Timing of Orthodontic Intervention for Pediatric Class II Malocclusion: A Systematic Review on Early vs. Late Treatment Outcomes
Highlights
- Early orthodontic intervention significantly improves skeletal development, arch dimensions, and airway space in patients with Class II malocclusion.
- Statistically significant differences favor early treatment in parameters such as gonial angle, maxillary width, and dental arch length.
- Timely application of growth-modifying appliances enhances treatment outcomes and may reduce the need for extractions or prolonged fixed appliance therapy.
- Individualized treatment timing, particularly favoring early intervention in selected cases, should be integrated into evidence-based planning for orthodontic treatment in pediatric patients.
Abstract
1. Introduction
- Population (P): children (6–14 years old) with malocclusion, primarily Class II cases.
- Intervention (I): early orthodontic treatment initiated during the deciduous or early mixed dentition phase (evaluate the effectiveness of growth-modifying appliances (e.g., cervical headgear (CH), Modified C-palatal plates (MCPP), the Eruption Guidance Appliance, EGA) when applied at different stages of dentofacial development).
- Comparison (C): late orthodontic treatment initiated during the late mixed or early permanent dentition phase.
- Outcomes (O): Skeletal, dental, and airway-related changes; treatment duration and efficiency; need for extractions or fixed appliances; and long-term stability.
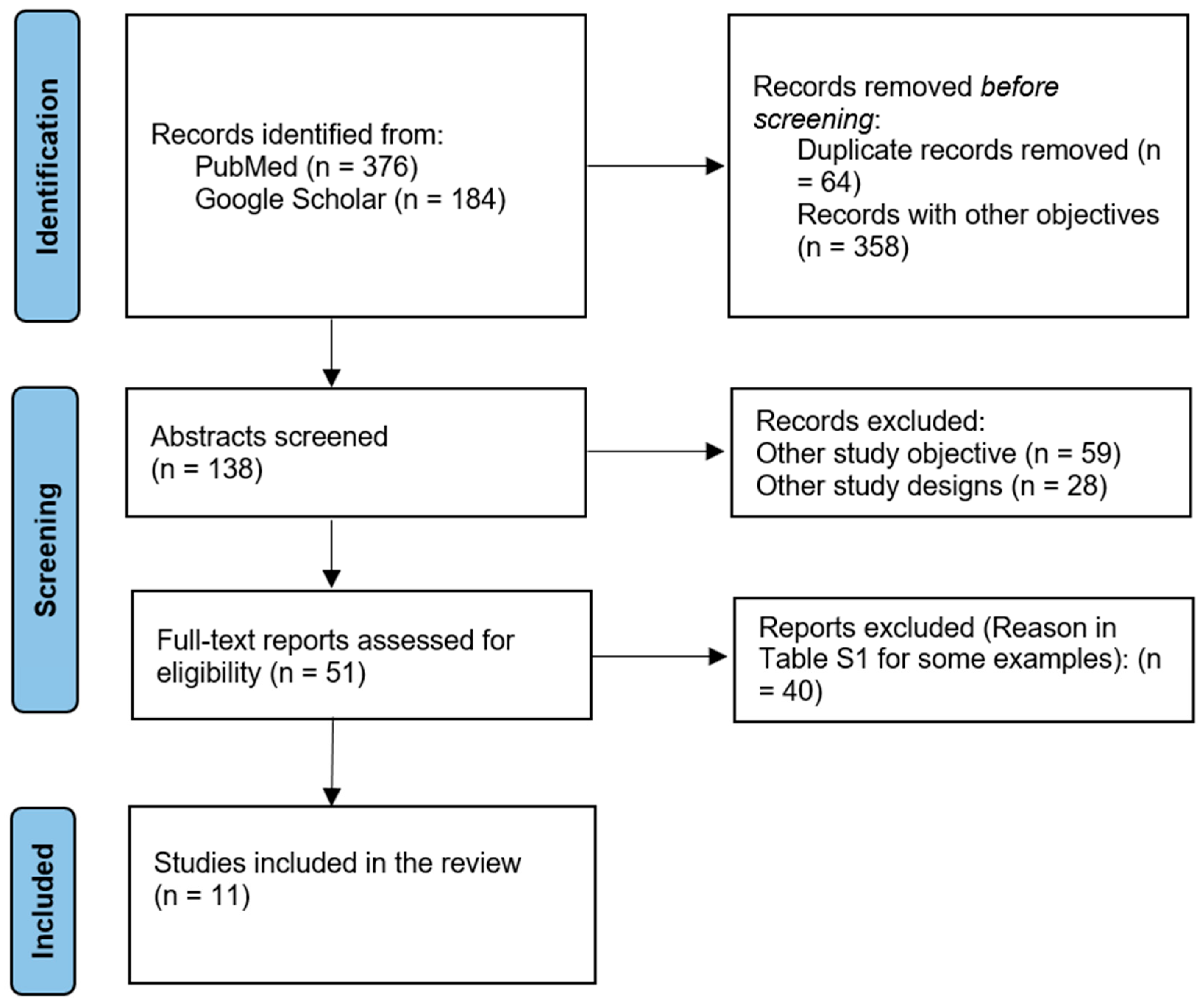
2. Materials and Methods
2.1. Study Design
2.2. Study Selection and Eligibility Criteria
- The population of interest included children aged 6 to 14 years who were free from craniofacial syndromes or cleft conditions.
- The intervention had to involve orthodontic treatment with fixed, removable, or functional appliances, initiated either in early childhood (ages 6–9) or during the later mixed to early permanent dentition stage (ages 10–14).
- Essentially, studies were required to offer a clear comparison between early and late treatment groups, ideally with at least a two-year age gap between cohorts.
- Only studies published in English were included.
- Included studies also had to report on at least one of the following outcomes: occlusal changes, treatment duration, post-treatment stability, or patient-centered outcomes such as satisfaction or psychosocial impact.
- Case reports, narrative or systematic reviews, editorials, and expert opinions.
- Studies involving non-orthodontic interventions or mixed-age samples without distinct early and late treatment groups.
- Articles lacking sufficient data for extraction or reporting outcomes unrelated to treatment timing.
2.3. Data Items and Data Analysis
2.4. Risk of Bias Assessment
3. Results
3.1. Overview of Selected Studies
| Study ID | Country | Study Design | Age Range/ Mean Age (years) | Number of Participants | Type of Malocclusion | Treatment Modality | Follow-Up Duration | Skeletal Maturity Stage at Treatment Onset | Key Findings |
|---|---|---|---|---|---|---|---|---|---|
| Julku et al., 2019 [9] | Finland | RCT | 7–18 | 56 | Class II | Cervical headgear (CH) | 11 yrs | EG = Prepubertal (CVMS I–II); LG = Pubertal (CVMS III) | Early treatment improved the anteroposterior jaw relationship, with minimal differences in long-term outcomes. |
| Käsmä et al., 2025 [12] | Finland | RCT | 7–18 | 67 | Class II | CH treatment | 14 yrs | EG = Prepubertal (CVMS I–II); LG = Pubertal (CVMS III) | Later treatment improved eruption timing and alignment; the early group showed more molar tipping. |
| Kallunki et al., 2022 [13] | Sweden | RCT | 9–11 | 56 | Class II | Headgear activator | 24 mo | EG = Prepubertal (CVMS I–II); LG = Pubertal (CVMS III) | Similar costs and outcomes were observed between the early and late groups, with a reduction in overjet in both. |
| Julku et al., 2019 [10] | Finland | RCT | Mean age 7.2 | 67 | Class II | CH treatment | 24–26 mo | EG = Prepubertal (CVMS I–II); LG = Pubertal (CVMS III) | Early CH treatment is more effective in males due to differences in skeletal maturation. |
| Kim et al., 2024 [14] | Korea | RCT | 9.6–12.3 | 71 | Hyperdivergent Class II | MCPP and CH | - | EG = Pubertal (CVMS III); LG = Postpubertal (CVMS IV) | Early MCPP showed greater vertical control and skeletal balance (p < 0.010). |
| Männchen et al., 2022 [17] | Italy | Retrospective study | 8–18 | 527 | Class II | Functional and fixed appliances | 6 yrs | Not reported | Early treatment reduced the need for extraction and fixed appliances, but resulted in a longer total treatment time. |
| Mandall et al., 2022 [15] | United Kingdom | RCT | 11–13 | 75 | Class II | Rapid maxillary expansion and facemask | ≥3 yrs | Not reported | Early intervention reduced ANB and overjet; similar psychosocial outcomes. |
| Julku et al., 2018 [11] | Finland | RCT | 7–11.5 | 67 | Class II | CH treatment | 4.5 yrs | Prepubertal (CVMS I–II) | Significant posterior maxillary movement in early treatment males. |
| Myrlund et al., 2018 [19] | Norway | Prospective cohort study | 7.7–9.1 | 35 | Class II | EGA | 6 yrs | EG = Prepubertal (CVMS I–II); LG = Pubertal (CVMS III) | Significant improvements in overjet, overbite, and crowding after early intervention. |
| Fourneron et al., 2020 [18] | France | Retrospective study | <7 vs. ≤13 | 40 | Unilateral posterior crossbite (UPCB) | Quad Helix (QH) | 18 mo | EG = Prepubertal (CVMS I–II); LG = Pubertal–Postpubertal (CVMS III–IV) | Early treatment improved mandibular asymmetry correction (+1 mm, p = 0.008) |
| Hannula et al., 2023 [16] | Finland | RCT | 7–18 | 46 | Class II | CH treatment | 14 yrs | Prepubertal (CVMS I–II) | The early group showed greater gains in arch width and length, particularly in males. |
3.2. Risk of Bias
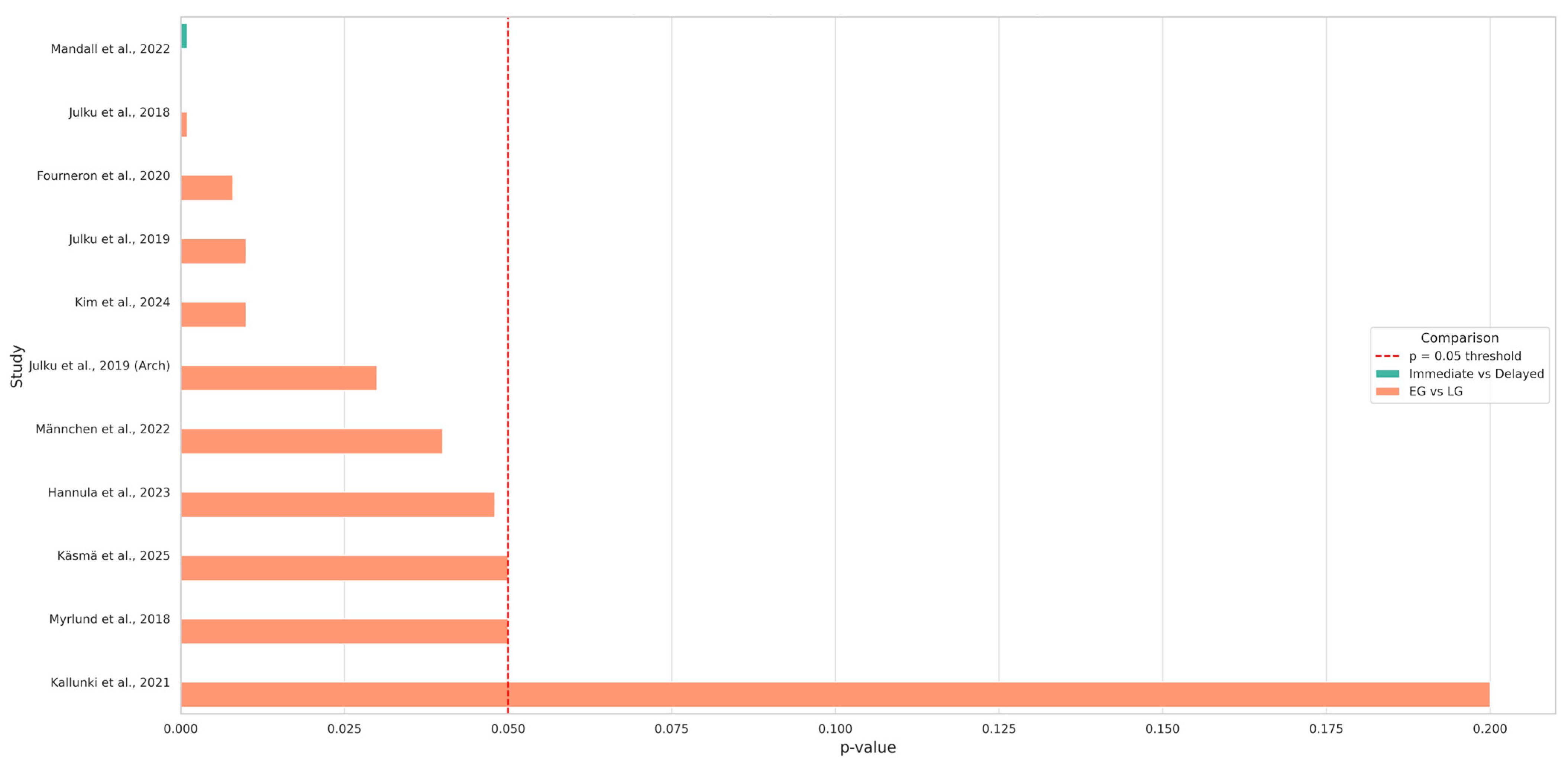
3.3. Statistical Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statements
Acknowledgments
Conflicts of Interest
Abbreviations
| CH | Cervical Headgear |
| MCPP | Modified C-palatal Plate |
| EGA | Eruption Guidance Appliance |
| RCT | Randomized Controlled Trial |
| OSA | Obstructive Sleep Apnea |
| EG | Early Group |
| LG | Late Group |
| FFA | Full Fixed Appliance |
| DPT | Dental Panoramic Tomograph |
| ANB | A point–Nasion–B point (cephalometric angle) |
| FMA | Frankfort–Mandibular Plane Angle |
| SN-GoGn | Sella–Nasion to Gonion–Gnathion angle |
| NSL-PL | Nasion–Sella Line to Palatal Line |
| rl1–rl2 | Retroglottic airway linear measurement |
References
- Fleming, P.S.; Andrews, J. Orthodontic treatment: Getting the timing right. Semin. Orthod. 2023, 29, 137–145. [Google Scholar] [CrossRef]
- Schneider-Moser, U.E.M.; Moser, L. Very early orthodontic treatment: When, why and how? Dental Press J. Orthod. 2022, 27, e22spe2. [Google Scholar] [CrossRef]
- Atasever İşler, A.A.; Hezenci, Y.; Bulut, M. Prevalence of orthodontic malocclusion in children aged 10–12: An epidemiological Study. BMC Oral Health 2025, 25, 249. [Google Scholar] [CrossRef] [PubMed]
- Giuntini, V.; McNamara, J.A.; Franchi, L. Treatment of class II malocclusion in the growing patient: Early or late? Semin. Orthod. 2023, 29, 183–188. [Google Scholar] [CrossRef]
- Keski-Nisula, K.; Hernesniemi, R.; Heiskanen, M.; Keski-Nisula, L.; Varrela, J. Orthodontic intervention in the early mixed dentition: A prospective, controlled study on the effects of the eruption guidance appliance. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 254–260. [Google Scholar] [CrossRef] [PubMed]
- Di Spirito, F.; Cannatà, D.; Schettino, V.; Galdi, M.; Bucci, R.; Martina, S. Perceived orthodontic needs and attitudes towards early evaluation and interventions: A survey-based study among parents of Italian school-aged children. Clin. Pract. 2024, 14, 1159–1170. [Google Scholar] [CrossRef]
- DiBiase, A. The timing of orthodontic treatment. Dent. Update 2002, 29, 434–441. [Google Scholar] [CrossRef][Green Version]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- Julku, J.; Pirilä-Parkkinen, K.; Tolvanen, M.; Pirttiniemi, P. Comparison of effects of cervical headgear treatment on skeletal facial changes when the treatment time is altered: A randomized controlled trial. Eur. J. Orthod. 2019, 41, 631–640. [Google Scholar] [CrossRef]
- Julku, J.; Hannula, M.; Pirilä-Parkkinen, K.; Tolvanen, M.; Pirttiniemi, P. Dental arch effects after early and later timed cervical headgear treatment—A randomized controlled trial. Eur. J. Orthod. 2019, 41, 622–630. [Google Scholar] [CrossRef]
- Julku, J.; Pirilä-Parkkinen, K.; Pirttiniemi, P. Airway and hard tissue dimensions in children treated with early and later timed cervical headgear—A randomized controlled trial. Eur. J. Orthod. 2018, 40, 285–295. [Google Scholar] [CrossRef]
- Käsmä, K.; Silvola, A.-S.; Vuollo, V.; Julku, J. Effects of early and later timed cervical headgear treatment on the eruption timing and pattern of permanent upper canines and molars: Follow-up of a randomized controlled trial. Eur. J. Orthod. 2025, 47, cjaf056. [Google Scholar] [CrossRef] [PubMed]
- Kallunki, J.; Bondemark, L.; Paulsson, L. Comparisons of costs and treatment effects—An RCT on headgear activator treatment of excessive overjet in the mixed and late mixed dentition. Eur. J. Orthod. 2022, 44, 86–94. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, N.-K.; Kook, Y.-A.; Kim, Y.; Park, C.O.; Chou, A.H.K.; Han, S.-H.; Park, J.H. Long-Term Skeletodental Changes with early and late treatment using modified C-palatal plates in hyperdivergent Class II adolescents. Angle Orthod. 2024, 94, 303–312. [Google Scholar] [CrossRef]
- Mandall, N.; Littlewood, S.; Shah, J.; Watkinson, S.; Glossop, S.; Dugdale, C.; Curran, E.; Walsh, T. The effect of treatment timing on clinical and psychological outcomes with Twin Block therapy: A multicenter two-Arm parallel randomized controlled trial. J. Orthod. 2023, 50, 45–54. [Google Scholar] [CrossRef] [PubMed]
- Hannula, M.; Tolvanen, M.; Pirttiniemi, P.; Pirilä-Parkkinen, K.; Julku, J. Effects of headgear timing on dental arch changes from 7 to 18 years of age: A follow-up study. Eur. J. Orthod. 2023, 45, 496–504. [Google Scholar] [CrossRef]
- Männchen, R.; Serafin, M.; Fastuca, R.; Caprioglio, A. Does early treatment improve clinical outcome of Class II patients? A retrospective study. Children 2022, 9, 232. [Google Scholar] [CrossRef]
- Fourneron, M.; Morant, F.; Boutin, F.; Frapier, L. Is the Quad Helix more efficient to correct mandibular asymmetry before age 7? A retrospective comparative study. Int. Orthod. 2020, 18, 443–450. [Google Scholar] [CrossRef]
- Myrlund, R.; Keski-Nisula, K.; Kerosuo, H. Stability of orthodontic treatment outcomes after 1-year treatment with the eruption guidance appliance in the early mixed dentition: A follow-up study. Angle Orthod. 2019, 89, 206–213. [Google Scholar] [CrossRef]
- Batista, K.B. Orthodontic treatment for prominent upper front teeth (Class II malocclusion) in children and adolescents (Review). Cochrane Database Syst. Rev. 2018, 3, CD003452. [Google Scholar] [CrossRef]
- Cha, J.-Y.; Kennedy, D.B.; Turley, P.K.; Joondeph, D.R.; Baik, H.-S.; Hwang, C.-J.; Sinclair, P.M. Outcomes of early versus late treatment of severe Class II high-angle patients. Am. J. Orthod. Dentofac. Orthop. 2019, 156, 375–382. [Google Scholar] [CrossRef]
- Kaje, R.; Rashme, R.; Manimegalan, P.; Vundela, R.R.; Saidalavi, S.K.; Jadhav, A.V. Assessing the efficacy of early versus late orthodontic intervention in the management of Class II malocclusion: A comparative analysis. J. Pharm. Bioallied Sci. 2024, 16, S2691–S2693. [Google Scholar] [CrossRef]
- Ardani, I.G.W.; Aini, H.; Narmada, I.; Deshmukh, S.; Nugraha, A. Class II division 1 malocclusion treatment trends in the last 10 years by skeletal classification: A review article. J. Int. Oral Health 2023, 15, 342. [Google Scholar] [CrossRef]
- Khan, M.I.; Neela, P.K.; Unnisa, N.; Jaiswal, A.K.; Ahmed, N.; Purkayastha, A. Dentoskeletal effects of Twin Block appliance in patients with Class II malocclusion. Med. Pharm. Rep. 2022, 95, 191–196. [Google Scholar] [CrossRef]
- Pavičić, D.Š.; Svirčić, A.; Gašparović, B.; Šimunović, L.; Crnković, S.; Katić, V. Effect of the functional appliances on skeletal, dentoalveolar, and facial soft tissue characteristics. Appl. Sci. 2025, 15, 7529. [Google Scholar] [CrossRef]
- Kallunki, J.; Bondemark, L.; Paulsson-Björnsson, L. Outcomes of early Class II malocclusion treatment—A systematic review. Dent. Oral Health Craniofac. Res. 2018, 3, 1–7. [Google Scholar] [CrossRef]
- Hamidaddin, M.A. Optimal treatment timing in orthodontics: A scoping review. Eur. J. Dent. 2024, 18, 86–96. [Google Scholar] [CrossRef]
- Huo, B.; Che, X.; Li, X. Timing of early correction of mandibular hypoplasia in skeletal Class II malocclusion: A review. J. Clin. Pediatr. Dent. 2023, 47, 11–20. [Google Scholar] [CrossRef]
- Parkin, N.A.; McKeown, H.F.; Sandler, P.J. Comparison of two modifications of the Twin-Block appliance in matched Class II samples. Am. J. Orthod. Dentofac. Orthop. 2001, 119, 572–577. [Google Scholar] [CrossRef] [PubMed]
- Xu, F.; Fang, Y.; Sui, X.; Yao, Y. Comparison of Twin Block appliance and Herbst appliance in the treatment of Class II malocclusion among children: A meta-analysis. BMC Oral Health 2024, 24, 278. [Google Scholar] [CrossRef]
- Pacha, M.M.; Fleming, P.S.; Pandis, N.; Shagmani, M.; Johal, A. The use of the Hanks Herbst vs Twin-Block in Class II malocclusion: A randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2023, 164, 314–324.e1. [Google Scholar] [CrossRef]
- Tomblyn, T.; Rogers, M.; Andrews, L.; Martin, C.; Tremont, T.; Gunel, E.; Ngan, P. Cephalometric study of Class II division 1 patients treated with an extended-duration, reinforced, banded Herbst appliance followed by fixed appliances. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 818–830. [Google Scholar] [CrossRef] [PubMed]
- Henriques, F.P.; Janson, G.; Henriques, J.F.C.; Pupulim, D.C. Effects of cervical headgear appliance: A systematic review. Dent. Press J. Orthod. 2015, 20, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Mereani, S.; Indijani, R.K.; Alotaibi, A. The Impact of Headgear on Distalization in Class II Division I Malocclusion: A Case Report. Cureus 2024, 16, e52213. [Google Scholar] [CrossRef]
- Rosa, A.J.; Nascimento, R.R.D.; Mucha, J.N.; Vilella, O.d.V. Effects of the cervical headgear in growing Angle Class II malocclusion patients: A prospective study. Dent. Press J. Orthod. 2020, 25, 25–31. [Google Scholar] [CrossRef]
- Haralabakis, N.B.; Sifakakis, I.B. The effect of cervical headgear on patients with high or low mandibular plane angles and the “myth” of posterior mandibular rotation. Am. J. Orthod. Dentofac. Orthop. 2004, 126, 310–317. [Google Scholar] [CrossRef]
- Bates, W.R.; Cevidanes, L.S.; Larson, B.E.; Adams, D.; Ruellas, A.C.D.O. Three-dimensional cone-beam computed technology evaluation of skeletal and dental changes in growing patients with Class II malocclusion treated with the cervical pull face-bow headgear appliance. Am. J. Orthod. Dentofac. Orthop. 2022, 162, 491–501. [Google Scholar] [CrossRef]
- Park, J.H.; Saito, T.; Yoo, S.K.; Alfaifi, M.; Kook, Y.-A. Distalization with a modified C-palatal plate for severe upper crowding and a missing lower incisor. Korean J. Orthod. 2020, 50, 52–62. [Google Scholar] [CrossRef] [PubMed]
- Joo, M.C.; Bayome, M.; Kang, S.J.; Ham, L.K.; Lee, N.; Park, J.H.; Kook, Y. Evaluation of modified C-palatal plates on speech articulation using acoustic analysis. Orthod. Craniofacial Res. 2022, 26, 277–284. [Google Scholar] [CrossRef]
- Park, J.H.; Park, T.H.; Kook, Y.-A. A Modified C-Palatal Plate as a Skeletal Anchorage Appliance for Efficient Molar Distalization. J. Calif. Dent. Assoc. 2023, 51, 2193371. [Google Scholar] [CrossRef]
- Keski-Nisula, K.; Keski-Nisula, L.; Varrela, J. Class II treatment in early mixed dentition with the eruption guidance appliance: Effects and long-term stability. Eur. J. Orthod. 2019, 42, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Pellegrino, M.; Caruso, S.; Cantile, T.; Pellegrino, G.; Ferrazzano, G.F. Early Treatment of Anterior Crossbite with Eruption Guidance Appliance: A Case Report. Int. J. Environ. Res. Public Health 2020, 17, 3587. [Google Scholar] [CrossRef]
- Huang, S.; Chen, Y.; Chen, T.; Mallineni, S.K.; McGrath, C.; Hagg, U. Clinical effectiveness of the Eruption Guidance Appliances in treating malocclusion in the mixed dentition: A systematic review and meta-analysis. Int. J. Paediatr. Dent. 2022, 32, 843–855. [Google Scholar] [CrossRef] [PubMed]
- Dinu, S.; Buzatu, R.; Macasoi, I.; Popa, M.; Vlad, C.S.; Marcovici, I.; Pinzaru, I.; Dehelean, C.A.; Moacă, E.-A.; Barbu-Tudoran, L.; et al. Toxicological Profile of Biological Environment of Two Elastodontic Devices. Processes 2021, 9, 2116. [Google Scholar] [CrossRef]
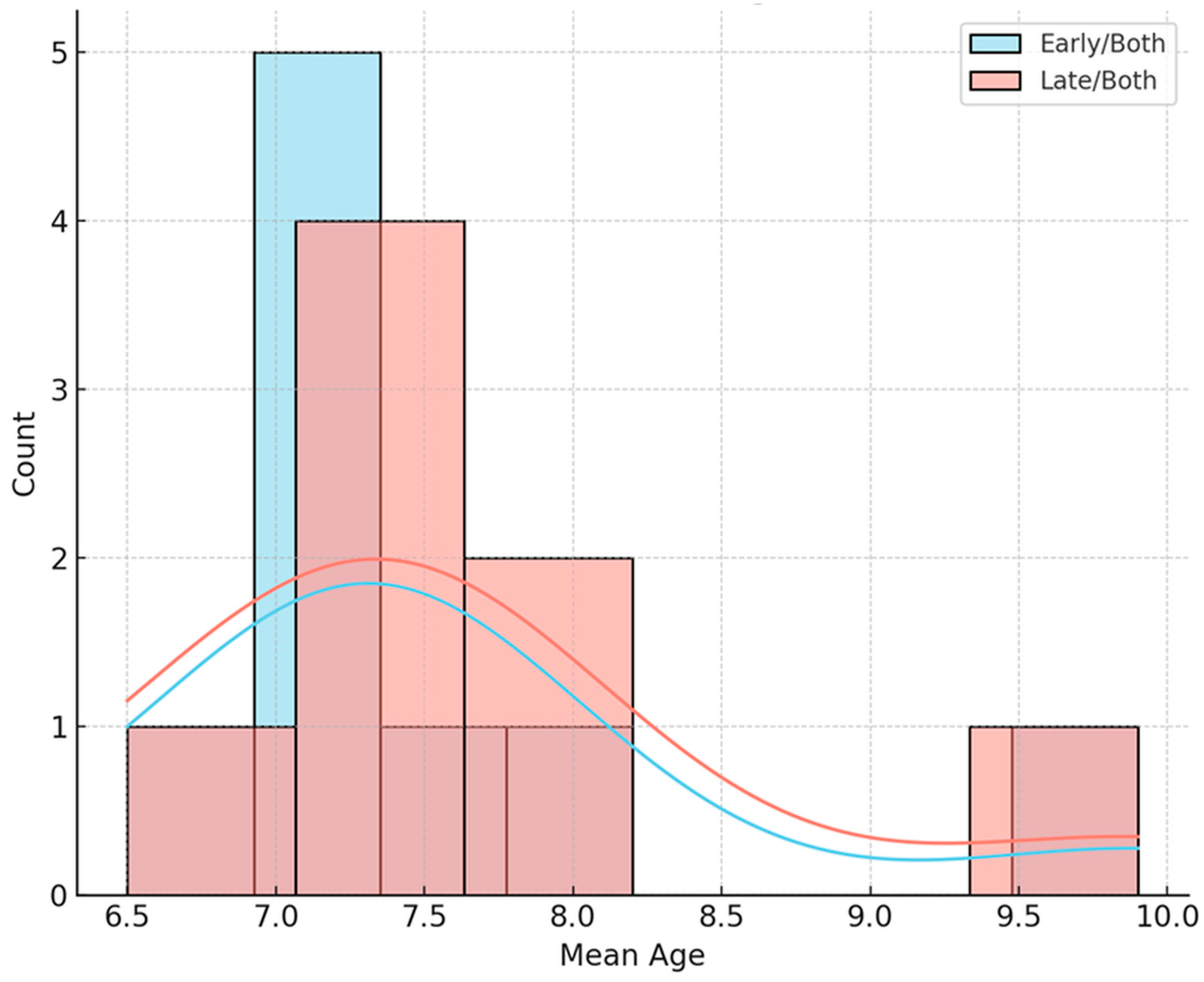
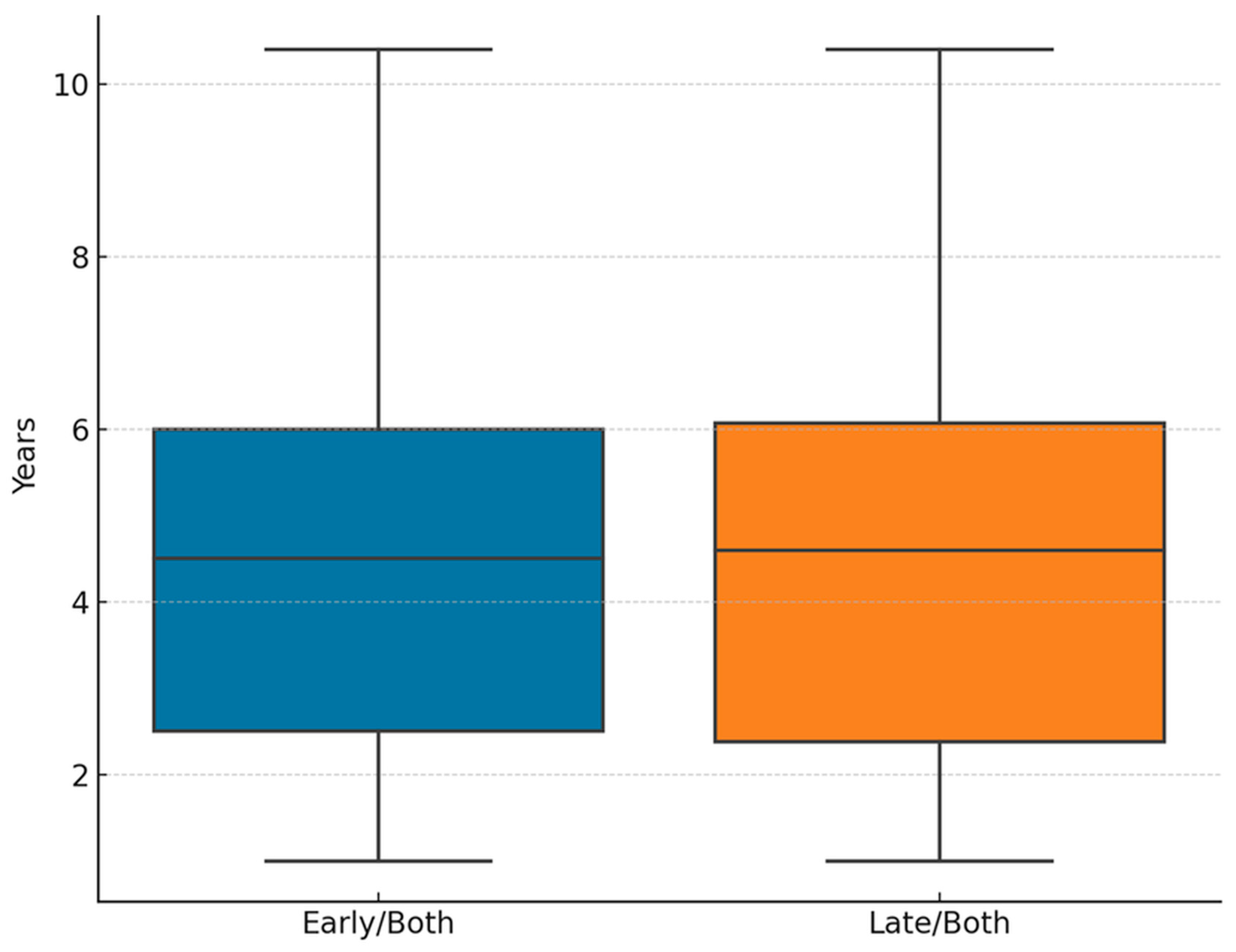
| Variable | Early/Both Mean ± SD | Late/Both Mean ± SD | t/U Value | p-Value | Interpretation |
|---|---|---|---|---|---|
| Mean age at treatment start (years) | 9.43 ± 1.21 | 9.51 ± 1.34 | t = −0.10 | 0.920 | No significant difference |
| Mean follow-up duration (years) | 4.34 ± 2.76 | 4.36 ± 2.45 | t = −0.01 | 0.990 | Comparable observation length |
| Composite success score | 2.75 ± 0.46 | 2.33 ± 0.58 | U = 17.0 | 0.270 | Not statistically significant |
| Treatment complexity (single vs. mixed) | — | — | r = 0.31 | — | Small to moderate effect favoring single-modality |
| Study | Parameter(s) with Significant Difference | Direction of Effect | p-Value | Effect Size/ Magnitude | Favored Group |
|---|---|---|---|---|---|
| Julku et al., 2019 [10] | N-ANS, gonial angle | ↓ gonial angle, ↑ facial height | 0.010 | — | Early |
| Julku et al., 2018 [11] | Airway (rl1–rl2), SNA | ↑ airway, ↓ SNA | 0.001–0.012 | — | Early |
| Käsmä et al., 2025 [12] | Eruption timing, molar overlap | Better alignment | <0.050 | — | Late |
| Kim et al., 2024 [14] | SN–GoGn, FMA | Improved vertical control | <0.010 | Moderate | Early |
| Hannula et al., 2023 [16] | Intermolar/intercanine width | ↑ maxillary width | 0.001–0.048 | — | Early |
| Mandall et al., 2022 [15] | ANB, overjet | Reduction in both | <0.001 | Large | Early |
| Männchen et al., 2022 [17] | Extraction rate, FFA use | ↓ extractions, ↓ FFA needs | <0.050 | — | Early |
| Fourneron et al., 2020 [18] | Corpus asymmetry (ΔL) | +1.0 mm correction | 0.008 | — | Early |
| Kallunki et al., 2022 [13] | Cost, trauma incidence | n.s. | 0.200 | — | None |
| Myrlund et al., 2018 [19] | Overjet, overbite, crowding | All improved | <0.050 | — | Early |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dinu, S.; Igna, A.; Petrescu, E.L.; Braila, E.B.; Dinu, D.C.; Horhat, R.M.; Mihai, C.; Traila, I.-A.; Nica, D.F.; Popa, M. Timing of Orthodontic Intervention for Pediatric Class II Malocclusion: A Systematic Review on Early vs. Late Treatment Outcomes. Children 2025, 12, 1533. https://doi.org/10.3390/children12111533
Dinu S, Igna A, Petrescu EL, Braila EB, Dinu DC, Horhat RM, Mihai C, Traila I-A, Nica DF, Popa M. Timing of Orthodontic Intervention for Pediatric Class II Malocclusion: A Systematic Review on Early vs. Late Treatment Outcomes. Children. 2025; 12(11):1533. https://doi.org/10.3390/children12111533
Chicago/Turabian StyleDinu, Stefania, Andreea Igna, Emanuela Lidia Petrescu, Emilia Brandusa Braila, Dorin Cristian Dinu, Razvan Mihai Horhat, Cristina Mihai, Iuliana-Anamaria Traila, Diana Florina Nica, and Malina Popa. 2025. "Timing of Orthodontic Intervention for Pediatric Class II Malocclusion: A Systematic Review on Early vs. Late Treatment Outcomes" Children 12, no. 11: 1533. https://doi.org/10.3390/children12111533
APA StyleDinu, S., Igna, A., Petrescu, E. L., Braila, E. B., Dinu, D. C., Horhat, R. M., Mihai, C., Traila, I.-A., Nica, D. F., & Popa, M. (2025). Timing of Orthodontic Intervention for Pediatric Class II Malocclusion: A Systematic Review on Early vs. Late Treatment Outcomes. Children, 12(11), 1533. https://doi.org/10.3390/children12111533








