Increased Utilization of Abdominal Surgical Procedures, Endoscopy and Imaging After Negative Rectal Biopsies for Suspected Hirschsprung’s Disease: A Danish Nationwide Matched Cohort Study
Abstract
1. Introduction
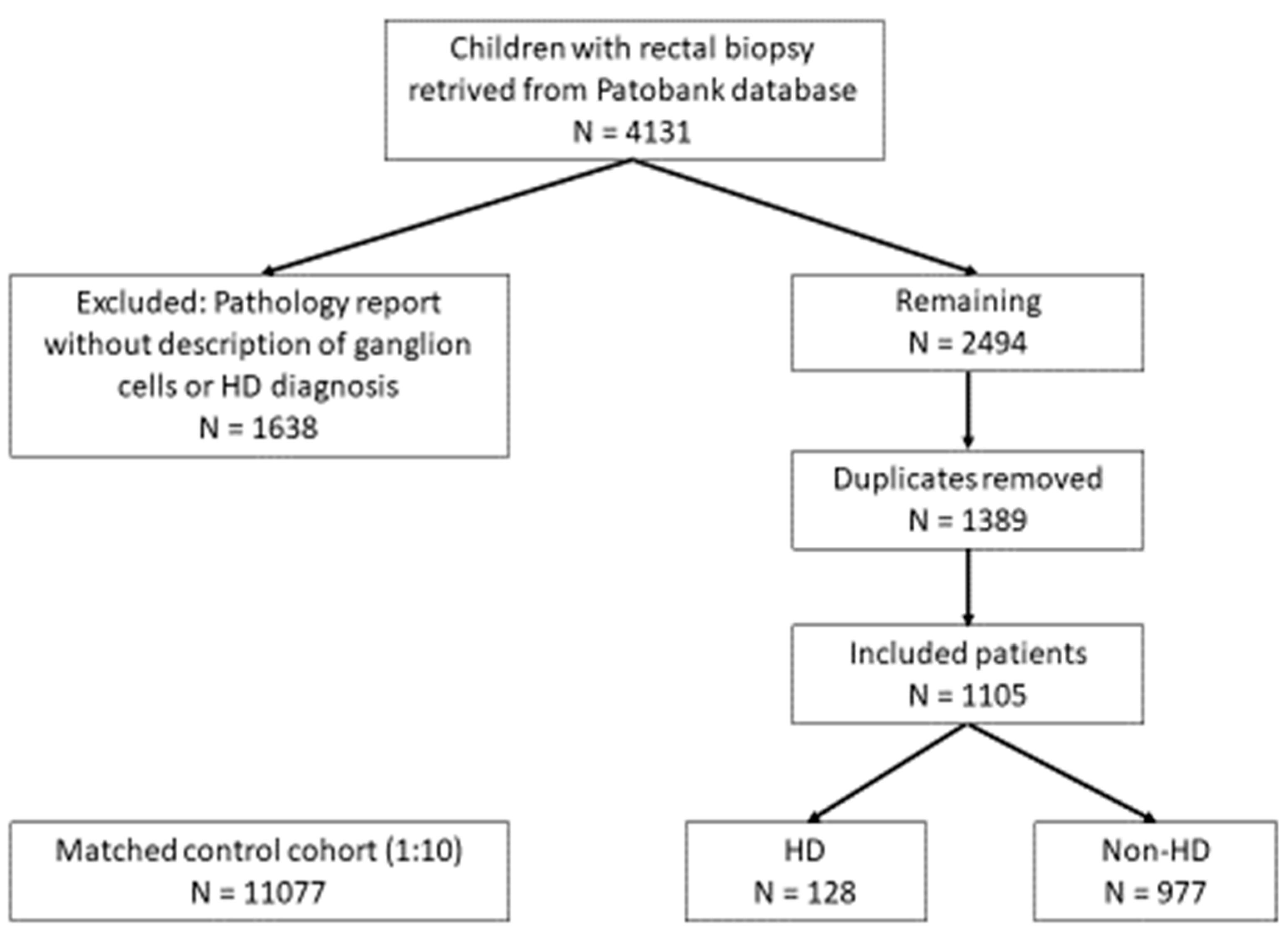
2. Materials and Methods
2.1. Study Design
2.2. Setting
2.3. Population
2.4. Outcomes
2.5. Covariates
2.6. Statistical Analysis
2.7. Data Management
3. Results
3.1. Surgery
3.2. Endoscopy
3.3. Imaging
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- van den Berg, M.M.; Benninga, M.A.; Di Lorenzo, C. Epidemiology of childhood constipation: A systematic review. Am. J. Gastroenterol. 2006, 101, 2401–2409. [Google Scholar] [CrossRef] [PubMed]
- National Institute for Health and Care Excellence (NICE). Available online: https://www.nice.org.uk/guidance/cg99 (accessed on 29 May 2025).
- Best, K.E.; Addor, M.C.; Arriola, L.; Balku, E.; Barisic, I.; Bianchi, F.; Calzolari, E.; Curran, R.; Dorau, B.; Draper, E.; et al. Hirschsprung’s disease prevalence in Europe: A register based study. Birth Defects Res. A Clin. Mol. Teratol. 2014, 100, 695–702. [Google Scholar] [CrossRef] [PubMed]
- Kyrklund, K.; Sloots, C.E.J.; de Blaauw, I.; Bjørnland, K.; Rolle, U.; Cavalieri, D.; Francalanci, P.; Fusaro, F.; Lemli, A.; Schwartzer, N.; et al. ERNICA guidelines for the management of rectosigmoid Hirschsprung’s disease. Orphanet J. Rare Dis. 2020, 15, 164. [Google Scholar] [CrossRef]
- Allen, A.R.; Putnam, A.R.; Presson, A.P.; Allen, C.M.; Barnhart, D.C.; Rollins, M.D. Accuracy of suction rectal biopsy for diagnosis of Hirschsprung’s disease in neonates. Eur. J. Pediatr. Surg. 2019, 29, 425–430. [Google Scholar] [CrossRef]
- Bjørn, N.; Rasmussen, L.; Qvist, N.; Detlefsen, S.; Ellebæk, M.B. Full-thickness rectal biopsy in children suspicious for Hirschsprung’s disease is safe and yields a low number of insufficient biopsies. J. Pediatr. Surg. 2018, 53, 1942–1944. [Google Scholar] [CrossRef] [PubMed]
- Friedmacher, F.; Puri, P. Rectal suction biopsy for the diagnosis of Hirschsprung’s disease: A systematic review of diagnostic accuracy and complications. Pediatr. Surg. Int. 2015, 31, 821–830. [Google Scholar] [CrossRef] [PubMed]
- Tran, K.; Staller, K.; Macklin, E.; Goldstein, A.; Belkind-Gerson, J.; Kuo, B. Need for rectal biopsy for childhood constipation predicts severity of illness and need for laxatives. J. Pediatr. Gastroenterol. Nutr. 2016, 62, 834–839. [Google Scholar] [CrossRef] [PubMed]
- Harlev, D.; Kharenko, O.; Waxman, J.; Frankel, T.; Turner, D.; Ledder, O. Long-term outcome of neonates with suspected Hirschsprung’s disease, but normal rectal biopsy. Eur. J. Gastroenterol. Hepatol. 2016, 28, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Belsey, J.; Greenfield, S.; Candy, D.; Geraint, M. Systematic review: Impact of constipation on quality of life in adults and children. Aliment. Pharmacol. Ther. 2010, 31, 938–949. [Google Scholar] [CrossRef] [PubMed]
- Liem, O.; Harman, J.; Benninga, M.; Kelleher, K.; Mousa, H.; Di Lorenzo, C. Health utilization and cost impact of childhood constipation in the United States. J. Pediatr. 2009, 154, 258–262. [Google Scholar] [CrossRef] [PubMed]
- Statistics Denmark. Available online: https://www.dst.dk/da/Statistik/emner/borgere/befolkning/befolkningstal (accessed on 29 May 2025).
- Bjerregaard, B.; Larsen, O.B. The Danish Pathology Register. Scand. J. Public Health 2011, 39, 72–74. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Pedersen, L.; Sørensen, H.T. The Danish civil registration system as a tool in epidemiology. Eur. J. Epidemiol. 2014, 29, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Schmidt, S.A.; Sandegaard, J.L.; Ehrenstein, V.; Pedersen, L.; Sorensen, H.T. The Danish National Patient Registry: A review of content, data quality, and research potential. Clin. Epidemiol. 2015, 7, 449–490. [Google Scholar] [CrossRef] [PubMed]
- Nordic Health & Welfare Statistics. Available online: https://nhwstat.org/publications/ncsp-classification-surgical-procedures (accessed on 29 May 2025).
- Bliddal, M.; Broe, A.; Pottegard, A.; Olsen, J.; Langhoff-Roos, J. The Danish Medical Birth Register. Eur. J. Epidemiol. 2018, 33, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Swanson, K.A.; Phelps, H.M.; Chapman, W.C.; Glasgow, S.C.; Smith, R.K.; Joerger, S.; Utterson, E.C.; Shakhsheer, B.A. Surgery for chronic idiopathic constipation: Pediatric and adult patients–a systematic review. J. Gastrointest. Surg. 2024, 28, 170–177. [Google Scholar] [CrossRef] [PubMed]
- van Ginkel, R.; Reitsma, J.B.; Buller, H.A.; van Wijk, M.P.; Taminiau, J.A.; Benninga, M.A. Childhood constipation: Longitudinal follow-up beyond puberty. Gastroenterology 2003, 125, 357–363. [Google Scholar] [CrossRef] [PubMed]
- Bongers, M.E.; van Wijk, M.P.; Reitsma, J.B.; Benninga, M.A. Long-term prognosis for childhood constipation: Clinical outcomes in adulthood. Pediatrics 2010, 126, e156–e162. [Google Scholar] [CrossRef] [PubMed]
- Jønsson, I.M.; Siggaard, C.; Rittig, S.; Hagstrøm, S.; Djurhuus, J.C. Transabdominal ultrasound of rectum as a diagnostic tool in childhood constipation. J. Urol. 2008, 79, 1997–2002. [Google Scholar] [CrossRef] [PubMed]
| Variable | HD (N = 128) | Non-HD (N = 977) | Control (N = 11,077) | p-Value (HD vs. Non-HD) | p-Value (Non-HD vs. Control) |
|---|---|---|---|---|---|
| Age at biopsy (years) | 0.9 (2.0) | 2.8 (3.2) | 2.6 (3.2) | <0.001 | 0.108 |
| Follow-up (years) | 6.8 (3.9) | 5.6 (3.8) | 5.8 (3.9) | 0.002 | 0.150 |
| Gestational age at birth (days) | 272.9 (19.4) | 269.8 (22.5) | 277.5 (13.3) | 0.136 | <0.001 |
| Length at birth (cm) | 49.8 (9.5) | 49.1 (9.2) | 51.3 (5.6) | 0.430 | <0.001 |
| Mother’s BMI | 23.9 (3.9) | 24.9 (5.8) | 24.5 (7.4) | 0.069 | 0.124 |
| APGAR score (5 min) | 9.1 (0.64) | 9.1 (0.73) | 9.86 (0.61) | 0.932 | 0.002 |
| Equivalated family income (EUR) | 30,461 (17,850) | 28,984 (14,496) | 29,852 (18,089) | 0.293 | 0.146 |
| Mother’s smoking status | |||||
| Not active | 107 (83.6%) | 774 (79.2) | 9272 (83.7%) | ||
| Active | 21 (16.4%) | 203 (20.8%) | 1805 (16.3%) | 0.247 | <0.001 |
| Sex | |||||
| Female | 29 (22.7%) | 487 (49.8%) | 5172 (46.7%) | <0.001 | 0.058 |
| Male | 99 (77.3%) | 490 (50.2%) | 5905 (53.3%) |
| Procedure | HD (N = 128) | Non-HD (N = 977) | Control (N = 11,077) | p-Value (HD vs. Non-HD) | p-Value (Non-HD vs. Control) |
|---|---|---|---|---|---|
| Surgery before ID | 34 (26.6%) | 158 (16.2%) | 131 (1.2%) | 0.004 | <0.001 |
| Surgery after ID | 128 (100.0%) | 109 (11.2%) | 175 (1.6%) | <0.001 | <0.001 |
| Number of surgeries after ID | |||||
| 0 | 0 | 868 (88.9%) | 10,902 (98.4%) | <0.001 | <0.001 |
| 1–3 | 71 (56.8%) | 91 (9.3%) | 162 (1.5%) | ||
| 4–7 | 38 (30.4%) | 11 (1.1%) | 13 (0.1%) | ||
| 8+ | 16 (12.8%) | 5 (0.5%) | 0 (0.0%) | ||
| Endoscopy before ID | 5 (3.9%) | 61 (6.2%) | 33 (0.3%) | 0.294 | <0.001 |
| Endoscopy after ID | 52 (40.6%) | 92 (9.4%) | 57 (0.5%) | <0.001 | <0.001 |
| Any imaging before ID | 121 (94.5%) | 644 (65.9%) | 550 (5.0%) | <0.001 | <0.001 |
| Any imaging after ID | 78 (60.9%) | 362 (37.1%) | 862 (7.8%) | <0.001 | <0.001 |
| US before ID | 36 (28.1%) | 378 (38.7%) | 419 (3.8%) | 0.020 | <0.001 |
| US after ID | 42 (32.8%) | 277 (28.4%) | 743 (6.7%) | 0.295 | <0.001 |
| X-ray before ID | 116 (90.6%) | 503 (51.5%) | 179 (1.6%) | <0.001 | <0.001 |
| X-ray after ID | 69 (53.9%) | 187 (19.1%) | 142 (1.3%) | <0.001 | <0.001 |
| CT before ID | 5 (3.9%) | 20 (2.0%) | 12 (0.1%) | 0.183 | <0.001 |
| CT after ID | 8 (6.2%) | 17 (1.7%) | 29 (0.3%) | 0.001 | <0.001 |
| MRI before ID | 0 (0.0%) | 12 (1.2%) | 4 (0.0%) | 0.207 | <0.001 |
| MRI after ID | 4 (3.1%) | 21 (2.1%) | 22 (0.2%) | 0.485 | <0.001 |
| NSCP Code | Procedure | HD (N = 128) | Non-HD (N = 977) | Control (N = 11,077) |
|---|---|---|---|---|
| KJF | Small and large intestine | 99 (16.2%) | 91 (39.4%) | 7 (2.6%) |
| KJA | Abdominal wall | 28 (4.6%) | 48 (20.8%) | 159 (58.7%) |
| KJH | Anus | 326 (53.4%) | 33 (14.3%) | 13 (4.8%) |
| KJD | Stomach and duodenum | 1 (0.2%) | 26 (11.3%) | 19 (7.0%) |
| KJG | Rectum | 148 (24.3%) | 11 (4.8%) | 3 (1.1%) |
| KJC | Esophagus | - | 10 (4.3%) | 5 (1.9%) |
| KJE | Appendix | 71 (0.2%) | 7 (3.0%) | 59 (21.8%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bjørn, N.; Madsen, G.; Nielsen, R.G.; Sanberg, J.; Qvist, N.; Ellebæk, M.B. Increased Utilization of Abdominal Surgical Procedures, Endoscopy and Imaging After Negative Rectal Biopsies for Suspected Hirschsprung’s Disease: A Danish Nationwide Matched Cohort Study. Children 2025, 12, 1112. https://doi.org/10.3390/children12091112
Bjørn N, Madsen G, Nielsen RG, Sanberg J, Qvist N, Ellebæk MB. Increased Utilization of Abdominal Surgical Procedures, Endoscopy and Imaging After Negative Rectal Biopsies for Suspected Hirschsprung’s Disease: A Danish Nationwide Matched Cohort Study. Children. 2025; 12(9):1112. https://doi.org/10.3390/children12091112
Chicago/Turabian StyleBjørn, Niels, Gunvor Madsen, Rasmus Gaardskær Nielsen, Jonas Sanberg, Niels Qvist, and Mark Bremholm Ellebæk. 2025. "Increased Utilization of Abdominal Surgical Procedures, Endoscopy and Imaging After Negative Rectal Biopsies for Suspected Hirschsprung’s Disease: A Danish Nationwide Matched Cohort Study" Children 12, no. 9: 1112. https://doi.org/10.3390/children12091112
APA StyleBjørn, N., Madsen, G., Nielsen, R. G., Sanberg, J., Qvist, N., & Ellebæk, M. B. (2025). Increased Utilization of Abdominal Surgical Procedures, Endoscopy and Imaging After Negative Rectal Biopsies for Suspected Hirschsprung’s Disease: A Danish Nationwide Matched Cohort Study. Children, 12(9), 1112. https://doi.org/10.3390/children12091112






