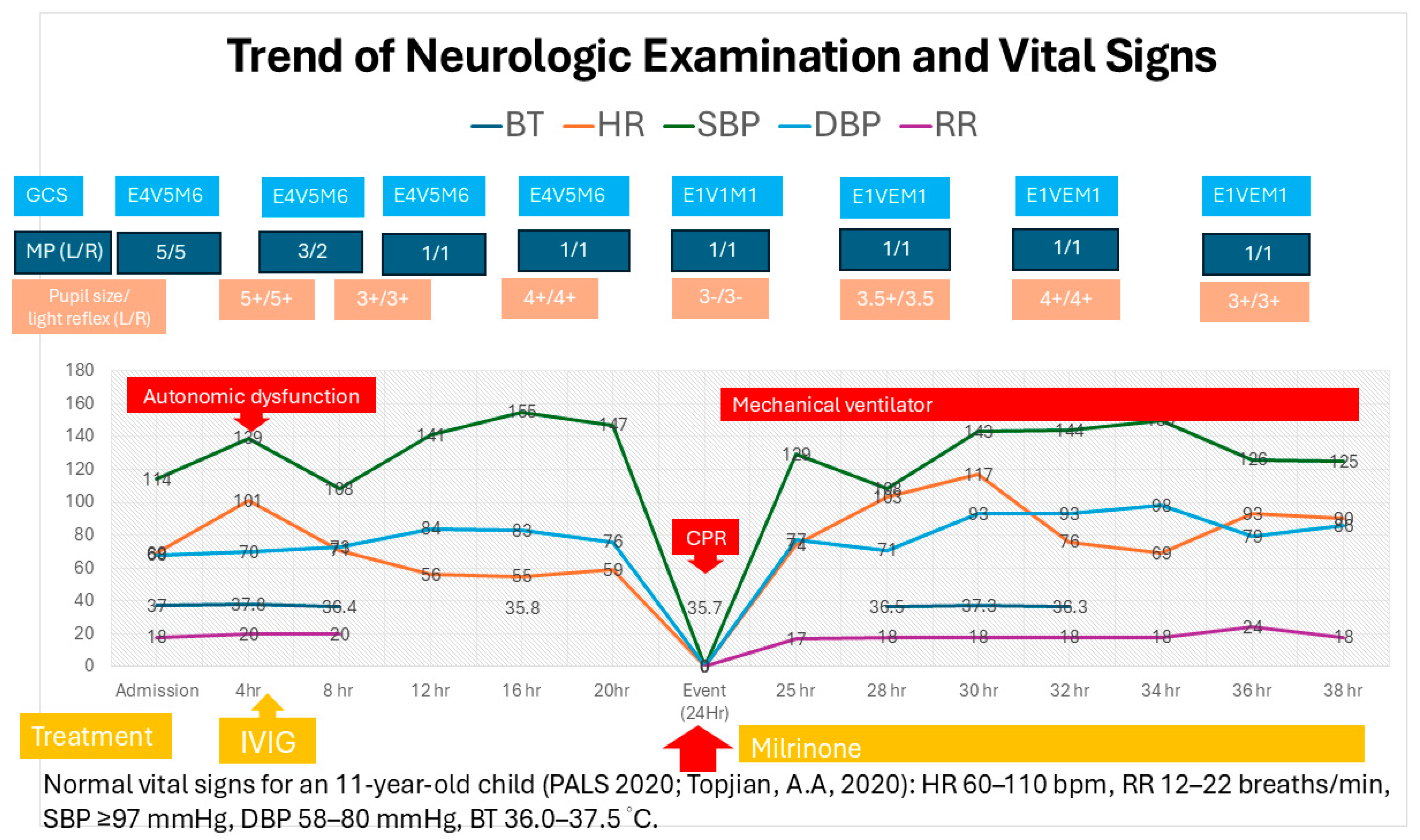
Pediatric Cardiac Arrest Secondary to Guillain-Barré Syndrome-Induced Dysautonomia
Abstract
Highlights
- Pediatric Guillain-Barré Syndrome (GBS) can progress rapidly to life-threatening dysautonomia.
- Early cardiac arrest due to autonomic dysfunction may occur even in initially mild cases.
- Vigilant monitoring for autonomic instability is critical in pediatric GBS.
- Early recognition and timely intervention can improve outcomes.
Abstract
1. Introduction
2. Case Presentation
3. Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lin, J.J.; Hsia, S.H.; Wang, H.S.; Lyu, R.K.; Chou, M.L.; Hung, P.C.; Hsieh, M.-Y.; Lin, K.-L. Clinical variants of Guillain-Barré syndrome in children. Pediatr. Neurol. 2012, 47, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Leonhard, S.E.; Mandarakas, M.R.; Gondim, F.A.A.; Bateman, K.; Ferreira, M.L.B.; Cornblath, D.R.; van Doorn, P.A.; Dourado, M.E.; Hughes, R.A.C.; Islam, B.; et al. Diagnosis and management of Guillain-Barré syndrome in ten steps. Nat. Rev. Neurol. 2019, 15, 671–683. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Shen, D.; Li, T.; Zhang, B.; Li, C.; Mao, M.; Zhao, J.; Liu, K.; Zhang, H.-L. Distinct Clinical Characteristics of Pediatric Guillain-Barré Syndrome: A Comparative Study between Children and Adults in Northeast China. PLoS ONE 2016, 11, e0151611. [Google Scholar] [CrossRef] [PubMed]
- Dimario, F.J., Jr.; Edwards, C. Autonomic dysfunction in childhood Guillain-Barré syndrome. J. Child Neurol. 2012, 27, 581–586. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, T.; Kramer, C.L.; Wijdicks, E.F.M.; Rabinstein, A.A. Dysautonomia in Guillain-Barré Syndrome: Prevalence, Clinical Spectrum, and Outcomes. Neurocrit. Care 2020, 32, 113–120. [Google Scholar] [PubMed]
- Fryman, E.; Saleem, S.; Singh, A. Guillain-Barré Syndrome Induced Dysautonomia Resulting in Cardiac Arrest. Cureus 2020, 12, e12149. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.Y.; Li, X.J.; Cheng, M.; Wang, J.; Xie, L.L.; Yao, Z.X.; Jiang, L. Clinical characteristics of children with Guillain-Barré syndrome and factors associated with disease severity. J. Clin. Neurosci. 2021, 92, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, G.; Schiller, B.; Kruse, J.; Netzer, J. Indicators of dysautonomia in severe Guillain-Barré syndrome. J. Neurol. 1999, 246, 1015–1022. [Google Scholar] [CrossRef] [PubMed]
- Mukerji, S.; Aloka, F.; Farooq, M.U.; Kassab, M.Y.; Abela, G.S. Cardiovascular complications of the Guillain-Barré syndrome. Am. J. Cardiol. 2009, 104, 1452–1455. [Google Scholar] [CrossRef] [PubMed]
- Topjian, A.A.; Raymond, T.T.; Atkins, D.; Chan, M.; Duff, J.P.; Joyner, B.L.; Lasa, J.J.; Lavonas, E.J.; Levy, A.; Mahgoub, M.; et al. Part 4: Pediatric Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142 (Suppl. 2), S469–S523. [Google Scholar] [CrossRef] [PubMed]
- Fehmi, J.; Davies, A.J.; Walters, J.; Lavin, T.; Keh, R.; Rossor, A.M.; Munteanu, T.; Delanty, N.; Roberts, R.; Bäumer, D.; et al. IgG1 pan-neurofascin antibodies identify a severe yet treatable neuropathy with a high mortality. J. Neurol. Neurosurg. Psychiatry 2021, 92, 1089–1095. [Google Scholar] [CrossRef] [PubMed]
- Doppler, K.; Appeltshauser, L.; Villmann, C.; Martin, C.; Peles, E.; Krämer, H.H.; Haarmann, A.; Buttmann, M.; Sommer, C. Auto-antibodies to contactin-associated protein 1 (Caspr) in two patients with painful inflammatory neuropathy. Brain 2016, 139, 2617–2630. [Google Scholar] [CrossRef] [PubMed]
- Nakane, S.; Higuchi, O.; Koga, M.; Kanda, T.; Murata, K.; Suzuki, T.; Kurono, H.; Kunimoto, M.; Kaida, K.; Mukaino, A.; et al. Clinical features of autoimmune autonomic ganglionopathy and the detection of subunit-specific autoantibodies to the ganglionic acetylcholine receptor in Japanese patients. PLoS ONE 2015, 10, e0118312. [Google Scholar] [CrossRef] [PubMed]
- Imamura, M.; Mukaino, A.; Takamatsu, K.; Tsuboi, H.; Higuchi, O.; Nakamura, H.; Abe, S.; Ando, Y.; Matsuo, H.; Nakamura, T.; et al. Ganglionic Acetylcholine Receptor Antibodies and Autonomic Dysfunction in Autoimmune Rheumatic Diseases. Int. J. Mol. Sci. 2020, 21, 1332. [Google Scholar] [CrossRef] [PubMed]
- Zaeem, Z.; Siddiqi, Z.A.; Zochodne, D.W. Autonomic involvement in Guillain-Barré syndrome: An update. Clin Auton Res. 2019, 218, 289–299. [Google Scholar] [CrossRef] [PubMed]
- Pinto, V.L.; Adeyinka, A. Increased Intracranial Pressure. StatPearls, Updated 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK482119/ (accessed on 23 August 2025).
- Shen, M.J.; Zipes, D.P. Role of the Autonomic Nervous System in Modulating Cardiac Electrophysiology, Arrhythmogenesis, and Sudden Cardiac Death. Circ. Res. 2014, 114, 1004–1021. [Google Scholar] [CrossRef] [PubMed]
- Fedele, L.; Brand, T. The Intrinsic Cardiac Nervous System and Its Role in Cardiac Pacemaking and Conduction. J. Cardiovasc. Dev. Dis. 2020, 7, 54. [Google Scholar] [CrossRef] [PubMed]
- Morgan, R.W.; Kirschen, M.P.; Kilbaugh, T.J.; Sutton, R.M.; Topjian, A.A. Pediatric In-Hospital Cardiac Arrest and Cardiopulmonary Resuscitation in the United States: A Review. JAMA Pediatr. 2021, 175, 293–302. [Google Scholar] [CrossRef] [PubMed]
- Chevret, S.; Hughes, R.A.C.; Annane, D. Plasma exchange for Guillain-Barré syndrome. Cochrane Database Syst. Rev. 2017, 2, CD001798. [Google Scholar] [CrossRef] [PubMed]
| Examination Findings | |
| Examination | Finding |
| Physical examination | Right eye ptosis with progressive limb weakness |
| Brain MRI | No evidence of brainstem involvement |
| CSF analysis | Albuminocytologic dissociation (protein: 310 mg/dL; WBC: 9/mm3) |
| Electrophysiological studies (NCV) | Severe demyelinating polyneuropathy with secondary axonal involvement |
| Anti-ganglioside antibodies | Negative |
| Intervention Responses | |
| Intervention | Response |
| IVIG | No response |
| Plasmapheresis | Gradual improvement |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, P.-J.; Cheng, Y.-T.; Hsia, S.-H.; Chan, O.-W.; Lee, E.-P.; Lin, K.-L.; Lin, J.-J. Pediatric Cardiac Arrest Secondary to Guillain-Barré Syndrome-Induced Dysautonomia. Children 2025, 12, 1379. https://doi.org/10.3390/children12101379
Chen P-J, Cheng Y-T, Hsia S-H, Chan O-W, Lee E-P, Lin K-L, Lin J-J. Pediatric Cardiac Arrest Secondary to Guillain-Barré Syndrome-Induced Dysautonomia. Children. 2025; 12(10):1379. https://doi.org/10.3390/children12101379
Chicago/Turabian StyleChen, Po-Jung, Yi-Ting Cheng, Shao-Hsuan Hsia, Oi-Wa Chan, En-Pei Lee, Kuang-Lin Lin, and Jainn-Jim Lin. 2025. "Pediatric Cardiac Arrest Secondary to Guillain-Barré Syndrome-Induced Dysautonomia" Children 12, no. 10: 1379. https://doi.org/10.3390/children12101379
APA StyleChen, P.-J., Cheng, Y.-T., Hsia, S.-H., Chan, O.-W., Lee, E.-P., Lin, K.-L., & Lin, J.-J. (2025). Pediatric Cardiac Arrest Secondary to Guillain-Barré Syndrome-Induced Dysautonomia. Children, 12(10), 1379. https://doi.org/10.3390/children12101379





