Effect of Parental–Child Age Gaps and Skipped-Generation Families on Comorbidities Related to Attention Deficit Hyperactivity Disorder: A Population-Based Case–Control Study
Abstract
Highlights
- Older parental age is linked to higher risks of ASD and bipolar disorder in children with ADHD.
- Skipped-generation care increases emotional and behavioral comorbidities.
- Parental age and caregiving structure are key risk factors for ADHD comorbidities.
- Early screening may help guide targeted interventions.
Abstract
1. Introduction
- Examine associations between maternal and paternal age at childbirth and specific psychiatric and developmental comorbidities in children and adolescents with ADHD;
- Investigate the impact of skipped-generation family structures—conceptually defined as households with grandparent-paid insurance premiums and without parental cohabitation—on ADHD comorbidity patterns;
- Identify distinct comorbidity profiles associated with parental age extremes and grandparental caregiving to inform clinical risk stratification and family-centered intervention approaches.
2. Materials and Methods
2.1. Data Source
2.2. Study Population
2.3. Comorbidity Definitions
2.4. Definition of Parent–Child Age Gap and Skipped-Generation Family
2.5. Statistical Analysis
3. Results
3.1. Demographic Characteristics
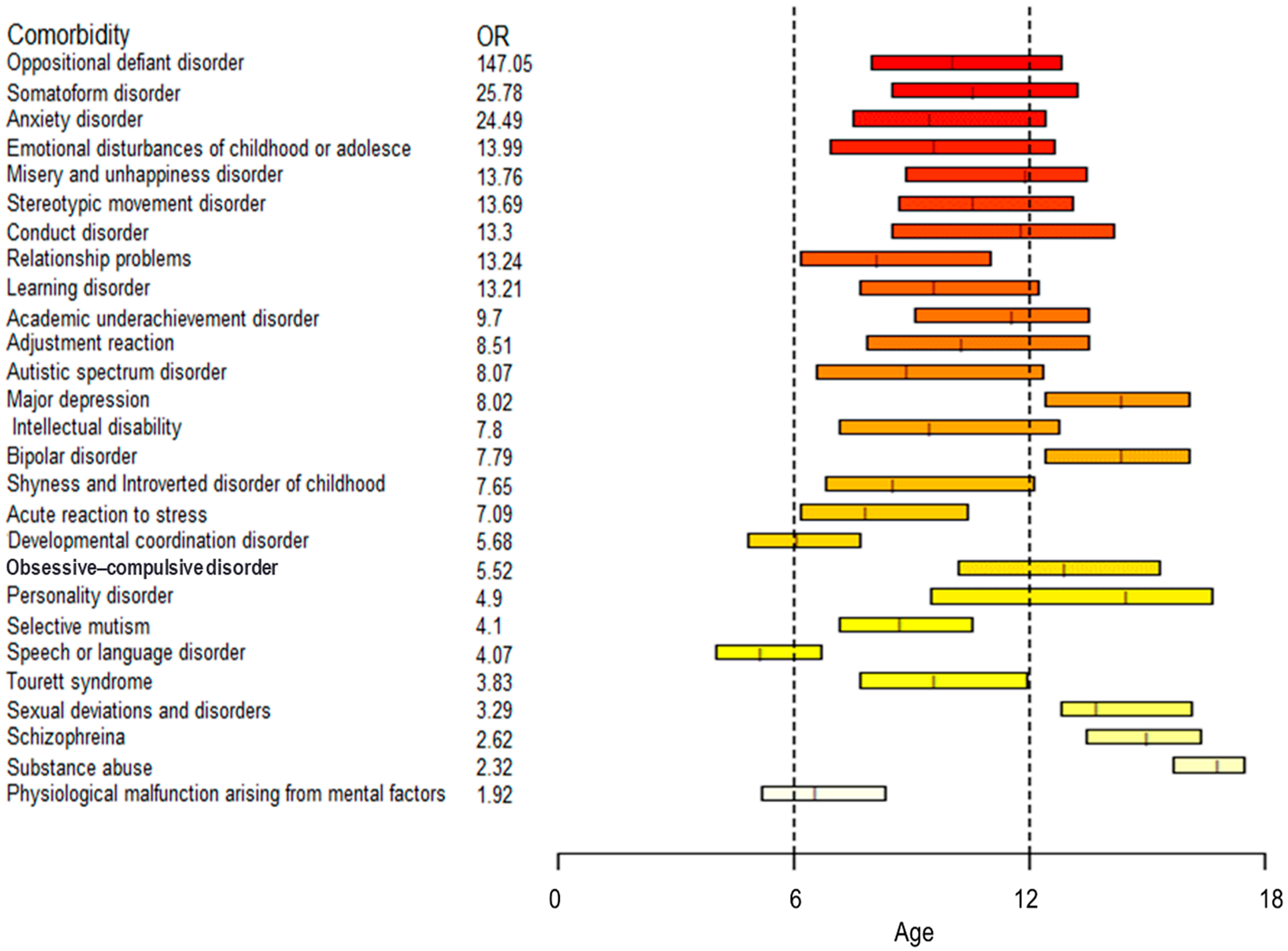
3.2. ADHD Comorbidities
- Age 0–6 years: ODD, somatoform disorder, anxiety disorder, academic underachievement disorder, and other personality disorders;
- Age 7–12 years: ODD, anxiety disorder, somatoform disorder, emotional disturbances, and learning disorder;
- Age 13–18 years: ODD, misery and unhappiness disorder, shyness and introverted disorder, stereotypic movement disorder, and learning disorder.
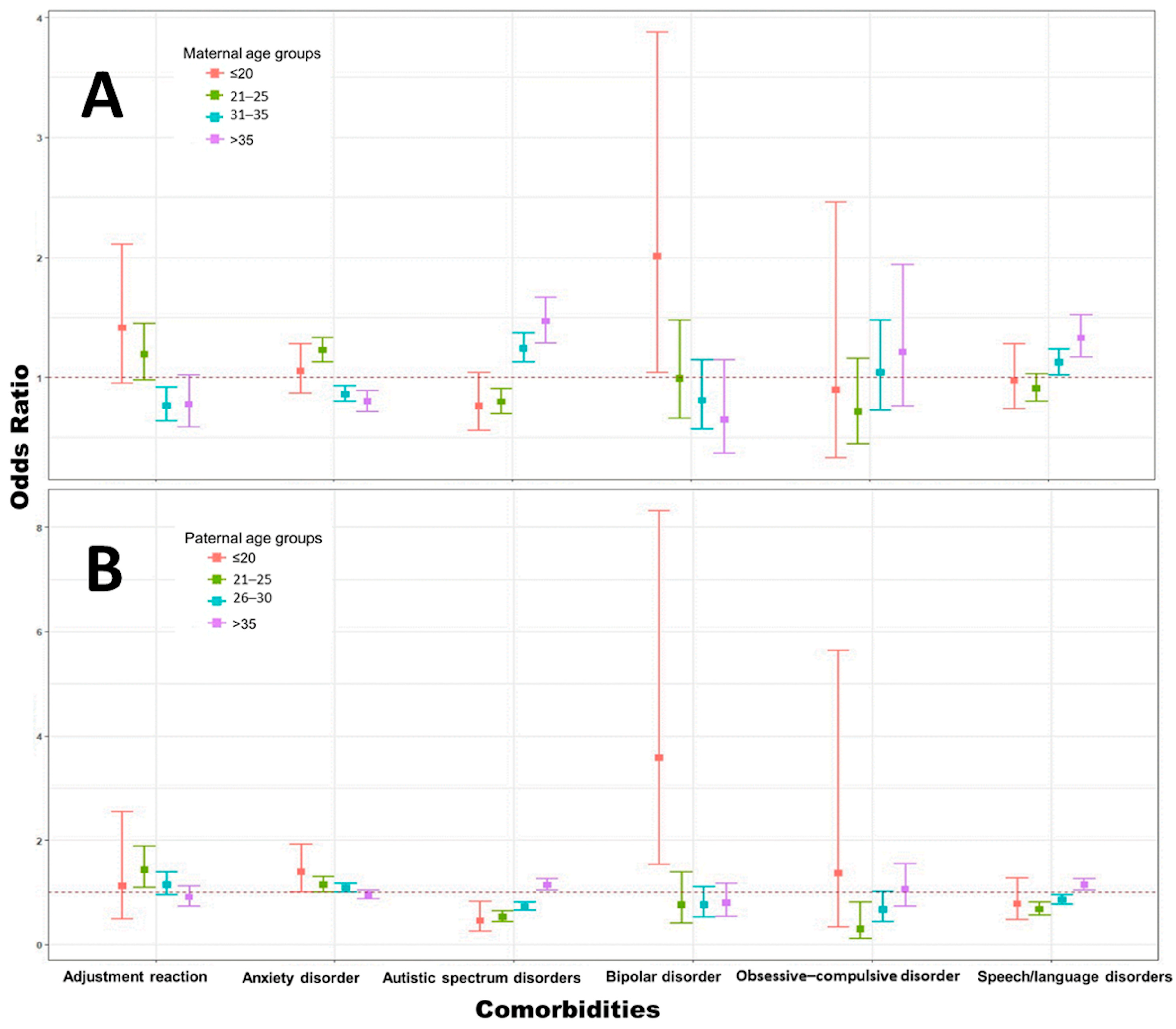
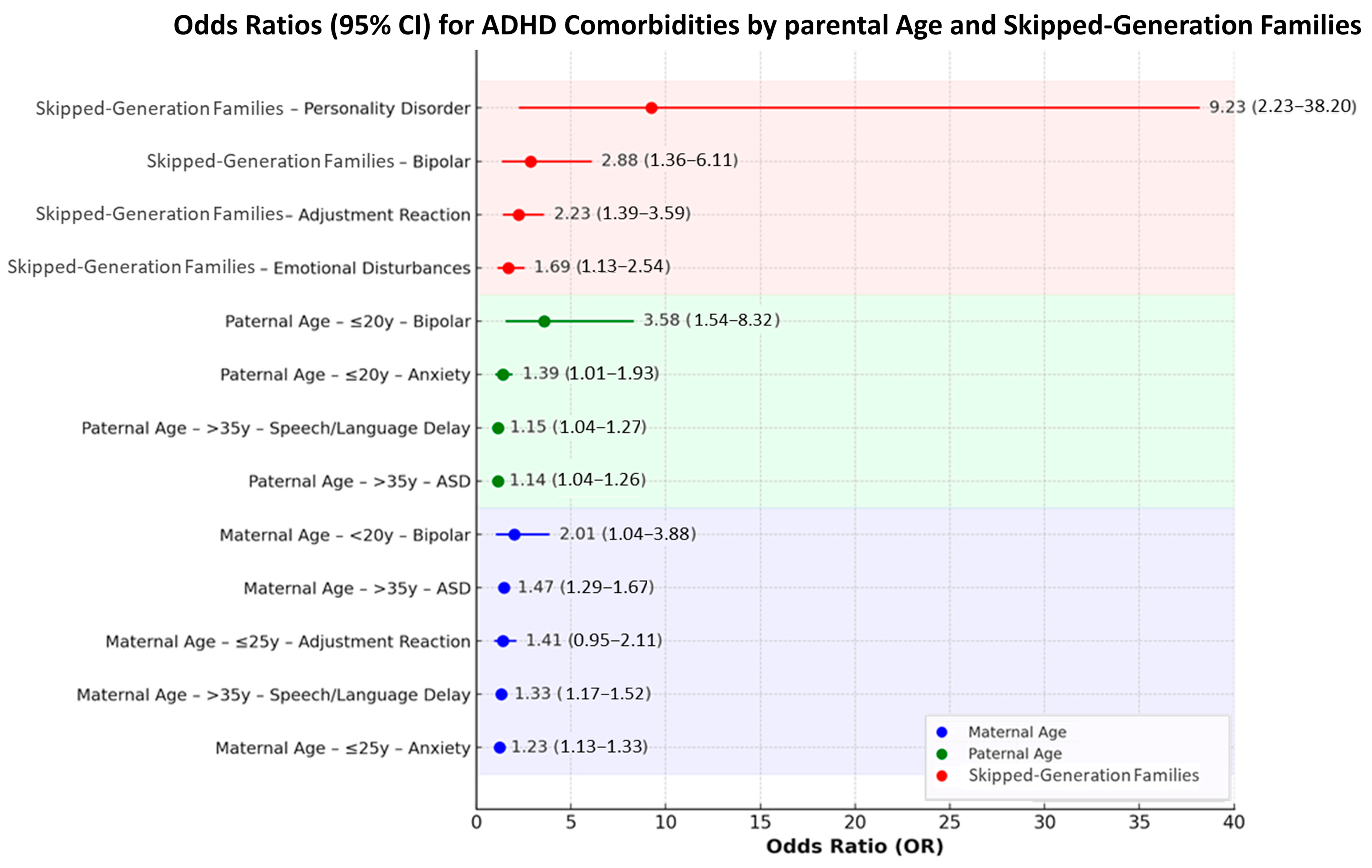
3.3. Impact of Parent–Child Age Gaps and Skipped-Generation Families on Common Comorbidities in Children with ADHD
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ADHD | Attention deficit/hyperactivity disorder |
| ASD | Autism spectrum disorder |
| DMDD | Disruptive mood dysregulation disorder |
| DSM-IV | Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition |
| ICD-9-CM | International Classification of Diseases, Ninth Revision, Clinical Modification |
| MACB | Maternal age at childbirth |
| NHIRD | National Health Insurance Research Database |
| OCD | Obsessive–compulsive disorder |
| ODD | Oppositional defiant disorder |
| ORs | Odds ratios |
| PACB | Paternal age at childbirth |
References
- Ayano, G.; Demelash, S.; Gizachew, Y.; Tsegay, L.; Alati, R. The global prevalence of attention deficit hyperactivity disorder in children and adolescents: An umbrella review of meta-analyses. J. Affect. Disord. 2023, 339, 860–866. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Yan, X.; Li, Q.; Li, Q.; Xu, G.; Lu, J.; Yang, W. Prevalence and Trends in Diagnosed ADHD Among US Children and Adolescents, 2017–2022. JAMA Netw. Open 2023, 6, e2336872. [Google Scholar] [CrossRef]
- Danielson, M.L.; Bitsko, R.H.; Ghandour, R.M.; Holbrook, J.R.; Kogan, M.D.; Blumberg, S.J. Prevalence of Parent-Reported ADHD Diagnosis and Associated Treatment Among U.S. Children and Adolescents, 2016. J. Clin. Child. Adolesc. Psychol. 2018, 47, 199–212. [Google Scholar] [CrossRef]
- Evans, S.W.; Owens, J.S.; Wymbs, B.T.; Ray, A.R. Evidence-Based Psychosocial Treatments for Children and Adolescents With Attention Deficit/Hyperactivity Disorder. J. Clin. Child. Adolesc. Psychol. 2018, 47, 157–198. [Google Scholar] [CrossRef]
- Lee, S.H.; Ripke, S.; Neale, B.M.; Faraone, S.V.; Purcell, S.M.; Perlis, R.H.; Mowry, B.J.; Thapar, A.; Goddard, M.E.; Witte, J.S.; et al. Genetic relationship between five psychiatric disorders estimated from genome-wide SNPs. Nat. Genet. 2013, 45, 984–994. [Google Scholar] [CrossRef]
- Demontis, D.; Walters, R.K.; Martin, J.; Mattheisen, M.; Als, T.D.; Agerbo, E.; Baldursson, G.; Belliveau, R.; Bybjerg-Grauholm, J.; Bækvad-Hansen, M.; et al. Discovery of the first genome-wide significant risk loci for attention deficit/hyperactivity disorder. Nat. Genet. 2019, 51, 63–75. [Google Scholar] [CrossRef]
- Faraone, S.V.; Larsson, H. Genetics of attention deficit hyperactivity disorder. Mol. Psychiatry 2019, 24, 562–575. [Google Scholar] [CrossRef]
- Taylor, M.J.; Martin, J.; Butwicka, A.; Lichtenstein, P.; D’Onofrio, B.; Lundström, S.; Larsson, H.; Rosenqvist, M.A. A twin study of genetic and environmental contributions to attention-deficit/hyperactivity disorder over time. J. Child. Psychol. Psychiatry 2023, 64, 1608–1616. [Google Scholar] [CrossRef]
- Taylor, M.J.; Martin, J.; Lu, Y.; Brikell, I.; Lundstrom, S.; Larsson, H.; Lichtenstein, P. Association of Genetic Risk Factors for Psychiatric Disorders and Traits of These Disorders in a Swedish Population Twin Sample. JAMA Psychiatry 2019, 76, 280–289. [Google Scholar] [CrossRef]
- Balint, S.; Bitter, I.; Czobor, P. Neurobiological correlates of cognitive flexibility in ADHD—A systematic review of the literature. Psychiatr. Hung. 2015, 30, 363–371. [Google Scholar] [PubMed]
- Chaim-Avancini, T.M.; Doshi, J.; Zanetti, M.V.; Erus, G.; Silva, M.A.; Duran, F.L.S.; Cavallet, M.; Serpa, M.H.; Caetano, S.C.; Louza, M.R.; et al. Neurobiological support to the diagnosis of ADHD in stimulant-naive adults: Pattern recognition analyses of MRI data. Acta Psychiatr. Scand. 2017, 136, 623–636. [Google Scholar] [CrossRef]
- Ercan, E.S.; Suren, S.; Bacanli, A.; Yazici, K.U.; Calli, C.; Ozyurt, O.; Aygunes, D.; Kosova, B.; Franco, A.R.; Rohde, L.A. Decreasing ADHD phenotypic heterogeneity: Searching for neurobiological underpinnings of the restrictive inattentive phenotype. Eur. Child. Adolesc. Psychiatry 2016, 25, 273–282. [Google Scholar] [CrossRef]
- Hart, H.; Chantiluke, K.; Cubillo, A.I.; Smith, A.B.; Simmons, A.; Brammer, M.J.; Marquand, A.F.; Rubia, K. Pattern classification of response inhibition in ADHD: Toward the development of neurobiological markers for ADHD. Hum. Brain Mapp. 2014, 35, 3083–3094. [Google Scholar] [CrossRef]
- Newcorn, J.H.; Ivanov, I.; Krone, B.; Li, X.; Duhoux, S.; White, S.; Schulz, K.P.; Bedard, A.V.; Pedraza, J.; Adler, L.; et al. Neurobiological basis of reinforcement-based decision making in adults with ADHD treated with lisdexamfetamine dimesylate: Preliminary findings and implications for mechanisms influencing clinical improvement. J. Psychiatr. Res. 2024, 170, 19–26. [Google Scholar] [CrossRef]
- Owens, M.M.; Allgaier, N.; Hahn, S.; Yuan, D.; Albaugh, M.; Adise, S.; Chaarani, B.; Ortigara, J.; Juliano, A.; Potter, A.; et al. Multimethod investigation of the neurobiological basis of ADHD symptomatology in children aged 9–10: Baseline data from the ABCD study. Transl. Psychiatry 2021, 11, 64. [Google Scholar] [CrossRef]
- Rommelse, N.; de Zeeuw, P. Neurobiological measures to classify ADHD: A critical appraisal. Eur. Child. Adolesc. Psychiatry 2014, 23, 243–246. [Google Scholar] [CrossRef]
- Schmitt, A.; Falkai, P. Neurobiological background of borderline personality disorder, PTSD and ADHD. Eur. Arch. Psychiatry Clin. Neurosci. 2016, 266, 289–290. [Google Scholar] [CrossRef]
- Shaw, P.; Polanczyk, G.V. Combining epidemiological and neurobiological perspectives to characterize the lifetime trajectories of ADHD. Eur. Child. Adolesc. Psychiatry 2017, 26, 139–141. [Google Scholar] [CrossRef]
- Saez, M.; Barcelo, M.A.; Farrerons, M.; Lopez-Casasnovas, G. The association between exposure to environmental factors and the occurrence of attention-deficit/hyperactivity disorder (ADHD). A population-based retrospective cohort study. Environ. Res. 2018, 166, 205–214. [Google Scholar] [CrossRef]
- Purece, A.; Thomsen, S.T.; Plass, D.; Spyropoulou, A.; Machera, K.; Palmont, P.; Crepet, A.; Benchrih, R.; Devleesschauwer, B.; Wieland, N.; et al. A preliminary estimate of the environmental burden of disease associated with exposure to pyrethroid insecticides and ADHD in Europe based on human biomonitoring. Environ. Health 2024, 23, 91. [Google Scholar] [CrossRef]
- Oh, J.; Kim, K.; Kannan, K.; Parsons, P.J.; Mlodnicka, A.; Schmidt, R.J.; Schweitzer, J.B.; Hertz-Picciotto, I.; Bennett, D.H. Early childhood exposure to environmental phenols and parabens, phthalates, organophosphate pesticides, and trace elements in association with attention deficit hyperactivity disorder (ADHD) symptoms in the CHARGE study. Res. Sq. 2023. [Google Scholar] [CrossRef]
- Moore, S.; Paalanen, L.; Melymuk, L.; Katsonouri, A.; Kolossa-Gehring, M.; Tolonen, H. The Association between ADHD and Environmental Chemicals-A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 2849. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, W. The association between attention deficit hyperactivity disorder (ADHD) and smoking experience or exposure to environmental tobacco smoke among children and adolescents. Tob. Induc. Dis. 2023, 21, 15. [Google Scholar] [CrossRef]
- Lebena, A.; Faresjo, A.; Jones, M.P.; Bengtsson, F.; Faresjo, T.; Ludvigsson, J. Early environmental predictors for attention-deficit hyperactivity disorder (ADHD), autism spectrum disorder (ASD) and their co-occurrence: The prospective ABIS-Study. Sci. Rep. 2024, 14, 14759. [Google Scholar] [CrossRef]
- Kim, J.H.; Kim, J.Y.; Lee, J.; Jeong, G.H.; Lee, E.; Lee, S.; Lee, K.H.; Kronbichler, A.; Stubbs, B.; Solmi, M.; et al. Environmental risk factors, protective factors, and peripheral biomarkers for ADHD: An umbrella review. Lancet Psychiatry 2020, 7, 955–970. [Google Scholar] [CrossRef]
- Faraone, S.V. Understanding Environmental Exposures and ADHD: A Pathway Forward. Prev. Sci. 2024, 25, 337–342. [Google Scholar] [CrossRef]
- Fan, H.C.; Chen, C.M.; Tsai, J.D.; Chiang, K.L.; Tsai, S.C.; Huang, C.Y.; Lin, C.L.; Hsu, C.Y.; Chang, K.H. Association between Exposure to Particulate Matter Air Pollution during Early Childhood and Risk of Attention-Deficit/Hyperactivity Disorder in Taiwan. Int. J. Environ. Res. Public Health 2022, 19, 16138. [Google Scholar] [CrossRef] [PubMed]
- Babadagi, Z.; Karabekiroglu, K.M.Z.; Ucar, F.; Say, G.N.; Yuce, M.; Yildirim, Z.G. Associations Between Father Temperament, Character, Rearing, Psychopathology and Child Temperament in Children Aged 3–6 Years. Psychiatr. Q. 2018, 89, 589–604. [Google Scholar] [CrossRef]
- Janecka, M.; Mill, J.; Basson, M.A.; Goriely, A.; Spiers, H.; Reichenberg, A.; Schalkwyk, L.; Fernandes, C. Advanced paternal age effects in neurodevelopmental disorders-review of potential underlying mechanisms. Transl. Psychiatry 2017, 7, e1019. [Google Scholar] [CrossRef]
- McGrath, J.J.; Petersen, L.; Agerbo, E.; Mors, O.; Mortensen, P.B.; Pedersen, C.B. A comprehensive assessment of parental age and psychiatric disorders. JAMA Psychiatry 2014, 71, 301–309. [Google Scholar] [CrossRef]
- Nilsen, A.B.; Waldenstrom, U.; Rasmussen, S.; Hjelmstedt, A.; Schytt, E. Characteristics of first-time fathers of advanced age: A Norwegian population-based study. BMC Pregnancy Childbirth 2013, 13, 29. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.H.; Wu, C.S.; Hsu, L.Y.; Lin, M.C.; Chen, P.C.; Thompson, W.K.; Fan, C.C. Paternal age and 13 psychiatric disorders in the offspring: A population-based cohort study of 7 million children in Taiwan. Mol. Psychiatry 2022, 27, 5244–5254. [Google Scholar] [CrossRef] [PubMed]
- Chittleborough, C.R.; Lawlor, D.A.; Lynch, J.W. Young maternal age and poor child development: Predictive validity from a birth cohort. Pediatrics 2011, 127, e1436–e1444. [Google Scholar] [CrossRef]
- Falster, K.; Hanly, M.; Banks, E.; Lynch, J.; Chambers, G.; Brownell, M.; Eades, S.; Jorm, L. Maternal age and offspring developmental vulnerability at age five: A population-based cohort study of Australian children. PLoS Med. 2018, 15, e1002558. [Google Scholar] [CrossRef]
- Jutte, D.P.; Roos, N.P.; Brownell, M.D.; Briggs, G.; MacWilliam, L.; Roos, L.L. The ripples of adolescent motherhood: Social, educational, and medical outcomes for children of teen and prior teen mothers. Acad. Pediatr. 2010, 10, 293–301. [Google Scholar] [CrossRef] [PubMed]
- Shaw, M.; Lawlor, D.A.; Najman, J.M. Teenage children of teenage mothers: Psychological, behavioural and health outcomes from an Australian prospective longitudinal study. Soc. Sci. Med. 2006, 62, 2526–2539. [Google Scholar] [CrossRef]
- Turley, R.N. Are children of young mothers disadvantaged because of their mother’s age or family background? Child. Dev. 2003, 74, 465–474. [Google Scholar] [CrossRef]
- Shang, L.D.; Rowe, F.; Lin, E.S. Estimating the causal impact of non-traditional household structures on children’s educational performance using a machine learning propensity score. Asia Pacific Educ. Rev. 2024, 25, 939–957. [Google Scholar] [CrossRef]
- Paulus, F.W.; Ohmann, S.; Mohler, E.; Plener, P.; Popow, C. Emotional Dysregulation in Children and Adolescents With Psychiatric Disorders. A Narrative Review. Front. Psychiatry 2021, 12, 628252. [Google Scholar] [CrossRef]
- Wang, Y.W.; Liu, C.C.; Chen, H.C.; Wu, C.S.; Chan, J.H.; Chen, C.C.; Huang, W.L.; Liao, S.C.; Hwang, T.J.; Chen, W.J. Assessing the Validity of Claims-Based Diagnostic Codes for Psychotic and Affective Disorders and the Influence of the Coding Transition from the ICD-9 to the ICD-10 in Taiwan’s National Health Insurance Research Database. Clin. Epidemiol. 2025, 17, 635–645. [Google Scholar] [CrossRef]
- Liu, Y.C.; Liao, Y.T.; Chen, V.C.; Chen, Y.L. ADHD and Risk of Precocious Puberty: Considering the Impact of MPH. Biomedicines 2024, 12, 2304. [Google Scholar] [CrossRef]
- Polanczyk, G.V.; Salum, G.A.; Sugaya, L.S.; Caye, A.; Rohde, L.A. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J. Child. Psychol. Psychiatry 2015, 56, 345–365. [Google Scholar] [CrossRef]
- French, B.; Nalbant, G.; Wright, H.; Sayal, K.; Daley, D.; Groom, M.J.; Cassidy, S.; Hall, C.L. The impacts associated with having ADHD: An umbrella review. Front. Psychiatry 2024, 15, 1343314. [Google Scholar] [CrossRef] [PubMed]
- Biederman, J.; Faraone, S.V. The effects of attention-deficit/hyperactivity disorder on employment and household income. MedGenMed 2006, 8, 12. [Google Scholar] [PubMed]
- Bertelsen, E.N.; Larsen, J.T.; Petersen, L.; Christensen, J.; Dalsgaard, S. Childhood Epilepsy, Febrile Seizures, and Subsequent Risk of ADHD. Pediatrics 2016, 138, e20154654. [Google Scholar] [CrossRef]
- Faraone, S.V.; Asherson, P.; Banaschewski, T.; Biederman, J.; Buitelaar, J.K.; Ramos-Quiroga, J.A.; Rohde, L.A.; Sonuga-Barke, E.J.; Tannock, R.; Franke, B. Attention-deficit/hyperactivity disorder. Nat. Rev. Dis. Primers 2015, 1, 15020. [Google Scholar] [CrossRef]
- Jensen, P.S.; Hinshaw, S.P.; Kraemer, H.C.; Lenora, N.; Newcorn, J.H.; Abikoff, H.B.; March, J.S.; Arnold, L.E.; Cantwell, D.P.; Conners, C.K.; et al. ADHD comorbidity findings from the MTA study: Comparing comorbid subgroups. J. Am. Acad. Child. Adolesc. Psychiatry 2001, 40, 147–158. [Google Scholar] [CrossRef]
- Reale, L.; Bartoli, B.; Cartabia, M.; Zanetti, M.; Costantino, M.A.; Canevini, M.P.; Termine, C.; Bonati, M.; Lombardy, A.G. Comorbidity prevalence and treatment outcome in children and adolescents with ADHD. Eur. Child. Adolesc. Psychiatry 2017, 26, 1443–1457. [Google Scholar] [CrossRef]
- Spencer, T.J. ADHD and comorbidity in childhood. J. Clin. Psychiatry 2006, 67, 27–31. [Google Scholar]
- Fristad, M.A.; Wolfson, H.; Algorta, G.P.; Youngstrom, E.A.; Arnold, L.E.; Birmaher, B.; Horwitz, S.; Axelson, D.; Kowatch, R.A.; Findling, R.L.; et al. Disruptive Mood Dysregulation Disorder and Bipolar Disorder Not Otherwise Specified: Fraternal or Identical Twins? J. Child. Adolesc. Psychopharmacol. 2016, 26, 138–146. [Google Scholar] [CrossRef] [PubMed]
- Roehr, B. American Psychiatric Association explains DSM-5. BMJ 2013, 346, f3591. [Google Scholar] [CrossRef]
- Chen, V.C.; Yang, Y.H.; Yu Kuo, T.; Lu, M.L.; Tseng, W.T.; Hou, T.Y.; Yeh, J.Y.; Lee, C.T.; Chen, Y.L.; Lee, M.J.; et al. Methylphenidate and the risk of burn injury among children with attention-deficit/hyperactivity disorder. Epidemiol. Psychiatr. Sci. 2020, 29, e146. [Google Scholar] [CrossRef]
- Lee, P.H.; Doyle, A.E.; Li, X.; Silberstein, M.; Jung, J.Y.; Gollub, R.L.; Nierenberg, A.A.; Liu, R.T.; Kessler, R.C.; Perlis, R.H.; et al. Genetic Association of Attention-Deficit/Hyperactivity Disorder and Major Depression With Suicidal Ideation and Attempts in Children: The Adolescent Brain Cognitive Development Study. Biol. Psychiatry 2022, 92, 236–245. [Google Scholar] [CrossRef]
- Liu, Y.C.; Chen, V.C.; Yang, Y.H.; Chen, Y.L.; Gossop, M. Association of psychiatric comorbidities with the risk of transport accidents in ADHD and MPH. Epidemiol. Psychiatr. Sci. 2021, 30, e14. [Google Scholar] [CrossRef] [PubMed]
- Mangus, R.S.; Bergman, D.; Zieger, M.; Coleman, J.J. Burn injuries in children with attention-deficit/hyperactivity disorder. Burns 2004, 30, 148–150. [Google Scholar] [CrossRef]
- Liu, S.T.; Tsai, F.J.; Lee, W.T.; Lee, C.M.; Fan, P.C.; Lin, W.S.; Chiu, Y.N.; Gau, S.S. Attentional processes and ADHD-related symptoms in pediatric patients with epilepsy. Epilepsy Res. 2011, 93, 53–65. [Google Scholar] [CrossRef]
- Min, X.; Li, C.; Yan, Y. Parental Age and the Risk of ADHD in Offspring: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 4939. [Google Scholar] [CrossRef]
- Croen, L.A.; Najjar, D.V.; Fireman, B.; Grether, J.K. Maternal and paternal age and risk of autism spectrum disorders. Arch. Pediatr. Adolesc. Med. 2007, 161, 334–340. [Google Scholar] [CrossRef]
- Sandin, S.; Hultman, C.M.; Kolevzon, A.; Gross, R.; MacCabe, J.H.; Reichenberg, A. Advancing maternal age is associated with increasing risk for autism: A review and meta-analysis. J. Am. Acad. Child. Adolesc. Psychiatry 2012, 51, 477–486. [Google Scholar] [CrossRef] [PubMed]
- Tearne, J.E.; Robinson, M.; Jacoby, P.; Allen, K.L.; Cunningham, N.K.; Li, J.; McLean, N.J. Older maternal age is associated with depression, anxiety, and stress symptoms in young adult female offspring. J. Abnorm. Psychol. 2016, 125, 1–10. [Google Scholar] [CrossRef]
- Tearne, J.E. Older maternal age and child behavioral and cognitive outcomes: A review of the literature. Fertil. Steril. 2015, 103, 1381–1391. [Google Scholar] [CrossRef] [PubMed]
- de Kluiver, H.; Buizer-Voskamp, J.E.; Dolan, C.V.; Boomsma, D.I. Paternal age and psychiatric disorders: A review. Am. J. Med. Genet. B Neuropsychiatr. Genet. 2017, 174, 202–213. [Google Scholar] [CrossRef] [PubMed]
- Gabis, L.; Raz, R.; Kesner-Baruch, Y. Paternal age in autism spectrum disorders and ADHD. Pediatr. Neurol. 2010, 43, 300–302. [Google Scholar] [CrossRef]
- Merikangas, A.K.; Calkins, M.E.; Bilker, W.B.; Moore, T.M.; Gur, R.C.; Gur, R.E. Parental Age and Offspring Psychopathology in the Philadelphia Neurodevelopmental Cohort. J. Am. Acad. Child. Adolesc. Psychiatry 2017, 56, 391–400. [Google Scholar] [CrossRef]
- Geronimus, A.T.; Korenman, S.; Hillemeier, M.M. Do young maternal ages adversely affect child development? Evidence from cousin comparisons in the United States. Popul. Dev. Rev. 1994, 20, 585–609. [Google Scholar] [CrossRef]
- Shaw, P.; Lerch, J.; Greenstein, D.; Sharp, W.; Clasen, L.; Evans, A.; Giedd, J.; Castellanos, F.X.; Rapoport, J. Longitudinal mapping of cortical thickness and clinical outcome in children and adolescents with attention-deficit/hyperactivity disorder. Arch. Gen. Psychiatry 2006, 63, 540–549. [Google Scholar] [CrossRef]
- Wang, Y.T.; Yang, W.S. Changes and trends in family structure in Taiwan, 1990 to 2010. J. Fam. Issues 2019, 40, 1896–1911. [Google Scholar] [CrossRef]
- Gender Equality Committee, Executive Yuan. Available online: https://gec.ey.gov.tw/en/ (accessed on 30 June 2025).
- Wu, Y.; Muentener, P.; Schulz, L.E. One- to four-year-olds connect diverse positive emotional vocalizations to their probable causes. Proc. Natl. Acad. Sci. USA 2017, 114, 11896–11901. [Google Scholar] [CrossRef]
- Weisleder, A.; Fernald, A. Talking to children matters: Early language experience strengthens processing and builds vocabulary. Psychol. Sci. 2013, 24, 2143–2152. [Google Scholar] [CrossRef]
- Leonard, J.A.; Lee, Y.; Schulz, L.E. Infants make more attempts to achieve a goal when they see adults persist. Science 2017, 357, 1290–1294. [Google Scholar] [CrossRef]
- Knudsen, E.I.; Heckman, J.J.; Cameron, J.L.; Shonkoff, J.P. Economic, neurobiological, and behavioral perspectives on building America’s future workforce. Proc. Natl. Acad. Sci. USA 2006, 103, 10155–10162. [Google Scholar] [CrossRef]
- Attar-Schwartz, S.; Tan, J.P.; Buchanan, A.; Flouri, E.; Griggs, J. Grandparenting and adolescent adjustment in two-parent biological, lone-parent, and step-families. J. Fam. Psychol. 2009, 23, 67–75. [Google Scholar] [CrossRef]
- Luo, Y.; Qi, M.; Huntsinger, C.S.; Zhang, Q.; Xuan, X.; Wang, Y. Grandparent involvement and preschoolers’ social adjustment in Chinese three-generation families: Examining moderating and mediating effects. Child. Youth Serv. Rev. 2020, 114, 105057. [Google Scholar] [CrossRef]
- Li, Y.; Cui, N.; Kok, H.T.; Deatrick, J.; Liu, J. The relationship between parenting styles practiced by grandparents and children’s emotional and behavioral problems. J. Child. Fam. Stud. 2019, 28, 1899–1913. [Google Scholar] [CrossRef]
- Demontis, D.; Walters, R.K.; Rajagopal, V.M.; Waldman, I.D.; Grove, J.; Als, T.D.; Dalsgaard, S.; Ribases, M.; Bybjerg-Grauholm, J.; Bækvad-Hansen, M. Risk variants and polygenic architecture of disruptive behavior disorders in the context of attention-deficit/hyperactivity disorder. Nat. Commun. 2021, 12, 576. [Google Scholar] [CrossRef]
- Jiang, W.; Li, Y.; Du, Y.; Fan, J. Emotional regulation and executive function deficits in unmedicated Chinese children with oppositional defiant disorder. Psychiatry Investig. 2016, 13, 277. [Google Scholar] [CrossRef]
- Minkler, M.; Fuller-Thomson, E.; Miller, D.; Driver, D. Depression in grandparents raising grandchildren: Results of a national longitudinal study. Arch. Fam. Med. 1997, 6, 445–452. [Google Scholar] [CrossRef] [PubMed]
- Vousoura, E.; Verdeli, H.; Warner, V.; Wickramaratne, P.; Baily, C.D.R. Parental Divorce, Familial Risk for Depression, and Psychopathology in Offspring: A Three-Generation Study. J. Child. Fam. Stud. 2012, 21, 718–725. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, S.A.; Silverstein, M. Relationships with grandparents and the emotional well-being of late adolescent and young adult grandchildren. J. Soc. Issues 2007, 63, 793–808. [Google Scholar] [CrossRef]
- Dunifon, R.E.; Ziol-Guest, K.M.; Kopko, K. Grandparent Coresidence and Family Well-Being: Implications for Research and Policy. Ann. Am. Acad. Pol. Soc. Sci. 2014, 654, 110–126. [Google Scholar] [CrossRef]
- Tong, L.; Kawachi, I. Factors moderating the link between early childhood non-parental care and ADHD symptoms. Heliyon 2021, 7, e08562. [Google Scholar] [CrossRef] [PubMed]
- Sari, E.; Moilanen, M.; Lindeboom, M. Long-term effects of grandparental child neglect on adult grandchildren’s mental health: A three-generation study. SSM Popul. Health 2024, 28, 101712. [Google Scholar] [CrossRef]


| ADHD Patients | Control Group | p-Value | |||
|---|---|---|---|---|---|
| n = 79,163 | Percentile | n = 395,815 | Percentile | ||
| Characteristic | |||||
| Sex | |||||
| Female | 16,295 | 20.58% | 81,475 | 20.58% | |
| Male | 62,868 | 79.42% | 314,340 | 79.42% | 1.00 |
| Age (years) | |||||
| 0–6 | 16,869 | 21.31% | 84,345 | 21.31% | |
| 7–12 | 45,524 | 57.51% | 22,7620 | 57.51% | |
| 13–18 | 16,770 | 21.18% | 83,850 | 21.18% | 1.00 |
| * Maternal age | |||||
| ≤20 | 900 | 2.47% | 5329 | 2.85% | |
| 21–25 | 6175 | 16.92% | 34,588 | 18.5% | |
| 26–30 | 14,538 | 39.83% | 76,240 | 40.78% | |
| 31–35 | 11,057 | 30.29% | 54,411 | 29.1% | |
| >35 | 3834 | 10.5% | 16,403 | 8.77% | <0.01 |
| * Paternal age | |||||
| ≤20 | 270 | 0.85% | 1669 | 1.04% | |
| 21–25 | 2516 | 7.92% | 14,311 | 8.93% | |
| 26–30 | 9327 | 29.38% | 47,636 | 29.72% | |
| 31–35 | 11,266 | 35.48% | 56,313 | 35.13% | |
| >35 | 8371 | 26.37% | 40,364 | 25.18% | <0.01 |
| * Skipped-generation family | |||||
| Yes | 381 | 0.48% | 1637 | 0.41% | |
| No | 78,782 | 99.52% | 394,178 | 99.59% | <0.01 |
| Comorbidity | Yes (n = 381) | No (n = 78,782) | OR | 95% CI | p-Value |
|---|---|---|---|---|---|
| Oppositional defiant disorder | 31 | 6079 | 1.06 | (0.73, 1.53) | 0.830 |
| Somatoform disorder | 3 | 758 | 0.82 | (0.26, 2.55) | 0.930 |
| Anxiety disorder | 44 | 10,515 | 0.85 | (0.62, 1.16) | 0.340 |
| Emotional disturbances during childhood and adolescence | 25 | 3138 | 1.69 | (1.13, 2.54) | 0.015 * |
| Misery and unhappiness disorder | 1 | 54 | 3.84 | (0.53, 27.80) | 0.650 |
| Stereotypic movement disorder | 0 | 52 | --- | --- | 1.000 |
| Conduct disorder | 11 | 1474 | 1.56 | (0.85, 2.85) | 0.200 |
| Relationship problems | 3 | 1231 | 0.50 | (0.16, 1.60) | 0.310 |
| Learning disorder | 13 | 2220 | 1.22 | (0.70, 2.12) | 0.590 |
| Identity disorders during childhood and adolescence | 0 | 5 | --- | --- | 1.000 |
| Academic underachievement disorder | 0 | 207 | --- | --- | 0.620 |
| The adjustment reaction | 18 | 1713 | 2.23 | (1.39, 3.59) | <0.01 ** |
| Autistic spectrum disorder | 20 | 5641 | 0.72 | (0.46, 1.13) | 0.180 |
| Bipolar disorder | 7 | 509 | 2.88 | (1.36, 6.11) | 0.010 * |
| Shyness and introverted disorder in childhood | 0 | 107 | --- | --- | 0.980 |
| Acute reaction to stress | 1 | 190 | 1.09 | (0.15, 7.79) | 1.000 |
| Obsessive–compulsive disorder | 2 | 370 | 1.12 | (0.28, 4.47) | 1.000 |
| Personality disorder | 2 | 45 | 9.23 | (2.23, 38.20) | <0.01 ** |
| Speech or language developmental disorder | 19 | 5621 | 0.68 | (0.43, 1.08) | 0.130 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fan, H.-C.; Kuo, F.-C.; Lee, J.-Y.; Chang, Y.-M.; Chiang, K.-T.; Chiang, K.-L. Effect of Parental–Child Age Gaps and Skipped-Generation Families on Comorbidities Related to Attention Deficit Hyperactivity Disorder: A Population-Based Case–Control Study. Children 2025, 12, 1123. https://doi.org/10.3390/children12091123
Fan H-C, Kuo F-C, Lee J-Y, Chang Y-M, Chiang K-T, Chiang K-L. Effect of Parental–Child Age Gaps and Skipped-Generation Families on Comorbidities Related to Attention Deficit Hyperactivity Disorder: A Population-Based Case–Control Study. Children. 2025; 12(9):1123. https://doi.org/10.3390/children12091123
Chicago/Turabian StyleFan, Hueng-Chuen, Fang-Chuan Kuo, Jen-Yu Lee, Yu-Mei Chang, Kuo-Tung Chiang, and Kuo-Liang Chiang. 2025. "Effect of Parental–Child Age Gaps and Skipped-Generation Families on Comorbidities Related to Attention Deficit Hyperactivity Disorder: A Population-Based Case–Control Study" Children 12, no. 9: 1123. https://doi.org/10.3390/children12091123
APA StyleFan, H.-C., Kuo, F.-C., Lee, J.-Y., Chang, Y.-M., Chiang, K.-T., & Chiang, K.-L. (2025). Effect of Parental–Child Age Gaps and Skipped-Generation Families on Comorbidities Related to Attention Deficit Hyperactivity Disorder: A Population-Based Case–Control Study. Children, 12(9), 1123. https://doi.org/10.3390/children12091123






