A Child’s Concept of Pain: An International Survey of Pediatric Pain Experts
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Survey Design
2.4. Data Analysis
3. Results
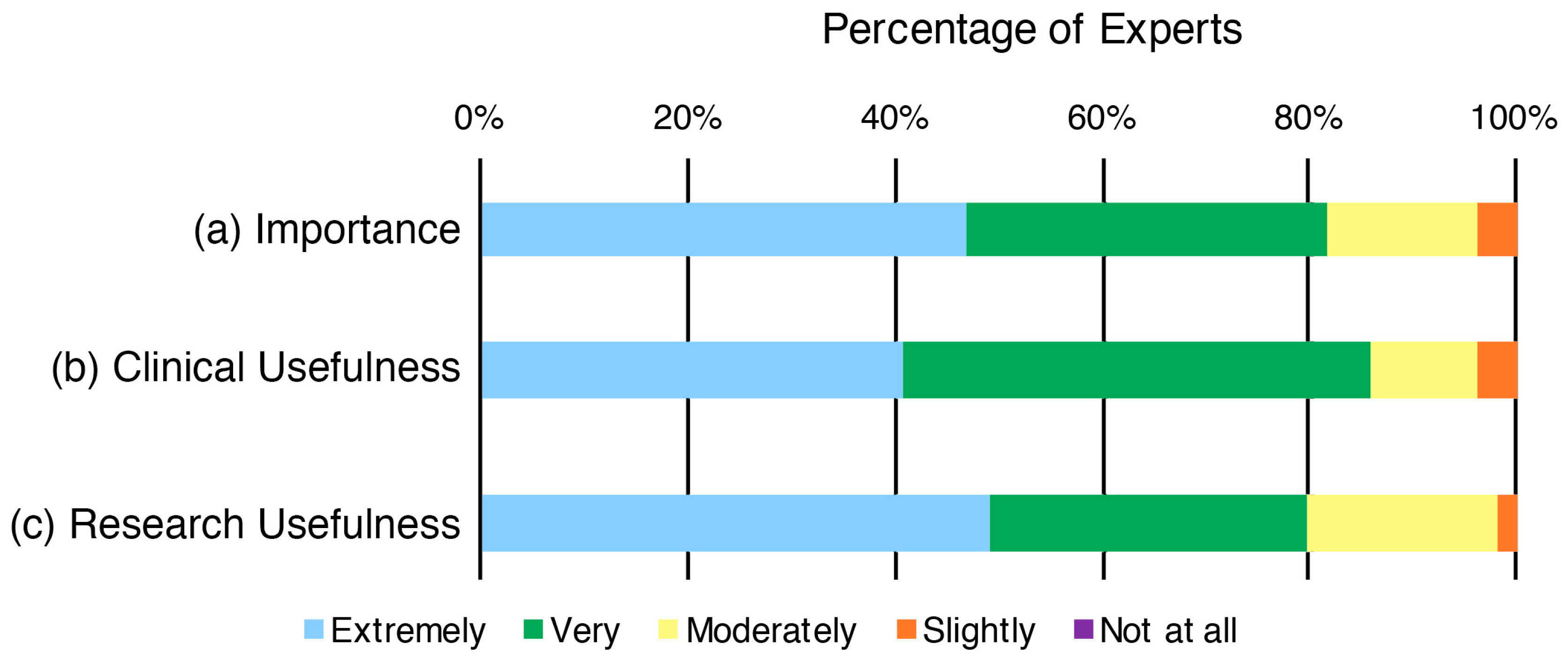
3.1. The Importance and Usefulness of Assessing a Child’s Concept of Pain in Clinical and/or Research Settings (1)
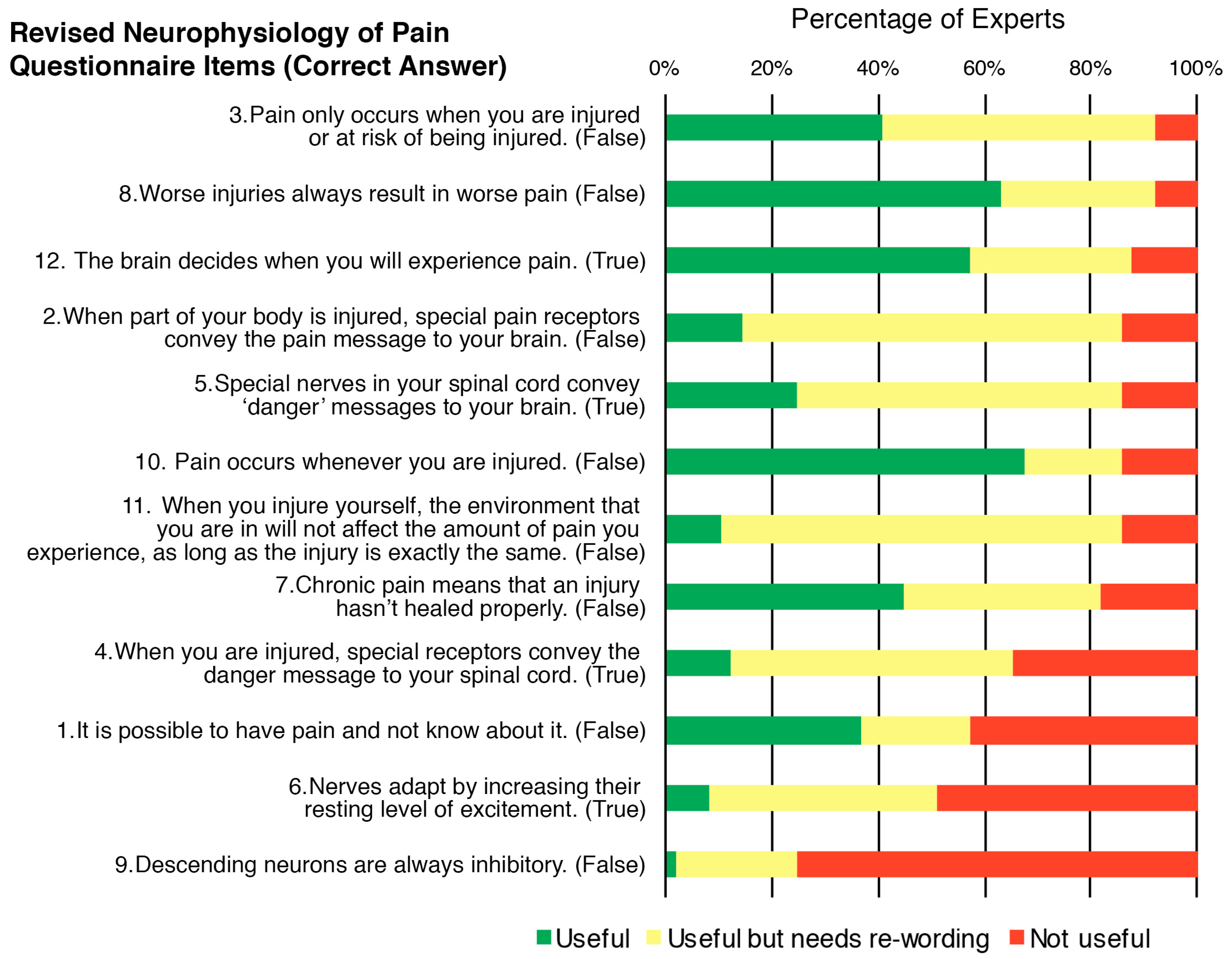
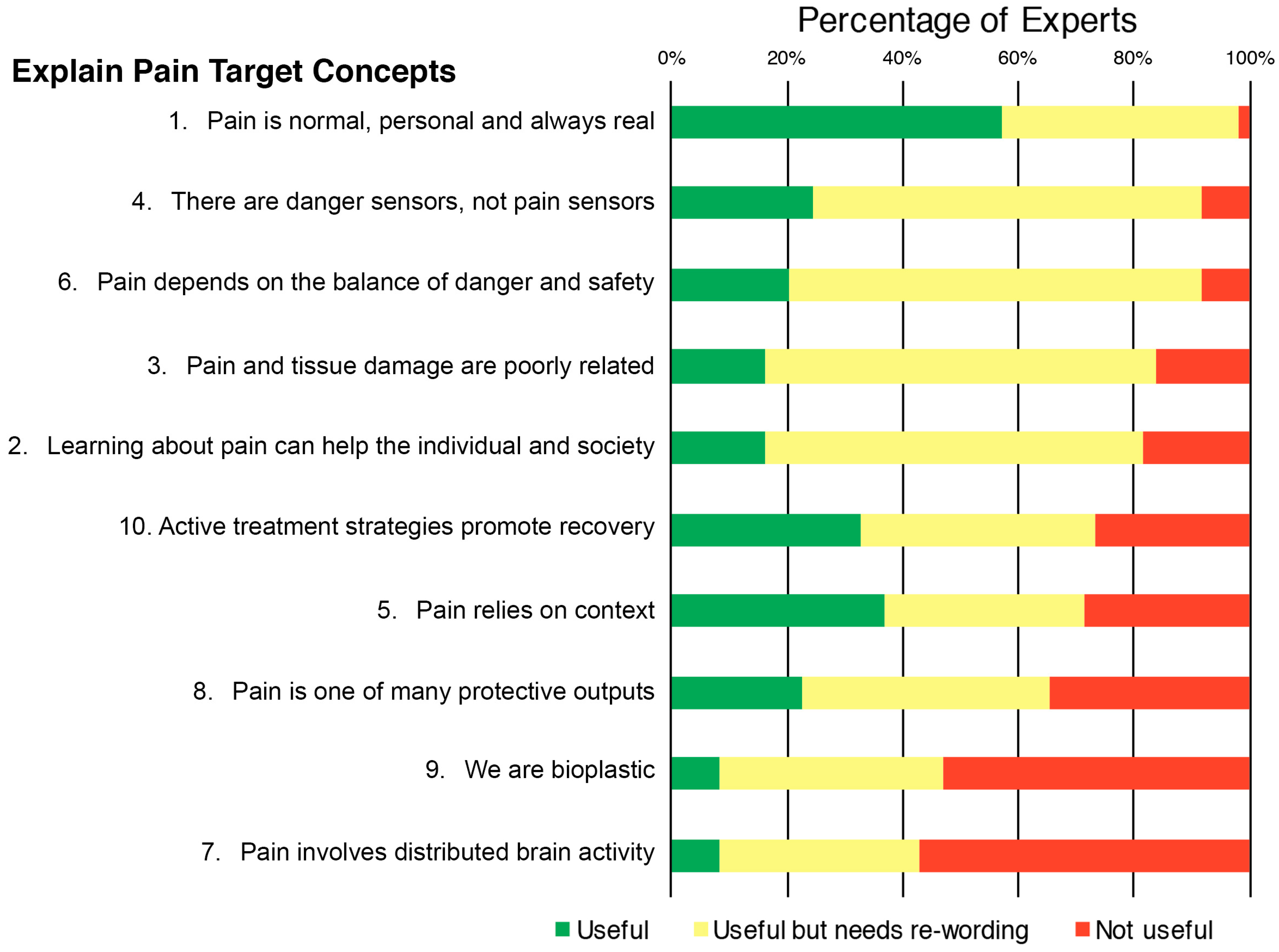
3.2. The Usefulness of the Content of Items within Currently Published Resources for Assessing a Child’s Concept of Pain (2)
3.3. Domains of a Child’s Concept of Pain That Are Important to Assess (3)
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Acknowledgments
Author Contributions
Conflicts of Interest
References
- King, S.; Chambers, C.T.; Huguet, A.; MacNevin, R.C.; McGrath, P.J.; Parker, L.; MacDonald, A.J. The epidemiology of chronic pain in children and adolescents revisited: A systematic review. Pain 2011, 152, 2729–2738. [Google Scholar] [CrossRef] [PubMed]
- Swain, M.S.; Henschke, N.; Kamper, S.J.; Gobina, I.; Ottová-Jordan, V.; Maher, C.G. An international survey of pain in adolescents. BMC Public Health 2014, 14, 447. [Google Scholar] [CrossRef] [PubMed]
- Coffelt, T.A.; Bauer, B.D.; Carroll, A.E. Inpatient characteristics of the child admitted with chronic pain. Pediatrics 2013, 132, e422–e429. [Google Scholar] [CrossRef] [PubMed]
- Odell, S.; Logan, D.E. Pediatric pain management: The multidisciplinary approach. J. Pain Res. 2013, 6, 785. [Google Scholar] [CrossRef] [PubMed]
- Hassett, A.L.; Hilliard, P.E.; Goesling, J.; Clauw, D.J.; Harte, S.E.; Brummett, C.M. Reports of chronic pain in childhood and adolescence among patients at a tertiary care pain clinic. J. Pain 2013, 14, 1390–1397. [Google Scholar] [CrossRef] [PubMed]
- Hunfeld, J.A.; Perquin, C.W.; Duivenvoorden, H.J.; Hazebroek-Kampschreur, A.A.; Passchier, J.; van Suijlekom-Smit, L.W.; van der Wouden, J.C. Chronic pain and its impact on quality of life in adolescents and their families. J. Pediatr. Psychol. 2001, 26, 145–153. [Google Scholar] [CrossRef] [PubMed]
- Lisman-van Leeuwen, Y.; Spee, L.A.; Benninga, M.A.; Bierma-Zeinstra, S.M.; Berger, M.Y. Prognosis of abdominal pain in children in primary care—A prospective cohort study. Ann. Fam. Med. 2013, 11, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Kosola, S.; Mundy, L.K.; Sawyer, S.M.; Canterford, L.; van der Windt, D.A.; Dunn, K.M.; Patton, G.C. Pain and learning in primary school: A population-based study. Pain 2017, 158, 1825–1830. [Google Scholar] [CrossRef] [PubMed]
- Zernikow, B.; Wager, J.; Hechler, T.; Hasan, C.; Rohr, U.; Dobe, M.; Meyer, A.; Hübner-Möhler, B.; Wamsler, C.; Blankenburg, M. Characteristics of highly impaired children with severe chronic pain: A 5-year retrospective study on 2249 pediatric pain patients. BMC Pediatr. 2012, 12, 54. [Google Scholar] [CrossRef] [PubMed]
- Groenewald, C.B.; Essner, B.S.; Wright, D.; Fesinmeyer, M.D.; Palermo, T.M. The economic costs of chronic pain among a cohort of treatment-seeking adolescents in the United States. J. Pain 2014, 15, 925–933. [Google Scholar] [CrossRef] [PubMed]
- Moseley, G.L.; Butler, D.S. Fifteen years of explaining pain: The past, present, and future. J. Pain 2015, 16, 807–813. [Google Scholar] [CrossRef] [PubMed]
- Engel, G.L. The need for a new medical model: A challenge for biomedicine. Holist. Med. 1989, 4, 37–53. [Google Scholar] [CrossRef]
- Posner, G.J.; Strike, K.A.; Hewson, P.W.; Gertzog, W.A. Accommodation of a scientific conception: Toward a theory of conceptual change. Sci. Educ. 1982, 66, 211–227. [Google Scholar] [CrossRef]
- Turk, D.C.; Gatchel, R.J. Psychological Approaches to Pain Management: A Practitioner’s Handbook, 2nd ed.; The Guilford Press: New York, NY, USA, 2002; 590 p. [Google Scholar]
- Fillingim, R.B. Individual differences in pain: Understanding the mosaic that makes pain personal. Pain 2017, 158, S11–S18. [Google Scholar] [CrossRef] [PubMed]
- Gaffney, A.; Dunne, E.A. Developmental aspects of children’s definitions of pain. Pain 1986, 26, 105–117. [Google Scholar] [CrossRef]
- Catley, M.J.; O’Connell, N.E.; Moseley, G.L. How good is the neurophysiology of pain questionnaire? A rasch analysis of psychometric properties. J. Pain 2013, 14, 818–827. [Google Scholar] [CrossRef] [PubMed]
- Louw, A.; Diener, I.; Butler, D.S.; Puentedura, E.J. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Arch. Phys. Med. Rehabil. 2011, 92, 2041–2056. [Google Scholar] [CrossRef] [PubMed]
- Louw, A.; Diener, I.; Landers, M.R.; Puentedura, E.J. Preoperative pain neuroscience education for lumbar radiculopathy: A multicenter randomized controlled trial with 1-year follow-up. Spine 2014, 39, 1449–1457. [Google Scholar] [CrossRef] [PubMed]
- Moseley, G.L.; Nicholas, M.K.; Hodges, P.W. A randomized controlled trial of intensive neurophysiology education in chronic low back pain. Clin. J. Pain 2004, 20, 324–330. [Google Scholar] [CrossRef] [PubMed]
- Puentedura, E.J.; Flynn, T. Combining manual therapy with pain neuroscience education in the treatment of chronic low back pain: A narrative review of the literature. Physiother. Theory Pract. 2016, 32, 408–414. [Google Scholar] [CrossRef] [PubMed]
- Van Ittersum, M.W.; van Wilgen, C.P.; van der Schans, C.P.; Lambrecht, L.; Groothoff, J.W.; Nijs, J. Written pain neuroscience education in fibromyalgia: A multicenter randomized controlled trial. Pain Pract. 2014, 14, 689–700. [Google Scholar] [CrossRef] [PubMed]
- Van Oosterwijck, J.; Meeus, M.; Paul, L.; De Schryver, M.; Pascal, A.; Lambrecht, L.; Nijs, J. Pain physiology education improves health status and endogenous pain inhibition in fibromyalgia: A double-blind randomized controlled trial. Clin J. Pain 2013, 29, 873–882. [Google Scholar] [CrossRef] [PubMed]
- Van Oosterwijck, J.; Nijs, J.; Meeus, M.; Truijen, S.; Craps, J.; Van den Keybus, N.; Paul, L. Pain neurophysiology education improves cognitions, pain thresholds, and movement performance in people with chronic whiplash: A pilot study. J. Rehabil. Res. Dev. 2011, 48, 43–58. [Google Scholar] [CrossRef] [PubMed]
- Wijma, A.J.; van Wilgen, C.P.; Meeus, M.; Nijs, J. Clinical biopsychosocial physiotherapy assessment of patients with chronic pain: The first step in pain neuroscience education. Physiother. Theory Pract. 2016, 32, 368–384. [Google Scholar] [CrossRef] [PubMed]
- Meeus, M.; Nijs, J.; Van Oosterwijck, J.; Van Alsenoy, V.; Truijen, S. Pain physiology education improves pain beliefs in patients with chronic fatigue syndrome compared with pacing and self-management education: A double-blind randomized controlled trial. Arch. Phys. Med. Rehabil. 2010, 91, 1153–1159. [Google Scholar] [CrossRef] [PubMed]
- Nijs, J.; Paul van Wilgen, C.; Van Oosterwijck, J.; van Ittersum, M.; Meeus, M. How to explain central sensitization to patients with ‘unexplained’ chronic musculoskeletal pain: Practice guidelines. Man. Ther. 2011, 16, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Traeger, A.C.; Moseley, G.L.; Hubscher, M.; Lee, H.; Skinner, I.W.; Nicholas, M.K.; Henschke, N.; Refshauge, K.M.; Blyth, F.M.; Main, C.J.; et al. Pain education to prevent chronic low back pain: A study protocol for a randomised controlled trial. BMJ Open 2014, 4, e005505. [Google Scholar] [CrossRef] [PubMed]
- Moseley, L. Unraveling the barriers to reconceptualization of the problem in chronic pain: The actual and perceived ability of patients and health professionals to understand the neurophysiology. J. Pain 2003, 4, 184–189. [Google Scholar] [CrossRef]
- Sowell, E.R.; Thompson, P.M.; Leonard, C.M.; Welcome, S.E.; Kan, E.; Toga, A.W. Longitudinal mapping of cortical thickness and brain growth in normal children. J. Neurosci. 2004, 24, 8223–8231. [Google Scholar] [CrossRef] [PubMed]
- Louw, A.; Zimney, K.; Puentedura, E.J.; Diener, I. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother. Theory. Pract. 2016, 32, 332–355. [Google Scholar] [CrossRef] [PubMed]
- Robins, H.; Perron, V.; Heathcote, L.C.; Simons, L.E. Pain neuroscience education: State of the art and application in pediatrics. Children 2016, 3, 43. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; Hübscher, M.; Moseley, G.L.; Kamper, S.J.; Traeger, A.C.; Mansell, G.; McAuley, J.H. How does pain lead to disability? A systematic review and meta-analysis of mediation studies in people with back and neck pain. Pain 2015, 156, 988–997. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.; McAuley, J.H.; Hubscher, M.; Kamper, S.J.; Traeger, A.C.; Moseley, G.L. Does changing pain-related knowledge reduce pain and improve function through changes in catastrophizing? Pain 2016, 157, 922–930. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, M.J. Controlling for “confounders” in psychosocial pain research. Pain 2016, 157, 775–776. [Google Scholar] [CrossRef] [PubMed]
- Gedaly-Duff, V. Developmental issues: Preschool and school-age children. In Children in Pain; Springer: Berlin/Heidelberg, Germany, 1991; pp. 195–229. [Google Scholar]
- Arbuckle, R.; Abetz-Webb, L. “Not just little adults”: Qualitative methods to support the development of pediatric patient-reported outcomes. Patient 2013, 6, 143–159. [Google Scholar] [CrossRef] [PubMed]
- Qualtrics. Available online: www.qualtrics.com (accessed on 7 May 2017).
- Moseley, G.L.; Butler, D.S. Explain Pain Supercharged; NOI Group: Adelaide, Australia, 2017. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows; Version 22.0; IBM Corp.: Armonk, NY, USA, 2013. [Google Scholar]
- DeVellis, R.F. Scale Development: Theory and Applications, 4th ed.; SAGE: Los Angeles, CA, USA, 2017; 262p. [Google Scholar]
- Yeung, K.-K.; Engle, L.; Rabel, A.; Adamson, K.; Schwellnus, H.; Evans, C. It just feels weird!: A qualitative study of how children aged 10–18 years describe neuropathic pain. Disabil. Rehabil. 2017, 39, 1695–1702. [Google Scholar] [CrossRef] [PubMed]
- Noel, M.; Palermo, T.M.; Chambers, C.T.; Taddio, A.; Hermann, C. Remembering the pain of childhood: Applying a developmental perspective to the study of pain memories. Pain 2015, 156, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Smail, B.; Kelly, A. Sex differences in science and technology among 11-year-old schoolchildren: II—Affective. Res. Sci. Technol. Educ. 1984, 2, 87–106. [Google Scholar] [CrossRef]
- Christidou, V.; Koulaidis, V.; Christidis, T. Children’s use of metaphors in relation to their mental models: The case of the ozone layer and its depletion. Res. Sci. Educ. 1997, 27, 541–552. [Google Scholar] [CrossRef]
- McGrath, P.J.; Craig, K.D. Developmental and psychological factors in children’s pain. Pediatr. Clin. N. Am. 1989, 36, 823–836. [Google Scholar] [CrossRef]
- Gallagher, L.; McAuley, J.; Moseley, G.L. A randomized-controlled trial of using a book of metaphors to reconceptualize pain and decrease catastrophizing in people with chronic pain. Clin. J. Pain 2013, 29, 20–25. [Google Scholar] [CrossRef] [PubMed]
- Borgers, N.; De Leeuw, E.; Hox, J. Children as respondents in survey research: Cognitive development and response quality 1. Bull. Methodol. Sociol. 2000, 66, 60–75. [Google Scholar] [CrossRef]
- Piolino, P.; Hisland, M.; Ruffeveille, I.; Matuszewski, V.; Jambaqué, I.; Eustache, F. Do school-age children remember or know the personal past? Conscious Cogn. 2007, 16, 84–101. [Google Scholar] [CrossRef] [PubMed]
- Flavell, J.H.; Flavell, E.R.; Green, F.L. Development of children’s understanding of connections between thinking and feeling. Psychol. Sci. 2001, 12, 430–432. [Google Scholar] [CrossRef] [PubMed]
- Piaget, J.; Inhelder, B. The Psychology of the Child; Basic Books: New York, NY, USA, 1969; Volume 5001. [Google Scholar]

| Characteristic | Experts (n = 49) |
|---|---|
| Clinical-only experts: n (%) | 15 (31%) |
| Research-only experts: n (%) | 16 (33%) |
| Clinical/research experts: n (%) | 18 (37%) |
| Professional discipline: n (%) | |
| Psychologist | 27 (55%) |
| Physiotherapist | 8 (16%) |
| Medical | 6 (12%) |
| Nurse | 4 (8%) |
| Occupational Therapist | 4 (8%) |
| Years of experience in pediatric pain: n (%) | |
| 2–5 years | 9 (18%) |
| 6–10 years | 15 (31%) |
| 11+ years | 25 (51%) |
| Number of pediatric pain patients per week by clinicians: n (%) | |
| 0 | 1 (3%) |
| 1–5 | 9 (27%) |
| 6–10 | 14 (42%) |
| 11–20 | 8 (24%) |
| 20+ | 1 (3%) |
| Gender: n (%) | |
| Male | 9 (18%) |
| Female | 40 (82%) |
| Geography: n (%) | |
| USA | 14 (29%) |
| Australia | 13 (26%) |
| Canada | 11 (22%) |
| Belgium | 3 (6%) |
| Denmark | 2 (4%) |
| The Netherlands | 2 (4%) |
| New Zealand | 1 (2%) |
| The Philippines | 1 (2%) |
| England | 1 (2%) |
| Ireland | 1 (2%) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pate, J.W.; Hush, J.M.; Hancock, M.J.; Moseley, G.L.; Butler, D.S.; Simons, L.E.; Pacey, V. A Child’s Concept of Pain: An International Survey of Pediatric Pain Experts. Children 2018, 5, 12. https://doi.org/10.3390/children5010012
Pate JW, Hush JM, Hancock MJ, Moseley GL, Butler DS, Simons LE, Pacey V. A Child’s Concept of Pain: An International Survey of Pediatric Pain Experts. Children. 2018; 5(1):12. https://doi.org/10.3390/children5010012
Chicago/Turabian StylePate, Joshua W., Julia M. Hush, Mark J. Hancock, G. Lorimer Moseley, David S. Butler, Laura E. Simons, and Verity Pacey. 2018. "A Child’s Concept of Pain: An International Survey of Pediatric Pain Experts" Children 5, no. 1: 12. https://doi.org/10.3390/children5010012
APA StylePate, J. W., Hush, J. M., Hancock, M. J., Moseley, G. L., Butler, D. S., Simons, L. E., & Pacey, V. (2018). A Child’s Concept of Pain: An International Survey of Pediatric Pain Experts. Children, 5(1), 12. https://doi.org/10.3390/children5010012






