Optimal Duration of Umbilical Cord Clamping with Ventilation in a Preterm Asphyxiated Ovine Model
Highlights
- Delayed umbilical cord clamping with ventilation (DCCV) for 5 min significantly increased the proportion of preterm asphyxiated lambs achieving heart rate ≥ 100 bpm and oxygen saturation ≥80% within 5 min of resuscitation.
- DCCV for 5 min also improved pulmonary blood flow and gas exchange compared to shorter DCCV durations and early cord clamping with ventilation (ECCV).
- Initiating ventilation while maintaining an intact umbilical cord for 5 min may facilitate a smoother cardiopulmonary transition in preterm neonates.
- These findings highlight the potential physiological benefits of prolonged DCCV and warrant further validation in clinical studies.
Abstract
1. Introduction
2. Materials and Methods
Data Collection and Statistical Analysis
3. Results
- (i)
- Primary Composite Outcome
- (a)
- Incidence of achieving combined heart rate (HR) ≥ 100 bpm and preductal saturation (SpO2) ≥ 80% by 5 min: (Table 2)All lambs in DCCV5 (100%) achieved the primary composite outcome of a heart rate (HR) of ≥100 bpm and a preductal oxygen saturation (SpO2) level of ≥80% by 5 min. In ECCV and DCCV2, only 20% of lambs achieved this primary composite outcome, while DCCV1 and DCCV4 saw 16% success in attaining the criteria. DCCV3 had 33% of lambs meeting the composite outcome of HR ≥ 100 bpm and preductal SpO2 ≥ 80% by 5 min.
- (b)
- Time taken to achieve combined heart rate (HR) ≥ 100 bpm & preductal saturation (SpO2) ≥ 80% by 5 min: (Table 2)The time taken to achieve the primary outcome was significantly lower in DCCV5 (5 ± 1 min) compared to DCCV1 (13 ± 6 min) (p = 0.02—post hoc, ANOVA). With ECCV, it took 8 ± 3 min, DCCV2 required 10 ± 4 min, while DCCV3 took 11 ± 5 min. DCCV4 attained the primary outcome in 8 ± 2 min.
- (ii)
- Secondary outcomes: Gas exchange and hemodynamics
- (a)
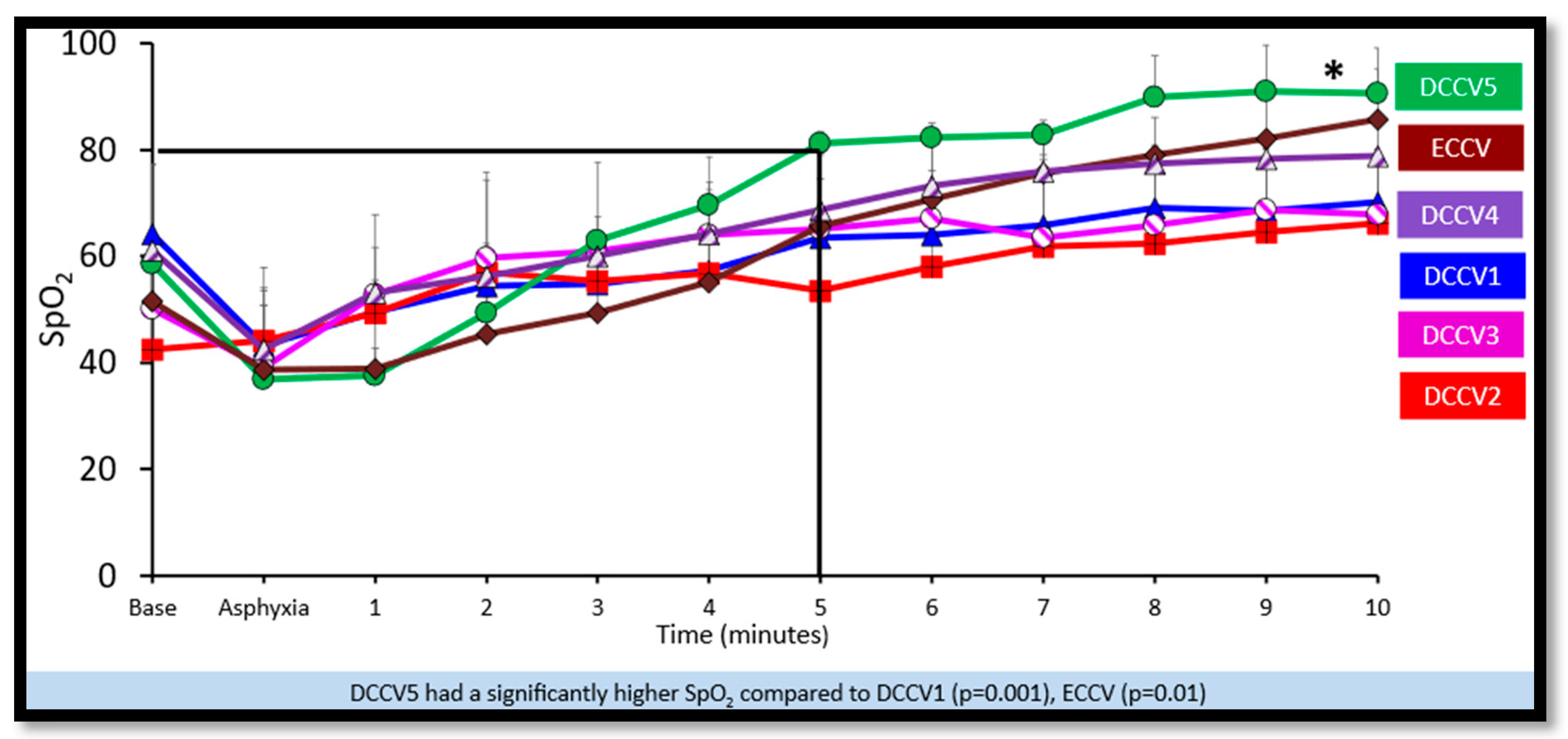
- Preductal saturations: As shown in Figure 3, DCCV5 had significantly higher preductal saturations compared to DCCV1, DCCV3 and ECCV. DCCV5 attained a preductal saturation of 80% in 5 min.
- (b)
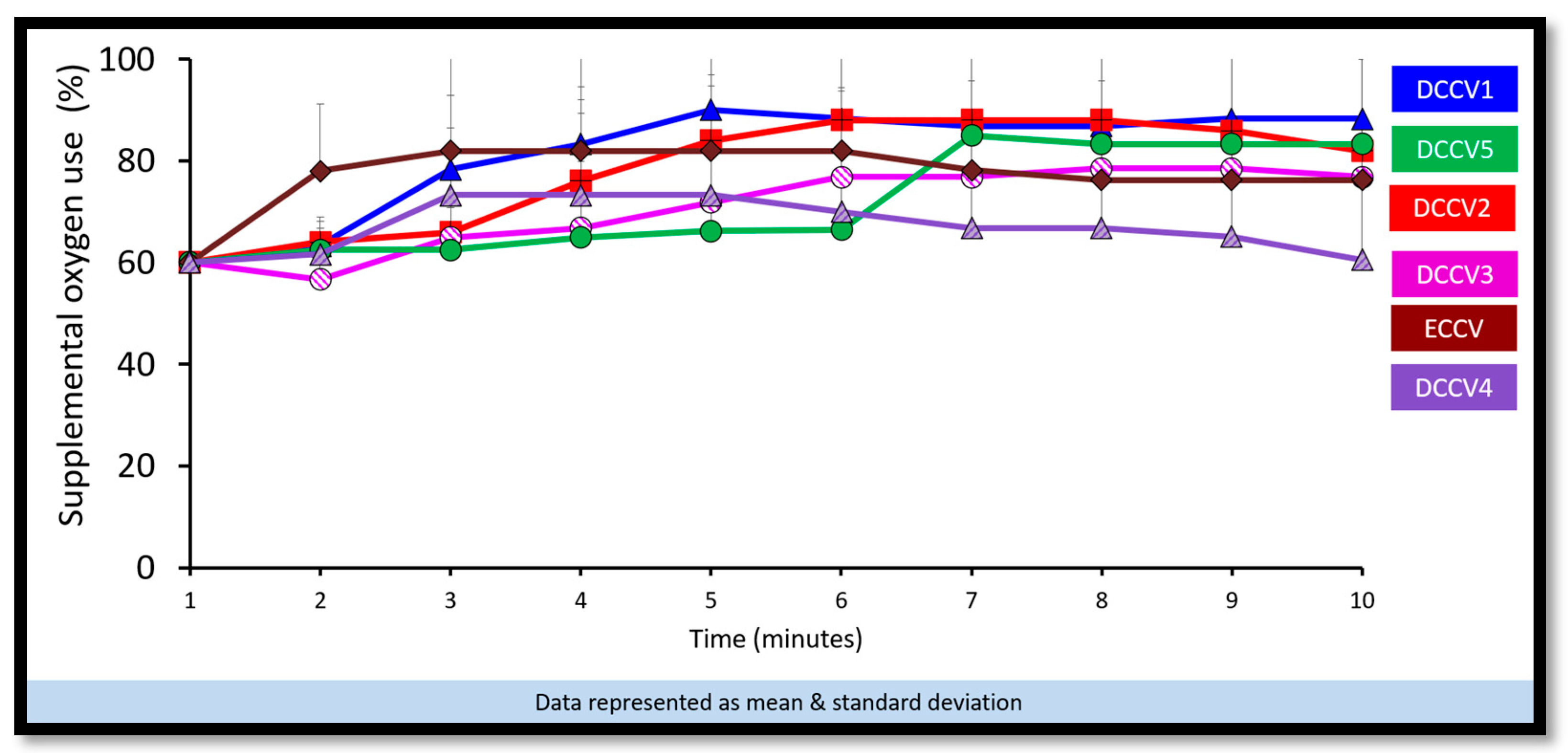
- Supplemental oxygen use: The supplemental oxygen used during the first ten minutes is shown in Figure 4. An initial supplemental oxygen of 60% was used in all groups in our study. There was no statistical difference between the groups’ supplemental O2 exposure. Oxygen was titrated according to the NRP recommended preductal saturation targets.
- (c)
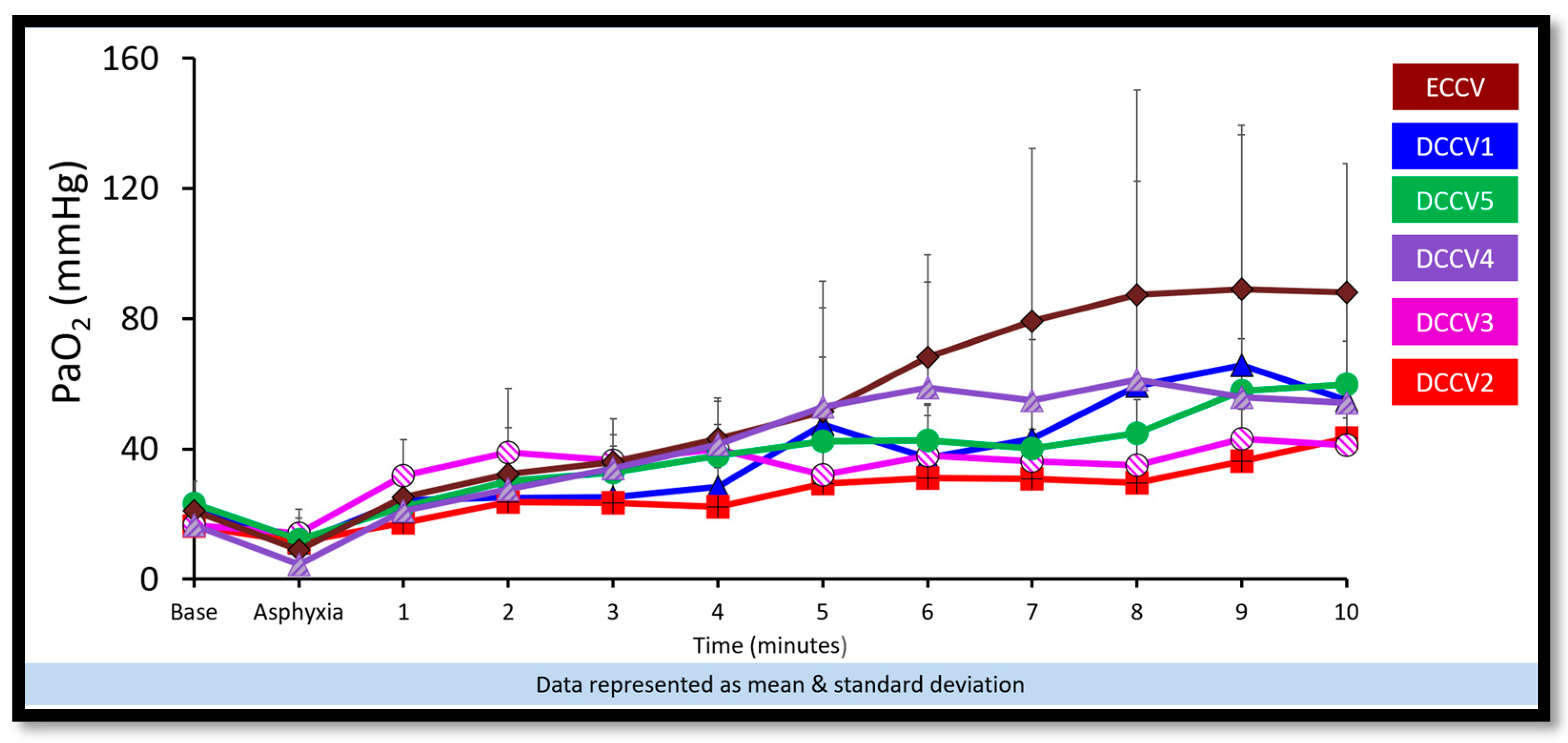
- Partial pressure of oxygen in arterial blood (PaO2): Figure 5 shows the partial pressure of oxygen in arterial blood in the first ten minutes. There was no statistical difference in PaO2 between the groups. Despite starting at a higher supplemental oxygen level of 60% in all the groups, none of the groups exceeded mean PaO2 values of 100 mmHg within the initial ten minutes while weaning FiO2 per NRP recommendations.
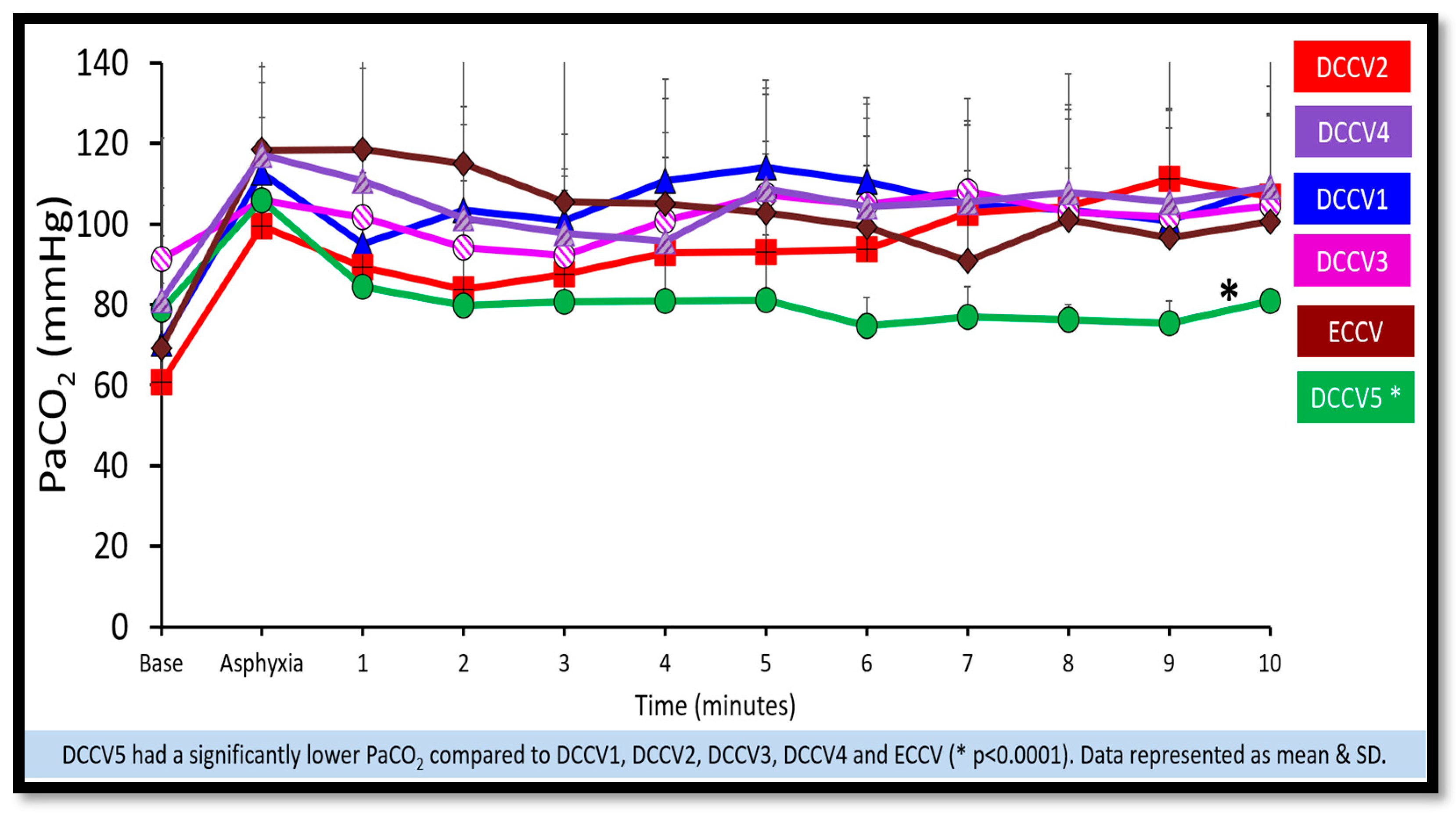
- (d)
- Partial pressure of carbon dioxide in arterial blood (PaCO2): DCCV5 had significantly lower carbon dioxide in arterial blood (PaCO2) compared to other groups (p = 0.0001) as shown in Figure 6.
- (iii)
- Hemodynamics:
- (a)
- Pulmonary blood flow: The peak pulmonary blood flow in the first ten minutes is shown in Figure 7. DCCV4 and DCCV5 had a significantly higher peak pulmonary blood flow compared to ECCV and DCCV1 (p < 0.0001). The pulmonary blood flow was lowest in the ECCV group.
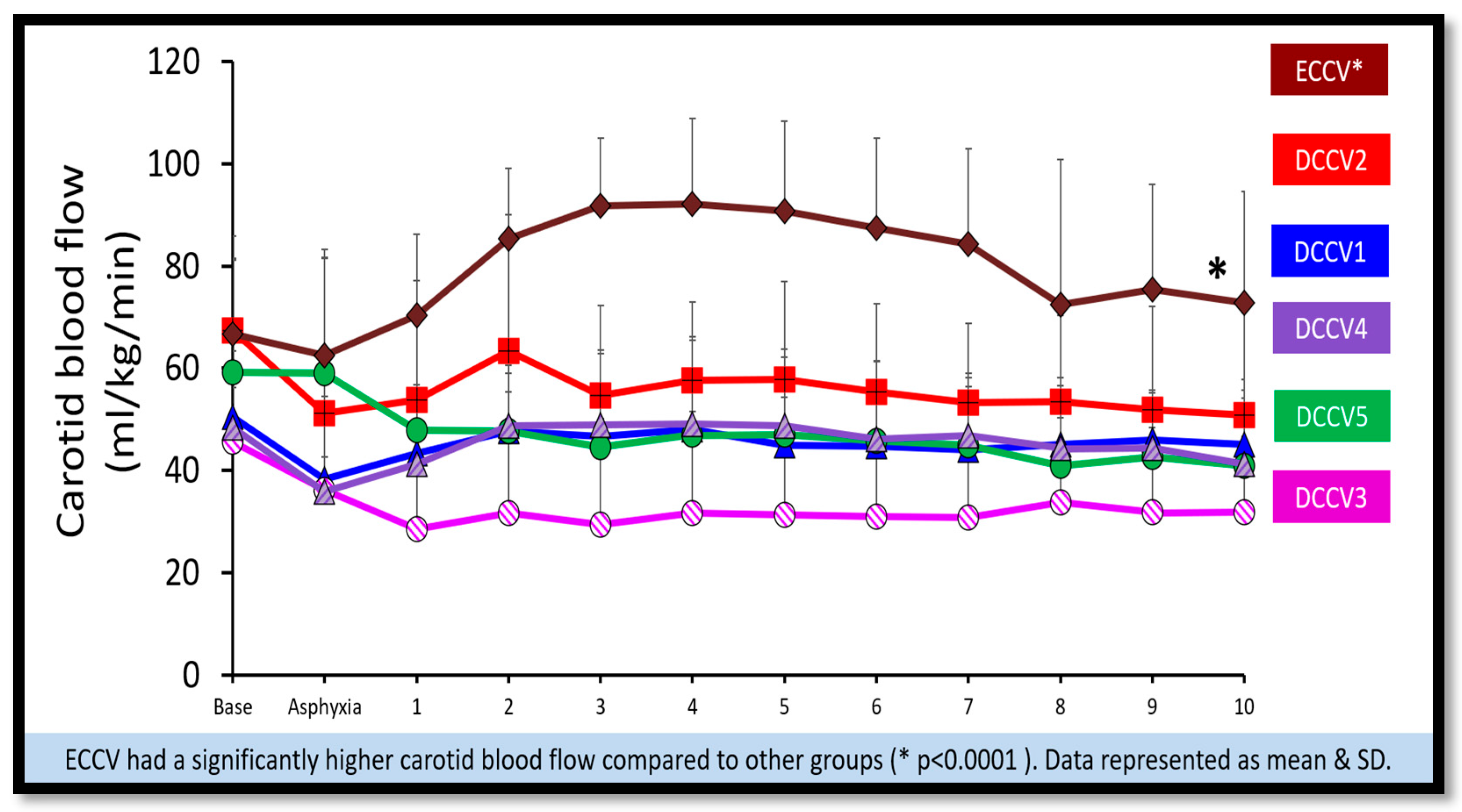
- (b)
- Carotid blood flow: The peak carotid blood flow during the first ten minutes is shown in Figure 8. The highest peak carotid blood flow was seen in the ECCV group and was statistically different (p = < 0.0001) compared to other groups.
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AAP-NRP | American Academy of Pediatrics Neonatal Resuscitation Program |
| ACOG | American College of Obstetricians and Gynecologists |
| DCC | Delayed cord clamping |
| DCCV | Delayed cord clamping with ventilation |
| ECC | Early cord clamping |
| ECCV | Early cord clamping with ventilation |
| ECG | Electrocardiogram |
| ETT | Endotracheal tube |
| ETCO2 | End- tidal Carbon dioxide |
| FiO2 | Fraction of inspired oxygen |
| IACUC | Institutional Animal Care and Use Committee |
| PPV | Positive pressure ventilation |
| PaCO2 | Partial pressure of carbon dioxide in arterial blood |
| PaO2 | Partial pressure of oxygen in arterial blood |
| NRP | Neonatal Resuscitation Program |
| SpO2 | Preductal oxygen saturation |
| WHO | World Health Organization |
References
- Ohuma, E.O.; Moller, A.B.; Bradley, E.; Chakwera, S.; Hussain-Alkhateeb, L.; Lewin, A.; Okwaraji, Y.B.; Mahanani, W.R.; Johansson, E.W.; Lavin, T.; et al. National, regional, and global estimates of preterm birth in 2020, with trends from 2010: A systematic analysis. Lancet 2023, 402, 1261–1271, Erratum in Lancet 2024, 403, 618. https://doi.org/10.1016/S0140-6736(24)00267-8. [Google Scholar] [CrossRef] [PubMed]
- Aziz, K.; Lee, H.C.; Escobedo, M.B.; Hoover, A.V.; Kamath-Rayne, B.D.; Kapadia, V.S.; Magid, D.J.; Niermeyer, S.; Schmölzer, G.M.; Szyld, E.; et al. Part 5: Neonatal Resuscitation: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142 (Suppl. 2), S524–S550. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists. Committee Opinion No. 684: Delayed Umbilical Cord Clamping After Birth. Obstet. Gynecol. 2017, 129, e5–e10. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guidelines on Basic Newborn Resuscitation; WHO: Geneva, Switzerland, 2012. [Google Scholar]
- Yamada, N.K.; Szyld, E.; Strand, M.L.; Finan, E.; Illuzzi, J.L.; Kamath-Rayne, B.D.; Kapadia, V.S.; Niermeyer, S.; Schmölzer, G.M.; Williams, A.; et al. 2023 American Heart Association and American Academy of Pediatrics Focused Update on Neonatal Resuscitation: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics 2024, 153, e2023065030. [Google Scholar] [CrossRef] [PubMed]
- Wyckoff, M.H.; Aziz, K.; Escobedo, M.B.; Kapadia, V.S.; Kattwinkel, J.; Perlman, J.M.; Simon, W.M.; Weiner, G.M.; Zaichkin, J.G. Part 13: Neonatal Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015, 132 (Suppl. 2), S543–S560. [Google Scholar] [CrossRef] [PubMed]
- Fogarty, M.; Osborn, D.A.; Askie, L.; Seidler, A.L.; Hunter, K.; Lui, K.; Simes, J.; Tarnow-Mordi, W. Delayed vs early umbilical cord clamping for preterm infants: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. 2018, 218, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Rabe, H.; Diaz-Rossello, J.L.; Duley, L.; Dowswell, T. Effect of timing of umbilical cord clamping and other strategies to influence placental transfusion at preterm birth on maternal and infant outcomes. Cochrane Database Syst. Rev. 2012, CD003248, Erratum in Cochrane Database Syst. Rev. 2019, 9, CD003248. https://doi.org/10.1002/14651858.CD003248.pub4. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, S.; Polglase, G.R.; Wallace, E.M.; Te Pas, A.B.; Hooper, S.B. Ventilation before Umbilical Cord Clamping Improves the Physiological Transition at Birth. Front. Pediatr. 2014, 2, 113. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chandrasekharan, P.; Gugino, S.; Koenigsknecht, C.; Helman, J.; Nielsen, L.; Bradley, N.; Nair, J.; Sankaran, D.; Bawa, M.; Rawat, M.; et al. Placental transfusion during neonatal resuscitation in an asphyxiated preterm model. Pediatr. Res. 2022, 92, 678–684. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Nevill, E.; Meyer, M.P. Effect of delayed cord clamping (DCC) on breathing and transition at birth in very preterm infants. Early Hum. Dev. 2015, 91, 407–411. [Google Scholar] [CrossRef] [PubMed]
- Seidler, A.L.; Libesman, S.; Hunter, K.E.; Barba, A.; Aberoumand, M.; Williams, J.G.; Shrestha, N.; Aagerup, J.; Sotiropoulos, J.X.; Montgomery, A.A.; et al. Short, medium, and long deferral of umbilical cord clamping compared with umbilical cord milking and immediate clamping at preterm birth: A systematic review and network meta-analysis with individual participant data. Lancet 2023, 402, 2223–2234, Erratum in Lancet 2023, 402, 2196. https://doi.org/10.1016/S0140-6736(23)02710-1. [Google Scholar] [CrossRef] [PubMed]
- Kilkenny, C.; Browne, W.J.; Cuthill, I.C.; Emerson, M.; Altman, D.G. Improving bioscience research reporting: The ARRIVE guidelines for reporting animal research. PLoS Biol. 2010, 8, e1000412. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chandrasekharan, P.; Gugino, S.; Helman, J.; Koenigsknecht, C.; Nielsen, L.; Bradley, N.; Nair, J.; Agrawal, V.; Bawa, M.; Mari, A.; et al. Resuscitation with an Intact Cord Enhances Pulmonary Vasodilation and Ventilation with Reduction in Systemic Oxygen Exposure and Oxygen Load in an Asphyxiated Preterm Ovine Model. Children 2021, 8, 307. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Seidler, A.L.; Aberoumand, M.; Hunter, K.E.; Barba, A.; Libesman, S.; Williams, J.G.; Shrestha, N.; Aagerup, J.; Sotiropoulos, J.X.; Montgomery, A.A.; et al. Deferred cord clamping, cord milking, and immediate cord clamping at preterm birth: A systematic review and individual participant data meta-analysis. Lancet 2023, 402, 2209–2222. [Google Scholar] [CrossRef] [PubMed]
- Liyanage, S.K.; Ninan, K.; McDonald, S.D. Guidelines on Deferred Cord Clamping and Cord Milking: A Systematic Review. Pediatrics 2020, 146, e20201429. [Google Scholar] [CrossRef] [PubMed]
- Aldemerdash, M.A.; Abdellatif, M.; Refaey, D.; AbuSammour, Y.; Refaey, M.; Janem, A.M.; Hasan, M.T.; Aldemerdash, A.; Shihab, H.; Hamouda, N. Comparing Umbilical Cord Management Strategies in Nonvigorous Newborns: A Systematic Review and Network Meta-analysis. Am. J. Perinatol. 2025. [Google Scholar] [CrossRef] [PubMed]
- Polglase, G.R.; Dawson, J.A.; Kluckow, M.; Gill, A.W.; Davis, P.G.; Te Pas, A.B.; Crossley, K.J.; McDougall, A.; Wallace, E.M.; Hooper, S.B. Ventilation onset prior to umbilical cord clamping (physiological-based cord clamping) improves systemic and cerebral oxygenation in preterm lambs. PLoS ONE 2015, 10, e0117504. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Padilla-Sánchez, C.; Baixauli-Alacreu, S.; Cañada-Martínez, A.J.; Solaz-García, Á.; Alemany-Anchel, M.J.; Vento, M. Delayed vs Immediate Cord Clamping Changes Oxygen Saturation and Heart Rate Patterns in the First Minutes after Birth. J. Pediatr. 2020, 227, 149–156.e1. [Google Scholar] [CrossRef] [PubMed]
- Andersson, O.; Rana, N.; Ewald, U.; Målqvist, M.; Stripple, G.; Basnet, O.; Subedi, K.; Ashish, K.C. Intact cord resuscitation versus early cord clamping in the treatment of depressed newborn infants during the first 10 minutes of birth (Nepcord III)—A randomized clinical trial. Matern. Health Neonatol. Perinatol. 2019, 5, 15. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Major, G.S.; Unger, V.; Nagy, R.; Hernádfői, M.; Veres, D.S.; Zolcsák, Á.; Szabó, M.; Garami, M.; Hegyi, P.; Varga, P.; et al. Umbilical cord management in newborn resuscitation: A systematic review and meta-analysis. Pediatr. Res. 2025, 97, 1481–1491. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Wyckoff, M.H.; Wyllie, J.; Aziz, K.; de Almeida, M.F.; Fabres, J.; Fawke, J.; Guinsburg, R.; Hosono, S.; Isayama, T.; Kapadia, V.S.; et al. Neonatal Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2020, 142 (Suppl. 1), S185–S221. [Google Scholar] [CrossRef] [PubMed]
- Oei, J.L.; Finer, N.N.; Saugstad, O.D.; Wright, I.M.; Rabi, Y.; Tarnow-Mordi, W.; Rich, W.; Kapadia, V.; Rook, D.; Smyth, J.P.; et al. Outcomes of oxygen saturation targeting during delivery room stabilisation of preterm infants. Arch. Dis. Child. Fetal Neonatal. Ed. 2018, 103, F446–F454. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dekker, J.; Martherus, T.; Lopriore, E.; Giera, M.; McGillick, E.V.; Hutten, J.; van Leuteren, R.W.; van Kaam, A.H.; Hooper, S.B.; Te Pas, A.B. The Effect of Initial High vs. Low FiO2 on Breathing Effort in Preterm Infants at Birth: A Randomized Controlled Trial. Front Pediatr. 2019, 7, 504. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Sotiropoulos, J.X.; Oei, J.L.; Schmölzer, G.M.; Libesman, S.; Hunter, K.E.; Williams, J.G.; Webster, A.C.; Vento, M.; Kapadia, V.; Rabi, Y.; et al. Initial Oxygen Concentration for the Resuscitation of Infants Born at Less Than 32 Weeks’ Gestation: A Systematic Review and Individual Participant Data Network Meta-Analysis. JAMA Pediatr. 2024, 178, 774–783. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Knol, R.; Brouwer, E.; van den Akker, T.; DeKoninck, P.L.J.; Onland, W.; Vermeulen, M.J.; de Boode, W.P.; van Kaam, A.H.; Lopriore, E.; Reiss, I.K.M.; et al. Physiological versus time based cord clamping in very preterm infants (ABC3): A parallel-group, multicentre, randomised, controlled superiority trial. Lancet Reg. Health Eur. 2024, 48, 101146. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pratesi, S.; Ciarcià, M.; Boni, L.; Ghirardello, S.; Germini, C.; Troiani, S.; Tulli, E.; Natile, M.; Ancora, G.; Barone, G.; et al. Resuscitation With Placental Circulation Intact Compared With Cord Milking: A Randomized Clinical Trial. JAMA Netw. Open 2024, 7, e2450476. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Fairchild, K.D.; Petroni, G.R.; Varhegyi, N.E.; Strand, M.L.; Josephsen, J.B.; Niermeyer, S.; Barry, J.S.; Warren, J.B.; Rincon, M.; Fang, J.L.; et al. Ventilatory Assistance Before Umbilical Cord Clamping in Extremely Preterm Infants: A Randomized Clinical Trial. JAMA Netw. Open 2024, 7, e2411140. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Katheria, A.C.; Ines, F.; Lee, H.C.; Sollinger, C.; Vali, P.; Morales, A.; Sanjay, S.; Dorner, R.; Koo, J.; Gollin, Y.; et al. Deferred Cord Clamping With High Oxygen in Extremely Preterm Infants: A Randomized Clinical Trial. JAMA Pediatr. 2025, 179, 971–978. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bawa, M.; Gugino, S.; Helman, J.; Nielsen, L.; Bradley, N.; Mani, S.; Prasath, A.; Blanco, C.; Mari, A.; Nair, J.; et al. Initial Use of 100% but Not 60% or 30% Oxygen Achieved a Target Heart Rate of 100 bpm and Preductal Saturations of 80% Faster in a Bradycardic Preterm Model. Children 2022, 9, 1750. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]


| Characteristic | ECCV (N-5) |
DCCV1 (N-6) | DCCV2 (N-5) | DCCV3 (N-6) | DCCV4 (N-6) | DCCV5 (N-4) |
|---|---|---|---|---|---|---|
| Gestational age (days) | 128 ± 0.84 | 126 ± 0.47 | 126 ± 0.97 | 126 ± 1.5 | 126 ± 0.47 | 127 ± 0.52 |
| Female (N) | 3 | 5 | 2 | 3 | 3 | 4 |
| Birth weight (kg) | 3.3 ± 0.70 | 2.9 ± 0.35 | 2.9 ± 0.42 | 3.0 ± 0.30 | 3.16 ± 0.45 | 3.3 ± 0.63 |
| Heart rate at asphyxia (bpm) | 86 ± 10 | 80 ± 9 | 87 ± 2 | 86 ± 4 | 85 ± 13 | 88 ± 8 |
| pH before resuscitation | 6.91 ± 0.04 | 6.98 ± 0.07 | 7.07 ± 0.07 | 7.00 ± 0.09 | 6.96 ± 0.08 | 6.98 ± 0.06 |
| PaCO2 before resuscitation (mmHg) | 119 ± 31 | 113 ± 22 | 100 ± 2 | 106 ± 21 | 117 ± 22 | 106 ± 11 |
| PaO2 before resuscitation (mmHg) | 9 ± 6 | 11 ± 6 | 12 ± 6 | 14 ± 5 | 8 ± 3 | 12 ± 9 |
| Parameter | Control (ECCV) (N-5) | STUDY (DCCV) | ||||
|---|---|---|---|---|---|---|
| DCCV1 (N-6) | DCCV2 (N-5) | DCCV3 (N-6) | DCCV4 (N-6) | DCCV5 * (N-4) | ||
| Combined HR ≥ 100 bpm & preductal SpO2 ≥ 80% by 5 min N (%) | 1/5 (20%) | 1/6 (16%) | 1/5 (20%) | 2/6 (33%) | 1/6 (16%) | 4/4 (100%) |
| Time to achieve primary outcome (minutes) | 8 ± 3 | 13 ± 6 | 10 ± 4 | 11 ± 5 | 8 ± 2 | 5 ± 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bawa, M.; Gugino, S.; Helman, J.; Bradley, N.; Nielsen, L.; Prasath, A.; Blanco, C.; Kasu, M.D.; Abbasi, H.; Rawat, M.; et al. Optimal Duration of Umbilical Cord Clamping with Ventilation in a Preterm Asphyxiated Ovine Model. Children 2025, 12, 1462. https://doi.org/10.3390/children12111462
Bawa M, Gugino S, Helman J, Bradley N, Nielsen L, Prasath A, Blanco C, Kasu MD, Abbasi H, Rawat M, et al. Optimal Duration of Umbilical Cord Clamping with Ventilation in a Preterm Asphyxiated Ovine Model. Children. 2025; 12(11):1462. https://doi.org/10.3390/children12111462
Chicago/Turabian StyleBawa, Mausma, Sylvia Gugino, Justin Helman, Nicole Bradley, Lori Nielsen, Arun Prasath, Clariss Blanco, Mary Divya Kasu, Hamza Abbasi, Munmun Rawat, and et al. 2025. "Optimal Duration of Umbilical Cord Clamping with Ventilation in a Preterm Asphyxiated Ovine Model" Children 12, no. 11: 1462. https://doi.org/10.3390/children12111462
APA StyleBawa, M., Gugino, S., Helman, J., Bradley, N., Nielsen, L., Prasath, A., Blanco, C., Kasu, M. D., Abbasi, H., Rawat, M., & Chandrasekharan, P. (2025). Optimal Duration of Umbilical Cord Clamping with Ventilation in a Preterm Asphyxiated Ovine Model. Children, 12(11), 1462. https://doi.org/10.3390/children12111462







