Fundamental Motor Skills Intervention for Children with Autism Spectrum Disorder: A 10-Year Narrative Review
Abstract
:1. Introduction
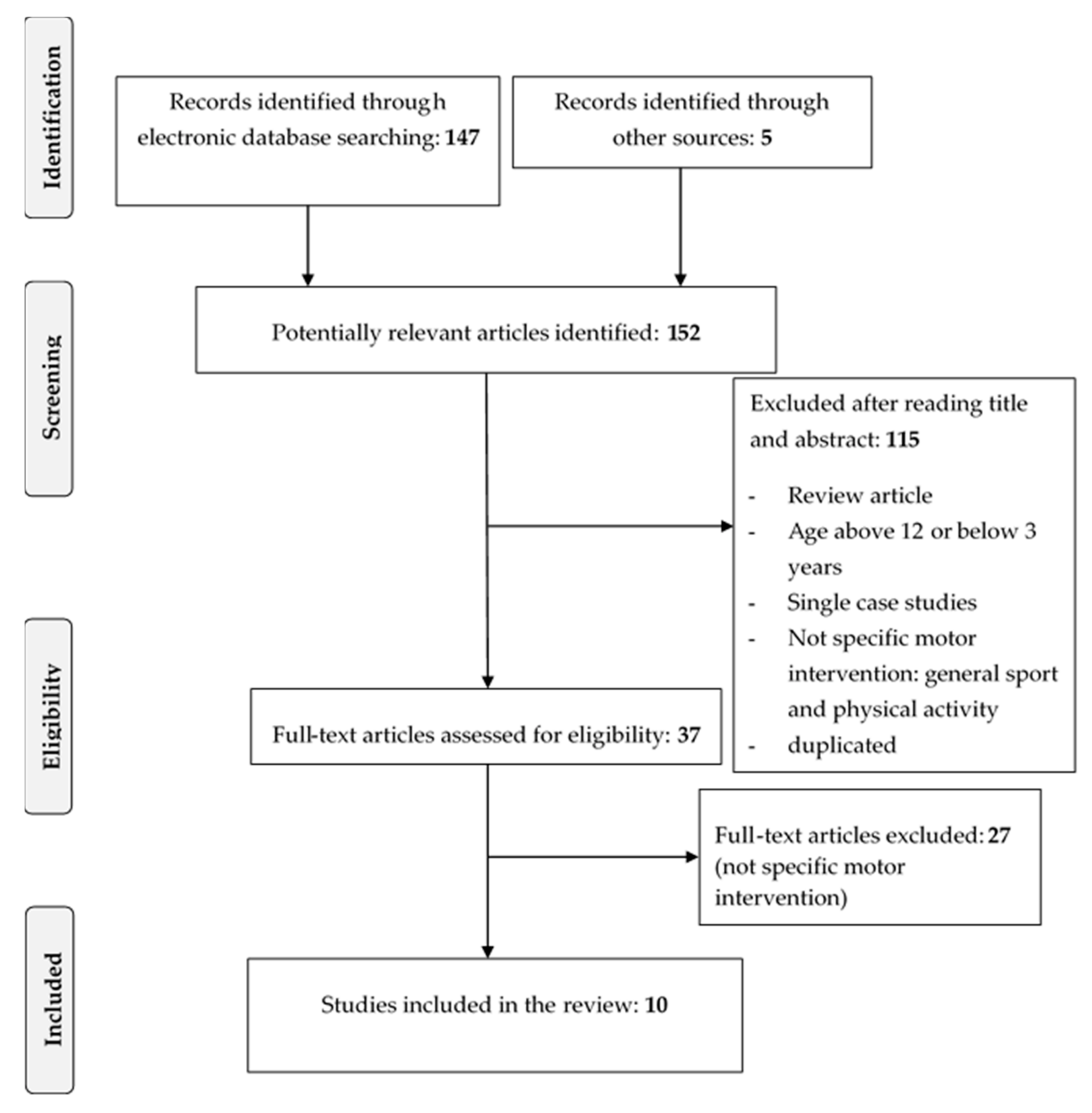
2. Methods
3. Results
3.1. Participants: Clinical and Demographic Characteristics
3.2. Studies Designs
3.3. Types of the Interventions
3.4. Durations of the Interventions
3.5. Settings
3.6. Outcome Measures and Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-V-TR); American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Gowen, E.; Hamilton, A. Motor abilities in autism: A review using a computational context. J. Autism Dev. Disord. 2013, 43, 323–344. [Google Scholar] [CrossRef]
- Fournier, K.A.; Hass, C.J.; Naik, S.K.; Lodha, N.; Cauraugh, J.H. Motor coordination in autism spectrum disorders: A synthesis and meta-analysis. J. Autism Dev. Disord. 2010, 40, 1227–1240. [Google Scholar] [CrossRef] [PubMed]
- Bhat, A.N. Is Motor Impairment in Autism Spectrum Disorder Distinct from Developmental Coordination Disorder? A Report from the SPARK Study. Phys. Ther. 2020, 100, 633–644. [Google Scholar] [CrossRef]
- Srinivasan, S.M.; Kaur, M.; Park, I.K.; Gifford, T.D.; Marsh, K.L.; Bhat, A. The Effects of Rhythm and Robotic Interventions on the Imitation/Praxis, Interpersonal Synchrony, and Motor Performance of Children with Autism Spectrum Disorder (ASD): A Pilot Randomized Controlled Trial. Autism Res. Treat. 2015, 2015, 736516. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bremer, E.; Crozier, M.; Lloyd, M. A systematic review of the behavioural outcomes following exercise interventions for children and youth with autism spectrum disorder. Autism 2016, 20, 899–915. [Google Scholar] [CrossRef] [PubMed]
- Bryson, S.E.; Zwaigenbaum, L.; Brian, J.; Roberts, W.; Szatmari, P.; Rombough, V.; McDermott, C. A Prospective Case Series of High-risk Infants who Developed Autism. J. Autism Dev. Disord. 2007, 37, 12–24. [Google Scholar] [CrossRef] [PubMed]
- Esposito, G.; Venuti, P. Analysis of Toddlers’ Gait after Six Months of Independent Walking to Identify Autism: A Preliminary Study. Percept. Mot. Ski. 2008, 106, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Phagava, H.; Muratori, F.; Einspieler, C.; Maestro, S.; Apicella, F.; Guzzetta, A.; Prechtl, H.F.R.; Cioni, G. General movements in infants with autism spectrum disorders. Georgian Med. News 2008, 156, 100–105. [Google Scholar]
- Esposito, G.; Venuti, P.; Apicella, F.; Muratori, F. Analysis of unsupported gait in toddlers with autism. Brain Dev. 2011, 33, 367–373. [Google Scholar] [CrossRef]
- Sacrey, L.-A.R.; Bennett, J.A.; Zwaigenbaum, L. Early Infant Development and Intervention for Autism Spectrum Disorder. J. Child Neurol. 2015, 30, 1921–1929. [Google Scholar] [CrossRef]
- Iverson, J.M. Early Motor and Communicative Development in Infants with an Older Sibling with Autism Spectrum Disorder. J. Speech Lang. Heart Res. 2018, 61, 2673–2684. [Google Scholar] [CrossRef] [PubMed]
- Landa, R.J.; Gross, A.L.; Stuart, E.A.; Bauman, M. Latent class analysis of early developmental trajectory in baby siblings of children with autism. J. Child Psychol. Psychiatry 2012, 53, 986–996. [Google Scholar] [CrossRef] [Green Version]
- Landa, R.J.; Gross, A.L.; Stuart, E.A.; Faherty, A. Developmental Trajectories in Children with and without Autism Spectrum Disorders: The First 3 Years. Child Dev. 2013, 84, 429–442. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lloyd, M.; Macdonald, M.; Lord, C. Motor skills of toddlers with autism spectrum disorders. Autism 2013, 17, 133–146. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ulrich, D. Test of Gross Motor Development, 2nd ed.; Examiner’s Manual: Austin, TX, USA, 2000. [Google Scholar]
- Pellegrini, A.D.; Smith, P. Physical Activity Play: The Nature and Function of a Neglected Aspect of Play. Child Dev. 1998, 69, 577–598. [Google Scholar] [CrossRef]
- Reinders, N.J.; Branco, A.; Wright, K.; Fletcher, P.C.; Bryden, P.J. Scoping Review: Physical Activity and Social Functioning in Young People with Autism Spectrum Disorder. Front. Psychol. 2019, 10, 120. [Google Scholar] [CrossRef] [Green Version]
- Esposito, G.; Paşca, S.P. Motor abnormalities as a putative endophenotype for Autism Spectrum Disorders. Front. Integr. Neurosci. 2013, 7, 43. [Google Scholar] [CrossRef] [Green Version]
- Leary, M.R.; Hill, D.A. Moving on: Autism and movement disturbance. Ment. Retard. 1996, 34, 39–53. [Google Scholar]
- Baranek, G.T. Efficacy of Sensory and Motor Interventions for Children with Autism. J. Autism Dev. Disord. 2002, 32, 397–422. [Google Scholar] [CrossRef]
- Scharoun, S.M.; Wright, K.T.; Robertson-Wilson, P.C.F.J.E.; Bryden, P.J. Physical Activity in Individuals with Autism Spectrum Disorders (ASD): A Review. In Autism: Paradigms, Recent Research and Clinical Applications; BoD—Books on Demand: Norderstedt, Germany, 2017. [Google Scholar]
- Bishop, J.C.; Pangelinan, M.M. Motor skills intervention research of children with disabilities. Res. Dev. Disabil. 2018, 74, 14–30. [Google Scholar] [CrossRef]
- Healy, S.; Nacario, A.; Braithwaite, R.E.; Hopper, C. The effect of physical activity interventions on youth with autism spectrum disorder: A meta-analysis. Autism Res. 2018, 11, 818–833. [Google Scholar] [CrossRef] [PubMed]
- Lang, R.; Koegel, L.K.; Ashbaugh, K.; Regester, A.; Ence, W.; Smith, W. Physical exercise and individuals with autism spectrum disorders: A systematic review. Res. Autism Spectr. Disord. 2010, 4, 565–576. [Google Scholar] [CrossRef]
- Sorensen, C.; Zarrett, N. Benefits of Physical Activity for Adolescents with Autism Spectrum Disorders: A Comprehensive Review. Rev. J. Autism Dev. Disord. 2014, 1, 344–353. [Google Scholar] [CrossRef]
- Sowa, M.; Meulenbroek, R. Effects of physical exercise on Autism Spectrum Disorders: A meta-analysis. Res. Autism Spectr. Disord. 2012, 6, 46–57. [Google Scholar] [CrossRef]
- Colombo-Dougovito, A.M.; Block, M.E. Fundamental Motor Skill Interventions for Children and Adolescents on the Autism Spectrum: A Literature Review. Rev. J. Autism Dev. Disord. 2019, 6, 159–171. [Google Scholar] [CrossRef]
- Case, L.; Yun, J. The Effect of Different Intervention Approaches on Gross Motor Outcomes of Children with Autism Spectrum Disorder: A Meta-Analysis. Adapt. Phys. Act. Q. 2019, 36, 501–526. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Functioning, Disability and Health: Children and Youth Version: ICF-CY; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- Mahdi, S.; Albertowski, K.; Almodayfer, O.; Arsenopoulou, V.; Carucci, S.; Dias, J.C.; Khalil, M.; Knüppel, A.; Langmann, A.; Lauritsen, M.B.; et al. An International Clinical Study of Ability and Disability in Autism Spectrum Disorder Using the WHO-ICF Framework. J. Autism Dev. Disord. 2018, 48, 2148–2163. [Google Scholar] [CrossRef] [Green Version]
- Bremer, E.; Balogh, R.; Lloyd, M. Effectiveness of a fundamental motor skill intervention for 4-year-old children with autism spectrum disorder: A pilot study. Autism 2014, 19, 980–991. [Google Scholar] [CrossRef]
- Edwards, J.; Jeffrey, S.; May, T.; Rinehart, N.J.; Barnett, L.M. Does playing a sports active video game improve object control skills of children with autism spectrum disorder? J. Sport Health Sci. 2017, 6, 17–24. [Google Scholar] [CrossRef]
- Felzer-Kim, I.T.; Hauck, J.L. How Much Instructional Time Is Necessary? Mid-intervention Results of Fundamental Movement Skills Training within ABA Early Intervention Centers. Front. Integr. Neurosci. 2020, 14, 24. [Google Scholar] [CrossRef]
- Guest, L.; Balogh, R.; Dogra, S.; Lloyd, M. Examining the Impact of a Multi-Sport Camp for Girls Ages 8–11 with Autism Spectrum Disorder. Ther. Recreat. J. 2017, 51, 109–126. [Google Scholar] [CrossRef]
- Hassani, F.; Shahrbanian, S.; Shahidi, S.H.; Sheikh, M. Playing games can improve physical performance in children with autism. Int. J. Dev. Disabil. 2020, 1–8. [Google Scholar] [CrossRef]
- Henderson, H.; Fuller, A.; Noren, S.; Stout, V.M.; Williams, D. The effects of a physical education program on the motor skill performance of children with autism spectrum disorder. Palaestra 2016, 30, 41–50. [Google Scholar]
- Ketcheson, L.; Hauck, J.; Ulrich, D. The effects of an early motor skill intervention on motor skills, levels of physical activity, and socialization in young children with autism spectrum disorder: A pilot study. Autism 2017, 21, 481–492. [Google Scholar] [CrossRef]
- Pfeiffer, B.A.; Koenig, K.; Kinnealey, M.; Sheppard, M.; Henderson, L. Effectiveness of sensory integration interventions in children with autism spectrum disorders: A pilot study. Am. J. Occup. Ther. 2011, 65, 76–85. [Google Scholar] [CrossRef] [Green Version]
- Wiart, L.; Darrah, J. Review of four tests of gross motor development. Dev. Med. Child Neurol. 2001, 43, 279–285. [Google Scholar] [CrossRef]
- Odom, S.L.; Thompson, J.L.; Hedges, S.; Boyd, B.A.; Dykstra, J.R.; Duda, M.A.; Szidon, K.L.; Smith, L.E.; Bord, A. Technology-Aided Interventions and Instruction for Adolescents with Autism Spectrum Disorder. J. Autism Dev. Disord. 2015, 45, 3805–3819. [Google Scholar] [CrossRef]
- Srinivasan, S.M.; Lynch, K.A.; Bubela, D.J.; Gifford, T.D.; Bhat, A.N. Effect of Interactions between a Child and a Robot on the Imitation and Praxis Performance of Typically Devloping Children and a Child with Autism: A Preliminary Study. Percept. Mot. Ski. 2013, 116, 885–904. [Google Scholar] [CrossRef]
- Pennisi, P.; Tonacci, A.; Tartarisco, G.; Billeci, L.; Ruta, L.; Gangemi, S.; Pioggia, G. Autism and social robotics: A systematic review. Autism Res. 2016, 9, 165–183. [Google Scholar] [CrossRef]
- Casellato, C.; Gandolla, M.; Crippa, A.; Pedrocchi, A. Robotic set-up to quantify hand-eye behavior in motor execution and learning of children with autism spectrum disorder. In Proceedings of the 2017 International Conference on Rehabilitation Robotics (ICORR), London, UK, 17–20 July 2017; pp. 953–958. [Google Scholar]
- Bellani, M.; Fornasari, L.; Chittaro, L.; Brambilla, P. Virtual reality in autism: State of the art. Epidemiol. Psychiatr. Sci. 2011, 20, 235–238. [Google Scholar] [CrossRef]
- Biffi, E.; Costantini, C.; Ceccarelli, S.B.; Cesareo, A.; Marzocchi, G.M.; Nobile, M.; Molteni, M.; Crippa, A. Gait Pattern and Motor Performance During Discrete Gait Perturbation in Children With Autism Spectrum Disorders. Front. Psychol. 2018, 9. [Google Scholar] [CrossRef] [PubMed]
- Yang, D.Y.-J.; Allen, T.; Abdullahi, S.M.; Pelphrey, K.A.; Volkmar, F.R.; Chapman, S.B. Neural mechanisms of behavioral change in young adults with high-functioning autism receiving virtual reality social cognition training: A pilot study. Autism Res. 2018, 11, 713–725. [Google Scholar] [CrossRef] [PubMed]
- Donnellan, A.M.P.; Hill, D.A.M.; Leary, M.R.M. Rethinking autism: Implications of sensory and movement differences for understanding and support. Front. Integr. Neurosci. 2013, 6, 124. [Google Scholar] [CrossRef] [Green Version]
- Trevarthen, C.; Delafield-Butt, J.T. Autism as a developmental disorder in intentional movement and affective engagement. Front. Integr. Neurosci. 2013, 7, 49. [Google Scholar] [CrossRef] [Green Version]
- Ruggeri, A.; Dancel, A.; Johnson, R.; Sargent, B. The effect of motor and physical activity intervention on motor outcomes of children with autism spectrum disorder: A systematic review. Autism 2019, 24, 544–568. [Google Scholar] [CrossRef] [PubMed]
- Crippa, A.; Tesei, A.; Sangiorgio, F.; Salandi, A.; Trabattoni, S.; Grazioli, S.; Agostoni, C.; Molteni, M.; Nobile, M. Behavioral and cognitive effects of docosahexaenoic acid in drug-naïve children with attention-deficit/hyperactivity disorder: A randomized, placebo-controlled clinical trial. Eur. Child Adolesc. Psychiatry 2018, 28, 571–583. [Google Scholar] [CrossRef]
- Piccin, S.; Crippa, A.; Nobile, M.; Hardan, A.Y.; Brambilla, P. Video modeling for the development of personal hygiene skills in youth with autism spectrum disorder. Epidemiol. Psychiatr. Sci. 2017, 27, 127–132. [Google Scholar] [CrossRef]
- Rosenberg, N.; Schwartz, I.; Davis, N.C.A. Evaluating the Utility of Commercial Videotapes for Teaching Hand Washing to Children with Autism. Educ. Treat. Child. 2010, 33, 443–455. [Google Scholar] [CrossRef]
| Study | Location | Study Type | Participants (N, Groups) | Age Range (Mean ± SD) | Intervention Approach | Intervention Length | Setting | Outcome Measures | Results |
|---|---|---|---|---|---|---|---|---|---|
| Bremer et al. [6] | Canada | Multiple-method study with pre-/posttest | N = 5 (4 ASD, 1 autism-like characteristics) One group (1f/4m) | 3–7 years (5.46 ± 1.49) | Fundamental motor skill intervention (FMSI): each session focused on teaching and strengthening of both locomotor and object control skills. Each week focused on teaching one core skill with previously learned skills integrated into the sessions. | 12 weeks split into two blocks (each block: 45 min per day for 3 days per week) for a total of 36 sessions | Local elementary school |
| Improvements on the majority of the individual TGMD-2 items, 4 of the participants showed improvements in locomotor skills, furthermore 3 of the participants in object-control from Assessments 1–3. Improvements in SSIS on all items. The special education teacher noted the increase of motor skills and knowledge in the participants, the treatment program could be easily generalized and her own perception of her ability to teach physical education improved. |
| Bremer et al. [32] | Canada | Wait-list control experimental design with pre-/post-follow up test | N = 9 ASD 2 groups: EG N = 5 (5m); CG N = 4 (1f/3m) | 4 years (EG = 4.30 ± 0.25; CG = 4.33 ± 0.22) | Fundamental motor skill intervention (FMSI): each session focused on teaching and strengthening of both locomotor and object control skills (they progressed in difficulty over the intervention period), while integrating previously learned skills into the review period and obstacle course. | Phase I: group 1 attended a 12-week FMS intervention for 1 h per week, while group 2 acted as a control. Phase II: group 2 attended a 6-week FMS intervention for 2 h each week (1 h per day on 2 separate days) | Local Children’s Treatment Centre |
| Intervention effectiveness: higher scores on object manipulation and total motor quotient PDMS-2 for EG compared to CG. No significant differences between two groups regarding adaptive behavior (VABS-2) and social skills (SSIS). Intensity effectiveness: time played a role on all PDMS-2 variables but not on adaptive behavior and social skills. No differences were found on outcomes between the two intervention intensities. |
| Edwards et al. [33] | Australia | Pre- and posttest experimental design | N = 30 (11 ASD, 8m/3f; 19 TD, 10m/9f) | 6–10 years (ASD = 7.64 ± 1.12; TD = 7.89 ± 1.45) | Active Video Games (AVGs) like Kinect Sports Season 1, Kinect Sports Season 2, Sports Rivals and Kinect Adventures (TD group only). | ASD = 6 session (45/60 min each one, 3 times per week for 2 weeks) TD = 6 session (50 min each one, once a week for 6 weeks) | For ASD at home, for TD group at school during lunchtime |
| There was no increase between pre- and postintervention for actual OC skill both in ASD and in TD group. Only in children with ASD, there was an increase of perception of skill. |
| Felzer-Kim and Lynn Hauck [34] | USA | RCT; pre-/posttest design | N = 14 ASD 2 groups: EG (1f/7m); CG (3f/3m) | 4 years (EG = 4.5 ± 0.6; CG = 4.5 ± 0.6) | Fundamental motor skill intervention (FMSI): each session focused on training one of the 13 FMS. Each trial consisted of viewing a tablet-displayed video of the FMS, a picture task card and a verbal instruction. Then participants completed one trial of the skill, with physical prompt and reinforcement. | 20 weeks split into two blocks (each block: 15 min per day for 4 days per week) for a total of 20 h | Campus of an ABA EIBI clinic |
| No significant interaction between time*group was found: 10 h of intervention did not alter FMS in this sample. Time*group interaction approached significance for ball skills and total but more time is necessary. Overall, locomotor skill improvement seems to be lower than ball skills and total skills. |
| Guest et al. [35] | Canada | Pre-/posttest quasi-experimental design with follow-up 8 weeks later. | 15 ASD (13f) | 8–11 (9.76 ± 1.00) | Special Olympics FUNdamentals program based on Long Term Athlete Development Model (LTAD) focused on locomotor skills and object control skills. Motor skills were incorporated into active group games and became difficult throughout the week. | Five full-day | School gymnasium |
| Significant improvement after the intervention in Test of Gross Motor Development-2, physical self-perception in CY-PSPP, and social skills domain in VABS |
| Hassani et al. [36] | IRAN | Pre-/posttest design | 30 ASD (10f/20m) 3 groups: EG-training 1 (4f/6m); EG-training2 (3f/8m); CG (3f/6m) | 8–11 years (EG-training 1 = 9.10 ± 0.87; EG-training 2 = 8.55 ± 0.68; CG = 8.70 ± 0.70) |
| Sixteen indoor sessions, with two sessions of 60 min each per week performed after school. | Sport arena |
| Both treatments incremented gross MS in comparison with the control group, with a major effect of ICPL group. Interestingly ICPL training also improved fine MS, unlike SPARK training. |
| Henderson et al. [37] | USA | Pre-/posttest design | 37 ASD (35m, 2f) | 5–12 (8.4 ± 2.06) | Physical education program targeting the six locomotor and six object control skills of the TGMD-2 | 40 min twice a week for six months, total: 40 classes | Gymnasium at a center for children with ASD |
| Significant improvement after intervention for both gross motor skills and object control skills. |
| Ketcheson et al. [38] | USA | Pre-/post-follow-up test design | N = 20 ASD 2 groups: EG N = 11 (2f/9m); CT N = 9 (3f/6m) | 4–6 years (EG = 4.87 ± 0.61; CG = 5.04 ± 0.61) | The intervention implies a weekly rotation between the Test of Gross Motor Development-2 (TGMD-2) subtests: locomotor skills and object control skills, using the eight components from the Classroom Pivotal Response Teaching (CPRT) manual as the framework for delivery of instruction. | 4 h per day, 5 days per week for 8 weeks | Gymnasium and outdoor environment |
| Significant increase in motor proficiency in EG (locomotor skills, object control and gross quotient TGMD-2) compared with CG. A decrease in solitary scale in POPE was found. For all levels of PA, no significant group differences were observed. For joint engagement, parallel play and onlooking, no significant effects of time were found. |
| Pfeiffer et al. [39] | USA | Pilot study for subsequent randomized controlled trial; pre-/posttest design | N = 37 (21 ASD; 16 PDD-NOS) 2 groups: EG N = 20 (3f/17m); CG N = 17 (2f/15m) | 6–12 years (EG = 8.3 ± 2.06; CG = 9.21 ± 2.06) |
| 18 treatment interventions of 45 min each for 6 weeks | Three areas with appropriate equipment for SI; a separate room for FM. |
| Decrease in mannerisms (a subscale of the SRS) in SI group; both groups showed significant improvement on the GAS, although the improvement was significantly greater in SI group. No significant differences between the two groups on sensory processing standardized scores (SPM), other subscales of SRS and the QNST–II. |
| Srinivasan et al. [5] | USA | RCT; pre-/posttest | N = 36 ASD 3 groups: EG1 N = 12 (2f/10m); EG2 N = 12 (1f/11m); CG N = 12 (1f/11m). | 5–12 years (EG1 = 7.88 ± 2.56; EG2 = 7.52 ± 2.22; CG = 7.36 ± 2.02) | In the Rhythm and Robot group, gross motor skills including balance, bilateral coordination, imitation, interpersonal synchrony, and manual dexterity were trained whereas in the comparison group fine motor skills such as symmetrical and asymmetrical grips and pinches, coloring, drawing, cutting, and gluing were promoted. In all three groups, training enhanced social communication skills. | 32 sessions (16 expert and 16 parent sessions) of 45 min each one over 8 weeks | Participants’ home |
| Improvements in body coordination for both rhythm and robot group. Improvements on the fine manual control composite for the control group. Improvements on Imitation/praxis for all groups and on interpersonal synchrony for the two EGs. No improvement in fine motor performance for both rhythm and robot group. No improvement in the body coordination composite for the control group. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Busti Ceccarelli, S.; Ferrante, C.; Gazzola, E.; Marzocchi, G.M.; Nobile, M.; Molteni, M.; Crippa, A. Fundamental Motor Skills Intervention for Children with Autism Spectrum Disorder: A 10-Year Narrative Review. Children 2020, 7, 250. https://doi.org/10.3390/children7110250
Busti Ceccarelli S, Ferrante C, Gazzola E, Marzocchi GM, Nobile M, Molteni M, Crippa A. Fundamental Motor Skills Intervention for Children with Autism Spectrum Disorder: A 10-Year Narrative Review. Children. 2020; 7(11):250. https://doi.org/10.3390/children7110250
Chicago/Turabian StyleBusti Ceccarelli, Silvia, Camilla Ferrante, Erica Gazzola, Gian Marco Marzocchi, Maria Nobile, Massimo Molteni, and Alessandro Crippa. 2020. "Fundamental Motor Skills Intervention for Children with Autism Spectrum Disorder: A 10-Year Narrative Review" Children 7, no. 11: 250. https://doi.org/10.3390/children7110250
APA StyleBusti Ceccarelli, S., Ferrante, C., Gazzola, E., Marzocchi, G. M., Nobile, M., Molteni, M., & Crippa, A. (2020). Fundamental Motor Skills Intervention for Children with Autism Spectrum Disorder: A 10-Year Narrative Review. Children, 7(11), 250. https://doi.org/10.3390/children7110250





