Testicular Torsion in Inguinal Cryptorchidism: Report on Two Patients and Literature Review
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
6. Future Prospects
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| UT | Undescended testis |
| TT | Testicular torsion |
| CT | Computerized tomography |
| MRI | Magnetic resonance imaging |
References
- Dupond-Athénor, A.; Peycelon, M.; Abbo, O.; Rod, J.; Haraux, E.; Scalabre, A.; Arnaud, A.; Guérin, F.; Irtan, S. A multicenter review of undescended testis torsion: A plea for early management. J. Pediatr. Urol. 2021, 17, e1–e191. [Google Scholar] [CrossRef] [PubMed]
- European Association of Urology. Guidelines; Edn presented at the EAU Annual Congress, Paris 2024; European Association of Urology: Arnhem, The Netherlands, 2024. [Google Scholar]
- Zhao, L.C.; Lautz, T.B.; Meeks, J.J.; Maizels, M. Pediatric testicular torsion epidemiology using a national database: Incidence, risk of orchiectomy and possible measures toward improving the quality of care. J. Urol. 2011, 186, 2009–2013. [Google Scholar] [CrossRef]
- Zvizdic, Z.; Jonuzi, A.; Glamoclija, U.; Zvizdic, D.; Vranic, S. Clinical characteristics and outcome of children with acute cryptorchid testicular torsion: A single-center, retrospective case series study. Am. J. Emerg. Med. 2024, 82, 4–7. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Andrade, K.; Smith, S.; Goodarzian, F. An infant 300 with an ectopic torsed testis in the abdominal wall. Emerg. Radiol. 2014, 21, 223–225. [Google Scholar] [CrossRef] [PubMed]
- Candocia, F.J.; Sack-Solomon, K. An infant with testicular torsion in the inguinal canal. Pediatr. Radiol. 2003, 33, 722–724. [Google Scholar] [CrossRef] [PubMed]
- Deng, T.; Zhang, X.; Wang, G.; Duan, S.; Fu, M.; Zhong, J.; Li, J.; Jiang, X. Children with Cryptorchidism Complicated by Testicular Torsion: A Case Series. Urol. Int. 2019, 102, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, F.F.; Talati, I.; Krill, A. Intravaginal torsion of undescended testes. BMJ Case Rep. 2019, 12, e231244. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Komarowska, M.D.; Pawelczyk, A.; Matuszczak, E.; Dębek, W.; Hermanowicz, A. Is Testicular Torsion a Real Problem in Pediatric Patients with Cryptorchidism? Front. Pediatr. 2021, 8, 575741. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Lio, K.; Nomura, O.; Kinumaki, A.; Aoki, Y.; Satoh, H.; Sakakibara, H.; Hataya, H. Testicular Torsion in an Infant with Undescended Testis. J. Pediatr. 2018, 197, 312–312.e1. [Google Scholar] [CrossRef]
- Pogorelić, Z.; Mrklić, I.; Jurić, I.; Biočić, M.; Furlan, D. Testicular torsion in the inguinal canal in children. J. Pediatr. Urol. 2013, 9, 793–797. [Google Scholar] [CrossRef] [PubMed]
- Erdoğan, A.; Günay, E.C.; Gündoğdu, G.; Avlan, D. Testicular torsion in the left inguinal canal in a patient with inguinal hernia: A difficult case to diagnose. Mol. Imaging Radionucl. Ther. 2011, 20, 108–110. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Naouar, S.; Braiek, S.; El Kamel, R. Testicular torsion in undescended testis: A persistent challenge. Asian J. Urol. 2017, 4, 111–115. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Kargl, S.; Haid, B. Torsion of an undescended testis—A surgical pediatric emergency. J. Pediatr. Surg. 2020, 55, 660–664. [Google Scholar] [CrossRef] [PubMed]
- Stoykov, B.; Kolev, N.; Dunev, V.; Genov, P. Torsion of the testis 334 with perineal ectopy. Urol. Case Rep. 2019, 29, 101087. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shayegani, H.; Divband, G.; Tavakkoli, M.; Banihasan, M.; Sadeghi, R. Torsion of the undescended testis detected by 99mTc testicular scintigraphy: A case report. Nucl. Med. Rev. Cent. East. Eur. 2016, 19, 24–25. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Knight, R.M.; Cuenca, P.J. Torsion of undescended testis in a 14-month-old child refusing to bear weight. West. J. Emerg. Med. 2011, 12, 515–519. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mowad, J.J.; Konvolinka, C.W. Torsion of undescended testis. Urology 1978, 12, 567–568. [Google Scholar] [CrossRef] [PubMed]
- Singal, A.K.; Jain, V.; Dubey, M.; Deshpande, P. Undescended testis and torsion: Is the risk understated? Arch. Dis. Child. 2013, 98, 77–79. [Google Scholar] [CrossRef] [PubMed]
- Şener, N.C.; Bas, O.; Karakoyunlu, N.; Ercil, H.; Yesil, S.; Zengin, K.; Imamoglu, A. A rare emergency: Testicular torsion in the inguinal canal. Biomed. Res. Int. 2015, 2015, 320780. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Yang, M.; Wen, S.; Lin, T.; Liu, X.; Zhang, D.Y.; Liu, F.; Wu, S.D.; Wei, G.H.; He, P.R.; Hua, Y. Diagnosis, treatment, outcome, and reasons for delayed treatment of cryptorchidism with torsion in children: A 16-year retrospective study in a large pediatric medical center. Asian J. Androl. 2022, 24, 386–389. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Mäkelä, E.; Lahdes-Vasama, T.; Rajakorpi, H.; Wikström, S. A 19-year review of paediatric patients with acute scrotum. Scand. J. Surg. 2007, 96, 62–66. [Google Scholar] [CrossRef] [PubMed]
- Zilberman, D.; Inbar, Y.; Heyman, Z.; Shinhar, D.; Bilik, R.; Avigad, I.; Jonas, P.; Ramon, J.; Mor, Y. Torsion of the cryptorchid testis—Can it be salvaged? J. Urol. 2006, 175, 2287–2289, discussion 2289. [Google Scholar] [CrossRef] [PubMed]
- Tryfonas, G.; Violaki, A.; Tsikopoulos, G.; Avtzoglou, P.; Zioutis, J.; Limas, C.; Gregoriadis, G.; Badouraki, M. Late postoperative results in males treated for testicular torsion during childhood. J. Pediatr. Surg. 1994, 29, 553–556. [Google Scholar] [CrossRef] [PubMed]
- Revzin, M.V.; Ersahin, D.; Israel, G.M.; Kirsch, J.D.; Mathur, M.; Bokhari, J.; Scoutt, L.M. US of the Inguinal Canal: Comprehensive Review of Pathologic Processes with CT and MR Imaging Correlation. Radiographics 2016, 36, 2028–2048. [Google Scholar] [CrossRef] [PubMed]
- Elder, J.S. Surgical Management of the Undescended Testis: Recent Advances and Controversies. Eur. J. Pediatr. Surg. 2016, 26, 418–426. [Google Scholar] [CrossRef] [PubMed]
- Pensabene, M.; Sergio, M.; Baldanza, F.; Grasso, F.; Serra, G.; Spataro, B.; Bonfiglio, R.; Patti, M.; Maggiore, V.; Cambiaso, C.; et al. Penile Length Assessment of Children Treated for Primary Buried Penis: Can Satisfying Penile Growth Always Be Achieved? Children 2023, 10, 1254. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Serra, G.; Cimador, M.; Giuffrè, M.; Insinga, V.; Montante, C.; Pensabene, M.; Piro, E.; Salerno, S.; Schierz, I.A.M.; Corsello, G. Report and follow-up on two new patients with congenital mesoblastic nephroma. Ital. J. Pediatr. 2023, 49, 124. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pensabene, M.; Di Pace, M.R.; Baldanza, F.; Grasso, F.; Patti, M.; Sergio, M.; La Placa, S.; Giuffre’, M.; Serra, G.; Casuccio, A.; et al. Quality of life improving after propranolol treatment in patients with Infantile Hemangiomas. Ital. J. Pediatr. 2022, 48, 140. [Google Scholar] [CrossRef]
- Serra, G.; Giuffrè, M.; Piro, E.; Corsello, G. The social role of pediatrics in the past and present times. Ital. J. Pediatr. 2021, 47, 239. [Google Scholar] [CrossRef]
- Serra, G.; Giambrone, C.; Antona, V.; Cardella, F.; Carta, M.; Cimador, M.; Corsello, G.; Giuffrè, M.; Insinga, V.; Maggio, M.C.; et al. Congenital hypopituitarism and multiple midline defects in a newborn with non-familial CatEye syndrome. Ital. J. Pediatr. 2022, 48, 170. [Google Scholar] [CrossRef] [PubMed]
- Batra, N.V.; DeMarco, R.T.; Bayne, C.E. A narrative review of the history and evidence-base for the timing of orchiopexy for cryptorchidism. J. Pediatr. Urol. 2021, 17, 239–245. [Google Scholar] [CrossRef] [PubMed]

| Author | Age (Months) | Side | Onset | Symptoms | Treatment |
|---|---|---|---|---|---|
| Zvizdic et al. [4] | 2 | L | 4 h | Restlessness, decreased intake, and inguinal swelling | Orchiopexy |
| 5 | L | 60 h | Restlessness, inguinal swelling, and pain | Orchiectomy | |
| Andrade et al. [6] | 6 | R | 24 h | Vomiting and inconsolable crying | Orchiectomy |
| Candocia et al. [7] | 7 | L | 5 h | Inguinal swelling, inconsolable crying | Orchiectomy |
| Deng et al. [8] | 4 | L | 24 h | Abdominal pain, inguinal swelling, and inconsolable crying | Orchiectomy |
| 10 | L | 18 h | Pain, vomiting, and inguinal swelling | Orchiectomy | |
| Carvalho et al. [9] | 5 | L | 24 h | Inguinal swelling | Orchiectomy |
| Komarowska et al. [10] | 6 | L | 96 h | Pain, fever, and inguinal swelling | Orchiectomy |
| Lio K. et al. [11] | 4 | R | 48 h | Restlessness, inguinal swelling, and fever | Orchiectomy |
| Pogorelic et al. [12] | 12 | L | 36 h | Inguinal swelling, pain, and inconsolable crying | Orchiectomy |
| Erdogan et al. [13] | 8 | L | 10 h | Inguinal swelling and inconsolable crying | Orchiectomy |
| Naouar et al. [14] | 12 | R | 3 h | Inguinal swelling and inconsolable crying | Orchiopexy |
| Kargl et al. [15] | 9 | R | 48 h | Vomiting and inguinal swelling | Orchiectomy |
| 11 | R | 8 h | Inguinal swelling and restlessness | Orchiectomy | |
| 7 | L | 24 h | Inguinal swelling and pain | Orchiectomy | |
| 9 | R | 12 h | Inguinal swelling and pain | Orchiopexy | |
| 12 | L | 24 h | Inguinal swelling and pain | Orchiectomy | |
| 4 | L | 6 h | Inguinal swelling and pain | Orchiopexy | |
| 6 | L | 12 h | Inguinal swelling and pain | Orchiectomy | |
| 1 | R | 16 h | Inguinal swelling | Orchiectomy | |
| 11 | L | 12 h | Restlessness and inguinal swelling | Orchiectomy | |
| 12 | R | 6 h | Asymptomatic | Orchiopexy | |
| Stoykov et al. [16] | 18 | L | 6 h | Perineal swelling | Orchiopexy |
| Shayegani et al. [17] | 9 | L | 13 h | Inconsolable crying | Orchiopexy |
| Knight et al. [18] | 14 | L | 12 h | Refusing to bear weight | Orchiectomy |
| Mowad et al. [19] | 5 | L | 48 h | Inguinal swelling | Orchiectomy |
| Singal et al. [20] | 4 | L | 48 h | Inguinal swelling and inconsolable crying | Orchiectomy |
| 4 | L | 48 h | Inguinal swelling | Orchiectomy | |
| 5 | L | 36 h | Inguinal swelling | Orchiectomy | |
| 11 | R | 48 h | Inguinal swelling | Orchiectomy | |
| 10 | L | 36 h | Inguinal swelling | Orchiectomy | |
| Sener et al. [21] | 16 | R | 7 h | Inconsolable crying, inguinal swelling, and pain | Orchiopexy |
| 15 | L | 11 h | Inconsolable crying, inguinal swelling, and pain | Orchiectomy | |
| 18 | L | 22 h | Inconsolable crying, inguinal swelling, and pain | Orchiectomy | |
| 16 | L | 8 h | Inconsolable crying, inguinal swelling, and pain | Orchiopexy | |
| 8 | R | 4 h | Inconsolable crying, inguinal swelling, and pain | Orchiopexy | |
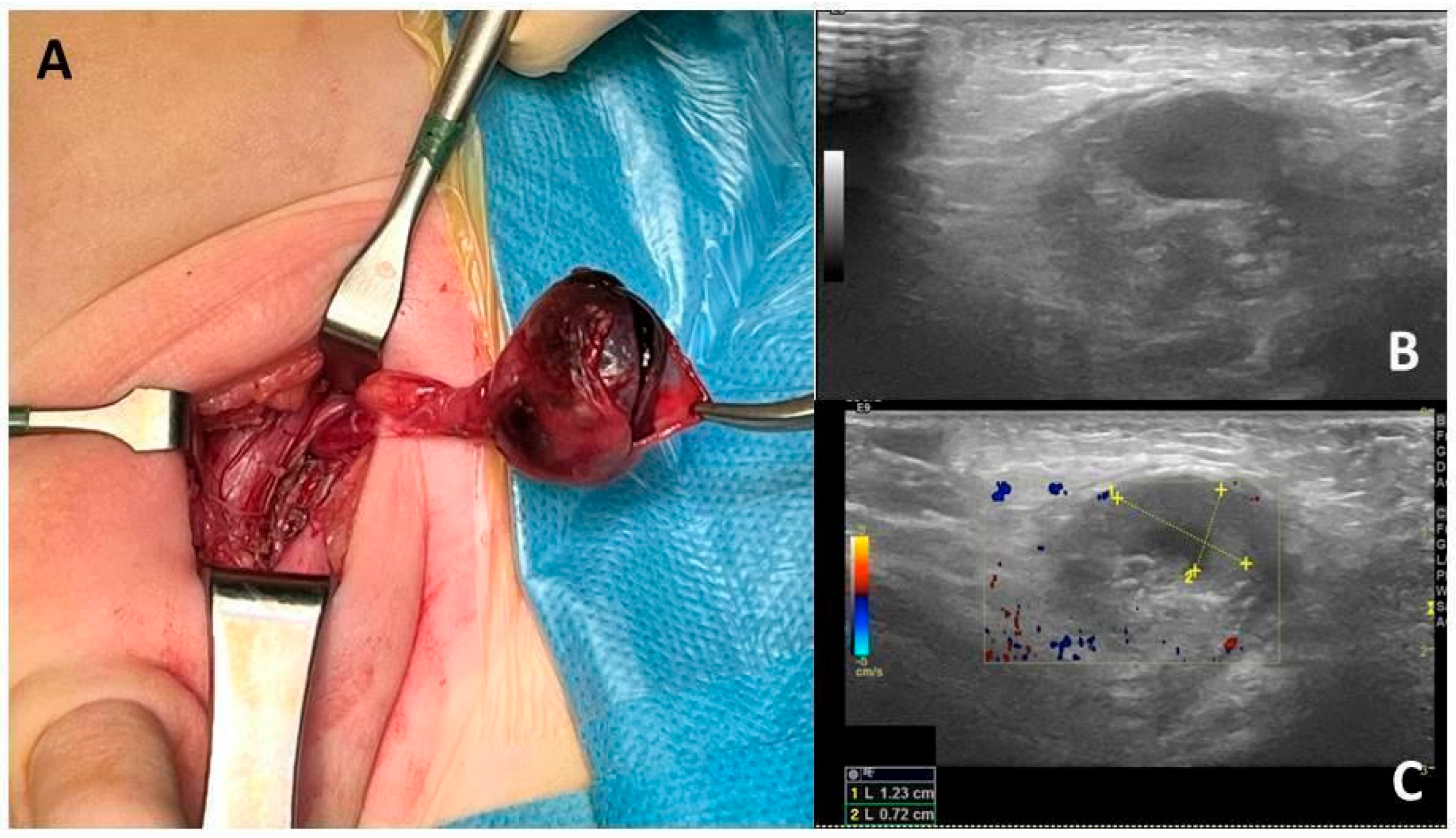
| Baldanza et al. | 10 | L | 36 h | Inconsolable crying, inguinal swelling, and pain | Orchiectomy |
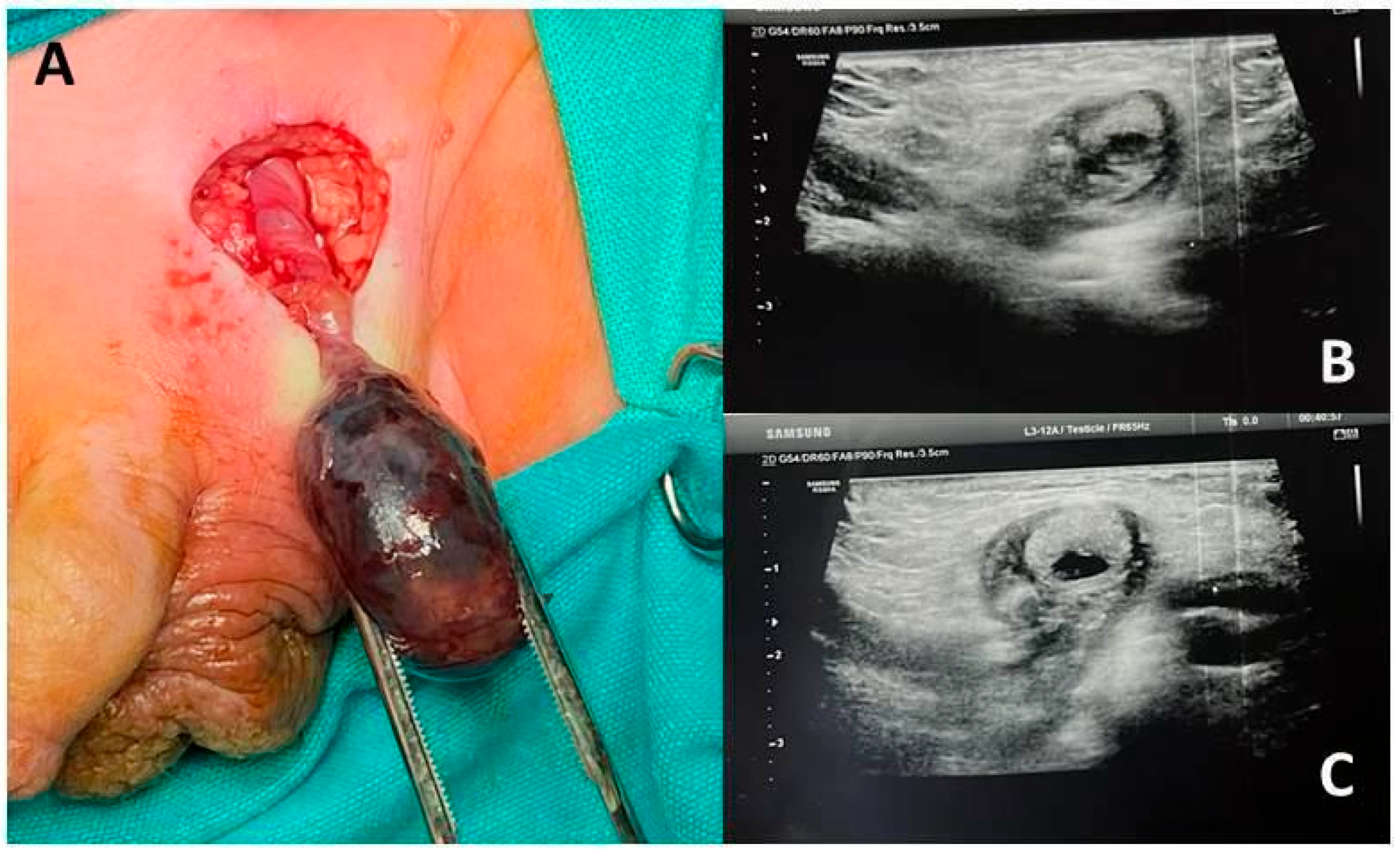
| 7 | L | 36 h | Inconsolable crying, inguinal swelling, and pain | Orchiectomy |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baldanza, F.; Grasso, F.; Sergio, M.; Patti, M.; Maggiore, V.; Serra, G.; Giuffré, M.; Corsello, G.; Di Pace, M.R.; Pensabene, M. Testicular Torsion in Inguinal Cryptorchidism: Report on Two Patients and Literature Review. Children 2025, 12, 1531. https://doi.org/10.3390/children12111531
Baldanza F, Grasso F, Sergio M, Patti M, Maggiore V, Serra G, Giuffré M, Corsello G, Di Pace MR, Pensabene M. Testicular Torsion in Inguinal Cryptorchidism: Report on Two Patients and Literature Review. Children. 2025; 12(11):1531. https://doi.org/10.3390/children12111531
Chicago/Turabian StyleBaldanza, Fabio, Francesco Grasso, Maria Sergio, Maria Patti, Valentina Maggiore, Gregorio Serra, Mario Giuffré, Giovanni Corsello, Maria Rita Di Pace, and Marco Pensabene. 2025. "Testicular Torsion in Inguinal Cryptorchidism: Report on Two Patients and Literature Review" Children 12, no. 11: 1531. https://doi.org/10.3390/children12111531
APA StyleBaldanza, F., Grasso, F., Sergio, M., Patti, M., Maggiore, V., Serra, G., Giuffré, M., Corsello, G., Di Pace, M. R., & Pensabene, M. (2025). Testicular Torsion in Inguinal Cryptorchidism: Report on Two Patients and Literature Review. Children, 12(11), 1531. https://doi.org/10.3390/children12111531







