Role of RDW in Prediction of Burn after Caustic Substance Ingestion
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
Author Contributions
Conflicts of Interest
References
- Lupa, M.; Magne, J.; Guarisco, J.L.; Amedee, R. Update on the diagnosis and treatment of caustic ingestion. Ochsner J. 2009, 9, 54–59. [Google Scholar] [PubMed]
- Aydın, E.; Özcan, R.; Emre, Ş.; Elicevik, M.; Tutuncu, C.; Kurugoglu, S.; Erdogan, E.; Tekant, G.T. Corosive ingestion in pediatric age group: Analysis of 681 patients. Turk. Assoc. Pediatr. Surg. 2012, 26, 26–31. [Google Scholar] [CrossRef]
- Betalli, P.; Falchetti, D.; Giuliani, S.; Pane, A.; Dall’Oglio, L.; de Angelis, G.L.; Caldore, M.; Romano, C.; Gamba, P.; Baldo, V. Caustic ingestion in children: Is endoscopy always indicated? The results of an Italian multicenter observational study. Gastrointest. Endosc. 2008, 68, 434–439. [Google Scholar] [CrossRef] [PubMed]
- Gaudreault, P.; Parent, M.; McGuigan, M.A.; Chicoine, L.; Lovejoy, F.H., Jr. Predictability of esophageal injury from signs and symptoms: A study of caustic ingestion in 378 children. Pediatrics 1983, 71, 767–770. [Google Scholar] [PubMed]
- Tuncez, A.; Cetin, M.S.; Cetin, E.H.; Yilmaz, S.; Korkmaz, A.; Ucar, F.M. Association between RDW and stent thrombosis in patients with ST-elevation myocardial infarction undergoing primary percutaneous coronary intervention. Medicine (Baltimore) 2017, 96, e5986. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Zhao, Y.; Feng, L.; Guo, R. Comparison of the prognostic values of inflammation markers in patients with acute pancreatitis: A retrospective cohort study. BMJ Open 2017, 7, e013206. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Hong, N.; Robertson, M.; Wang, C.; Jiang, G. Preoperative red cell distribution width and neutrophil-to-lymphocyte ratio predict survival in patients with epithelial ovarian cancer. Sci. Rep. 2017, 7, 43001. [Google Scholar] [CrossRef] [PubMed]
- Demirkol, S.; Balta, S.; Cakar, M.; Unlu, M.; Arslan, Z.; Kucuk, U. Red cell distribution width: A novel inflammatory marker in clinical practice. Cardiol. J. 2013, 20, 209. [Google Scholar] [CrossRef] [PubMed]
- Lippi, G.; Targher, G.; Montagnana, M.; Salvagno, G.L.; Zoppini, G.; Guidi, G.C. Relation between red blood cell dstribution width and inflammatory biomarkers in a large cohort of unselected patients. Arch. Pathol. Lab. Med. 2009, 133, 628–632. [Google Scholar] [PubMed]
- Evans, T.C.; Jehle, D. The red blood cell distribution width. J. Emerg. Med. 1991, 9, 71–74. [Google Scholar] [CrossRef]
- Cakir, L.; Aktas, G.; Mercimek, O.B.; Enginyurt, O.; Kaya, Y.; Mercimek, K. Are red cell distribution width and mean platelet volume associated with rheumatoid arthritis? Biomed. Res. 2016, 27, 292–294. [Google Scholar]
- Abdel-Razik, A.; Eldars, W.; Rizk, E. Platelet indices and inflammatory markers as diagnostic predictors for ascitic fluid infection. Eur. J. Gastroenterol. Hepatol. 2014, 26, 1342–1347. [Google Scholar] [CrossRef] [PubMed]
- Zargar, S.A.; Kochhar, R.; Mehta, S.; Mehta, S.K. The role of fiberoptic endoscopy in the management of corrosive ingestion and modified endoscopic classification of burns. Gastrointest. Endosc. 1991, 37, 165–169. [Google Scholar] [CrossRef]
| Age | 95% CI | ||
|---|---|---|---|
| No burn | 3.29 ± 3.21 | 2.72–3.86 | |
| Burn | Grade 1 | 3.73 ± 3.59 | 1.31–6.14 |
| Grade 2 | 4.32 ± 4.55 | 2.30–6.34 | |
| Grade 3 | 5.25 ± 4.60 | −36.05–46.55 |
| Burn (+) | Burn (−) | p | |
|---|---|---|---|
| age | 4.03 ± 4.04 | 3.29 ± 3.21 | 0.246 |
| gender | 0.925 | ||
| male | 21 (55.3%) | 68 (54.4%) | |
| female | 17 (44.7%) | 57 (45.6%) | |
| type of substance | 0.742 | ||
| acid | 12 (31.6%) | 36 (28.8%) | |
| base | 26 (68.4%) | 89 (71.2%) |
| Burn (+) | Burn (−) | p | |
|---|---|---|---|
| wbc | 10,760.26 ± 3211.55 | 11,192.11 ± 3602.84 | 0.508 |
| plt | 337,157.89 ± 78,561.46 | 341,478.16 ± 91,441.24 | 0.793 |
| hgb | 12.98 ± 1.13 | 12.84 ± 1.40 | 0.575 |
| htc | 35.90 ± 3.07 | 37.87 ± 3.66 | 0.704 |
| mcv | 85.28 ± 4.26 | 84.23 ± 4.17 | 0.153 |
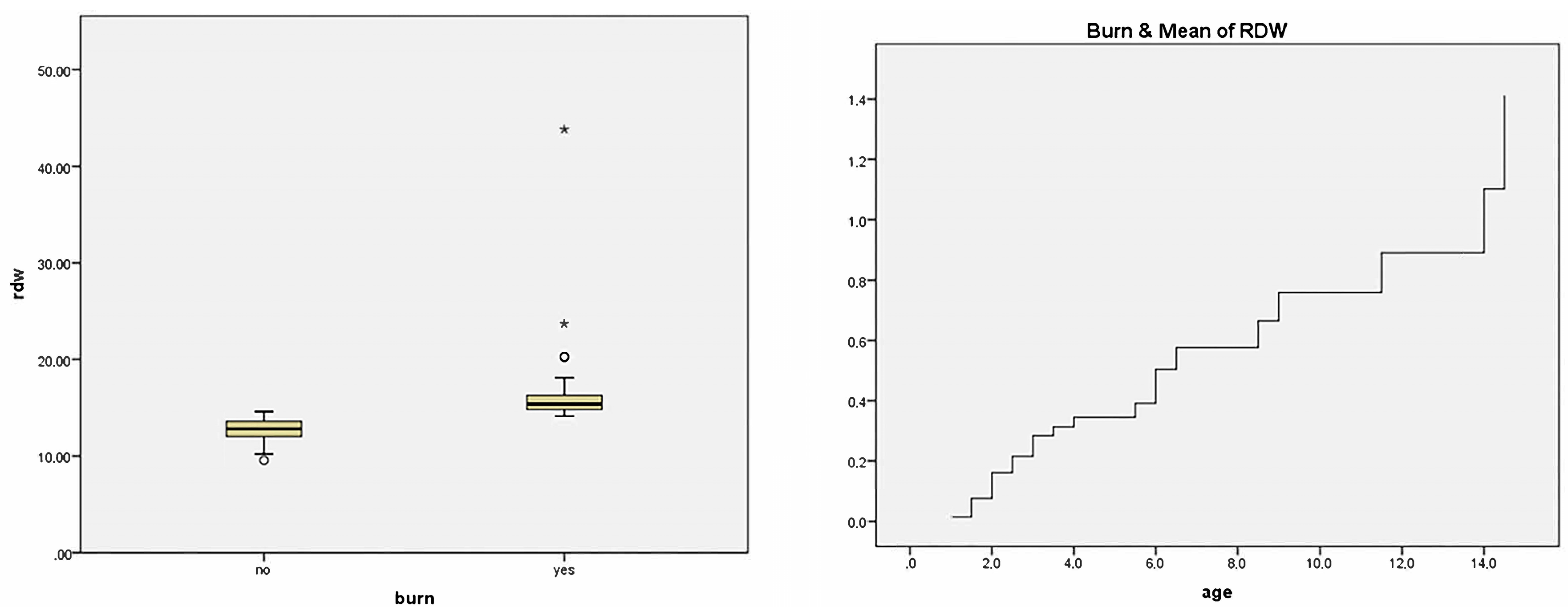
| rdw | 14.63 ± 5.45 | 11.99 ± 1.40 | 0.000 * |
| mpw | 8.61 ± 1.69 | 8.39 ± 1.60 | 0.478 |
| pdw | 13.86 ± 4.47 | 13.44 ± 4.23 | 0.606 |
| lym | 5.35 ± 2.42 | 5.44 ± 2.31 | 0.835 |
| mono | 0.86 ± 0.31 | 0.83 ± 0.30 | 0.600 |
| neut | 4.19 ± 1.7 | 4.55 ± 2.71 | 0.451 |
| eos | 0.32 ± 0.23 | 0.33 ± 0.36 | 0.850 |
| baso | 0.11 ± 0.2 | 0.11 ± 0.17 | 0.882 |
| neut/lym | 1.05 ± 0.86 | 1.04 ± 0.98 | 0.930 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aydin, E.; Beser, O.F.; Sazak, S.; Duras, E. Role of RDW in Prediction of Burn after Caustic Substance Ingestion. Children 2018, 5, 5. https://doi.org/10.3390/children5010005
Aydin E, Beser OF, Sazak S, Duras E. Role of RDW in Prediction of Burn after Caustic Substance Ingestion. Children. 2018; 5(1):5. https://doi.org/10.3390/children5010005
Chicago/Turabian StyleAydin, Emrah, Omer Faruk Beser, Soner Sazak, and Ensar Duras. 2018. "Role of RDW in Prediction of Burn after Caustic Substance Ingestion" Children 5, no. 1: 5. https://doi.org/10.3390/children5010005
APA StyleAydin, E., Beser, O. F., Sazak, S., & Duras, E. (2018). Role of RDW in Prediction of Burn after Caustic Substance Ingestion. Children, 5(1), 5. https://doi.org/10.3390/children5010005





