Cumulative Transcutaneous Spinal Stimulation with Locomotor Training Safely Improves Trunk Control in Children with Spinal Cord Injury: Pilot Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
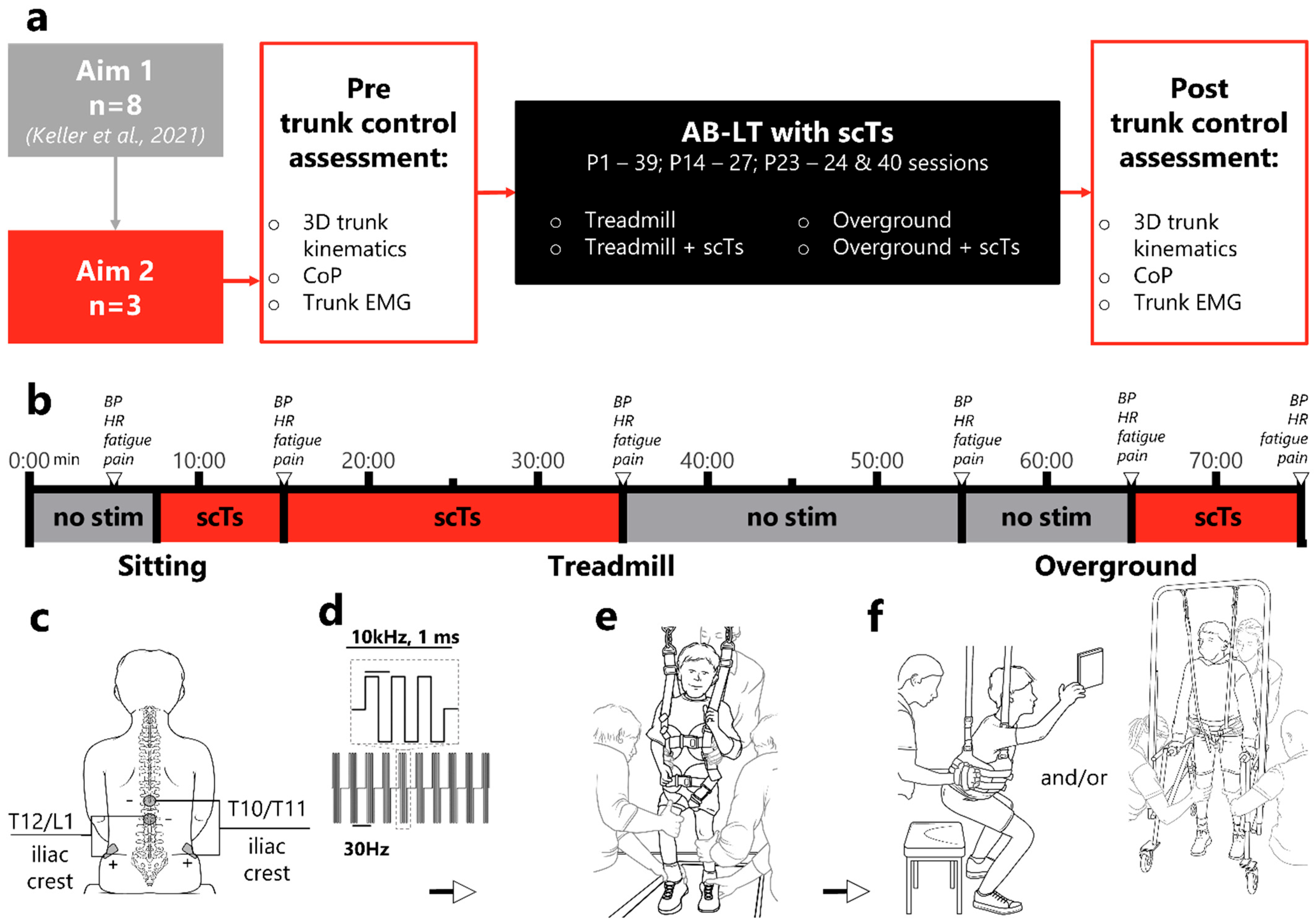
2.2. Experimental Design
2.2.1. Activity-Based Locomotor Training (AB-LT)
2.2.2. Transcutaneous Spinal Cord Stimulation (scTS)
2.2.3. Risk Estimation and Hemodynamic Monitoring
2.2.4. Trunk Control Assessment
- Quiet sitting with arms crossed over the chest for 10 s;
- Leaning forward, backward, right, and left with arms crossed over the chest as far as possible, without falling;
- Raising the right arm rapidly as a self-perturbing task.
- Quiet sitting. The patient’s hands lay on his knees without propping on them and asked to maintain sitting balance as long as he can;
- Sit upright as best as possible, actively attempting to straighten his trunk without support from trainers for 5 s.
2.2.5. 3D Trunk Kinematics
2.2.6. Center of Pressure (CoP)
2.2.7. Electromyography (EMG)
2.3. Statistical Analysis
3. Results
3.1. Adverse Effects
3.2. Fatigue & Pain Levels
3.3. Blood Pressure and Heart Rate
3.4. Trunk Control
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Anderson, K.D. Targeting recovery: Priorities of the spinal cord-injured population. J. Neurotrauma 2004, 21, 1371–1383. [Google Scholar] [CrossRef] [PubMed]
- Mehta, S.; Betz, R.; Mulcahey, M.J.; McDonald, C.; Vogel, L. Effect of Bracing on Paralytic Scoliosis Secondary to Spinal Cord Injury. J. Spinal Cord Med. 2004, 27, S88–S92. [Google Scholar] [CrossRef] [PubMed]
- Mulcahey, M.J.; Gaughan, J.P.; Betz, R.R.; Samdani, A.F.; Barakat, N.; Hunter, L.N. Neuromuscular scoliosis in children with spinal cord injury. Top. Spinal Cord Inj. Rehabil. 2013, 19, 96–103. [Google Scholar] [CrossRef]
- Singh, G.; Lucas, K.; Keller, A.; Martin, R.; Behrman, A.; Vissarionov, S.; Gerasimenko, Y.P. Transcutaneous Spinal Stimulation From Adults to Children: A Review. Top. Spinal Cord Inj. Rehabil. 2023, 29, 16–32. [Google Scholar] [CrossRef]
- Singh, G.; Keller, A.; Lucas, K.; Borders, C.; Stout, D.; King, M.; Parikh, P.; Stepp, N.; Ugiliweneza, B.; D’Amico, J.M.; et al. Safety and Feasibility of Cervical and Thoracic Transcutaneous Spinal Cord Stimulation to Improve Hand Motor Function in Children with Chronic Spinal Cord Injury. Neuromodulation 2024, 27, 661–671. [Google Scholar] [CrossRef] [PubMed]
- Neighbors, E.; Brunn, L.; Casamento-Moran, A.; Martin, R. Transcutaneous Spinal Cord Stimulation Enables Recovery of Walking in Children with Acute Flaccid Myelitis. Children 2024, 11, 1116. [Google Scholar] [CrossRef]
- Solopova, I.A.; Sukhotina, I.A.; Zhvansky, D.S.; Ikoeva, G.A.; Vissarionov, S.V.; Baindurashvili, A.G.; Edgerton, V.R.; Gerasimenko, Y.P.; Moshonkina, T.R. Effects of spinal cord stimulation on motor functions in children with cerebral palsy. Neurosci. Lett. 2017, 639, 192–198. [Google Scholar] [CrossRef]
- Atkinson, D.; Barta, K.; Bizama, F.; Anderson, H.; Brose, S.; Sayenko, D.G. Transcutaneous Spinal Stimulation Combined with Locomotor Training Improves Functional Outcomes in a Child with Cerebral Palsy: A Case Study. Children 2024, 11, 1439. [Google Scholar] [CrossRef]
- Shrivastav, S.R.; DeVol, C.R.; Landrum, V.M.; Bjornson, K.F.; Roge, D.; Steele, K.M.; Moritz, C.T. Transcutaneous Spinal Stimulation and Short-Burst Interval Treadmill Training in Children With Cerebral Palsy: A Pilot Study. IEEE Trans. Biomed. Eng. 2025, 72, 1775–1784. [Google Scholar] [CrossRef]
- Allen, K.J.; Leslie, S.W. Autonomic Dysreflexia; StatPearls: Treasure Island, FL, USA, 2025. [Google Scholar]
- Veith, D.D.; Asp, A.J.; Gill, M.L.; Fernandez, K.A.; Mills, C.J.; Linde, M.B.; Jahanian, O.; Beck, L.A.; Zhao, K.D.; Grahn, P.J.; et al. Prevalence of autonomic dysreflexia during spinal cord stimulation after spinal cord injury. J. Neurophysiol. 2024, 132, 1371–1375. [Google Scholar] [CrossRef]
- Keller, A.; Singh, G.; Sommerfeld, J.H.; King, M.; Parikh, P.; Ugiliweneza, B.; D’Amico, J.; Gerasimenko, Y.; Behrman, A.L. Noninvasive spinal stimulation safely enables upright posture in children with spinal cord injury. Nat. Commun. 2021, 12, 5850. [Google Scholar] [CrossRef]
- Martin, R. Utility and Feasibility of Transcutaneous Spinal Cord Stimulation for Patients With Incomplete SCI in Therapeutic Settings: A Review of Topic. Front. Rehabil. Sci. 2021, 2, 724003. [Google Scholar] [CrossRef]
- Gerasimenko, Y.; Gorodnichev, R.; Moshonkina, T.; Sayenko, D.; Gad, P.; Reggie Edgerton, V. Transcutaneous electrical spinal-cord stimulation in humans. Ann. Phys. Rehabil. Med. 2015, 58, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Hofstoetter, U.S.; Minassian, K. Transcutaneous Spinal Cord Stimulation: Advances in an Emerging Non-Invasive Strategy for Neuromodulation. J. Clin. Med. 2022, 11, 3836. [Google Scholar] [CrossRef]
- Rath, M.; Vette, A.H.; Ramasubramaniam, S.; Li, K.; Burdick, J.; Edgerton, V.R.; Gerasimenko, Y.P.; Sayenko, D.G. Trunk Stability Enabled by Noninvasive Spinal Electrical Stimulation after Spinal Cord Injury. J. Neurotrauma 2018, 35, 2540–2553. [Google Scholar] [CrossRef]
- Edgerton, V.R.; Gad, P. Spinal automaticity of movement control and its role in recovering function after spinal injury. Expert Rev. Neurother. 2022, 22, 655–667. [Google Scholar] [CrossRef] [PubMed]
- Gad, P.; Choe, J.; Shah, P.; Garcia-Alias, G.; Rath, M.; Gerasimenko, Y.; Zhong, H.; Roy, R.R.; Edgerton, V.R. Sub-threshold spinal cord stimulation facilitates spontaneous motor activity in spinal rats. J. Neuroeng. Rehabil. 2013, 10, 108. [Google Scholar] [CrossRef] [PubMed]
- Harkema, S.; Behrman, A.; Barbeau, H. Locomotor Training: Principles and Practice, 1st ed.; Oxford University Press: Oxford, UK, 2011. [Google Scholar]
- Roy, R.R.; Harkema, S.J.; Edgerton, V.R. Basic concepts of activity-based interventions for improved recovery of motor function after spinal cord injury. Arch. Phys. Med. Rehabil. 2012, 93, 1487–1497. [Google Scholar] [CrossRef]
- Behrman, A.L.; Nair, P.M.; Bowden, M.G.; Dauser, R.C.; Herget, B.R.; Martin, J.B.; Phadke, C.P.; Reier, P.J.; Senesac, C.R.; Thompson, F.J.; et al. Locomotor training restores walking in a nonambulatory child with chronic, severe, incomplete cervical spinal cord injury. Phys. Ther. 2008, 88, 580–590. [Google Scholar] [CrossRef]
- Argetsinger, L.C.; Trimble, S.A.; Roberts, M.T.; Thompson, J.E.; Ugiliweneza, B.; Behrman, A.L. Sensitivity to change and responsiveness of the Segmental Assessment of Trunk Control (SATCo) in children with spinal cord injury. Dev. Neurorehabilit. 2019, 22, 260–271. [Google Scholar] [CrossRef]
- Argetsinger, L.C.; Singh, G.; Bickel, S.G.; Calvery, M.L.; Behrman, A.L. Spinal cord injury in infancy: Activity-based therapy impact on health, function, and quality of life in chronic injury. Spinal Cord Ser. Cases 2020, 6, 13. [Google Scholar] [CrossRef] [PubMed]
- Goode-Roberts, M.; Noonan, K.; Stout, D.; Calvery, M.; Brothers, K.; Doonan, N.W.; Behrman, A.L. Case Report: Capitalizing on Development and Activity-Dependent Plasticity, an Interaction With Pediatric-Onset Spinal Cord Injury. Front. Pediatr. 2022, 10, 804622. [Google Scholar] [CrossRef] [PubMed]
- Howland, D.R.; Trimble, S.A.; Fox, E.J.; Tester, N.J.; Spiess, M.R.; Senesac, C.R.; Kleim, J.A.; Spierre, L.Z.; Rose, D.K.; Johns, J.S.; et al. Recovery of walking in nonambulatory children with chronic spinal cord injuries: Case series. J. Neurosci. Res. 2023, 101, 826–842. [Google Scholar] [CrossRef]
- Lucas, K.; Singh, G.; Alvarado, L.R.; King, M.; Stepp, N.; Parikh, P.; Ugiliweneza, B.; Gerasimenko, Y.; Behrman, A.L. Non-invasive spinal neuromodulation enables stepping in children with complete spinal cord injury. Brain J. Neurol. 2025. online ahead of print. [Google Scholar] [CrossRef]
- Reeves, B.; Smith, E.; Broussard, M.; Martin, R. Activity based restorative therapy considerations for children: Medical and therapeutic perspectives for the pediatric population. Front. Rehabil. Sci. 2023, 4, 1186212. [Google Scholar] [CrossRef] [PubMed]
- Butler, P.; Saavedra, S.; Sofranac, M.; Jarvis, S.; Woollacott, M. Refinement, reliability and validity of the Segmental Assessment of Trunk Control (SATCo). Pediatr. Phys. Ther. 2010, 22, 246–257. [Google Scholar] [CrossRef]
- Inanici, F.; Samejima, S.; Gad, P.; Edgerton, V.R.; Hofstetter, C.P.; Moritz, C.T. Transcutaneous Electrical Spinal Stimulation Promotes Long-Term Recovery of Upper Extremity Function in Chronic Tetraplegia. IEEE Trans. Neural Syst. Rehabil. Eng. Publ. IEEE Eng. Med. Biol. Soc. 2018, 26, 1272–1278. [Google Scholar] [CrossRef]
- Robert-Lachaine, X.; Mecheri, H.; Larue, C.; Plamondon, A. Validation of inertial measurement units with an optoelectronic system for whole-body motion analysis. Med. Biol. Eng. Comput. 2017, 55, 609–619. [Google Scholar] [CrossRef]
- Zhang, J.T.; Novak, A.C.; Brouwer, B.; Li, Q. Concurrent validation of Xsens MVN measurement of lower limb joint angular kinematics. Physiol. Meas. 2013, 34, N63–N69. [Google Scholar] [CrossRef]
- Garcia-Soidan, J.L.; Leiros-Rodriguez, R.; Romo-Perez, V.; Garcia-Lineira, J. Accelerometric Assessment of Postural Balance in Children: A Systematic Review. Diagnostics 2020, 11, 8. [Google Scholar] [CrossRef]
- Quijoux, F.; Nicolai, A.; Chairi, I.; Bargiotas, I.; Ricard, D.; Yelnik, A.; Oudre, L.; Bertin-Hugault, F.; Vidal, P.P.; Vayatis, N.; et al. A review of center of pressure (COP) variables to quantify standing balance in elderly people: Algorithms and open-access code. Physiol. Rep. 2021, 9, e15067. [Google Scholar] [CrossRef] [PubMed]
- Indrayan, A.; Holt, M.P. Concise Encyclopedia of Biostatistics for Medical Professionals; Chapman and Hall, CRC: Boca Raton, FL, USA, 2016. [Google Scholar]
- Bakdash, J.Z.; Marusich, L.R. Repeated Measures Correlation. Front. Psychol. 2017, 8, 456. [Google Scholar] [CrossRef]
- Evans, J.D. Straightforward Statistics for the Behavioral Sciences; Thomson Brooks, Cole Publishing Co.: Monterey, CA, USA, 1996. [Google Scholar]
- Cragg, J.; Krassioukov, A. Autonomic dysreflexia. CMAJ Can. Med. Assoc. J. 2012, 184, 66. [Google Scholar] [CrossRef] [PubMed]
- Eldahan, K.C.; Rabchevsky, A.G. Autonomic dysreflexia after spinal cord injury: Systemic pathophysiology and methods of management. Auton. Neurosci. Basic Clin. 2018, 209, 59–70. [Google Scholar] [CrossRef]
- Hickey, K.J.; Vogel, L.C.; Willis, K.M.; Anderson, C.J. Prevalence and etiology of autonomic dysreflexia in children with spinal cord injuries. J. Spinal Cord Med. 2004, 27 (Suppl. S1), S54–S60. [Google Scholar] [CrossRef]
- Partida, E.; Mironets, E.; Hou, S.; Tom, V.J. Cardiovascular dysfunction following spinal cord injury. Neural Regen. Res. 2016, 11, 189–194. [Google Scholar] [CrossRef]
- Teasell, R.W.; Arnold, J.M.; Krassioukov, A.; Delaney, G.A. Cardiovascular consequences of loss of supraspinal control of the sympathetic nervous system after spinal cord injury. Arch. Phys. Med. Rehabil. 2000, 81, 506–516. [Google Scholar] [CrossRef]
- Krassioukov, A. Autonomic function following cervical spinal cord injury. Respir. Physiol. Neurobiol. 2009, 169, 157–164. [Google Scholar] [CrossRef]
- Engel-Haber, E.; Bheemreddy, A.; Bayram, M.B.; Ravi, M.; Zhang, F.; Su, H.; Kirshblum, S.; Forrest, G.F. Neuromodulation in Spinal Cord Injury Using Transcutaneous Spinal Stimulation—Mapping for a Blood Pressure Response: A Case Series. Neurotrauma Rep. 2024, 5, 845–856. [Google Scholar] [CrossRef]
- Samejima, S.; Malik, R.N.; Ge, J.; Rempel, L.; Cao, K.; Desai, S.; Shackleton, C.; Kyani, A.; Sarikhani, P.; D’Amico, J.M.; et al. Cardiovascular safety of transcutaneous spinal cord stimulation in cervical spinal cord injury. Neurotherapeutics 2025, 22, e00528. [Google Scholar] [CrossRef]
- Solinsky, R.; Burns, K.; Tuthill, C.; Hamner, J.W.; Taylor, J.A. Transcutaneous spinal cord stimulation and its impact on cardiovascular autonomic regulation after spinal cord injury. Am. J. Physiol.-Heart Circ. Physiol. 2023, 326, H116–H122. [Google Scholar] [CrossRef] [PubMed]
- Flynn, J.T.; Kaelber, D.C.; Baker-Smith, C.M.; Blowey, D.; Carroll, A.E.; Daniels, S.R.; de Ferranti, S.D.; Dionne, J.M.; Falkner, B.; Flinn, S.K.; et al. Clinical Practice Guideline for Screening and Management of High Blood Pressure in Children and Adolescents. Pediatrics 2017, 140, e20171904. [Google Scholar] [CrossRef] [PubMed]
- Damato, A.N.; Galante, J.G.; Smith, W.M. Hemodynamic response to treadmill exercise in normal subjects. J. Appl. Physiol. 1966, 21, 959–966. [Google Scholar] [CrossRef]
- Itoh, M.; Endo, M.Y.; Hojo, T.; Yoshimura, M.; Fukuoka, Y. Characteristics of cardiovascular responses to an orthostatic challenge in trained spinal cord-injured individuals. J. Physiol. Anthropol. 2018, 37, 22. [Google Scholar] [CrossRef]
- Krassioukov, A.; Claydon, V.E. The clinical problems in cardiovascular control following spinal cord injury: An overview. In Progress in Brain Research; Weaver, L.C., Polosa, C., Eds.; Elsevier: Amsterdam, The Netherlands, 2006; Volume 152, pp. 223–229. [Google Scholar]
- Raguindin, P.F.; Fränkl, G.; Itodo, O.A.; Bertolo, A.; Zeh, R.M.; Capossela, S.; Minder, B.; Stoyanov, J.; Stucki, G.; Franco, O.H.; et al. The neurological level of spinal cord injury and cardiovascular risk factors: A systematic review and meta-analysis. Spinal Cord 2021, 59, 1135–1145. [Google Scholar] [CrossRef]
- Sachdeva, R.; Nightingale, T.E.; Krassioukov, A.V. The Blood Pressure Pendulum following Spinal Cord Injury: Implications for Vascular Cognitive Impairment. Int. J. Mol. Sci. 2019, 20, 2464. [Google Scholar] [CrossRef] [PubMed]
- Peters, C.G.; Harel, N.Y.; Weir, J.P.; Wu, Y.K.; Murray, L.M.; Chavez, J.; Fox, F.E.; Cardozo, C.P.; Wecht, J.M. Transcutaneous Spinal Cord Stimulation to Stabilize Seated Systolic Blood Pressure in Persons With Chronic Spinal Cord Injury: Protocol Development. Neurotrauma Rep. 2023, 4, 838–847. [Google Scholar] [CrossRef]
- Beliaeva, N.N.; Moshonkina, T.R.; Mamontov, O.V.; Zharova, E.N.; Condori Leandro, H.I.; Gasimova, N.Z.; Mikhaylov, E.N. Transcutaneous Spinal Cord Stimulation Attenuates Blood Pressure Drops in Orthostasis. Life 2022, 13, 26. [Google Scholar] [CrossRef]
- Aslan, S.C.; Legg Ditterline, B.E.; Park, M.C.; Angeli, C.A.; Rejc, E.; Chen, Y.; Ovechkin, A.V.; Krassioukov, A.; Harkema, S.J. Epidural Spinal Cord Stimulation of Lumbosacral Networks Modulates Arterial Blood Pressure in Individuals With Spinal Cord Injury-Induced Cardiovascular Deficits. Front. Physiol. 2018, 9, 565. [Google Scholar] [CrossRef]
- Sayenko, D.G.; Rath, M.; Ferguson, A.R.; Burdick, J.W.; Havton, L.A.; Edgerton, V.R.; Gerasimenko, Y.P. Self-Assisted Standing Enabled by Non-Invasive Spinal Stimulation after Spinal Cord Injury. J. Neurotrauma 2019, 36, 1435–1450. [Google Scholar] [CrossRef]
- Seelen, H.A.M.; Potten, Y.J.M.; Drukker, J.; Reulen, J.P.H.; Pons, C. Development of new muscle synergies in postural control in spinal cord injured subjects. J. Electromyogr. Kinesiol. 1998, 8, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Minassian, K.; Freundl, B.; Lackner, P.; Hofstoetter, U.S. Transcutaneous spinal cord stimulation neuromodulates pre- and postsynaptic inhibition in the control of spinal spasticity. Cell Rep. Med. 2024, 5, 101805. [Google Scholar] [CrossRef] [PubMed]
- Gladchenko, D.A.; Roshchina, L.V.; Bogdanov, S.M.; Chelnokov, A.A. Effect of transcutaneous electrical spinal cord stimulation on the functional activity of reciprocal and presynaptic inhibition in healthy subjects. Russ. Open Med. J. 2022, 11, 1–9. [Google Scholar] [CrossRef]
- Taccola, G.; Sayenko, D.; Gad, P.; Gerasimenko, Y.; Edgerton, V.R. And yet it moves: Recovery of volitional control after spinal cord injury. Prog. Neurobiol. 2018, 160, 64–81. [Google Scholar] [CrossRef] [PubMed]





| Publication ID (Sex) | Age, yrs | Height, cm | Weight, kg | Time Since SCI, yrs | SATCo | SCI Level (ASIA Impairment Scale) | SCI Etiology |
|---|---|---|---|---|---|---|---|
| P1 (m) | 14 | 164 | 53 | 9 | 12/20 | C3–T5 (B) | epidural hematoma |
| P14 (m) | 10 | 122 | 19 | 6 | 11/20 | C7 (A) | motor vehicle accident |
| P23 (m) | 6 | 109 | 18 | 6 | 9/20 | C4–C7 (B) | transverse myelitis |
| Publication ID (n of AB-LT) | Treadmill Speed, mph | Treadmill Body Weight Support, % | Treadmill Time, min | Overground Time, min | Total AB-LT Time, min |
|---|---|---|---|---|---|
| P1 (39) | 2 ± 0.01 | 78.6 ± 1.3 | 44.3 ± 1.7 | 16.5 ± 1.1 | 64.8 |
| P14 (27) | 1.1 ± 0.19 | 49.8 ± 2.5 | 60.9 ± 1.3 | 12.3 ± 1.0 | 78.1 |
| P23 (64) * | 1.8 ± 0.06 | 55.7 ± 1.4 | 46.1 ± 1.6 | 21. ± 1.8 | 74.2 |
| Motor Threshold in Sitting, mA | Treadmill Submotor Intensity, mA | Overground Submotor Intensity, mA | Average scTS Duration per One AB-LT, min | Total scTS Duration per All AB-LTs, Hours | ||||
|---|---|---|---|---|---|---|---|---|
| ID (n of scTS) | T10/T11 | T12/L1 | T10/T11 | T12/L1 | T10/T11 | T12/L1 | T10/11 & T12/L1 | T10/11 & T12/L1 |
| P1 (39) | 137.1 ± 1.7 | 152.8 ± 1.8 | 101.4 ± 0.7 | 105.1 ± 0.7 | 107.5 ± 1.2 | 111.6 ± 1.1 | 44.1 ± 0.9 | 28.7 |
| P14 (27) | 78.3 ± 2.0 | 82.1 ± 2.5 | 68.3 ± 2.6 | 70.6 ± 2.6 | 71.9 ± 2.9 | 72.2 ± 3.2 | 45.2 ± 1.5 | 17.3 |
| P23 (64) | 92.8 ± 2.4 | 91.1 ± 3.4 | 88.2 ± 1.4 | 83.2 ± 2.2 | 91.5± 2.2 | 88.8 ± 3.5 | 34.8 ± 1.5 | 36.5 |
| P1’s Events | P14’s Events | P23’s Events | |||||
|---|---|---|---|---|---|---|---|
| Adverse Occurrence | (n = 39 Sessions) | (n = 27 Sessions) | (n = 64 Sessions) | Occurrence Rate | Risk | Likelihood | |
| Risks associated with scTS | Autonomic dysreflexia | 2 | 0 | 5 | 7/130 | 5.38% | Very unlikely to occur |
| Skin redness from electrodes | 0 | 5 | 1 | 6/130 | 4.61% | Very unlikely to occur | |
| Headache | 0 | 2 | 0 | 2/130 | 1.54% | Very unlikely to occur | |
| Spasticity | 0 | 0 | 0 | 0/130 | 0% | Very unlikely to occur | |
| Pain | 0 | 0 | 0 | 0/130 | 0% | Very unlikely to occur | |
| Numbness from stimulation | 0 | 0 | 0 | 0/130 | 0% | Very unlikely to occur | |
| Bowel accident | 0 | 0 | 0 | 0/130 | 0% | Very unlikely to occur | |
| Overall risk associated with scTS | 2 | 7 | 6 | 15/130 | 11.53% | Unlikely to occur | |
| Risks associated with AB-LT | Skin irritation from a harness | 3 | 4 | 4 | 11/130 | 8.46% | Very unlikely to occur |
| Skin irritation from trainers’ manual cues | 0 | 1 | 2 | 3/130 | 2.31% | Very unlikely to occur | |
| Joint sprain | 0 | 0 | 0 | 0/130 | 0% | Very unlikely to occur | |
| Bone fracture | 0 | 0 | 0 | 0/130 | 0% | Very unlikely to occur | |
| Muscle soreness | 0 | 0 | 0 | 0/130 | 0% | Very unlikely to occur | |
| Fall | 0 | 0 | 0 | 0/130 | 0% | Very unlikely to occur | |
| Overall risk associated with AB-LT | 3 | 5 | 6 | 14/130 | 10.77% | Unlikely to occur | |
| Other † | 1 | 1 | 0 | 2/130 | 1.54% | Very unlikely to occur |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amirova, L.; Keller, A.; Singh, G.; King, M.; Parikh, P.; Stepp, N.; Ugiliweneza, B.; Gerasimenko, Y.; Behrman, A.L. Cumulative Transcutaneous Spinal Stimulation with Locomotor Training Safely Improves Trunk Control in Children with Spinal Cord Injury: Pilot Study. Children 2025, 12, 817. https://doi.org/10.3390/children12070817
Amirova L, Keller A, Singh G, King M, Parikh P, Stepp N, Ugiliweneza B, Gerasimenko Y, Behrman AL. Cumulative Transcutaneous Spinal Stimulation with Locomotor Training Safely Improves Trunk Control in Children with Spinal Cord Injury: Pilot Study. Children. 2025; 12(7):817. https://doi.org/10.3390/children12070817
Chicago/Turabian StyleAmirova, Liubov, Anastasia Keller, Goutam Singh, Molly King, Parth Parikh, Nicole Stepp, Beatrice Ugiliweneza, Yury Gerasimenko, and Andrea L. Behrman. 2025. "Cumulative Transcutaneous Spinal Stimulation with Locomotor Training Safely Improves Trunk Control in Children with Spinal Cord Injury: Pilot Study" Children 12, no. 7: 817. https://doi.org/10.3390/children12070817
APA StyleAmirova, L., Keller, A., Singh, G., King, M., Parikh, P., Stepp, N., Ugiliweneza, B., Gerasimenko, Y., & Behrman, A. L. (2025). Cumulative Transcutaneous Spinal Stimulation with Locomotor Training Safely Improves Trunk Control in Children with Spinal Cord Injury: Pilot Study. Children, 12(7), 817. https://doi.org/10.3390/children12070817





