Primary and Secondary Prophylaxis of Gastrointestinal Bleeding in Children with Portal Hypertension: A Multicenter National Study by SIGENP
Abstract
1. Introduction
2. Materials and Methods
3. Results
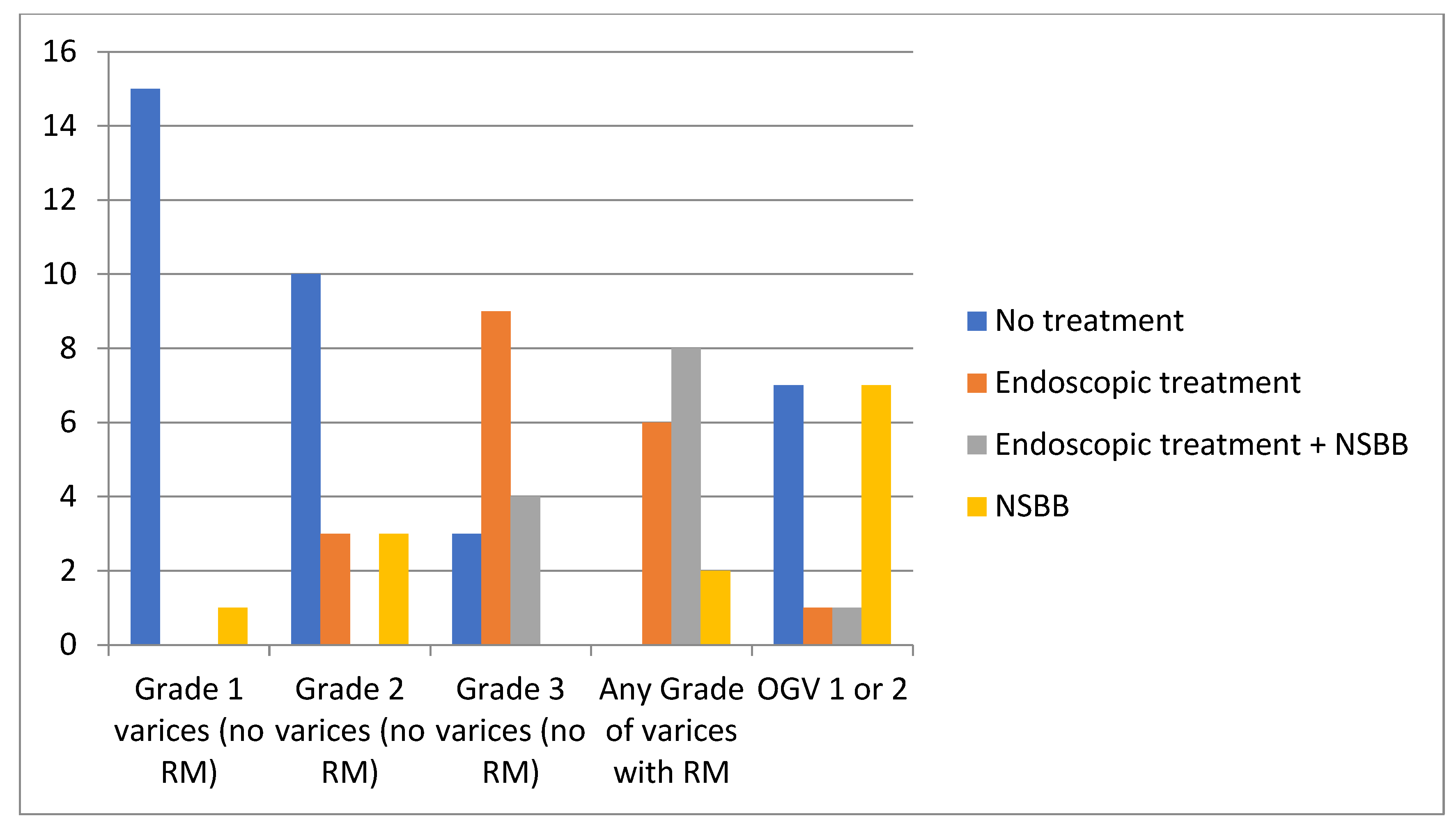
- (a)
- Endoscopy and NSBBs in 8/16 centers (50%);
- (b)
- Endoscopy alone in 6/16 (38%);
- (c)
- NSBBs alone in 2/16 (12%).
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| GI | Gastrointestinal |
| NSBBs | Non-selective beta-blockers |
| OGV | Esophagogastric varices |
| PH | Portal hypertension |
| RM | Red marks |
| TIPS | Transjugular Intrahepatic Portosystemic Shunt |
References
- Di Giorgio, A.; Nicastro, E.; Dalla Rosa, D.; Nebbia, G.; Sonzogni, A.; D’Antiga, L. Transplant-free Survival in Chronic Liver Disease Presenting as Acute Liver Failure in Childhood. Transplantation 2019, 103, 544–551. [Google Scholar] [CrossRef] [PubMed]
- Di Giorgio, A.; De Angelis, P.; Cheli, M.; Vajro, P.; Iorio, R.; Cananzi, M.; Riva, S.; Maggiore, G.; Indolfi, G.; Calvo, P.L.; et al. Etiology, presenting features and outcome of children with non-cirrhotic portal vein thrombosis: A multicentre national study. Dig. Liver Dis. 2019, 51, 1179–1184. [Google Scholar] [CrossRef] [PubMed]
- Giouleme, O.; Theocharidou, E. Management of portal hypertension in children with portal vein thrombosis. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 419–425. [Google Scholar] [CrossRef] [PubMed]
- Grammatikopoulos, T.; McKiernan, P.J.; Dhawan, A. Portal hypertension and its management in children. Arch. Dis. Child. 2018, 103, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Luoto, T.T.; Koivusalo, A.I.; Pakarinen, M.P. Long-term Outcomes and Health Perceptions in Pediatric-onset Portal Hypertension Complicated by Varices. J. Pediatr. Gastroenterol. Nutr. 2020, 70, 628–634. [Google Scholar] [CrossRef] [PubMed]
- Luoto, T.T.; Pakarinen, M.P. Evolving management of paediatric portal hypertension. Arch. Dis. Child. 2021, 106, 939–940. [Google Scholar] [CrossRef] [PubMed]
- D’Antiga, L.; Betalli, P.; De Angelis, P.; Davenport, M.; Di Giorgio, A.; McKiernan, P.J.; McLin, V.; Ravelli, P.; Durmaz, O.; Talbotec, C.; et al. Interobserver Agreement on Endoscopic Classification of Oesophageal Varices in Children. J. Pediatr. Gastroenterol. Nutr. 2015, 61, 176–181. [Google Scholar] [CrossRef] [PubMed]
- Shneider, B.L.; de Ville de Goyet, J.; Leung, D.H.; Srivastava, A.; Ling, S.C.; Duche, M.; McKiernan, P.; Superina, R.; Squires, R.H.; Bosch, J.; et al. Primary prophylaxis of variceal bleeding in children and the role of MesoRex Bypass: Summary of the Baveno VI Pediatric Satellite Symposium. Hepatology 2016, 63, 1368–1380. [Google Scholar] [CrossRef] [PubMed]
- Duche, M.; Ducot, B.; Ackermann, O.; Guerin, F.; Jacquemin, E.; Bernard, O. Portal hypertension in children: High-risk varices, primary prophylaxis and consequences of bleeding. J. Hepatol. 2017, 66, 320–327. [Google Scholar] [CrossRef] [PubMed]
- Novak, I.; Bass, L.M. Gastrointestinal Bleeding in Children: Current Management, Controversies, and Advances. Gastrointest. Endosc. Clin. 2023, 33, 401–421. [Google Scholar] [CrossRef] [PubMed]
- Zargar, S.A.; Javid, G.; Khan, B.A.; Yattoo, G.N.; Shah, A.H.; Gulzar, G.M.; Singh, J.; Rehman, B.U.; Din, Z. Endoscopic ligation compared with sclerotherapy for bleeding esophageal varices in children with extrahepatic portal venous obstruction. Hepatology 2002, 36, 666–672. [Google Scholar] [CrossRef] [PubMed]
- Sutton, H.; Dhawan, A.; Grammatikopoulos, T. Non-invasive Markers of Portal Hypertension: Appraisal of Adult Experience and Potential Utilisation in Children. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 559–569. [Google Scholar] [CrossRef] [PubMed]
- Hasan, M.I.; Rukunuzzaman, M.; Nurullah, M.; Sultana, F. Clinical and Laboratory Predictors of Esophageal Varices in Children with Chronic Liver Disease. Mymensingh Med. J. 2017, 26, 341–350. [Google Scholar] [PubMed]
- Poddar, U.; Samanta, A.; Sarma, M.S.; Kumar, B.; Lal, R.; Srivastava, A.; Upadhyaya, V.D.; Yachha, S.K.; Mandelia, A. How to suspect the presence of high-risk esophageal varices and when to start endoscopic surveillance in children with biliary atresia? J. Gastroenterol. Hepatol. 2023, 38, 1610–1617. [Google Scholar] [CrossRef] [PubMed]
- Ravindranath, A.; Yachha, S.K. An Approach to Investigations of Chronic Liver Disease. Indian. J. Pediatr. 2024, 91, 262–269. [Google Scholar] [CrossRef] [PubMed]
- Pinto, R.B.; Schneider, A.C.; da Silveira, T.R. Cirrhosis in children and adolescents: An overview. World J. Hepatol. 2015, 7, 392–405. [Google Scholar] [CrossRef] [PubMed]
- de Franchis, R.; Baveno, V.I.F. Expanding consensus in portal hypertension: Report of the Baveno VI Consensus Workshop: Stratifying risk and individualizing care for portal hypertension. J. Hepatol. 2015, 63, 743–752. [Google Scholar] [CrossRef] [PubMed]
- Shneider, B.L.; Bosch, J.; de Franchis, R.; Emre, S.H.; Groszmann, R.J.; Ling, S.C.; Lorenz, J.M.; Squires, R.H.; Superina, R.A.; Thompson, A.E.; et al. Portal hypertension in children: Expert pediatric opinion on the report of the Baveno v Consensus Workshop on Methodology of Diagnosis and Therapy in Portal Hypertension. Pediatr. Transplant. 2012, 16, 426–437. [Google Scholar] [CrossRef] [PubMed]
- de Franchis, R.; Bosch, J.; Garcia-Tsao, G.; Reiberger, T.; Ripoll, C.; Baveno, V.I.I.F. Baveno VII—Renewing consensus in portal hypertension. J. Hepatol. 2022, 76, 959–974. [Google Scholar] [CrossRef] [PubMed]
- Wani, Z.A.; Bhat, R.A.; Bhadoria, A.S.; Maiwall, R.; Choudhury, A. Gastric varices: Classification, endoscopic and ultrasonographic management. J. Res. Med. Sci. 2015, 20, 1200–1207. [Google Scholar] [CrossRef] [PubMed]
- Gana, J.C.; Turner, D.; Mieli-Vergani, G.; Davenport, M.; Miloh, T.; Avitzur, Y.; Yap, J.; Morinville, V.; Brill, H.; Ling, S.C. A clinical prediction rule and platelet count predict esophageal varices in children. Gastroenterology 2011, 141, 2009–2016. [Google Scholar] [CrossRef] [PubMed]
- Segna, D.; Mendoza, Y.P.; Lange, N.F.; Rodrigues, S.G.; Berzigotti, A. Non-invasive tools for compensated advanced chronic liver disease and portal hypertension after Baveno VII—An update. Dig. Liver Dis. 2023, 55, 326–335. [Google Scholar] [CrossRef] [PubMed]
- Angelico, R.; Pietrobattista, A.; Candusso, M.; Tomarchio, S.; Pellicciaro, M.; Liccardo, D.; Basso, M.S.; Grimaldi, C.; Saffioti, M.C.; Torroni, F.; et al. Primary Prophylaxis for Gastrointestinal Bleeding in Children With Biliary Atresia and Portal Hypertension Candidates for Liver Transplantation: A Single-Center Experience. Transplant. Proc. 2019, 51, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Ling, S.C.; Walters, T.; McKiernan, P.J.; Schwarz, K.B.; Garcia-Tsao, G.; Shneider, B.L. Primary prophylaxis of variceal hemorrhage in children with portal hypertension: A framework for future research. J. Pediatr. Gastroenterol. Nutr. 2011, 52, 254–261. [Google Scholar] [CrossRef] [PubMed]
- Jeanniard-Malet, O.; Duche, M.; Fabre, A. Survey on Clinical Practice of Primary Prophylaxis in Portal Hypertension in Children. J. Pediatr. Gastroenterol. Nutr. 2017, 64, 524–527. [Google Scholar] [CrossRef] [PubMed]
- Gana, J.C.; Valentino, P.L.; Morinville, V.; O’Connor, C.; Ling, S.C. Variation in care for children with esophageal varices: A study of physicians’, patients’, and families’ approaches and attitudes. J. Pediatr. Gastroenterol. Nutr. 2011, 52, 751–755. [Google Scholar] [CrossRef] [PubMed]
- Bozic, M.A.; Puri, K.; Molleston, J.P. Screening and Prophylaxis for Varices in Children with Liver Disease. Curr. Gastroenterol. Rep. 2015, 17, 27. [Google Scholar] [CrossRef] [PubMed]
- Cifuentes, L.I.; Gattini, D.; Torres-Robles, R.; Gana, J.C. Band ligation versus sham or no intervention for primary prophylaxis of oesophageal variceal bleeding in children and adolescents with chronic liver disease or portal vein thrombosis. Cochrane Database Syst. Rev. 2021, 1, CD011561. [Google Scholar] [CrossRef] [PubMed]
- Samanta, T.; Purkait, R.; Sarkar, M.; Misra, A.; Ganguly, S. Effectiveness of beta blockers in primary prophylaxis of variceal bleeding in children with portal hypertension. Trop. Gastroenterol. 2011, 32, 299–303. [Google Scholar] [PubMed]
- Li, T.; Ke, W.; Sun, P.; Chen, X.; Belgaumkar, A.; Huang, Y.; Xian, W.; Li, J.; Zheng, Q. Carvedilol for portal hypertension in cirrhosis: Systematic review with meta-analysis. BMJ Open 2016, 6, e010902. [Google Scholar] [CrossRef] [PubMed]
- Di Giorgio, A.; D’Adda, A.; Marseglia, A.; Sonzogni, A.; Licini, L.; Nicastro, E.; D’Antiga, L. Biliary features in liver histology of children with autoimmune liver disease. Hepatol. Int. 2019, 13, 510–518. [Google Scholar] [CrossRef] [PubMed]
- Deniz, S.; Schinner, R.; Monroe, E.J.; Horslen, S.; Srinivasa, R.N.; Lv, Y.; Fan, D.; Han, G.; Sarma, M.S.; Srivastava, A.; et al. Outcome of Children with Transjugular Intrahepatic Portosystemic Shunt: A Meta-Analysis of Individual Patient Data. Cardiovasc. Intervent Radiol. 2023, 46, 1203–1213. [Google Scholar] [CrossRef] [PubMed]
- Raissi, D.; Brahmbhatt, S.; Yu, Q.; Jiang, L.; Liu, C. Transjugular intrahepatic portosystemic shunt for pediatric portal hypertension: A meta-analysis. J. Clin. Imaging Sci. 2023, 13, 18. [Google Scholar] [CrossRef] [PubMed]
- Di Giorgio, A.; Nicastro, E.; Agazzi, R.; Colusso, M.; D’Antiga, L. Long-term Outcome of Transjugular Intrahepatic Portosystemic Shunt in Children With Portal Hypertension. J. Pediatr. Gastroenterol. Nutr. 2020, 70, 615–622. [Google Scholar] [CrossRef] [PubMed]
| (A) | |
| Acid suppression | 100% |
| Octreotide | 94% |
| Occlusion tube (e.g., Sengstaken–Blakemore) | 38% |
| Intravenous antibiotics | 63% |
| Endoscopy | 100% |
| (B) | |
| Treatment options after the first episode of variceal hemorrhage | |
| NSBBs | 87% |
| Endoscopic treatment (sclerotherapy or band ligation) When Endoscopy and NSBB fail to control variceal hemorrhage | 100% |
| TIPS | 94% |
| Surgical Shunt | 63% |
| Transplantation | 50% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sansotta, N.; De Angelis, P.; Alberti, D.; Di Dato, F.; Arrigo, S.; Bramuzzo, M.; Calcaterra, B.; Cananzi, M.; Cheli, M.; Chiaro, A.; et al. Primary and Secondary Prophylaxis of Gastrointestinal Bleeding in Children with Portal Hypertension: A Multicenter National Study by SIGENP. Children 2025, 12, 940. https://doi.org/10.3390/children12070940
Sansotta N, De Angelis P, Alberti D, Di Dato F, Arrigo S, Bramuzzo M, Calcaterra B, Cananzi M, Cheli M, Chiaro A, et al. Primary and Secondary Prophylaxis of Gastrointestinal Bleeding in Children with Portal Hypertension: A Multicenter National Study by SIGENP. Children. 2025; 12(7):940. https://doi.org/10.3390/children12070940
Chicago/Turabian StyleSansotta, Naire, Paola De Angelis, Daniele Alberti, Fabiola Di Dato, Serena Arrigo, Matteo Bramuzzo, Benedetta Calcaterra, Mara Cananzi, Maurizio Cheli, Andrea Chiaro, and et al. 2025. "Primary and Secondary Prophylaxis of Gastrointestinal Bleeding in Children with Portal Hypertension: A Multicenter National Study by SIGENP" Children 12, no. 7: 940. https://doi.org/10.3390/children12070940
APA StyleSansotta, N., De Angelis, P., Alberti, D., Di Dato, F., Arrigo, S., Bramuzzo, M., Calcaterra, B., Cananzi, M., Cheli, M., Chiaro, A., Cirillo, F., Colusso, M., Di Leo, G., Faraci, S., Gaio, P., Indolfi, G., Iuliano, S., Liccardo, D., Marseglia, A., ... Di Giorgio, A. (2025). Primary and Secondary Prophylaxis of Gastrointestinal Bleeding in Children with Portal Hypertension: A Multicenter National Study by SIGENP. Children, 12(7), 940. https://doi.org/10.3390/children12070940






