Psychometric Properties of the Experience of Cognitive Intrusion of Pain (ECIP) Scale in Pediatric Chronic Pain
Abstract
1. Introduction
The Experience of Cognitive Intrusion of Pain
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Measures
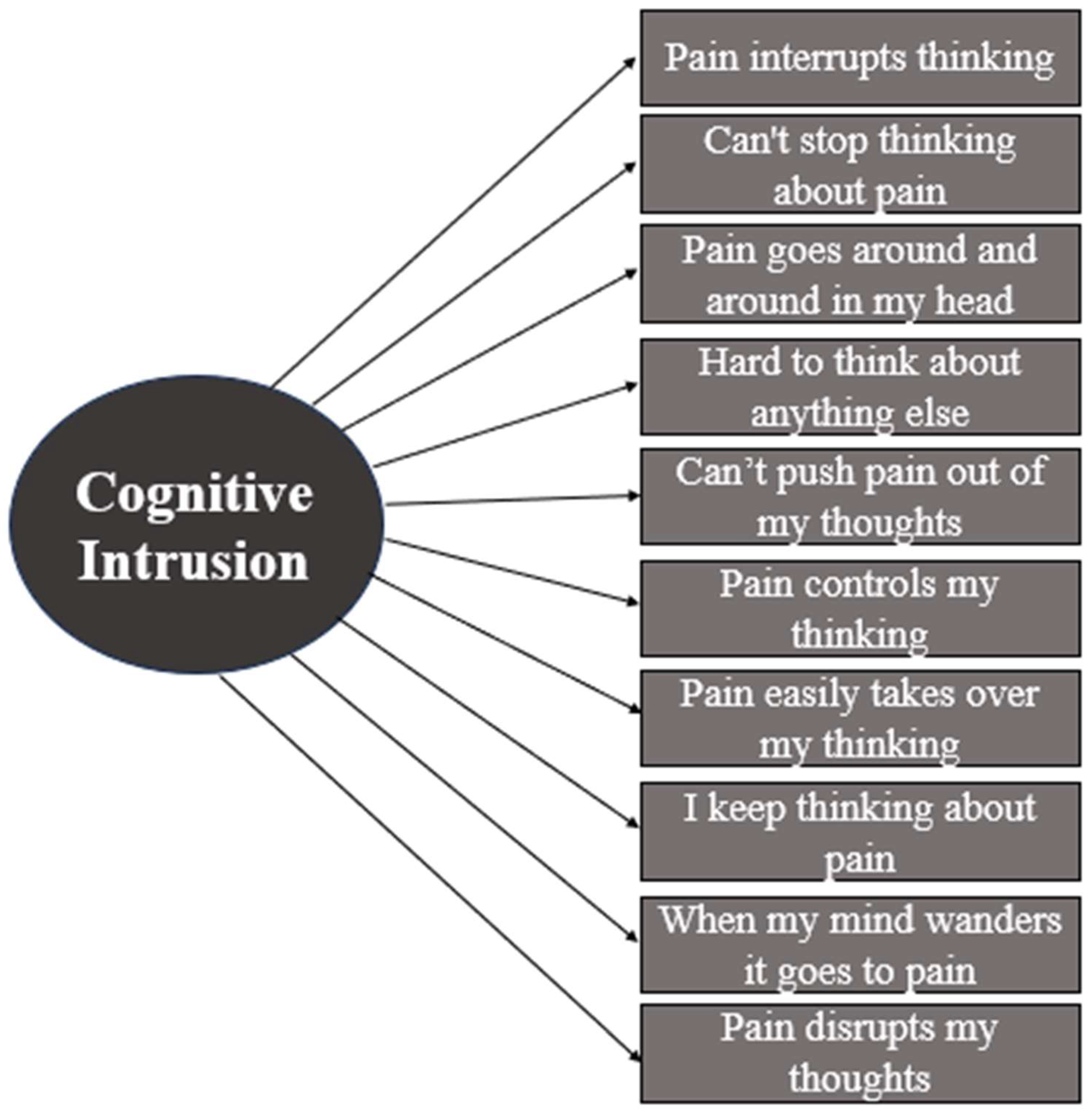
2.3.1. The Experience of Cognitive Intrusion of Pain (ECIP)
2.3.2. The Child Activity Limitations Interview (CALI-9)
2.3.3. The Patient-Reported Outcomes Measurement Information System Scale Anxiety (PROMIS—Pediatric Anxiety)
2.3.4. The Patient-Reported Outcomes Measurement Information System Scale Depression (PROMIS—Pediatric Depression)
2.3.5. Pain Frequency–Severity–Duration (PFSD) Scale
2.3.6. The Patient-Reported Outcomes Measurement Information System Pediatric Global Health Scale (PROMIS—Global Health-7)
2.3.7. Self-Management and Transition to Adulthood with Rx = Treatment (STARX)
2.4. Analytic Approach
3. Results
3.1. Sample Characteristics
3.2. Preliminary Analyses
3.3. ECIP Item Analysis
3.4. Internal Consistency Reliability
3.5. Confirmatory Factor Analysis
3.6. Convergent and Discriminant Validity
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ECIP | Experience of Cognitive Intrusion |
| CAT | Computerized adaptive testing |
| PROMIS | Patient-Reported Outcomes Measurement Information System Scale |
Appendix A

References
- Treede, R.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. A Classification of Chronic Pain for ICD-11. Pain 2015, 156, 1003–1007. [Google Scholar] [CrossRef] [PubMed]
- Chambers, C.T.; Dol, J.; Tutelman, P.R.; Langley, C.L.; Parker, J.A.; Cormier, B.T.; Macfarlane, G.J.; Jones, G.T.; Chapman, D.; Proudfoot, N.; et al. The Prevalence of Chronic Pain in Children and Adolescents: A Systematic Review Update and Meta-Analysis. J. Pain Res. 2024, 165, 2215–2234. [Google Scholar] [CrossRef] [PubMed]
- Gold, J.; Yetwin, A.; Mahrer, N.; Carson, M.; Griffin, A.; Palmer, S.; Joseph, M. Pediatric Chronic Pain and Health-Related Quality of Life. J. Pediatr. Nurs. 2009, 24, 141–150. [Google Scholar] [CrossRef] [PubMed]
- Jastrowski Mano, K.E.; Beckmann, E.; Fussner, L.; Kashikar-Zuck, S. Executive Functioning in Adolescents with Chronic Musculoskeletal Pain. Children 2020, 7, 273. [Google Scholar] [CrossRef]
- Liossi, C.; Howard, R. Pediatric Chronic Pain: Biopsychosocial Assessment and Formulation. J. Pediatr. 2016, 138, 1–14. [Google Scholar] [CrossRef]
- Puzzino, K.; Mindell, J. Sleep Disturbances in Pediatric Chronic Pain Patients: The Role of Cognitions. Transl. Issues Psychol. Sci. 2015, 1, 6–15. [Google Scholar] [CrossRef]
- Gibler, R.; Beckmann, E.; Lynch-Jordan, A.; Kashikar-Zuck, S.; Jastrowski Mano, K. Characterizing Social and Academic Aspects of School Anxiety in Pediatric Chronic Pain. Clin. J. Pain 2019, 35, 625–632. [Google Scholar] [CrossRef]
- Caes, L.; Dick, B.; Duncan, C.; Allan, J. The Cyclical Relation between Chronic Pain, Executive Functioning, Emotional Regulation and Self-Management. J. Pediatr. Psychol. 2020, 46, 286–292. [Google Scholar] [CrossRef]
- Gelonch, O.; Garolera, M.; Valls, J.; Rosselló, L.; Pifarré, J. Executive function in fibromyalgia: Comparing subjective and objective measures. Compr. Psychiatry 2016, 66, 113–122. [Google Scholar] [CrossRef]
- Gmuca, S.; Sonagra, M.; Xiao, R.; Mendoza, E.; Miller, K.S.; Thomas, N.H.; Young, J.F.; Weiss, P.F.; Sherry, D.D.; Gerber, J.S. Characterizing Neurocognitive Impairment in Juvenile Fibromyalgia Syndrome: Subjective and Objective Measures of Dyscognition. Front. Pediatr. 2022, 10, 848009. [Google Scholar] [CrossRef]
- Attridge, N.; Crombez, G.; Ryckeghem, D.; Keogh, E.; Eccleston, C. The Experience of Cognitive Intrusion of Pain: Scale Development and Validation. J. Pain Res. 2015, 156, 1978–1990. [Google Scholar] [CrossRef]
- Buhle, J.; Wager, T.D. Performance-Dependent Inhibition of Pain by an Executive Working Memory Task. Pain 2010, 149, 19–26. [Google Scholar] [CrossRef]
- Eccleston, C.; Crombez, G. Pain Demands Attention: A Cognitive-Affective Model of the Interruptive Function of Pain. Psychol. Bull. 1999, 125, 356–366. [Google Scholar] [CrossRef]
- Attridge, N.; Keogh, E.; Eccleston, C. The Effect of Pain on Task Switching: Pain Reduces Accuracy and Increases Reaction Times across Multiple Switching Paradigms. J. Pain Res. 2016, 157, 2179–2193. [Google Scholar] [CrossRef]
- Seward, J.; Rumble, D.; Attridge, N.; Stavrinos, D.; Moore, D.; Trost, Z. Cognitive Intrusion of Pain as a Mediator of the Relationship between Pain Catastrophizing and Driving Outcomes among Individuals with Chronic Low Back Pain. J. Pain Res. 2019, 20, S25. [Google Scholar] [CrossRef]
- Tabor, A.; Keogh, E.; Eccleston, C. Embodied Pain—Negotiating the Boundaries of Possible Action. J. Pain Res. 2017, 158, 1007–1011. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.J.; Keogh, E.; Eccleston, C. The Interruptive Effect of Pain on Attention. Q. J. Exp. Psychol. 2012, 65, 565–586. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.J.; Meints, S.; Lazaridou, A.; Johnson, D.; Franceschelli, O.; Cornelius, M.; Schreiber, K.; Edwards, R. The Effect of Induced and Chronic Pain on Attention. J. Pain Res. 2019, 20, 135–1361. [Google Scholar] [CrossRef]
- Kiliç, H.S.; Mercan, N. The Relationship Between Cognitive Intrusion of Pain, Fear of Surgery, and Comfort. Pain Manag. Nurs. 2024, 25, 467–473. [Google Scholar] [CrossRef]
- Talaei-Khoei, M.; Ogink, P.T.; Jha, R.; Ring, D.; Chen, N.; Vranceanu, A.-M. Cognitive intrusion of pain and catastrophic thinking independently explain interference of pain in the activities of daily living. J. Psychiatr. Res. 2017, 91, 156–163. [Google Scholar] [CrossRef]
- Adirim, T.; Meade, K.; Mistry, K. A New Era in Quality Measurement: The Development and Application of Quality Measures. Pediatrics 2017, 139, 1–11. [Google Scholar] [CrossRef]
- Mifflin, K.; Chorney, J.; Dick, B. Attention and working memory in female adolescents with chronic pain and pain-free female adolescents: A preliminary pilot study. Clin. J. Pain 2016, 32, 609–616. [Google Scholar] [CrossRef]
- Turner, K.M.P.; Wilcox, G.P.; Nordstokke, D.W.; Dick, B.P.; Schroeder, M.P.; Noel, M.P. Executive functioning in youth with and without chronic pain: A comparative analysis. Clin. J. Pain 2021, 37, 102–117. [Google Scholar] [CrossRef] [PubMed]
- Bhandari, R.P.; Feinstein, A.B.; Huestis, S.E.; Krane, E.J.; Dunn, A.L.; Cohen, L.L.; Kao, M.C.; Darnall, B.D.; Mackey, S.C. Pediatric-collaborative health outcomes information registry (Peds-CHOIR): A learning health system to guide pediatric pain research and treatment. Pain 2016, 157, 2033–2044. [Google Scholar] [CrossRef] [PubMed]
- Holley, A.; Zhou, C.; Wilson, A.; Hainsworth, K.; Palermo, T. The CALI-9: A Brief Measure for Assessing Activity Limitations in Children and Adolescents with Chronic Pain. J. Pain Res. 2018, 159, 48. [Google Scholar] [CrossRef] [PubMed]
- Cella, D.; Riley, W.; Stone, A.; Rothrock, N.; Reeve, B.; Yount, S.; Amtmann, D.; Bode, R.; Buysse, D.; Choi, S.; et al. The Patient-Reported Outcomes Measurement Information System (PROMIS) Developed and Tested Its First Wave of Adult Self-Reported Health Outcome Item Banks: 2005-2008. J. Clin. Epidemiol. 2010, 63, 1179–1194. [Google Scholar] [CrossRef]
- Pilkonis, P.; Choi, S.; Reise, S.; Stover, A.; Riley, W.; Cella, D. Item Banks for Measuring Emotional Distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, Anxiety, and Anger. Assessment 2011, 18, 263–283. [Google Scholar] [CrossRef]
- Li, R.; Gibler, R.; Rheel, E.; Slack, K.; Palermo, T. Recommendations for Patient-Reported Outcomes Measurement Information System Pediatric Measures in Youth with Chronic Pain: A COnsensus-Based Standards for the Selection of Health Measurement INstruments Systematic Review of Measurement Properties. J. Pain Res. 2024, 165, 258–295. [Google Scholar] [CrossRef]
- Nolte, S.; Coon, C.; Hudgens, S.; Verdam, M. Psychometric Evaluation of the PROMIS® Depression Item Bank: An Illustration of Classical Test Theory Methods. J. Patient-Rep. Outcomes 2019, 3, 1–10. [Google Scholar] [CrossRef]
- Salamon, K.S.; Davies, W.H.; Fuentes, M.R.; Weisman, S.J.; Hainsworth, K.R. The Pain Frequency-Severity-Duration Scale as a Measure of Pain: Preliminary Validation in a Pediatric Chronic Pain Sample. Pain Res. Treat. 2014, 2014, 1–6. [Google Scholar] [CrossRef]
- Forrest, C.; Bevans, K.; Pratiwadi, R.; Moon, J.; Teneralli, R.; Minton, J.; Tucker, C. Development of the PROMIS ® Pediatric Global Health (PGH-7) Measure. Qual. Life Res. 2014, 23, 1221–1231. [Google Scholar] [CrossRef]
- Luijten, M.; Haverman, L.; Litsenburg, R.; Roorda, L.; Grootenhuis, M.; Terwee, C. Advances in Measuring Pediatric Overall Health: The PROMIS® Pediatric Global Health Scale (PGH-7). Eur. J. Pediatr. 2022, 181, 2117–2125. [Google Scholar] [CrossRef]
- Cohen, S.; Hooper, S.; Javalkar, K.; Haberman, C.; Fenton, N.; Lai, H.; Mahan, J.; Massengill, S.; Kelly, M.; Cantú, G.; et al. Self-Management and Transition Readiness Assessment: Concurrent, Predictive and Discriminant Validation of the STARx Questionnaire. J. Pediatr. Nurs. 2015, 30, 668–676. [Google Scholar] [CrossRef] [PubMed]
- Ferris, M.; Cohen, S.; Haberman, C.; Javalkar, K.; Massengill, S.; Mahan, J.D.; Kim, S.; Bickford, K.; Cantu, G.; Medeiros, M.; et al. Self-Management and Transition Readiness Assessment: Development, Reliability, and Factor Structure of the STARx Questionnaire. J. Pediatr. Nurs. 2015, 30, 691–699. [Google Scholar] [CrossRef] [PubMed]
- Kim, H. Statistical Notes for Clinical Researchers: Assessing Normal Distribution (2) Using Skewness and Kurtosis. Restor. Dent. Endod. 2013, 38, 52–54. [Google Scholar] [CrossRef] [PubMed]
- Seng, E.K.; Klepper, J.E. Development of the Cogniphobia Scale for Headache Disorders (CS-HD): A pilot study. Psychol. Assess. 2017, 29, 1296–1301. [Google Scholar] [CrossRef]
- King, S.; Chambers, C.; Huguet, A.; MacNevin, R.; McGrath, P.; Parker, L.; MacDonald, A. The Epidemiology of Chronic Pain in Children and Adolescents Revisited: A Systematic Review. J. Pain Res. 2011, 152, 2729–2738. [Google Scholar] [CrossRef]
- Ebesutani, C.; Bernstein, A.; Martinez, J.I.; Chorpita, B.F.; Weisz, J. The Youth Self Report: Applicability and Validity across Younger and Older Youths. J. Clin. Child Adolesc. Psychol. 2011, 40, 338–346. [Google Scholar] [CrossRef]
- Sweeting, H.; Hunt, K. Adolescent Socio-Economic and School-Based Social Status, Health and Well-Being. Soc. Sci. Med. 2014, 121, 39–47. [Google Scholar] [CrossRef]
- Coakley, R.; Wihak, T. Evidence-Based Psychological Interventions for the Management of Pediatric Chronic Pain: New Directions in Research and Clinical Practice. Children 2017, 4, 9. [Google Scholar] [CrossRef]
- Haroz, E.; Kane, J.; Nguyen, A.; Bass, J.; Murray, L.; Bolton, P. When Less Is More: Reducing Redundancy in Mental Health and Psychosocial Instruments Using Item Response Theory. Glob. Ment. Health 2020, 7, 3. [Google Scholar] [CrossRef]
| M | SD | |
| Age | 14.25 | 2.15 |
| n | (%) | |
| Sex * | ||
| Female | 141 | 77.5 |
| Male | 41 | 22.5 |
| Race | ||
| White/Caucasian | 149 | 81.9 |
| Black/African American | 23 | 12.6 |
| Asian American/Pacific Islander | 3 | 1.6 |
| Multiracial | 2 | 1.1 |
| Preferred Not to Answer | 5 | 2.7 |
| Ethnicity | ||
| Hispanic/Latine/Latino | 20 | 10.9 |
| Not Hispanic/Latine/Latino | 160 | 87.9 |
| Preferred Not to Answer | 2 | 1.1 |
| Primary Pain Location | n | % |
| Head | 117 | 65 |
| Chest/Neck/Back | 10 | 5.5 |
| Extremities | 10 | 5.5 |
| Abdomen | 15 | 8.3 |
| Musculoskeletal | 19 | 10.5 |
| Other | 9 | 5 |
| M | SD | Minimum–Maximum | |
| Full Sample | 30.64 | 14.60 | 1–60 |
| Age (in years) | |||
| 11 | 33.84 | 16.67 | 2–60 |
| 12 | 27.52 | 14.75 | 1–53 |
| 13 | 31.57 | 13.57 | 2–57 |
| 14 | 31.60 | 17.36 | 6–59 |
| 15 | 32.16 | 14.43 | 4–60 |
| 16 | 28.07 | 14.32 | 1–51 |
| 17 | 30.42 | 14.28 | 3–50 |
| 18 | 28.71 | 7.78 | 18–38 |
| Sex | |||
| Female | 30.65 | 15.05 | 1–60 |
| Male | 30.53 | 13.12 | 1–59 |
| Race | |||
| White/Caucasian | 30.25 | 14.55 | 1–60 |
| Black/African American | 34.91 | 14.86 | 7–60 |
| Asian American/Pacific Islander | 19.00 | 13.75 | 7–34 |
| Multiracial | 26.50 | 13.44 | 17–36 |
| Preferred Not to Answer | 30.80 | 15.51 | 9–46 |
| Ethnicity | |||
| Hispanic/Latine/Latino | 23.50 | 15.17 | 1–56 |
| Not Hispanic/Latine/Latino | 31.33 | 14.26 | 1–60 |
| Preferred Not to Answer | 46.0 | 18.38 | 33–59 |
| Primary Pain Location | |||
| Head | 30.68 | 13.62 | 1–60 |
| Chest/Neck/Back | 26.60 | 16.64 | 2–53 |
| Extremities | 30.50 | 19.93 | 1–60 |
| Abdomen | 30.33 | 18.42 | 4–59 |
| Musculoskeletal | 26.95 | 12.66 | 4–46 |
| Other | 39.33 | 14.47 | 7–56 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Heard, C.; Hainsworth, K.R.; Jastrowski Mano, K.E. Psychometric Properties of the Experience of Cognitive Intrusion of Pain (ECIP) Scale in Pediatric Chronic Pain. Children 2025, 12, 1069. https://doi.org/10.3390/children12081069
Heard C, Hainsworth KR, Jastrowski Mano KE. Psychometric Properties of the Experience of Cognitive Intrusion of Pain (ECIP) Scale in Pediatric Chronic Pain. Children. 2025; 12(8):1069. https://doi.org/10.3390/children12081069
Chicago/Turabian StyleHeard, Cherish, Keri R. Hainsworth, and Kristen E. Jastrowski Mano. 2025. "Psychometric Properties of the Experience of Cognitive Intrusion of Pain (ECIP) Scale in Pediatric Chronic Pain" Children 12, no. 8: 1069. https://doi.org/10.3390/children12081069
APA StyleHeard, C., Hainsworth, K. R., & Jastrowski Mano, K. E. (2025). Psychometric Properties of the Experience of Cognitive Intrusion of Pain (ECIP) Scale in Pediatric Chronic Pain. Children, 12(8), 1069. https://doi.org/10.3390/children12081069





