Surgical Versus Non-Surgical Treatment of Patients with Myopathic Scoliosis: Clinical, Radiological and Functional Outcomes
Highlights
- •
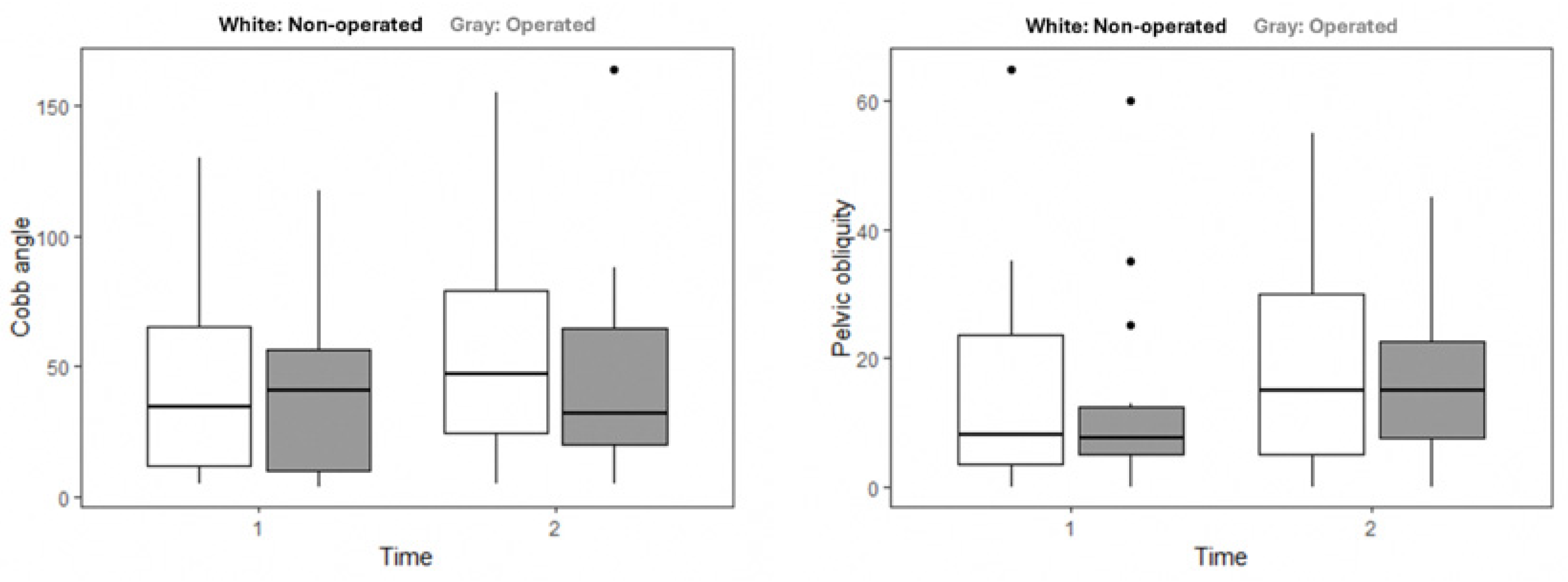
- In patients with myopathic scoliosis, both surgical and non-surgical groups showed similar worsening spinal deformity over time.
- •
- Despite similar radiological outcomes, surgically treated patients reported higher overall quality of life and functional independence, particularly in self-image domains.
- •
- Surgical correction may enhance subjective quality of life even when objective spinal improvement is limited, emphasizing the importance of patient-centered outcomes.
- •
- Decision-making for scoliosis surgery in myopathic patients should carefully balance medical risks with potential long-term gains in function and well-being.
Abstract
1. Introduction
2. Materials and Methods
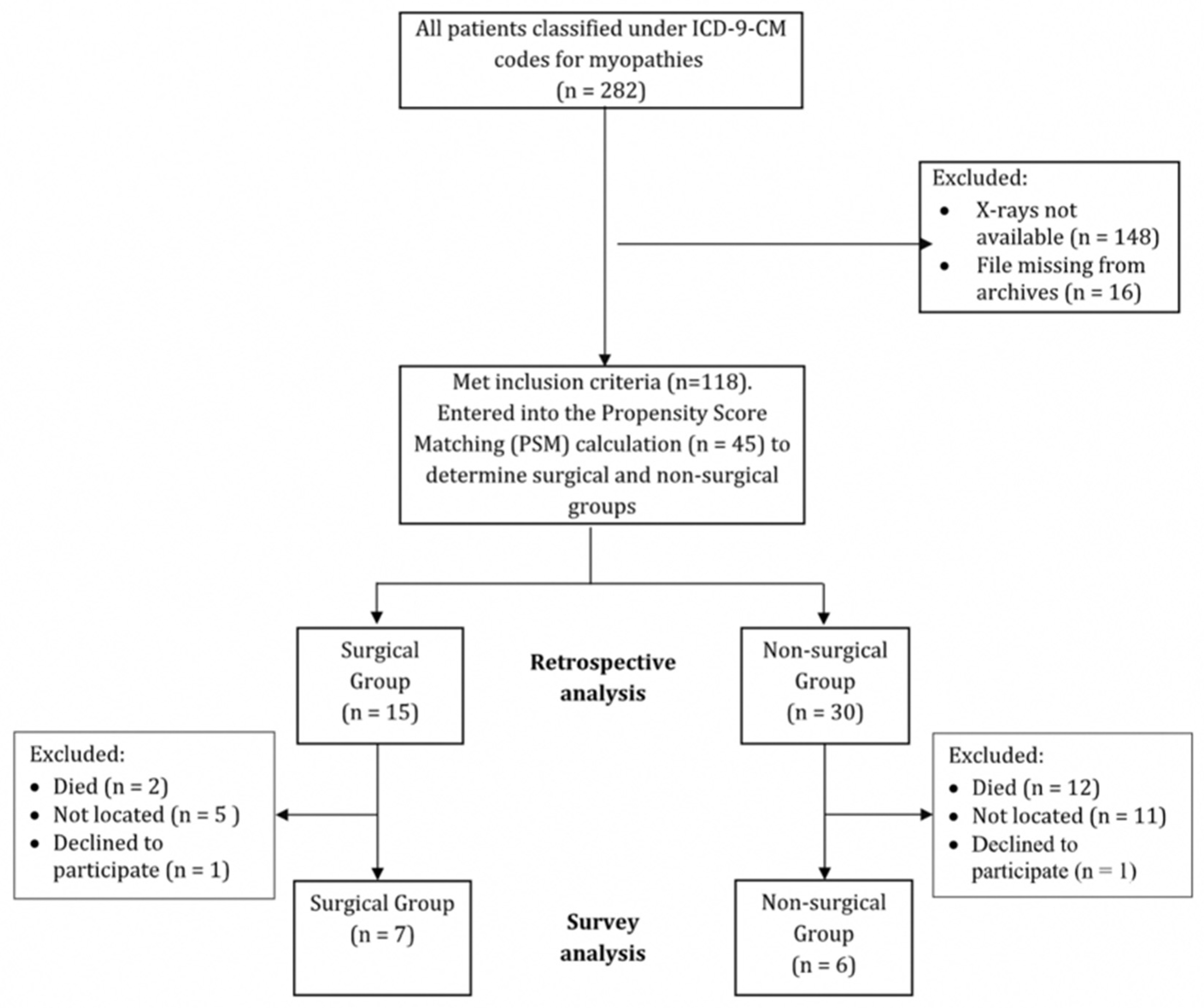
2.1. Study Design
2.2. Patients and Research Team
2.3. Context
2.4. Instruments
2.5. Data Retrieval and Analysis
3. Results
4. Discussion
5. Summary and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- McCarthy, R.E. Management of Neuromuscular Scoliosis. Orthop. Clin. N. Am. 1999, 30, 435–449. [Google Scholar] [CrossRef]
- Nelson, S.E.; Sanders, J.O. Natural history including measures of maturity. In Bridwell and DeWald’s Textbook of Spinal Surgery; Wolters Kuwar: Alphen aan den Rijn, The Netherlands, 2019; pp. 717–727. [Google Scholar]
- Mayer, O.H. Scoliosis and the Impact in Neuromuscular Disease. Paediatr. Respir. Rev. 2015, 16, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Sarwark, J.; Sarwahi, V. New Strategies and Decision Making in the Management of Neuromuscular Scoliosis. Orthop. Clin. N. Am. 2007, 38, 485–496. [Google Scholar] [CrossRef]
- Archer, J.E.; Gardner, A.C.; Roper, H.P.; Chikermane, A.A.; Tatman, A.J. Duchenne muscular dystrophy: The management of scoliosis. J. Spine Surg. 2016, 2, 185–194. [Google Scholar] [CrossRef]
- Wishart, B.D.; Kivlehan, E. Neuromuscular Scoliosis. Phys. Med. Rehabil. Clin. N. Am. 2021, 32, 547–556. [Google Scholar] [CrossRef] [PubMed]
- Howard, J.J.; Farrelly, J. In Paediatric Orthopaedics: An Evidence-Based Approach to Clinical Questions; Alshryda, S., Huntley, J.S., Banaszkiewicz, P.A., Eds.; Evidence-based treatment of neuromuscular scoliosis. Springer International Publishing: Cham, Switzerland, 2017; pp. 213–228. [Google Scholar] [CrossRef]
- Cheuk, D.K.; Wong, V.; Wraige, E.; Baxter, P.; Cole, A. Surgery for scoliosis in Duchenne muscular dystrophy. Cochrane Database Syst. Rev. 2015, 2015, CD005375. [Google Scholar] [CrossRef] [PubMed]
- Farber, H.J.; Phillips, W.A.; Kocab, K.L.; Hanson, D.S.; Heydemann, J.A.; Dahl, B.T.; Spoede, E.T.; Jefferson, L.S. Impact of scoliosis surgery on pulmonary function in patients with muscular dystrophies and spinal muscular atrophy. Pediatr. Pulmonol. 2020, 55, 1037–1042. [Google Scholar] [CrossRef]
- Murphy, R.F.; Mooney, J.F. Current concepts in neuromuscular scoliosis. Curr. Rev. Musculoskelet. Med. 2019, 12, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Reames, D.L.; Smith, J.S.; Fu, K.M.G.; Polly, D.W.; Ames, C.P.; Berven, S.H.; Perra, J.H.; Glassman, S.D.; McCarthy, R.E.; Knapp, R.D.; et al. Complications in the Surgical Treatment of 19,360 Cases of Pediatric Scoliosis. Spine 2011, 36, 1484–1491. [Google Scholar] [CrossRef] [PubMed]
- Rumalla, K.; Yarbrough, C.K.; Pugely, A.J.; Koester, L.; Dorward, I.G. Spinal fusion for pediatric neuromuscular scoliosis: National trends, complications, and in-hospital outcomes. J. Neurosurg. Spine 2016, 25, 500–508. [Google Scholar] [CrossRef] [PubMed]
- Loughenbury, P.R.; Tsirikos, A.I. Current concepts in the treatment of neuromuscular scoliosis: Clinical assessment, treatment options, and surgical outcomes. Bone Jt. Open 2022, 3, 85–92. [Google Scholar] [CrossRef]
- Tsirikos, A.I.; Roberts, S.B.; Bhatti, E. Incidence of spinal deformity surgery in a national health service from 2005 to 2018. Bone Jt. Open 2020, 1, 19–28. [Google Scholar] [CrossRef]
- Gaume, M.; Saghbiny, E.; Richard, L.; Thouement, C.; Vialle, R.; Miladi, L. Pelvic Fixation Technique Using the Ilio-Sacral Screw for 173 Neuromuscular Scoliosis Patients. Children 2024, 11, 199. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Swallow, J.; Gagnier, J.; Cahill, P.J.; Sponseller, P.D.; Garg, S.; Thompson, G.H.; Ramo, B.A.; Pediatric Spine Study Group. Growth-friendly surgery results in more growth but a higher complication rate and unplanned returns to the operating room compared to single fusion in neuromuscular early-onset scoliosis: A multicenter retrospective cohort study. Spine Deform. 2021, 9, 851–858. [Google Scholar] [CrossRef] [PubMed]
- Magee, L.; Bram, J.T.; Anari, J.B.; Ramo, B.; Mayer, O.H.; Matsumoto, H.; Brooks, J.T.; Andras, L.; Lark, R.; Fitzgerald, R.; et al. Outcomes and Complications in Management of Congenital Myopathy Early-Onset Scoliosis. J. Pediatr. Orthop. 2021, 41, 531–536. [Google Scholar] [CrossRef]
- Miladi, L.; Gaume, M.; Khouri, N.; Johnson, M.; Topouchian, V.; Glorion, C. Minimally Invasive Surgery for Neuromuscular Scoliosis. Spine 2018, 43, E968–E975. [Google Scholar] [CrossRef]
- Eylon, S.; Weiss, P.L.; Rigbi, A.; Hanna, R.; Schroeder, J.; Satanovsky, S. Patients with myopathy and scoliosis treated conservatively: Retrospective long-term follow-up and prospective outcomes. Glob. Spinal J. 2025, in press. [Google Scholar] [CrossRef]
- Stinissen, L.; Bouma, S.; Böhm, J.; van Tienen, J.; Fischer, H.; Hughes, Z.; Lennox, A.; Ward, E.; Wood, M.; Foley, A.R.; et al. The experience of clinical study and trial participation in rare diseases: A scoping review of centronuclear myopathy and other neuromuscular disorders. Neuromuscul. Disord. 2023, 38, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Satanovsky, A.; Eylon, S.; Kaplan, L.; Schroeder, J. Scoliosis in pediatric neuromuscular myopathy—A retrospective national cohort. Presented at: Global Spine Congress; May 2023; Prague, Czech Republic. Glob Spine J. 2023, 13 (Suppl. 2), 4S–214S. [Google Scholar] [CrossRef]
- World Health Organization. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM); Centers for Disease Control and Prevention: Atlanta, GA, USA, 1979. Available online: https://archive.cdc.gov/www_cdc_gov/nchs/icd/icd9cm.htm (accessed on 1 October 2025).
- Bradford, D.S.; Hensinger, R.N. The Pediatric Spine; Thieme: New York, NY, USA, 1985. [Google Scholar]
- Studer, D. Clinical investigation and imaging. J. Child. Orthop. 2013, 7, 29–35. [Google Scholar] [CrossRef]
- Karkenny, A.J.; Magee, L.C.; Landrum, M.R.; Anari, J.B.; Spiegel, D.; Baldwin, K. The Variability of Pelvic Obliquity Measurements in Patients with Neuromuscular Scoliosis. JBJS Open Access 2021, 6, e20. [Google Scholar] [CrossRef]
- Shrader, M.W.; Andrisevic, E.M.; Belthur, M.V.; White, G.R.; Boan, C.; Wood, W. Inter- and Intraobserver Reliability of Pelvic Obliquity Measurement Methods in Patients with Cerebral Palsy. Spine Deform. 2018, 6, 257–262. [Google Scholar] [CrossRef]
- Skevington, S.M.; McCrate, F.M. Expecting a good quality of life in health: Assessing people with diverse diseases and conditions using the WHOQOL-BREF. Health Expect. 2011, 15, 49–62. [Google Scholar] [CrossRef]
- Glattes, R.C.; Burton, D.C.; Lai, S.M.; Frasier, E.; Asher, M.A. The Reliability and Concurrent Validity of the Scoliosis Research Society-22r Patient Questionnaire Compared with the Child Health Questionnaire-CF87 Patient Questionnaire for Adolescent Spinal Deformity. Spine 2007, 32, 1778–1784. [Google Scholar] [CrossRef] [PubMed]
- Haidar, R.K.; Kassak, K.; Masrouha, K.; Ibrahim, K.; Mhaidli, H. Reliability and Validity of an Adapted Arabic Version of the Scoliosis Research Society-22r Questionnaire. Spine 2015, 40, E971–E977. [Google Scholar] [CrossRef]
- Niemeijer, A.S.; Reinders-Messelink, H.A.; Disseldorp, L.M.; Nieuwenhuis, M.K. Feasibility, Reliability, and Agreement of the WeeFIM Instrument in Dutch Children with Burns. Phys. Ther. 2012, 92, 958–966. [Google Scholar] [CrossRef]
- Ottenbacher, K.J.; Taylor, E.T.; Msall, M.E.; Braun, S.; Lane, S.J.; Granger, C.V.; Lyons, N.; Duffy, L.C. The stability and equivalence reliability of the functional independence measure for children. Dev. Med. Child Neurol. 1996, 38, 907–916. [Google Scholar] [CrossRef]
- Ziviani, J.; Ottenbacher, K.J.; Shephard, K.; Foreman, S.; Astbury, W.; Ireland, P. Concurrent Validity of the Functional Independence Measure for Children (WeeFIM(TM)) and the Pediatric Evaluation of Disabilities Inventory in Children with Developmental Disabilities and Acquired Brain Injuries. Phys. Occup. Ther. Pediatr. 2002, 21, 91–101. [Google Scholar] [CrossRef]
- Rosenbaum, P.R. Optimal Matching for Observational Studies. J. Am. Stat. Assoc. 1989, 84, 1024–1032. [Google Scholar] [CrossRef]
- Noguchi, K.; Gel, Y.R.; Brunner, E.; Konietschke, F. nparLD: An R Software Package for the Nonparametric Analysis of Longitudinal Data in Factorial Experiments. J. Stat. Softw. 2012, 50, 1–23. [Google Scholar] [CrossRef]
- Parr, A.; Askin, G. Paediatric scoliosis: Update on assessment and treatment. Aust. J. Gen. Pract. 2020, 49, 832–837. [Google Scholar] [CrossRef]
- Tsirikos, A.I.; Wordie, S.J. The surgical treatment of spinal deformity in children with non-ambulatory myelomeningocele. Bone Jt. J. 2021, 103-B, 1133–1141. [Google Scholar] [CrossRef] [PubMed]
- Tsirikos, A.I.; Chang, W.N.; Dabney, K.W.; Miller, F. Comparison of Parents’ and Caregivers’ Satisfaction After Spinal Fusion in Children with Cerebral Palsy. J. Pediatr. Orthop. 2004, 24, 54–58. [Google Scholar] [CrossRef]
- Bell, D.F.; Moseley, C.F.; Koreska, J. Unit Rod Segmental Spinal Instrumentation in the Management of Patients with Progressive Neuromuscular Spinal Deformity. Spine 1989, 14, 1301–1307. [Google Scholar] [CrossRef]
- Matsumoto, H.; Fano, A.N.; Herman, E.T.; Snyder, B.; Roye, B.D.; Cahill, P.; Ramo, B.; Sponseller, P.; Vitale, M.G.; Pediatric Spine Study Group. Mortality in Neuromuscular Early Onset Scoliosis Following Spinal Deformity Surgery. J. Pediatr. Orthop. 2022, 42, e234–e241. [Google Scholar] [CrossRef]
- Bridwell, K.H.; Baldus, C.; Iffrig, T.M.; Lenke, L.G.; Blanke, K. Process Measures and Patient/Parent Evaluation of Surgical Management of Spinal Deformities in Patients with Progressive Flaccid Neuromuscular Scoliosis (Duchenne’s Muscular Dystrophy and Spinal Muscular Atrophy). Spine 1999, 24, 1300. [Google Scholar] [CrossRef]
- Larsson, E.L.C.; Aaro, S.I.; Helena Öberg, B.E. Long-Term Follow-up of Functioning after Spinal Surgery in Patients with Neuromuscular Scoliosis. Spine 2005, 30, 2145–2152. [Google Scholar] [CrossRef] [PubMed]
- Ersberg, A.; Gerdhem, P. Pre- and postoperative quality of life in patients treated for scoliosis. Acta Orthop. 2013, 84, 537–543. [Google Scholar] [CrossRef] [PubMed]
- Barone, G.; Giudici, F.; Manzini, F.; Pironti, P.; Vigano, M.; Minoia, L.; Archetti, M.; Zagra, A.; Scaramuzzo, L. Adolescent Idiopathic Scoliosis Surgery: Postoperative Functional Outcomes at 32 Years Mean Follow-Up. Children 2024, 11, 52. [Google Scholar] [CrossRef]
| Matching Variable | Non-Surgical (n = 30) | Surgical (n = 15 *) | Significance |
|---|---|---|---|
| Age at first visit (Md., IQR) | 6.00, 13 | 4.90, 9.9 | Wilcoxon rank sum test: p = 0.22 |
| Cobb angle at baseline (Md., IQR) | 34.50, 56 | 41, 51 | Wilcoxon rank sum test: p = 0.79 |
| Number (%) | Number (%) | ||
| Diagnosis | Fisher exact test: p = 0.62 | ||
| Myopathy, unspecified | 10 (33) | 3 (20) | |
| Congenital myopathy—fiber type disproportion | 4 (13) | 5 (33) | |
| Congenital muscular dystrophy | 12 (40) | 5 (33) | |
| Congenital myopathy—nemaline | 2 (7) | 1 (7) | |
| Spinocerebellar disease | 2 (7) | 1 (7) |
| Non-Surgical | Surgical | |||
|---|---|---|---|---|
| First Visit | Last Visit | First Visit | Last Visit | |
| Cobb Angle Md. (IQR) | 34.5 (53.2) | 47 (54.7) | 41 (46.5) | 32 (44.5) |
| Pelvic Obliquity Md. (IQR) | 8 (20) | 15 (25) | 7.5 (7.2) | 15 (15) |
| Measure | Non-Surgical Patients Md. (IQR) (n = 6) | Surgical Patients Md. (IQR) (n = 7) |
|---|---|---|
| QoL * | 3.40 (0.88) | 4.15 (0.56) |
| WeeFIM | 3.47 (1.15) | 4.28 (3.88) |
| SRS general self-image | 4.50 (1.17) | 4.66 (1.00) |
| SRS pain | 4.71 (0.93) | 4.00 (0.86) |
| SRS general function | 4.33 (0.75) | 3.67 (0.67) |
| SRS Function activity | 3.67 (0.33) | 2.33 (1.00) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Satanovsky, A.; Hanna, R.; Weiss, P.L.; Rigbi, A.; Schroeder, J.E.; Eylon, S. Surgical Versus Non-Surgical Treatment of Patients with Myopathic Scoliosis: Clinical, Radiological and Functional Outcomes. Children 2025, 12, 1562. https://doi.org/10.3390/children12111562
Satanovsky A, Hanna R, Weiss PL, Rigbi A, Schroeder JE, Eylon S. Surgical Versus Non-Surgical Treatment of Patients with Myopathic Scoliosis: Clinical, Radiological and Functional Outcomes. Children. 2025; 12(11):1562. https://doi.org/10.3390/children12111562
Chicago/Turabian StyleSatanovsky, Alexandra, Rana Hanna, Patrice L. Weiss, Amihai Rigbi, Josh E. Schroeder, and Sharon Eylon. 2025. "Surgical Versus Non-Surgical Treatment of Patients with Myopathic Scoliosis: Clinical, Radiological and Functional Outcomes" Children 12, no. 11: 1562. https://doi.org/10.3390/children12111562
APA StyleSatanovsky, A., Hanna, R., Weiss, P. L., Rigbi, A., Schroeder, J. E., & Eylon, S. (2025). Surgical Versus Non-Surgical Treatment of Patients with Myopathic Scoliosis: Clinical, Radiological and Functional Outcomes. Children, 12(11), 1562. https://doi.org/10.3390/children12111562




_Weiss.png)


