Progress in the Management of Paediatric-Onset Multiple Sclerosis
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Statistical Analysis
2.4. Ethical Approval
3. Results
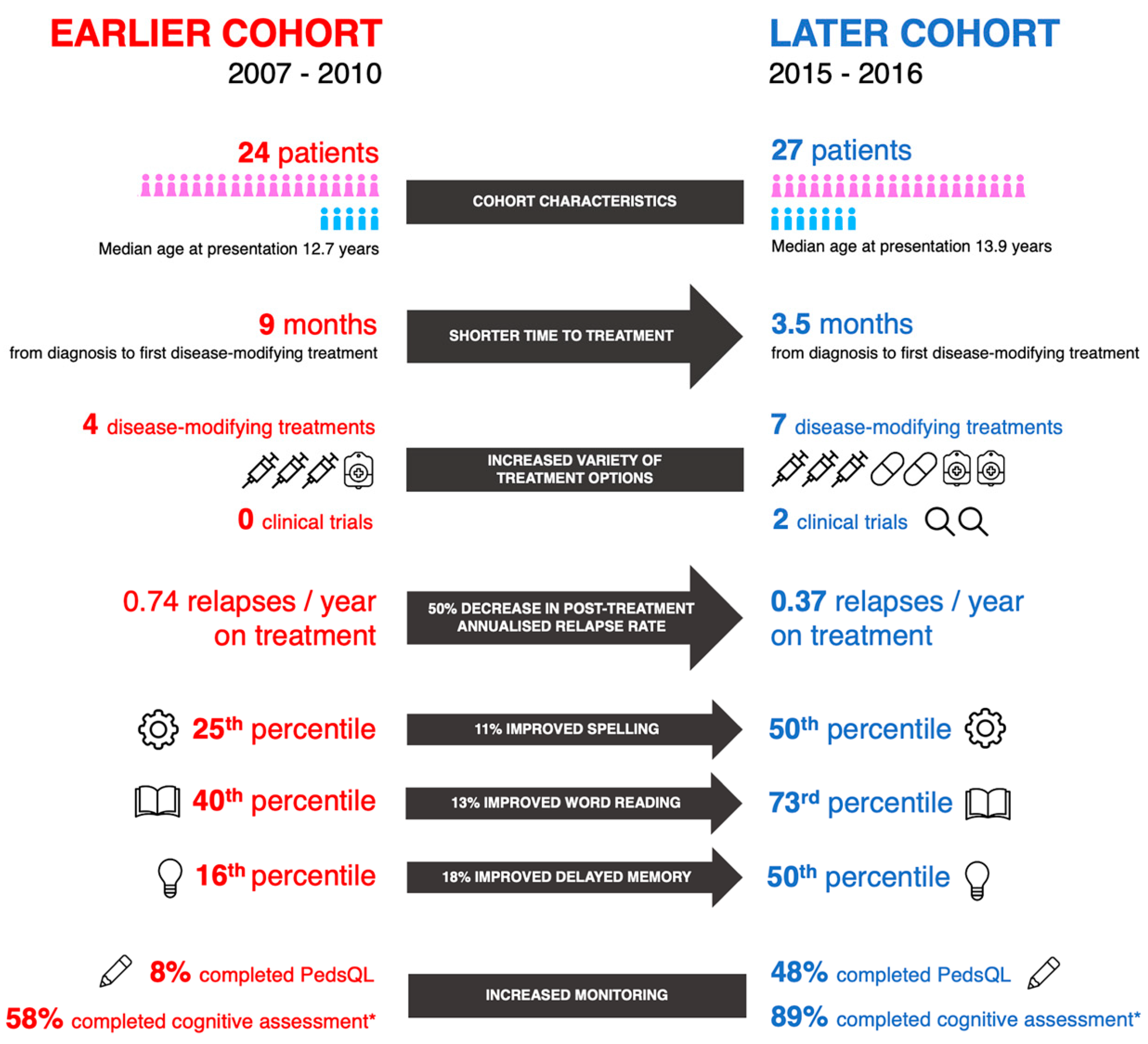
3.1. Cohort Characteristics
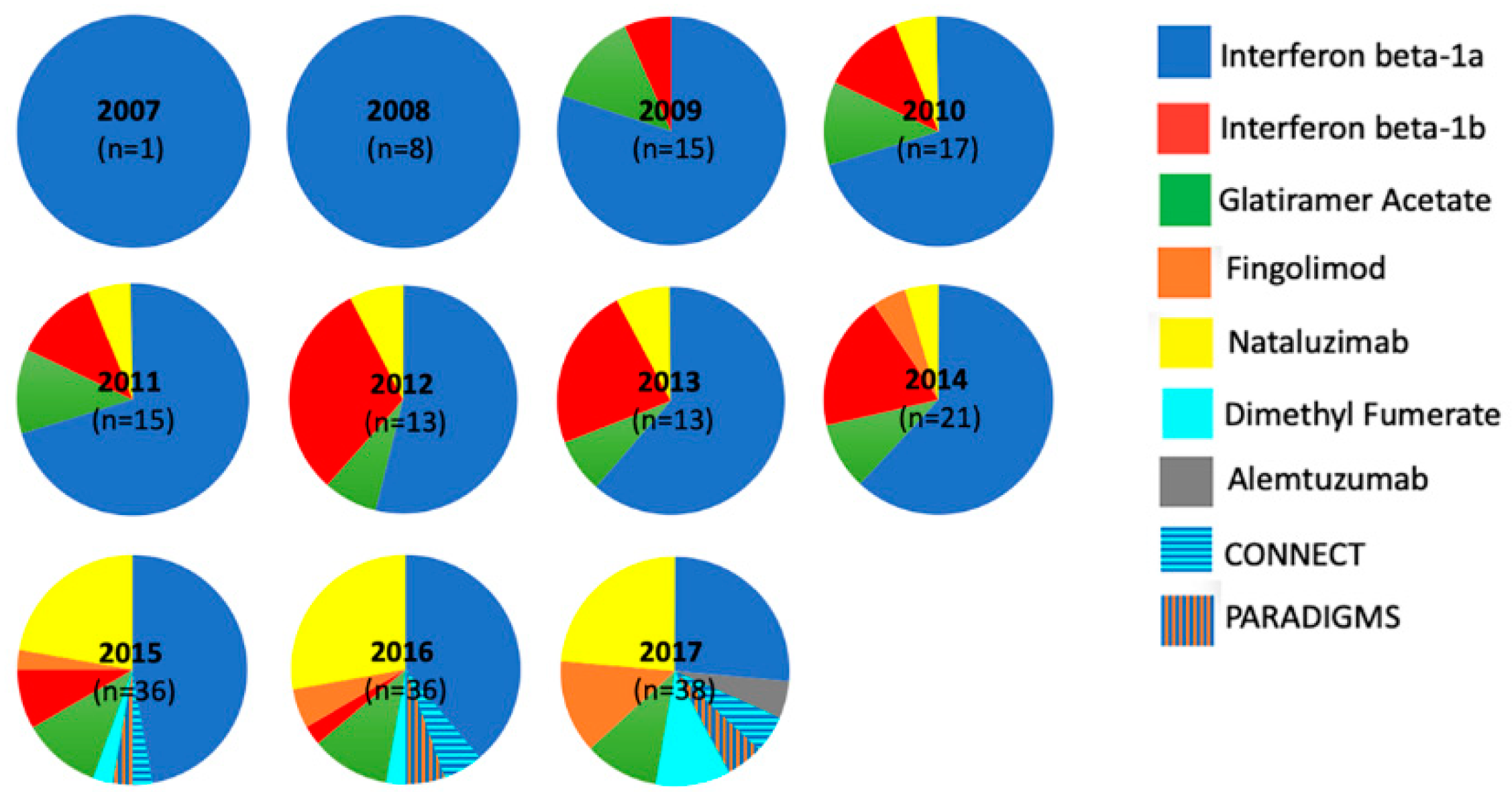
3.2. Changes in Management
3.3. Disease Course
3.4. Cognitive and Quality of Life Outcomes
4. Discussion
4.1. Evolution of Care
4.2. Changes in Outcomes
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Patient | Age at Testing (y) | Time from Onset (m) | FSIQ | WMI | PSI | WR | PD | Sp | NO | VMI | VP | MC | MSI | MSD | Any Impairment |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2 * | 8 | 24 | −3.1 | −2.5 | −1.5 | −1.5 | −0.6 | −1.2 | −3.7 | −1.4 | −2.5 | −2.7 | −1.7 | −1.3 | 1 |
| 3 | 16 | 55 | −2.0 | −2.3 | −3.3 | −1.4 | −1.6 | −0.9 | −3.2 | −2.8 | −3.1 | −3.6 | - | - | 1 |
| 7 * | 14 | 24 | 1.3 | 0.9 | 1.2 | 1.1 | 0.7 | 1.0 | 1.5 | −0.1 | −0.1 | −0.4 | −1.0 | −1.0 | |
| 9 * | 15 | 21 | 1.3 | −0.2 | 1.7 | 0.1 | −0.5 | −0.7 | 1.5 | −0.7 | −0.3 | 0.0 | 1.0 | 0.0 | |
| 10 | 15 | 31 | - | - | - | - | - | - | −0.9 | - | - | - | - | - | |
| 13 * | 13 | 30 | 1.5 | −0.9 | −1.8 | 0.3 | −0.3 | 0.1 | −0.3 | −0.7 | 0.0 | −2.4 | - | - | 1 |
| 14 * | 6 | 34 | 1.5 | −2.3 | −0.2 | −2.7 | −1.3 | −2.1 | 0.0 | −0.2 | −0.5 | −2.0 | - | - | 1 |
| 15 | 14 | 58 | - | −0.2 | −0.6 | 0.5 | 0.8 | −0.3 | −0.3 | 0.3 | −0.1 | 0.4 | −1.3 | −1.7 | |
| 16 | 11 | 11 | - | −2.1 | −2.3 | - | - | - | - | - | - | - | −0.7 | −1.0 | 1 |
| 17 | 12 | 73 | −2.4 | −1.5 | −1.7 | −0.3 | - | −0.3 | −1.9 | - | - | - | −1.0 | −0.3 | 1 |
| 20 | 19 | 34 | −0.1 | 0.1 | −1.6 | - | - | - | - | - | - | - | - | - | |
| 21 | 15 | 11 | −1.9 | −3.3 | −2.5 | −1.3 | - | −0.7 | −0.2 | - | - | - | −0.7 | −0.7 | 1 |
| 22 | 16 | 27 | −0.3 | 1.1 | −1.5 | - | - | - | - | - | - | - | −1.0 | −1.7 | |
| 24 | 15 | 22 | 1.4 | 0.1 | 1.7 | - | - | - | - | - | - | - | - | - | |
| 25 | 14 | 7 | −0.3 | 0.0 | −1.1 | 0.4 | 0.5 | −0.5 | 0.5 | −0.2 | −1.3 | −1.1 | 0.7 | 0.3 | |
| 26 | 11 | 53 | −0.8 | −0.7 | −0.7 | 0.9 | 0.9 | −0.7 | −0.2 | 0.3 | 0.3 | −0.7 | −0.7 | −0.3 | |
| 27 * | 15 | 33 | 0.5 | 0.9 | −0.2 | 0.7 | 0.9 | 0.5 | 0.7 | −1.1 | −0.1 | −0.7 | - | - | |
| 28 | 17 | 42 | −0.7 | 0.7 | −0.7 | 0.5 | 1.2 | 1.0 | 0.9 | −0.3 | −0.1 | −0.4 | - | - | |
| 29 | 16 | 40 | −0.5 | −1.1 | −0.5 | 0.5 | 0.7 | 0.1 | 1.6 | −0.3 | −1.2 | −1.3 | - | - | |
| 31 | 14 | 5 | −0.7 | −1.0 | 0.0 | −1.7 | −1.3 | −1.2 | −1.8 | −0.3 | −2.9 | −1.3 | −1.0 | −1.7 | 1 |
| 32 * | 16 | 33 | −0.7 | −0.5 | 0.0 | 0.1 | 0.7 | 0.3 | 0.3 | −0.9 | −0.4 | −1.0 | −1.0 | −1.0 | |
| 33 * | 17 | 31 | 0.4 | 1.2 | −0.4 | 1.1 | 0.7 | 1.1 | 1.3 | −0.7 | −0.2 | −1.0 | - | - | |
| 34 | 7 | 25 | 0.7 | 0.0 | 0.9 | 1.3 | - | - | - | −0.1 | - | - | - | - | |
| 35* | 8 | 17 | −0.1 | 0.7 | −0.4 | 1.0 | 0.5 | 0.5 | −1.0 | −0.4 | 0.4 | −0.9 | 0.0 | −0.7 | |
| 36 | 14 | 4 | −1.4 | 0.3 | −2.5 | −0.5 | −0.9 | −0.7 | 0.1 | −1.1 | −1.6 | −3.6 | −0.7 | −0.7 | 1 |
| 37 | 15 | 10 | −0.9 | −0.5 | −0.9 | 0.9 | 0.5 | −0.1 | −1.5 | −0.3 | 0.1 | −0.1 | −1.0 | −1.0 | |
| 38* | 15 | 23 | −0.6 | −0.2 | −0.9 | 0.6 | −0.7 | 0.7 | 0.1 | −1.4 | 0.1 | −0.1 | 0.7 | 0.7 | |
| 39 | 15 | 25 | 2.1 | 2.7 | 1.5 | 0.7 | 0.8 | 0.5 | 2.0 | −0.3 | 0.6 | 0.4 | 1.7 | 1.3 | |
| 40 | 12 | 18 | −0.6 | −0.7 | −0.6 | 0.0 | - | −0.3 | 1.5 | −0.2 | 0.1 | −0.1 | 0.3 | 0.0 | |
| 41 | 13 | 9 | 0.4 | 0.3 | 0.7 | 0.9 | - | −0.1 | − | −0.3 | −0.2 | 1.1 | −1.7 | −1.3 | |
| 42 | 14 | 14 | −1.7 | −1.7 | −0.9 | −0.1 | - | −0.3 | 1.3 | −2.8 | −2.9 | −2.1 | −1.7 | −1.7 | 1 |
| 43 | 12 | 26 | −1.6 | −1.0 | −0.6 | 0.3 | - | −0.5 | −1.5 | −1.0 | −0.4 | −1.7 | 0.0 | 0.3 | |
| 44 | 15 | 82 | 0.9 | 0.0 | 1.3 | 0.1 | - | 0.0 | 0.2 | −0.7 | 0.1 | −0.9 | 0.0 | 0.0 | |
| 45 | 13 | 25 | 0.1 | 0.3 | 0.2 | 1.5 | - | 1.7 | 0.9 | −0.3 | 0.1 | 0.4 | 0.7 | 0.3 | |
| 46 | 9 | 45 | 0.8 | 0.3 | 1.9 | −0.2 | - | −0.4 | 1.2 | −0.7 | 0.1 | 0.2 | 0.0 | 0.0 | |
| 47 | 14 | 10 | −1.3 | −0.3 | −1.3 | 0.1 | - | −0.7 | −1.0 | −1.1 | −0.7 | −1.0 | −0.7 | −0.7 | |
| 50 | 15 | 19 | 0.5 | −0.3 | 0.6 | 1.2 | - | 1.2 | 0.9 | −0.2 | −0.7 | −2.5 | 1.3 | 1.3 | 1 |
| 51 | 9 | 7 | 0.9 | 0.0 | 0.7 | 0.9 | - | 1.0 | 1.6 | −1.4 | 0.3 | −0.6 | 2.0 | 1.7 |
References
- Duignan, S.M.; Hemingway, C.A. Paediatric acquired demyelinating syndromes. Paediatr. Child Health 2019, 29, 468–475. [Google Scholar] [CrossRef]
- Waldman, A.; Ghezzi, A.; Bar-Or, A.; Mikaeloff, Y.; Tardieu, M.; Banwell, B. Multiple sclerosis in children: An update on clinical diagnosis, therapeutic strategies, and research. Lancet Neurol. 2014, 13, 936–948. [Google Scholar] [CrossRef]
- Marrie, R.A.; O’Mahony, J.; Maxwell, C.; Ling, V.; Yeh, E.A.; Arnold, D.L.; Bar-Or, A.; Banwell, B.; Canadian Pediatric Demyelinating Disease Network. Incidence and prevalence of MS in children: A population-based study in Ontario, Canada. Neurology 2018, 91, e1579–e1590. [Google Scholar] [CrossRef] [PubMed]
- Duignan, S.; Brownlee, W.; Wassmer, E.; Hemingway, C.; Lim, M.; Ciccarelli, O.; Hacohen, Y. Paediatric multiple sclerosis: A new era in diagnosis and treatment. Dev. Med. Child Neurol. 2019, 61, 1039–1049. [Google Scholar] [CrossRef] [PubMed]
- Waubant, E.; Chabas, D.; Okuda, D.T.; Glenn, O.; Mowry, E.; Henry, R.G.; Strober, J.B.; Soares, B.; Wintermark, M.; Pelletier, D. Difference in disease burden and activity in pediatric patients on brain magnetic resonance imaging at time of multiple sclerosis onset vs adults. Arch. Neurol. 2019, 66, 967–971. [Google Scholar] [CrossRef] [PubMed]
- Gorman, M.P.; Healy, B.C.; Polgar-Turcsanyi, M.; Chitnis, T. Increased relapse rate in pediatric-onset compared with adult-onset multiple sclerosis. Arch. Neurol. 2009, 66, 54–59. [Google Scholar] [CrossRef] [PubMed]
- Renoux, C.; Vukusic, S.; Confavreux, C. The natural history of multiple sclerosis with childhood onset. Clin. Neurol. Neurosurg. 2009. [Google Scholar] [CrossRef]
- Amato, M. Cognitive and psychosocial issues in pediatric multiple sclerosis: Where we are and where we need to go. Neuropediatrics 2012. [Google Scholar] [CrossRef]
- Baruch, N.F.; O’Donnell, E.H.; Glanz, B.I.; Benedict, R.H.; Musallam, A.J.; Healy, B.C.; Rintell, D.; Chitnis, T. Cognitive and patient-reported outcomes in adults with pediatric-onset multiple sclerosis. Mult. Scler. J. 2016, 22, 354–361. [Google Scholar] [CrossRef]
- Harding, K.E.; Liang, K.; Cossburn, M.D.; Ingram, G.; Hirst, C.L.; Pickersgill, T.P.; Naude, J.T.W.; Wardle, M.; Ben-Shlomo, Y.; Robertson, N.P. Long-term outcome of paediatric-onset multiple sclerosis: A population-based study. J. Neurol. Neurosurg. Psychiatry 2013. [Google Scholar] [CrossRef]
- Cockburn, R.; Duncan, M.; Johnston, C.; Bullock, H.; Mitchell, S.; Hemingway, C. A systematic review of the psychosocial impact of paediatric demyelinating disorders. Arch. Dis. Child 2019, 104 (Suppl. 4), A6. [Google Scholar] [CrossRef]
- Marrie, R.A.; O’Mahony, J.; Maxwell, C.; Ling, V.; Yeh, E.A.; Arnold, D.L.; Bar-Or, A.; Banwell, B.; Canadian Pediatric Demyelinating Disease Network. Increased mental health care use by mothers of children with multiple sclerosis. Neurology 2020, 94, e1040–e1050. [Google Scholar] [CrossRef] [PubMed]
- He, A.; Merkel, B.; Brown, J.W.L.; Ryerson, L.Z.; Kister, I.; Malpas, C.B.; Sharmin, S.; Horakova, D.; Havrdova, E.K.; Spelman, T.; et al. Timing of high-efficacy therapy for multiple sclerosis: A retrospective observational cohort study. Lancet Neurol. 2020, 19, 307–316. [Google Scholar] [CrossRef]
- Hinton, D.; Kirk, S. Paediatric multiple sclerosis: A qualitative study of families’ diagnosis experiences. Arch. Dis. Child 2015. [Google Scholar] [CrossRef] [PubMed]
- Krupp, L.B.; Banwell, B.; Tenembaum, S. Consensus definitions proposed for pediatric multiple sclerosis and related disorders. Neurology 2007, 68 (Suppl. 2). [Google Scholar] [CrossRef] [PubMed]
- Krupp, L.B.; Tardieu, M.; Amato, M.P.; Banwell, B.; Chitnis, T.; Dale, R.C.; Ghezzi, A.; Hintzen, R.; Kornberg, A.; Pohl, D.; et al. International Pediatric Multiple Sclerosis Study Group criteria for pediatric multiple sclerosis and immune-mediated central nervous system demyelinating disorders: Revisions to the 2007 definitions. Mult. Scler. J. 2013, 19, 1261–1267. [Google Scholar] [CrossRef]
- Hacohen, Y.; Wong, Y.Y.; Lechner, C.; Jurynczyk, M.; Wright, S.; Konuskan, B.; Kalser, J.; Poulat, A.L.; Maurey, H.; Ganelin-Cohen, E.; et al. Disease course and treatment responses in children with relapsing myelin oligodendrocyte glycoprotein antibody–Associated disease. JAMA Neurol. 2018, 75, 478–487. [Google Scholar] [CrossRef] [PubMed]
- Kurtzke, J.F. Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology 1983. [Google Scholar] [CrossRef] [PubMed]
- Varni, J.W.; Seid, M.; Rode, C.A. The PedsQLTM: Measurement model for the pediatric quality of life inventory. Med. Care 1999. [Google Scholar] [CrossRef]
- Varni, J.W.; Seid, M.; Kurtin, P.S. PedsQLTM 4.0: Reliability and Validity of the Pediatric Quality of Life InventoryTM Version 4.0 Generic Core Scales in Healthy and Patient Populations. Med. Care 2001, 39, 800–812. [Google Scholar] [CrossRef]
- Thompson, A.; Baranzini, S.; Geurts, J.; Hemmer, B.; Ciccarelli, O. Multiple sclerosis. Lancet 2018, 391, 1622–1636. [Google Scholar] [CrossRef]
- Krysko, K.M.; Graves, J.; Rensel, M.; Weinstock-Guttman, B.; Aaen, G.; Benson, L.; Chitnis, T.; Gorman, M.; Goyal, M.; Krupp, L.; et al. Use of newer disease-modifying therapies in pediatric multiple sclerosis in the US. Neurology 2018, 91, e1778–e1787. [Google Scholar] [CrossRef]
- Chitnis, T.; Arnold, D.L.; Banwell, B.; Brück, W.; Ghezzi, A.; Giovannoni, G.; Greenberg, B.; Krupp, L.; Rostásy, K.; Tardieu, M.; et al. Trial of fingolimod versus interferon beta-1a in pediatric multiple sclerosis. N. Engl. J. Med. 2018. [Google Scholar] [CrossRef]
- Giovannoni, G.; Tomic, D.; Bright, J.R.; Havrdová, E. “No evident disease activity”: The use of combined assessments in the management of patients with multiple sclerosis. Mult. Scler. J. 2017. [Google Scholar] [CrossRef]
- Chitnis, T.; Tenembaum, S.; Banwell, B.; Krupp, L.; Pohl, D.; Rostasy, K.; Yeh, E.A.; Bykova, O.; Wassmer, E.; Tardieu, M.; et al. Consensus statement: Evaluation of new and existing therapeutics for pediatric multiple sclerosis. Mult. Scler. J. 2012. [Google Scholar] [CrossRef]
- Polman, C.H.; Reingold, S.C.; Banwell, B.; Clanet, M.; Cohen, J.A.; Filippi, M.; Fujihara, K.; Havrdova, E.; Hutchinson, M.; Kappos, L.; et al. Diagnostic criteria for multiple sclerosis: 2010 Revisions to the McDonald criteria. Ann. Neurol. 2011. [Google Scholar] [CrossRef] [PubMed]
- Thompson, A.; Banwell, B.; Barkhof, F. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018, 162–173. [Google Scholar] [CrossRef]
- Sadaka, Y.; Verhey, L.H.; Shroff, M.M.; Branson, H.M.; Arnold, D.L.; Narayanan, S.; Sled, J.G.; Bar-Or, A.; Sadovnick, A.D.; McGowan, M.; et al. 2010 McDonald criteria for diagnosing pediatric multiple sclerosis. Ann. Neurol. 2012, 72, 211–223. [Google Scholar] [CrossRef]
- Sedani, S.; Lim, M.J.; Hemingway, C.; Wassmer, E.; Absoud, M. Paediatric multiple sclerosis: Examining utility of the McDonald 2010 criteria. Mult. Scler. J. 2011, 18, 679–682. [Google Scholar] [CrossRef] [PubMed]
- NHS England. Multiple Sclerosis Management Service for Children, Service Specification 170019/S. 2017. Available online: https://www.england.nhs.uk/wp-content/uploads/2017/08/multiple-sclerosis-mgt-for-children-sept-2017.pdf (accessed on 1 November 2020).
- Krysko, K.M.; Graves, J.S.; Rensel, M.; Weinstock-Guttman, B.; Rutatangwa, A.; Aaen, G.; Belman, A.; Benson, L.; Chitnis, T.; Gorman, M.; et al. Real-World Effectiveness of Initial Disease-Modifying Therapies in Pediatric Multiple Sclerosis. Ann. Neurol. 2020, 88, 42–55. [Google Scholar] [CrossRef]
- Huppke, P.; Huppke, B.; Ellenberger, D.; Rostasy, K.; Hummel, H.; Stark, W.; Brück, W.; Gärtner, J. Therapy of highly active pediatric multiple sclerosis. Mult. Scler. J. 2019. [Google Scholar] [CrossRef]
- Arnold, D.L.; Banwell, B.; Bar-Or, A.; Ghezzi, A.; Greenberg, B.M.; Waubant, E.; Giovannoni, G.; Wolinsky, J.S.; Gärtner, J.; Rostásy, K.; et al. Effect of fingolimod on MRI outcomes in patients with paediatric-onset multiple sclerosis: Results from the phase 3 PARADIGMS study. J. Neurol. Neurosurg. Psychiatry 2020, 91, 483–492. [Google Scholar] [CrossRef] [PubMed]
- Amato, M.P.; Krupp, L.B.; Charvet, L.E.; Penner, I.; Till, C. Pediatric multiple sclerosis: Cognition and mood. Neurology 2016. [Google Scholar] [CrossRef]
- Amato, M.P.; Goretti, B.; Ghezzi, A.; Hakiki, B.; Niccolai, C.; Lori, S.; Moiola, L.; Falautano, M.; Viterbo, R.G.; Patti, F.; et al. Neuropsychological features in childhood and juvenile multiple sclerosis: Five-year follow-up. Neurology 2014. [Google Scholar] [CrossRef]
- ClinicalTrials.gov. Efficacy, Safety and Pharmacokinetics of Teriflunomide In Pediatric Patients with Relapsing Forms of Multiple Sclerosis (TERIKIDS). National Library of Medicine (US). 2014. Available online: Clinicaltrials.gov/ct2/show/study/NCT02201108 (accessed on 1 November 2020).
- ClinicalTrials.gov. Phase 3 Efficacy and Safety Study of BG00012 in Pediatric Subjects With Relapsing-Remitting Multiple Sclerosis (RRMS) (CONNECT). National Library of Medicine (US). 2014. Available online: Clinicaltrials.gov/ct2/show/NCT02283853 (accessed on 1 November 2020).
- ClinicalTrials.gov. A Study to Evaluate Efficacy, Safety, and Tolerability of Alemtuzumab in Pediatric Patients with RRMS With Disease Activity on Prior DMT (LemKids). National Library of Medicine (US). 2017. Available online: Clinicaltrials.gov/ct2/show/NCT03368664 (accessed on 1 November 2020).
- Waubant, E.; Banwell, B.; Wassmer, E.; Sormani, M.P.; Amato, M.P.; Hintzen, R.; Krupp, L.; Rostásy, K.; Tenembaum, S.; Chitnis, T. Clinical Trials Of Disease-Modifying Agents In Pediatric MS: Opportunities, challenges, and recommendations from the IPMSSG. Neurology 2019, 92, e2538–e2549. [Google Scholar] [CrossRef]

| 2007–2010 (n = 24) | 2015–2016 (n = 27) | p-Value | |
|---|---|---|---|
| Age at presentation, median (IQR), y | 12.7 (10.9–14.2) | 13.9 (10.4–14.3) | 0.56 |
| Sex, M:F | 1:3.8 | 1:2.9 | 0.75 |
| Symptoms at onset (%) | |||
| Vision | 10/24 (42) | 9/27 (33) | 0.58 |
| Isolated motor | 12/24 (50) | 3/27 (11) | 0.005 * |
| Cerebellar syndrome | 5/24 (21) | 5/27 (19) | 1.0 |
| Sensory | 10/24 (42) | 9/27 (33) | 0.58 |
| Cranial nerve involvement | 4/24 (17) | 12/27 (44) | 0.040 * |
| Paraclinical features (%) | |||
| OCB | 20/21 (95) | 25/27 (93) | 1.0 |
| EBV IgG | 8/8 (100) | 23/23 (100) | 1.0 |
| Time to diagnosis, median (IQR), m | 10 (5–13) | 9 (5–17) | 0.94 |
| Follow-up time median (IQR), y | 5.0 (2.5–7.5) | 3.0 (2.0–5.0) | 0.13 |
| Patients not started on DMT (%) | 5/24 (21) | 3/27 (11) | 0.29 |
| Outcome | |||
| Pre-treatment ARR, mean (IQR), no. patients | 2.7 (1.3–4.0), 19/24 | 1.7 (0.4–2.0), 24/27 | 0.010 * |
| Post-treatment ARR, mean (IQR), no. patients | 0.7 (0.3–1.0), 19/24 | 0.4 (0.0–0.7), 24/27 | 0.029 * |
| EDSS at 2 y, median (IQR), no. patients | 1.0 (0.0–2.25), 18/24 | 1.0 (0.0–1.5), 27/27 | 0.47 |
| NEUROCOGNITIVE TEST | Numbers Tested in 2007–2010 | Numbers Tested in 2015–2016 | Median z- Score in 2007–2010 | Median z-Score in 2015–2016 | Increase in Median z-Score |
|---|---|---|---|---|---|
| Full-Scale IQ | 11 | 24 | −1.50 ** | −0.20 | 1.30 |
| Working Memory Index | 13 | 24 | −0.90 * | 0.00 | 0.90 |
| Processing Speed Index | 13 | 24 | −1.50 ** | −0.52 | 0.98 |
| Word Reading | 9 | 24 | −0.25 | 0.60 | 0.85 # |
| Pseudoword Decoding | 7 | 13 | −0.52 | 0.66 | 1.18 |
| Spelling | 9 | 23 | −0.67 | 0.00 | 0.67 # |
| Numerical Operations | 10 | 22 | −0.33 | 0.60 | 0.93 |
| Visual–Motor Integration | 7 | 24 | −0.67 | −0.33 | 0.34 |
| Visual Perception | 7 | 23 | −0.25 | −0.12 | 0.13 |
| Motor Coordination | 7 | 23 | −2.00 ** | −0.90 * | 1.10 |
| Memory Stories Immediate | 8 | 19 | −1.00 * | 0.00 | 1.00 |
| Memory Stories Delayed | 8 | 19 | −1.00 * | 0.00 | 1.00 # |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Luchesa Smith, A.; Benetou, C.; Bullock, H.; Kuczynski, A.; Rudebeck, S.; Hanson, K.; Crichton, S.; Mankad, K.; Siddiqui, A.; Byrne, S.; et al. Progress in the Management of Paediatric-Onset Multiple Sclerosis. Children 2020, 7, 222. https://doi.org/10.3390/children7110222
Luchesa Smith A, Benetou C, Bullock H, Kuczynski A, Rudebeck S, Hanson K, Crichton S, Mankad K, Siddiqui A, Byrne S, et al. Progress in the Management of Paediatric-Onset Multiple Sclerosis. Children. 2020; 7(11):222. https://doi.org/10.3390/children7110222
Chicago/Turabian StyleLuchesa Smith, Aphra, Christina Benetou, Hayley Bullock, Adam Kuczynski, Sarah Rudebeck, Katie Hanson, Sarah Crichton, Kshitij Mankad, Ata Siddiqui, Susan Byrne, and et al. 2020. "Progress in the Management of Paediatric-Onset Multiple Sclerosis" Children 7, no. 11: 222. https://doi.org/10.3390/children7110222
APA StyleLuchesa Smith, A., Benetou, C., Bullock, H., Kuczynski, A., Rudebeck, S., Hanson, K., Crichton, S., Mankad, K., Siddiqui, A., Byrne, S., Lim, M., & Hemingway, C. (2020). Progress in the Management of Paediatric-Onset Multiple Sclerosis. Children, 7(11), 222. https://doi.org/10.3390/children7110222






