Treatment of a Large Hemorrhagic Midbrain Cavernoma Within the Silvian Aqueduct in a Five-Year-Old Girl—A Case Report
Abstract
1. Introduction
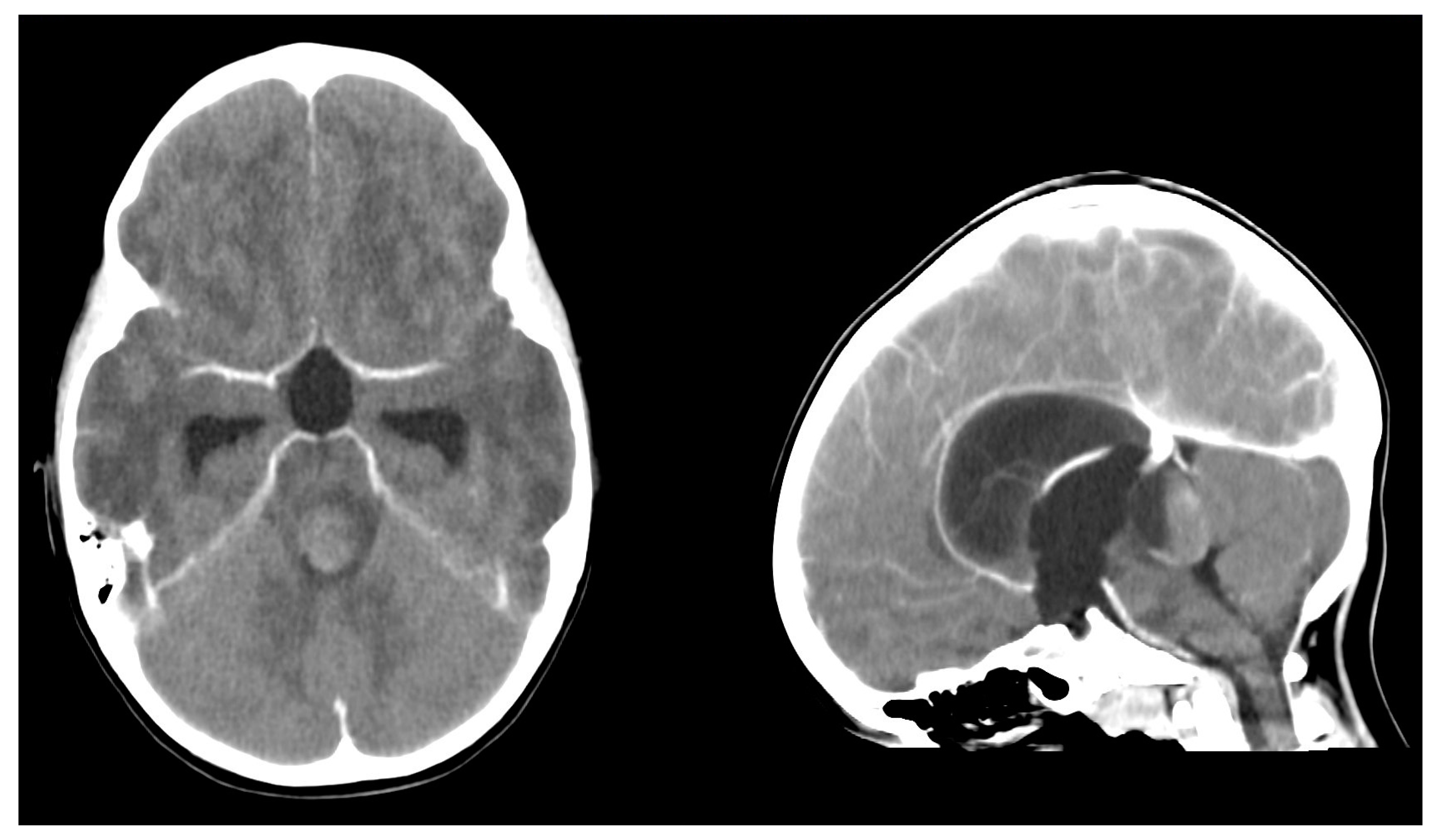
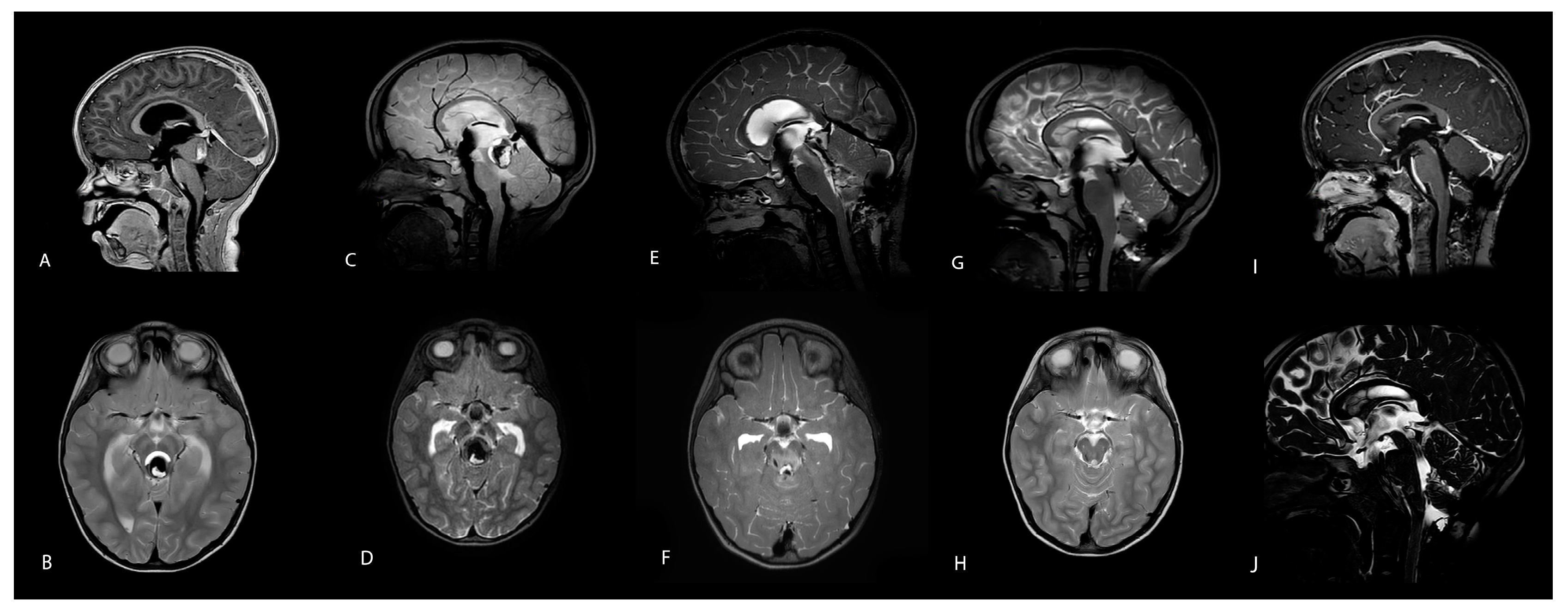
2. Case Description
3. Discussion
4. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| EVD | External Ventricular Drainage |
| DOAJ | Endoscopic Third Ventriculostomy |
| MRI | Magnetic Resonance Imaging |
References
- Goyal, A.; Fernandes-Torres, J.; Flemming, K.D.; Williams, L.N.; Daniels, D.J. Clinical presentation, natural history, and outcomes for infantile intracranial cavernous malformations: Case series and systematic review of the literature. Childs Nerv. Syst. 2023, 39, 1545–1554. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.N.; Rauschenbach, L.; Saban, D.; Chen, B.; Herten, A.; Dinger, T.F.; Li, Y.; Tippelt, S.; Della Marina, A.; Dohna-Schwake, C.; et al. Natural Course of Cerebral Cavernous Malformations in Children: A Five-Year Follow-Up Study. Stroke 2022, 53, 817–824. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, J.E.; Ryan, M.; Wittenberg, B.; Armstrong, J.; Greenan, K.; Wilkinson, C. Successful treatment of hemorrhagic brainstem cavernous malformation with hematoma evacuation and postoperative propranolol. Childs Nerv. Syst. 2020, 9, 2109–2112. [Google Scholar] [CrossRef] [PubMed]
- Bannur, U.; Korah, I.; Chandy, M.J. Midbrain venous angioma with obstructive hydrocephalus. Neurol. India 2002, 50, 207–209. [Google Scholar] [PubMed]
- Mottolese, C.; Hermier, M.; Stan, H.; Jouvet, A.; Saint-Pierre, G.; Froment, J.-C.; Bret, P.; Lapras, C. Central nervous system cavernomas in the pediatric age group. Neurosurg. Rev. 2001, 24, 55–71. [Google Scholar] [CrossRef] [PubMed]
- Al Barbarawi, M.M.; Asfour, H.A.; Qudsieh, S.M.; Alomari, S.O.; Barbarawi, A.M.; Ouda, S.H.; Allouh, M.Z. Isolated tectal cavernomas: A comprehensive literature review with a case presentation. Heliyon 2022, 8, e09244. [Google Scholar] [CrossRef] [PubMed]
- Bertolini, G.; Specchia, F.M.C.; Bertolini, P.; Giombelli, E. Suboccipital telovelar approach for microsurgical resection of a hemorrhagic brainstem cavernous malformation in an infant—How I do it. Acta Neurochir. 2023, 165, 1863–1867. [Google Scholar] [CrossRef] [PubMed]
- Shroff, K.; Deopujari, C.; Karmarkar, V.; Mohanty, C. Paediatric giant cavernomas: Report of three cases with a review of the literature. Childs Nerv. Syst. 2021, 37, 3835–3845. [Google Scholar] [CrossRef] [PubMed]
- Costa, A.; Marques-Matos, C.; Reis, C.; Carvalho, M.; Pinto, M. Alteração do comportamento e instabilidade da marcha: O valor da avaliação neuroimagiológica e da intervenção neurocirúrgica precoces. Acta Med. Port. 2017, 30, 77–79. [Google Scholar] [CrossRef] [PubMed]
- Catapano, J.S.; Rumalla, K.; Srinivasan, V.M.; Lawrence, P.M.; Keil, K.L.; Lawton, M.T. A taxonomy for brainstem cavernous malformations: Subtypes of midbrain lesions. J. Neurosurg. 2022, 136, 1667–1686. [Google Scholar] [CrossRef] [PubMed]
- Hura, N.; Vuppala, A.-A.D.; Sahraian, S.; Beheshtian, E.; Miller, N.R.; Yousem, D.M. Magnetic resonance imaging findings in Parinaud’s syndrome: Comparing pineal mass findings to other etiologies. Clin. Imaging 2019, 58, 170–176. [Google Scholar] [CrossRef]
- Pollak, L.; Zehavi-Dorin, T.; Eyal, A.; Milo, R.; Huna-Baron, R. Parinaud syndrome: Any clinicoradiological correlation? Acta Neurol. Scand. 2017, 136, 721–726. [Google Scholar] [CrossRef] [PubMed]
- Shields, M.; Sinkar, S.; Chan, W.; Crompton, J. Parinaud syndrome: A 25-year (1991–2016) review of 40 consecutive adult cases. Acta Ophthalmol. 2017, 95, e792–e793. [Google Scholar] [CrossRef] [PubMed]
- Hui, X.-H.; Li, H.; Ju, Y.; Cai, B.-W.; Chen, J.; You, C. Experience of microsurgical treatment of brainstem cavernomas: Report of 37 cases. Neurol. India 2009, 57, 269–273. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krause, M.; Michel, A.-J.; Koch, J.; Gradl, J.; Pfaff, J.A.R.; Griessenauer, C.J.; Stana-Hackenberg, L. Treatment of a Large Hemorrhagic Midbrain Cavernoma Within the Silvian Aqueduct in a Five-Year-Old Girl—A Case Report. Children 2025, 12, 564. https://doi.org/10.3390/children12050564
Krause M, Michel A-J, Koch J, Gradl J, Pfaff JAR, Griessenauer CJ, Stana-Hackenberg L. Treatment of a Large Hemorrhagic Midbrain Cavernoma Within the Silvian Aqueduct in a Five-Year-Old Girl—A Case Report. Children. 2025; 12(5):564. https://doi.org/10.3390/children12050564
Chicago/Turabian StyleKrause, Matthias, Armin-Johannes Michel, Johannes Koch, Johann Gradl, Johannes A. R. Pfaff, Christoph J. Griessenauer, and Lorenz Stana-Hackenberg. 2025. "Treatment of a Large Hemorrhagic Midbrain Cavernoma Within the Silvian Aqueduct in a Five-Year-Old Girl—A Case Report" Children 12, no. 5: 564. https://doi.org/10.3390/children12050564
APA StyleKrause, M., Michel, A.-J., Koch, J., Gradl, J., Pfaff, J. A. R., Griessenauer, C. J., & Stana-Hackenberg, L. (2025). Treatment of a Large Hemorrhagic Midbrain Cavernoma Within the Silvian Aqueduct in a Five-Year-Old Girl—A Case Report. Children, 12(5), 564. https://doi.org/10.3390/children12050564





