 0.261 |
| Dental History | Standard Care (n = 163) n (%) | Intervention (n = 168) n (%) | p-Value |
|---|---|---|---|
| Duration Since Last Dental Check-up | |||
| Never | 33 (20%) | 76 (45%) | Reference |
| Had previously a dental check-up | 130 (80%) | 92 (55%) | <0.001 * |
| <6 Months | 26 (16%) | 36 (21%) | - |
| 7–12 Months | 80 (49%) | 36 (21%) | - |
| 13–24 Months | 16 (10%) | 11 (6%) | - |
| >24 Months | 8 (5%) | 9 (5%) | - |
| Is a Previous Patient with Dianella Plenty Valley Health | |||
| Yes | 97 (60%) | 49 (29%) | Reference |
| No | 66 (40%) | 119 (71%) | <0.001 * |
| Previous Dental Service Type | |||
| Not Applicable | 29 (18%) | 77 (46%) | - |
| Public | 100 (61%) | 54 (32%) | - |
| Private | 29 (18%) | 31 (18%) | - |
| Overseas | 5 (3%) | 6 (4%) | - |
| Missed School Due to Dental Pain | |||
| Yes | 14 (9%) | 14 (8%) | Reference |
| No | 149 (91%) | 154 (92%) | 0.933 |
| Frequency of Missing School Due to Dental Pain | |||
| Never | 149 (91%) | 154 (92%) | - |
| Sometimes | 3 (2%) | 0 (0%) | Reference |
| Frequently | 11 (7%) | 14 (8%) | 0.067 |
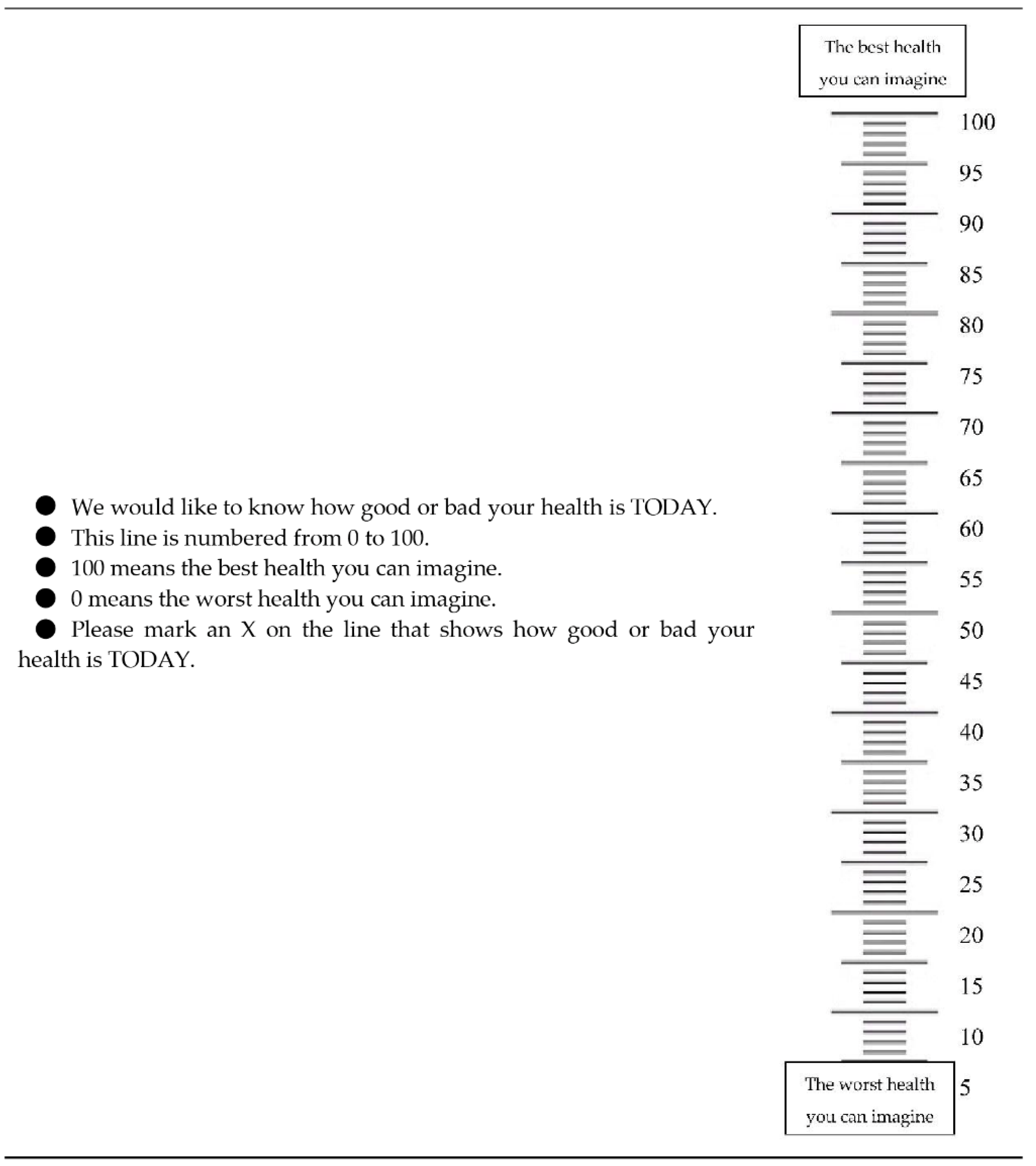
| EQ-5D-Y Dimension | Standard Care (n = 60) n (%) | Intervention (n = 40) n (%) | p-Value | |
|---|---|---|---|---|
| Mobility | No Problems | 58 (97%) | 35 (87%) | Reference |
| Problems | 2 (3%) | 5 (13%) | 0.078 | |
| Looking After Myself | No Problems | 56 (93%) | 31 (77%) | Reference |
| Problems | 4 (7%) | 9 (23%) | 0.021 * | |
| Doing Usual Activities | No Problems | 56 (93%) | 36 (90%) | Reference |
| Problems | 4 (7%) | 5 (10%) | 0.547 | |
| Having Pain or Discomfort | No Problems | 52 (87%) | 26 (65%) | Reference |
| Problems | 8 (13%) | 14 (35%) | 0.010 * | |
| Feeling Worried, Sad or Unhappy | No Problems | 52(87%) | 29 (72%) | Reference |
| Problems | 8 (13%) | 11 (28%) | 0.078 | |
| EQ VAS Data | ||||
| Mean (SD) | 90.7 (13.2) | 81.9 (18.0) | - | |
| 25th Percentile | 85 | 70 | - | |
| 50th Percentile | 97 | 82.5 | - | |
| 75th Percentile | 100 | 100 | - | |
| Health Status and Dental Care Characteristics | Standard Care (n = 163) n (%) | Intervention (n = 168) n (%) | p-Value |
|---|---|---|---|
| Weight Status | |||
| Unknown | 3 (2%) | 8 (5%) | - |
| Below Healthy Weight | 33 (20%) | 22 (13%) | - |
| Above Healthy Weight | 13 (8%) | 26 (15%) | - |
| Well Above Healthy Weight | 17 (10%) | 40 (24%) | - |
| Healthy Weight | 97 (60%) | 72 (43%) | Reference |
| Unhealthy Weight | 63 (39%) | 88 (55%) | 0.005 * |
| Untreated Dental Caries Baseline (Modified ICDAS II [20] | |||
| d2 | 2.40 (3.1) | 1.40 (2.2) | 0.001 * |
| d3–6 | 0.93 (1.8) | 1.39 (2.5) | 0.056 |
| D2 | 1.07 (2.1) | 0.57 (1.3) | 0.010 * |
| D3–6 | 0.19 (0.6) | 0.18 (0.7) | 0.873 |
| Untreated Cavitated Dental Caries at Follow-Up | |||
| d | 0.38 (1.1) | 0.64 (1.7) | 0.094 |
| D | 0.04 (0.2) | 0.05 (0.3) | 0.590 |
| Referred for Dental Treatment | |||
| Yes | 75 (46%) | 104 (62%) | Reference |
| No | 88 (54%) | 64 (38%) | 0.004 * |
| Received Surgical Dental Treatment | |||
| Yes | 46 (28%) | 41 (24%) | Reference |
| No | 117 (72%) | 127 (76%) | 0.430 |
| Child Retention Rates at Follow-Up | |||
| Yes | 71 (95%) | 76 (75%) | Reference |
| No | 4 (5%) | 25 (25%) | 0.001 * |
| Null Hypothesis Test (Intervention Only) | - | 75% | 0.954 |
| Dental Treatment Time (SD) (min) | 115.1 (120.6) | 79.6 (79.1) | 0.002 * |
| Number of Dental Visits (SD) | 3.2 (2.5) | 2.6 (1.7) | 0.011 * |
| Travel Costs (SD) (AU$) | 19.0 (27.3) | 8.0 (10.9) | 0.001 * |
| Dental Treatment Time Cost (SD) (AU$) | 40.4 (41.8) | 28.0 (28.4) | 0.002 * |
| Dental Treatment Cost (SD) (AU$) | |||
| Unadjusted | 695.4 (627.8) | 585.1 (516.5) | 0.081 |
| Adjusted | - | 517.6 (517.4) | 0.005 * |
| Total Society Cost (SD) (AU$) | |||
| Unadjusted | 754.7 (674.9) | 621.2 (547.8) | 0.049 * |
| Adjusted | - | 533.8 (548.8) | 0.003 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen, T.M.; Christian, B.; Koshy, S.; Morgan, M.V. A Validation and Cost-Analysis Study of a Targeted School-Based Dental Check-Up Intervention: Children’s Dental Program. Children 2020, 7, 257. https://doi.org/10.3390/children7120257
Nguyen TM, Christian B, Koshy S, Morgan MV. A Validation and Cost-Analysis Study of a Targeted School-Based Dental Check-Up Intervention: Children’s Dental Program. Children. 2020; 7(12):257. https://doi.org/10.3390/children7120257
Chicago/Turabian StyleNguyen, Tan Minh, Bradley Christian, Sajeev Koshy, and Michael Vivian Morgan. 2020. "A Validation and Cost-Analysis Study of a Targeted School-Based Dental Check-Up Intervention: Children’s Dental Program" Children 7, no. 12: 257. https://doi.org/10.3390/children7120257
APA StyleNguyen, T. M., Christian, B., Koshy, S., & Morgan, M. V. (2020). A Validation and Cost-Analysis Study of a Targeted School-Based Dental Check-Up Intervention: Children’s Dental Program. Children, 7(12), 257. https://doi.org/10.3390/children7120257





