Long-Term Outcomes of Prenatally Diagnosed Fetal Hemivertebra: A 15-Year Single-Center Review
Abstract
Highlights
- Isolated hemivertebra was associated with favorable long-term outcomes, including normal growth and development during childhood.
- Cases with multiple hemivertebrae were frequently accompanied by additional mal-formations or syndromic associations, leading to poorer prognosis and increased need for surgical intervention.
- Early prenatal detection of hemivertebra is crucial to identify associated anomalies and to rule out genetic syndromes, enabling accurate counseling regarding prognosis.
- Differentiating between isolated and multiple hemivertebrae can guide perinatal management and long-term follow-up, as outcomes vary significantly between these groups.
Abstract
1. Introduction
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Ethical Approval
2.3. Definitions
2.4. Prenatal Diagnosis
2.5. Postnatal Follow-Up
3. Results
3.1. Incidence and Demographics
3.2. Gestational Age at Diagnosis
3.3. Genetic Testing and Syndromic Associations
3.4. Perinatal Outcomes
3.5. Neonatal Outcomes and Follow-Up
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| Array-CGH | Array Comparative Genomic Hybridization |
| CS | Cesarean Section |
| CVS | Chorionic Villus Sampling |
| GA | Gestational Age |
| IUD | Intrauterine Demise |
| QF-PCR | Quantitative Fluorescent Polymerase Chain Reaction |
| SUA | Single Umbilical Artery |
| VACTERL | Vertebral Defects, Anal Atresia, Tracheoesophageal Fistula, Renal Dysplasia, and Limb Abnormalities |
| VD | Vaginal Delivery |
References
- Goldstein, I.; Makhoul, I.R.; Weissman, A.; Drugan, A. Hemivertebra: Prenatal Diagnosis, Incidence and Characteristics. Fetal Diagn. Ther. 2005, 20, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Forrester, M.B.; Merz, R.D. Descriptive Epidemiology of Hemivertebrae, Hawaii, 1986–2002. Congenit. Anom. 2006, 46, 172–176. [Google Scholar] [CrossRef] [PubMed]
- Varras, M.; Akrivis, C. Prenatal diagnosis of fetal hemivertebra at 20 weeks’ gestation with literature review. Int. J. Gen. Med. 2010, 3, 197–201. [Google Scholar] [CrossRef] [PubMed]
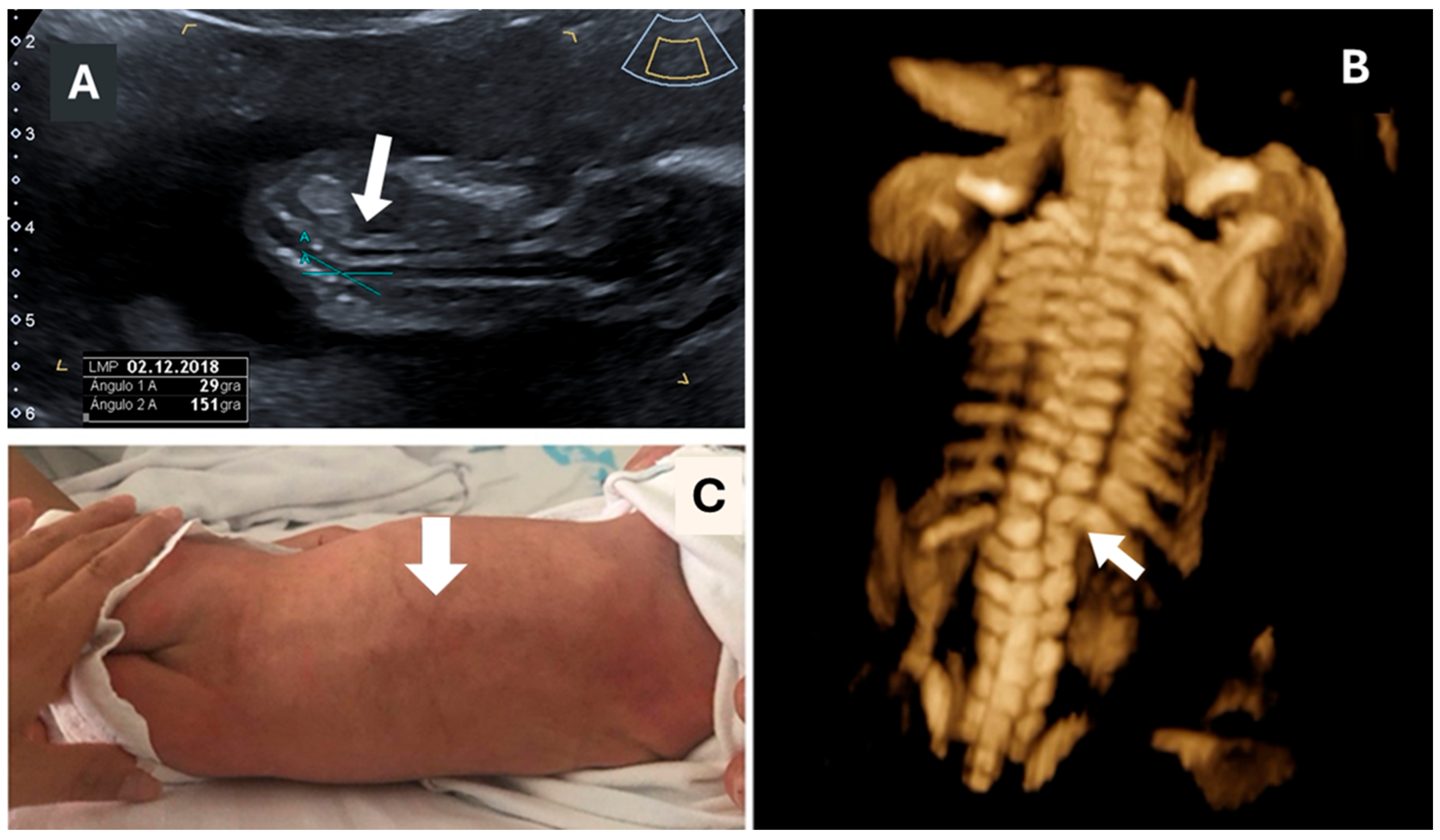
- Volpe, N.; Migliavacca, C.; Dall’Asta, A.; Kaihura, C.T.; Ghi, T.; Frusca, T. Prenatal Diagnosis of Fetal Multiple Hemivertebrae: The Importance of 3D Ultrasound Assessment. J. Matern. Neonatal Med. 2020, 33, 1755–1757. [Google Scholar] [CrossRef] [PubMed]
- Upasani, V.V.; Ketwaroo, P.D.; Estroff, J.A.; Warf, B.C.; Emans, J.B.; Glotzbecker, M.P. Prenatal Diagnosis and Assessment of Congenital Spinal Anomalies: Review for Prenatal Counseling. World J. Orthop. 2016, 7, 406–417. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, T.; Uhthoff, H.K. The Pathogenesis of Congenital Vertebral Malformations. A Study Based on Observations Made in 11 Human Embryos and Fetuses. Acta Orthop. Scand. 1981, 52, 413–425. [Google Scholar] [CrossRef] [PubMed]
- Alexander, P.G.; Tuan, R.S. Role of Environmental Factors in Axial Skeletal Dysmorphogenesis. Birth Defects Res. Part C-Embryo Today Rev. 2010, 90, 118–132. [Google Scholar] [CrossRef] [PubMed]
- Raitio, A.; Heiskanen, S.; Syvänen, J.; Leinonen, M.K.; Kemppainen, T.; Löyttyniemi, E.; Ahonen, M.; Gissler, M.; Helenius, I. Maternal Risk Factors for Congenital Vertebral Anomalies: A Population-Based Study. J. Bone Jt. Surg. 2023, 105, 1087–1092. [Google Scholar] [CrossRef] [PubMed]
- Hesemann, J.; Lauer, E.; Ziska, S.; Noonan, K.; Nemeth, B.; Scott-Schwoerer, J.; McCarty, C.; Rasmussen, K.; Goldberg, J.M.; Sund, S.; et al. Analysis of Maternal Risk Factors Associated with Congenital Vertebral Malformations. Spine 2013, 38, E293–E298. [Google Scholar] [CrossRef] [PubMed]
- Powel, J.E.; Sham, C.E.; Spiliopoulos, M.; Ferreira, C.R.; Rosenthal, E.; Sinkovskaya, E.S.; Brown, S.; Jelin, A.C.; Al-Kouatly, H.B. Genetics of Non-Isolated Hemivertebra: A Systematic Review of Fetal, Neonatal, and Infant Cases. Clin. Genet. 2022, 102, 262–287. [Google Scholar] [CrossRef] [PubMed]
- Wen, Y.; Xiang, G.; Liang, X.; Tong, X. The Clinical Value of Prenatal 3D Ultrasonic Diagnosis on Fetus Hemivertebra Deformity- A Preliminary Study. Curr. Med. Imaging Rev. 2018, 14, 139–142. [Google Scholar] [CrossRef] [PubMed]
- Basude, S.; Mcdermott, L.; Newell, S.; Wreyford, B.; Denbow, M.; Hutchinson, J.; Abdel-Fattah, S. Fetal Hemivertebra: Associations and Perinatal Outcome. Ultrasound Obstet. Gynecol. 2015, 45, 434–438. [Google Scholar] [CrossRef] [PubMed]
- Wax, J.R.; Watson, W.J.; Miller, R.C.; Ingardia, C.J.; Pinette, M.G.; Cartin, A.; Grimes, C.K.; Blackstone, J. Prenatal Sonographic Diagnosis of Hemivertebrae: Associations and Outcomes. J. Ultrasound Med. 2008, 27, 1023–1027. [Google Scholar] [CrossRef] [PubMed]
- Weisz, B.; Achiron, R.; Schindler, A.; Eisenberg, V.H.; Lipitz, S.; Zalel, Y. Prenatal Sonographic Diagnosis of Hemivertebra. J. Ultrasound Med. 2004, 23, 853–857. [Google Scholar] [CrossRef] [PubMed]
- Yulia, A.; Pawar, S.; Chelemen, O.; Ushakov, F.; Pandya, P.P. Fetal Hemivertebra at 11 to 14 Weeks’ Gestation. J. Ultrasound Med. 2020, 39, 1857–1863. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.; Chan, B.; Lam, T.P.W.; Shek, T.; Lee, C.P.; Tang, M.H.Y. Sonographic Features of Hemivertebra at 13 Weeks’ Gestation. J. Obstet. Gynaecol. Res. 2007, 33, 74–77. [Google Scholar] [CrossRef] [PubMed]
- Kalache, K.D.; Bamberg, C.; Proquitté, H.; Sarioglu, N.; Lebek, H.; Esser, T. Three-Dimensional Multi-Slice View: New Prospects for Evaluation of Congenital Anomalies in the Fetus. J. Ultrasound Med. 2006, 25, 1041–1049. [Google Scholar] [CrossRef] [PubMed]
- Lemire, G.T.; Beauregard-Lacroix, É.; Campeau, P.M.; Parent, S.; Roy-Beaudry, M.; Soglio, D.D.; Grignon, A.; Rypens, F.; Wavrant, S.; Laberge, A.M.; et al. Retrospective Analysis of Fetal Vertebral Defects: Associated Anomalies, Etiologies, and Outcome. Am. J. Med. Genet. Part A 2020, 182, 664–672. [Google Scholar] [CrossRef] [PubMed]
- Caredda, M.; Bandinelli, D.; Falciglia, F.; Giordano, M.; Aulisa, A.G. The Conservative Treatment of Congenital Scoliosis with Hemivertebra: Report of Three Cases. Front. Pediatr. 2022, 10, 951832. [Google Scholar] [CrossRef] [PubMed]

| Patient Number | Maternal Age (Years) | GA at Diagnosis (Weeks) | Amniocentesis /CVS | Localization | Single vs. Multiple | Fetal Gender | Syndromic Association | Other Malformations | Type of Delivery | Gestational Age at Delivery (Weeks) | Weight at Delivery (g) | Follow Up (Years) | Gestational Outcome | Evolution |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 40 | 12 | Yes | Dorsal | Single | Female | Marfan a | No | CS | 40 | 2695 | 1 | Live born | Asymptomatic, normal child life |
| 2 | 31 | 20 | Yes | Lumbar | Single | Male | No | No | VD | 36 | 2200 | 10 | Live born | Asymptomatic, normal child life |
| 3 | 20 | 20 | Yes | Lumbar + sacrum | Multiple | Male | No | Thallus foot | VD | 30 | 3160 | 11 | Live born | Trauma surgery at 7 years |
| 4 | 36 | 20 | No * | Sacrum | Single | Male | Unknown | No | VD | 39 | 3260 | 15 | Live born | Asymptomatic, normal child life |
| 5 | 34 | 20 | Yes | Lumbar | Single | Male | No | No | VD | 37 | 2940 | 13 | Live born | In a rehabilitation program, awaiting spinal surgery |
| 6 | 41 | 20 | Yes | Dorsal + lumbar | Multiple | Female | VACTERL | Renal agenesis, SUA | VD | 39 | 3620 | 9 | Live born | Vesico-ureteral fistula and anal surgeries |
| 7 | 36 | 20 | No * | Lumbar | Single | Male | Unknown | No | VD | 40 | 3320 | 0.2 | Live born | Asymptomatic, normal child life |
| 8 b | 20 | 20 | Yes | Dorsal | Single | Male | No | Hydrocephalus, SUA | - | - | - | - | IUD | - |
| 9 | 22 | 18 | No * | Thoracic | Multiple | Male | VACTERL | Ectopic kidney, partial pulmonary agenesis | CS | 33 | 2000 | 4 | Live born | In a rehabilitation program, awaiting spinal surgery |
| 10 | 38 | 19 | No * | Lumbar | Multiple | Male | No | No | CS | 38 | 2500 | 7 | Live born | Asymptomatic, normal child life |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costas, T.; Rodríguez, M.d.l.O.; Martín Esquilas, M.; Alarcón, V.; Goenaga, F.J.; Cabrero, M.Á.; Cubo, A.M. Long-Term Outcomes of Prenatally Diagnosed Fetal Hemivertebra: A 15-Year Single-Center Review. Children 2025, 12, 1236. https://doi.org/10.3390/children12091236
Costas T, Rodríguez MdlO, Martín Esquilas M, Alarcón V, Goenaga FJ, Cabrero MÁ, Cubo AM. Long-Term Outcomes of Prenatally Diagnosed Fetal Hemivertebra: A 15-Year Single-Center Review. Children. 2025; 12(9):1236. https://doi.org/10.3390/children12091236
Chicago/Turabian StyleCostas, Tatiana, María de la O Rodríguez, María Martín Esquilas, Verónica Alarcón, Francisco Javier Goenaga, María Ángeles Cabrero, and Ana María Cubo. 2025. "Long-Term Outcomes of Prenatally Diagnosed Fetal Hemivertebra: A 15-Year Single-Center Review" Children 12, no. 9: 1236. https://doi.org/10.3390/children12091236
APA StyleCostas, T., Rodríguez, M. d. l. O., Martín Esquilas, M., Alarcón, V., Goenaga, F. J., Cabrero, M. Á., & Cubo, A. M. (2025). Long-Term Outcomes of Prenatally Diagnosed Fetal Hemivertebra: A 15-Year Single-Center Review. Children, 12(9), 1236. https://doi.org/10.3390/children12091236






