Lesson from a Single Pediatric Emergency Department: Potentially Applicable Radiation-Minimizing Practices for Non-Traumatic Abdominal Pain in Adolescents
Abstract
Highlights
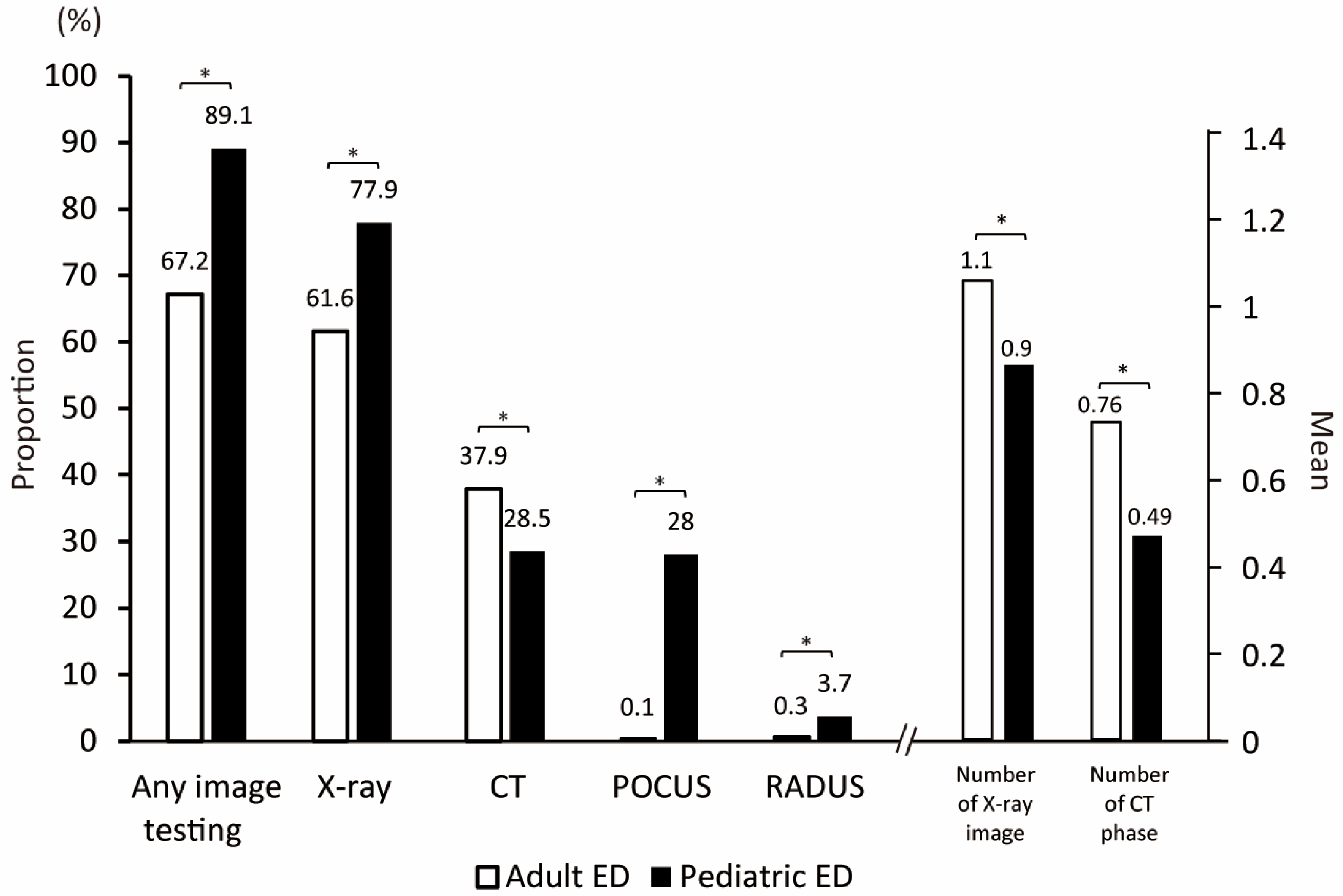
- Pediatric emergency department (PED) physicians used significantly fewer CT scans (28.5% vs. 37.9%) and fewer CT phases per patient (0.49 vs. 0.76 per patient) compared to adult ED physicians, while utilizing point-of-care ultrasound (POCUS) significantly more frequently (28.0% vs. 0.1%).
- Despite reduced radiation exposure and simplified imaging strategies (fewer CT phases and single-view X-rays), safety outcomes remained comparable between PED and AED.
- These findings support radiation-minimizing imaging practices in adolescents by highlighting the feasibility of POCUS as a frontline tool in the pediatric ED.
- Adoption of similar PED-style imaging strategies could reduce unnecessary radiation exposure in adolescents without compromising clinical outcomes.
Abstract
1. Introduction
2. Materials and Methods
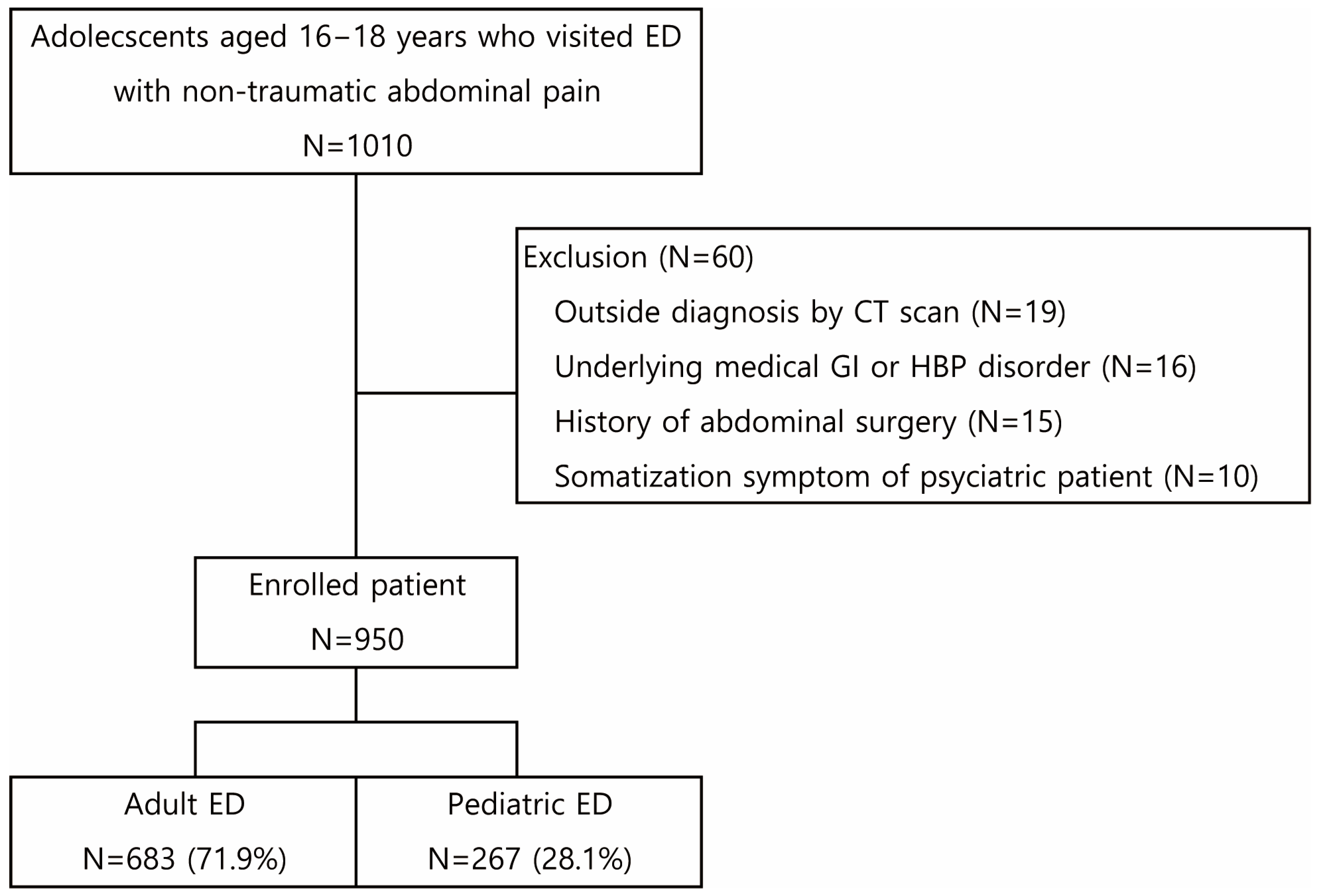
2.1. Population and Study Design
2.2. Data Collection
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ED | Emergency Department |
| PED | Pediatric ED |
| AED | Adult ED |
| CT | Computed Tomography |
| US | Ultrasound |
| POCUS | Point-Of-Care Ultrasound |
| KTAS | Korean Triage And Acuity Scale |
| CECT | Contrast-Enhanced CT |
| NECT | Non-Contrast-Enhanced CT |
| AGE | Acute Gastroenteritis |
| AJR | American Journal Of Roentgenology |
| ACR | American College Of Radiology |
| GI | Gastrointestinal |
| HBP | Hepatobiliary-Pancreas |
| RADUS | Radiologist-Performed Ultrasound |
Appendix A
| POCUS Not Performed | POCUS Performed | p-Value | ||
|---|---|---|---|---|
| N = 192 | N = 75 | |||
| Sex, male | 62 (32.3) | 25 (33.3) | 0.870 | |
| Age, year | 16 (16–17) | 16 (16–17) | 0.723 | |
| Mean (95% CI) | 16.6 (16.5–16.7) | 16.5 (16.4–16.7) | 0.638 | |
| 16 | 105 (54.7) | 41 (54.7) | NA | |
| 17 | 61 (31.8) | 28 (37.3) | ||
| 18 | 26 (13.5) | 6 (8) | ||
| Body weight, kg | 56 (49–66) | 56 (50–65) | 0.644 | |
| KTAS | ||||
| Mean (95% CI) | 2.84 (2.76–2.93) | 2.91 (2.78–3.04) | 0.079 | |
| 1 | 1 (0.5) | 1 (1.3) | NA | |
| 2 | 47 (24.5) | 14 (18.7) | ||
| 3 | 126 (65.6) | 51 (68) | ||
| 4 | 17 (8.9) | 9 (12) | ||
| 5 | 1 (0.5) | 0 (0) | ||
| Clinical manifestation | ||||
| NRS | 5 (3–7) | 4 (3–6) | 0.165 | |
| Localized tenderness | 104 (54.2) | 67 (89.3) | <0.001 | |
| Rebound tenderness | 5 (2.6) | 4 (5.3) | NA | |
| Any radiation exposure | 152 (79.2) | 58 (77.3) | 0.742 | |
| X-ray | 157 (82.6) | 51 (68) | 0.028 | |
| CT | 52 (27.1) | 24 (32) | 0.423 | |
| Disposition | ||||
| Discharge | 146 (76) | 56 (74.7) | 0.814 | |
| Need for admission | 45 (23.4) | 19 (25.3) | 0.744 | |
| Admission | 42 (21.9) | 14 (18.7) | 0.563 | |
| ICU admission | 0 (0) | 0 (0) | NA | |
| Transferred | 3 (1.6) | 5 (6.7) | 0.028 | |
| Mortality | 0 (0) | 0 (0) | NA | |
| ED LOS, min | 239 (157–451) | 223 (127–457) | 0.546 | |
| Revisit within two days | 13 (6.8) | 1 (1.3) | 0.071 | |
| Missed surgical abdomen | 1 | 0 (0) | NA | |
| Acute appendicitis | 1 | 0 (0) | NA | |
References
- Menoch, M.; Simon, H.K.; Hirsh, D.; Shim, Y.; Baxter, A.L.; Clifton, M.; Kim, D.; Sturm, J.J. Imaging for Suspected Appendicitis: Variation Between Academic and Private Practice Models. Pediatr. Emerg. Care 2017, 33, 147–151. [Google Scholar] [CrossRef]
- Blumfield, E.; Zember, J.; Guelfguat, M.; Blumfield, A.; Goldman, H. Evaluation of an initiative to reduce radiation exposure from CT to children in a non-pediatric-focused facility. Emerg. Radiol. 2015, 22, 631–641. [Google Scholar] [CrossRef]
- Park, J.S.; Byun, Y.H.; Choi, S.J.; Lee, J.S.; Ryu, J.M.; Lee, J.Y. Feasibility of Point-of-Care Ultrasound for Diagnosing Hypertrophic Pyloric Stenosis in the Emergency Department. Pediatr. Emerg. Care 2021, 37, 550–554. [Google Scholar] [CrossRef]
- Kim, J.H.; Lee, J.Y.; Kwon, J.H.; Cho, H.R.; Lee, J.S.; Ryu, J.M. Point-of-Care Ultrasound Could Streamline the Emergency Department Workflow of Clinically Nonspecific Intussusception. Pediatr. Emerg. Care 2020, 36, e90–e95. [Google Scholar] [CrossRef]
- Doniger, S.J.; Kornblith, A. Point-of-Care Ultrasound Integrated Into a Staged Diagnostic Algorithm for Pediatric Appendicitis. Pediatr. Emerg. Care 2018, 34, 109–115. [Google Scholar] [CrossRef]
- Portelli, J.L.; McNulty, J.P.; Bezzina, P.; Rainford, L. Frequency of paediatric medical imaging examinations performed at a European teaching hospital over a 7-year period. Eur. Radiol. 2016, 26, 4221–4230. [Google Scholar] [CrossRef]
- Frush, D.J.; Commander, C.W.; Hartman, T.S.; Cecil, A.K.; Handly, B.D.; Park, D.B.; Fordham, L.A. Utilization of computed tomography imaging in the pediatric emergency department. Pediatr. Radiol. 2020, 50, 470–475. [Google Scholar] [CrossRef]
- Menoch, M.J.; Hirsh, D.A.; Khan, N.S.; Simon, H.K.; Sturm, J.J. Trends in computed tomography utilization in the pediatric emergency department. Pediatrics 2012, 129, e690–e697. [Google Scholar] [CrossRef]
- Fahimi, J.; Kornblith, A.E.; Kanzaria, H.; Herring, A.; Wang, R.C. Computed Tomography Use Plateaus Among Children with Emergency Visits for Abdominal Pain. Pediatr. Emerg. Care 2019, 35, 194–198. [Google Scholar] [CrossRef]
- Wang, R.C.; Kornblith, A.E.; Grupp-Phelan, J.; Smith-Bindman, R.; Kao, L.S.; Fahimi, J. Trends in Use of Diagnostic Imaging for Abdominal Pain in U.S. Emergency Departments. AJR Am. J. Roentgenol. 2021, 216, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Chang, I.; Jung, J.Y.; Kwak, Y.H.; Kim, D.K.; Lee, J.H.; Jung, J.H.; Kwon, H.; Paek, S.H.; Park, J.W. Long-term changes in computed tomography and ultrasound utilization in a pediatric emergency department. Clin. Exp. Emerg. Med. 2018, 5, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Niles, L.M.; Goyal, M.K.; Badolato, G.M.; Chamberlain, J.M.; Cohen, J.S. US Emergency Department Trends in Imaging for Pediatric Nontraumatic Abdominal Pain. Pediatrics 2017, 140, e20170615. [Google Scholar] [CrossRef]
- Hwang, S.; Chung, H.J.; Park, J.W.; Lee, E.J.; Lee, H.N.; Kim, J.H.; Jue, J.H.; Choi, Y.H.; Jung, J.Y. Factors contributing to uncertainty in paediatric abdominal ultrasound reports in the paediatric emergency department. BMC Emerg. Med. 2023, 23, 120. [Google Scholar] [CrossRef]
- Abo, A.; Shannon, M.; Taylor, G.; Bachur, R. The influence of body mass index on the accuracy of ultrasound and computed tomography in diagnosing appendicitis in children. Pediatr. Emerg. Care 2011, 27, 731–736. [Google Scholar] [CrossRef]
- Murata, A.; Okamoto, K.; Mayumi, T.; Maramatsu, K.; Matsuda, S. Age-related differences in outcomes and etiologies of acute abdominal pain based on a national administrative database. Tohoku J. Exp. Med. 2014, 233, 9–15. [Google Scholar] [CrossRef]
- Kim, S.K.; Jung, J.H.; Lee, J.H.; Jung, J.Y.; Kwon, H.; Paek, S.H.; Kwak, Y.H.; Kim, D.K. The difference of Use of CT in the general versus pediatric emergency departments for adolescent patients in the same tertiary hospital. Clin. Exp. Emerg. Med. 2019, 6, 19–24. [Google Scholar] [CrossRef]
- Park, J.; Lim, T. Korean Triage and Acuity Scale (KTAS). J. Korean Soc. Emerg. Med. 2017, 28, 547–551. [Google Scholar]
- Breivik, H.; Borchgrevink, P.C.; Allen, S.M.; Rosseland, L.A.; Romundstad, L.; Hals, E.K.; Kvarstein, G.; Stubhaug, A. Assessment of pain. Br. J. Anaesth. 2008, 101, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Larson, P.A.; Berland, L.L.; Griffith, B.; Kahn, C.E., Jr.; Liebscher, L.A. Actionable findings and the role of IT support: Report of the ACR Actionable Reporting Work Group. J. Am. Coll. Radiol. 2014, 11, 552–558. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health. Radiation Risks and Pediatric Computed Tomography (CT): A Guide for Health Care Providers. Available online: https://www.cancer.gov/about-cancer/causes-prevention/risk/radiation/pediatric-ct-scans (accessed on 12 December 2024).
- The lmage Gently Alliance. Image Gently and Step Lightly Campaign. Available online: https://www.imagegently.org/ (accessed on 12 December 2024).
- Goske, M.J.; Applegate, K.E.; Boylan, J.; Butler, P.F.; Callahan, M.J.; Coley, B.D.; Farley, S.; Frush, D.P.; Hernanz-Schulman, M.; Jaramillo, D.; et al. The Image Gently campaign: Working together to change practice. AJR Am. J. Roentgenol. 2008, 190, 273–274. [Google Scholar] [CrossRef]
- Elikashvili, I.; Tay, E.T.; Tsung, J.W. The effect of point-of-care ultrasonography on emergency department length of stay and computed tomography utilization in children with suspected appendicitis. Acad. Emerg. Med. 2014, 21, 163–170. [Google Scholar] [CrossRef]
- Krishnamoorthi, R.; Ramarajan, N.; Wang, N.E.; Newman, B.; Rubesova, E.; Mueller, C.M.; Barth, R.A. Effectiveness of a staged US and CT protocol for the diagnosis of pediatric appendicitis: Reducing radiation exposure in the age of ALARA. Radiology 2011, 259, 231–239. [Google Scholar] [CrossRef]
- Marin, J.R.; Abo, A.M.; Arroyo, A.C.; Doniger, S.J.; Fischer, J.W.; Rempell, R.; Gary, B.; Holmes, J.F.; Kessler, D.O.; Lam, S.H.; et al. Pediatric emergency medicine point-of-care ultrasound: Summary of the evidence. Crit. Ultrasound J. 2016, 8, 16. [Google Scholar] [CrossRef] [PubMed]
- Marin, J.R.; Lyons, T.W.; Claudius, I.; Fallat, M.E.; Aquino, M.; Ruttan, T.; Daugherty, R.J. Optimizing Advanced Imaging of the Pediatric Patient in the Emergency Department: Technical Report. J. Am. Coll. Radiol. 2024, 21, e37–e69. [Google Scholar] [CrossRef] [PubMed]
- Smith-Bindman, R.; Aubin, C.; Bailitz, J.; Bengiamin, R.N.; Camargo, C.A., Jr.; Corbo, J.; Dean, A.J.; Goldstein, R.B.; Griffey, R.T.; Jay, G.D.; et al. Ultrasonography versus computed tomography for suspected nephrolithiasis. N. Engl. J. Med. 2014, 371, 1100–1110. [Google Scholar] [CrossRef]
- Lee, C.Y.; Chen, J.D. Diagnostic values of supine and erect abdominal radiographs for patients with acute abdomen: Which is better for decision making? J. Chin. Med. Assoc. 2022, 85, 709–716. [Google Scholar] [CrossRef] [PubMed]
- Alzyoud, K.; Al-Murshedi, S.; Abualkhael, K.; Alqawasmeh, F.; England, A. Supine and erect abdominal radiography: A comparison of radiation dose and image quality. Appl. Radiat. Isot. 2022, 190, 110477. [Google Scholar] [CrossRef]
- Mirvis, S.E.; Young, J.W.; Keramati, B.; McCrea, E.S.; Tarr, R. Plain film evaluation of patients with abdominal pain: Are three radiographs necessary? AJR Am. J. Roentgenol. 1986, 147, 501–503. [Google Scholar] [CrossRef]
- Kwon, H.; Jung, J.Y. Effectiveness of a radiation reduction campaign targeting children with gastrointestinal symptoms in a pediatric emergency department. Medicine 2017, 96, e5907. [Google Scholar] [CrossRef]
- Eurboonyanun, K.; Rungwiriyawanich, P.; Chamadol, N.; Promsorn, J.; Eurboonyanun, C.; Srimunta, P. Accuracy of Nonenhanced CT vs Contrast-Enhanced CT for Diagnosis of Acute Appendicitis in Adults. Curr. Probl. Diagn. Radiol. 2021, 50, 315–320. [Google Scholar] [CrossRef]
- Sadigh, G.; Applegate, K.E.; Baumgarten, D.A. Comparative accuracy of intravenous contrast-enhanced CT versus noncontrast CT plus intravenous contrast-enhanced CT in the detection and characterization of patients with hypervascular liver metastases: A critically appraised topic. Acad. Radiol. 2014, 21, 113–125. [Google Scholar] [CrossRef] [PubMed]
- Shaish, H.; Ream, J.; Huang, C.; Troost, J.; Gaur, S.; Chung, R.; Kim, S.; Patel, H.; Newhouse, J.H.; Khalatbari, S.; et al. Diagnostic Accuracy of Unenhanced Computed Tomography for Evaluation of Acute Abdominal Pain in the Emergency Department. JAMA Surg. 2023, 158, e231112. [Google Scholar] [CrossRef]
- Dym, R.J.; Duncan, D.R.; Spektor, M.; Cohen, H.W.; Scheinfeld, M.H. Renal stones on portal venous phase contrast-enhanced CT: Does intravenous contrast interfere with detection? Abdom. Imaging 2014, 39, 526–532. [Google Scholar] [CrossRef] [PubMed]
- Odenrick, A.; Kartalis, N.; Voulgarakis, N.; Morsbach, F.; Loizou, L. The role of contrast-enhanced computed tomography to detect renal stones. Abdom. Radiol. 2019, 44, 652–660. [Google Scholar] [CrossRef]
- Linet, M.S.; Kim, K.P.; Rajaraman, P. Children’s exposure to diagnostic medical radiation and cancer risk: Epidemiologic and dosimetric considerations. Pediatr. Radiol. 2009, 39 (Suppl. S1), 4–26. [Google Scholar] [CrossRef]
- Baysson, H.; Etard, C.; Brisse, H.J.; Bernier, M.O. [Diagnostic radiation exposure in children and cancer risk: Current knowledge and perspectives]. Arch. Pediatr. 2012, 19, 64–73. [Google Scholar] [CrossRef]
- Mathews, J.D.; Forsythe, A.V.; Brady, Z.; Butler, M.W.; Goergen, S.K.; Byrnes, G.B.; Giles, G.G.; Wallace, A.B.; Anderson, P.R.; Guiver, T.A.; et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: Data linkage study of 11 million Australians. BMJ 2013, 346, f2360. [Google Scholar] [CrossRef]
- Hong, J.Y.; Han, K.; Jung, J.H.; Kim, J.S. Association of Exposure to Diagnostic Low-Dose Ionizing Radiation With Risk of Cancer Among Youths in South Korea. JAMA Netw. Open 2019, 2, e1910584. [Google Scholar] [CrossRef] [PubMed]
- van Wassenaer, E.A.; Daams, J.G.; Benninga, M.A.; Rosendahl, K.; Koot, B.G.P.; Stafrace, S.; Arthurs, O.J.; van Rijn, R.R. Non-radiologist-performed abdominal point-of-care ultrasonography in paediatrics—A scoping review. Pediatr. Radiol. 2021, 51, 1386–1399. [Google Scholar] [CrossRef]
| Adult ED | Pediatric ED | p-Value | ||
|---|---|---|---|---|
| N = 683 | N = 267 | |||
| Sex, male | 284 (41.6) | 87 (32.6) | 0.011 | |
| Age, year | ||||
| Mean (95% CI) | 17.2 (17.1–17.2) | 16.6 (16.5–16.7) | <0.001 | |
| 16 | 174 (25.5) | 146 (54.7) | NA | |
| 17 | 225 (32.9) | 89 (33.3) | ||
| 18 | 284 (41.6) | 32 (12) | ||
| Body weight, kg | 58 (51.3–66.5) | 56 (49–65.5) | 0.124 | |
| KTAS | ||||
| Mean (95% CI) | 3.25 (3.22–3.29) | 2.86 (2.79–2.93) | <0.001 | |
| 1 | 1 (0.1) | 2 (0.7) | NA | |
| 2 | 13 (1.9) | 61 (22.8) | ||
| 3 | 484 (70.9) | 177 (66.3) | ||
| 4 | 182 (26.6) | 26 (9.7) | ||
| 5 | 3 (0.4) | 1 (0.4) | ||
| Clinical manifestation | ||||
| Pain scale | 4 (3–4) | 5 (3–7) | <0.001 | |
| Vomiting | 238 (34.8) | 91 (34.1) | 0.843 | |
| Diarrhea | 263 (38.5) | 71 (26.6) | 0.001 | |
| Tenderness | 307 (44.9) | 171 (64.0) | <0.001 | |
| Rebound tenderness | 24 (3.5) | 9 (3.4) | 0.242 | |
| Disposition | ||||
| Discharge | 587 (85.9) | 202 (75.7) | <0.001 | |
| Need for admission | 92 (13.5) | 64 (24.0) | 0.001 | |
| Admission | 27 (4) | 56 (21) | <0.001 | |
| ICU admission | 0 (0) | 0 (0) | NA | |
| Transfer | 65 (9.5) | 8 (3.0) | 0.001 | |
| Mortality | 0 (0) | 0 (0) | NA | |
| ED LOS, hour | 3.2 (1.9–5.2) | 4 (2.5–7.5) | <0.001 | |
| Revisit within 2 days | 19 (2.8) | 14 (5.2) | 0.061 | |
| Missed surgical emergency | 5 (0.7) | 1 (0.4) | NA | |
| Acute appendicitis | 4 (0.6) | 1 (0.4) | NA | |
| Ovarian torsion | 1 (0.1) | 0 (0) | NA | |
| Adult ED | Pediatric ED | p-Value | |||
|---|---|---|---|---|---|
| N = 683 | N = 267 | ||||
| Actionable emergency | 116 (17) | 49 (18.4) | 0.617 | ||
| Surgical emergency | 54 (7.9) | 18 (6.7) | 0.245 | ||
| Acute appendicitis | 39 (5.7) | 14 (5.2) | 0.778 | ||
| Ovarian torsion | 9 (1.3) | 0 (0) | 0.068 | ||
| Panperitonitis | 2 (0.3) | 0 (0) | NA | ||
| Pancreatic tumor rupture | 1 (0.1) | 0 (0) | NA | ||
| Sigmoid volvulus | 1 (0.1) | 0 (0) | NA | ||
| Splenic infarction | 1 (0.1) | 0 (0) | NA | ||
| Stomach perforation | 1 (0.1) | 0 (0) | NA | ||
| Duplication cyst | 0 (0) | 1 (0.4) | NA | ||
| Bowel obstruction due to lymphoma | 0 (0) | 1 (0.4) | NA | ||
| Venous malformation rupture | 0 (0) | 1 (0.4) | NA | ||
| Colonic perforation | 0 (0) | 1 (0.4) | NA | ||
| Cancer | 10 (1.5) | 6 (2.2) | 0.399 | ||
| Urinary stone | 9 (1.3) | 2 (0.7) | 0.737 | ||
| Ovarian cyst rupture | 7 (1) | 0 (0) | 0.200 | ||
| Biliary stone | 1 (0.1) | 5 (1.9) | NA | ||
| Pancreatitis | 2 (0.3) | 2 (0.7) | NA | ||
| Superior mesenteric artery syndrome | 2 (0.3) | 0 (0) | NA | ||
| Unexpected pregnancy | 1 (0.1) | 0 (0) | NA | ||
| Infection | |||||
| Acute pyelonephritis | 7 (1) | 8 (3) | 0.024 | ||
| Hepatitis | 6 (0.9) | 2 (0.7) | 1.000 | ||
| Cholangitis | 2 (0.3) | 3 (1.1) | NA | ||
| Diverticulitis | 5 (0.7) | 0 (0) | NA | ||
| Cholecystitis | 3 (0.4) | 0 (0) | NA | ||
| Intraabdominal abscess | 2 (0.3) | 1 (0.4) | NA | ||
| Pelvic inflammatory disease | 2 (0.3) | 0 (0) | NA | ||
| Epiploic appendicitis | 1 (0.1) | 0 (0) | NA | ||
| Extra-abdominal infection † | 2 (0.3) | 2 (0.7) | NA | ||
| Acute gastroenteritis | 395 (57.8) | 135 (50.6) | 0.096 | ||
| Non-specific abdominal pain | 130 (19) | 59 (22.1) | 0.211 | ||
| Others ‡ | 42 (6.1) | 24 (9) | NA | ||
| Adult ED | Pediatric ED | p-Value | ||||
|---|---|---|---|---|---|---|
| N = 683 | N = 267 | |||||
| Any image modality | 459 (67.2) | 238 (89.1) | <0.001 | |||
| X-ray | ||||||
| Mean (95% CI) number of images | 1.1 (1.08−1.22) | 0.9 (0.83−0.98) | <0.001 | |||
| Any | 421 (61.6) | 208 (77.9) | <0.001 | |||
| Supine only * | 10 (2.4) | 122 (58.7) | <0.001 | |||
| Erect only * | 46 (10.9) | 62 (29.8) | <0.001 | |||
| Both * | 366 (86.9) | 28 (13.5) | <0.001 | |||
| CT | ||||||
| Mean (95% CI) number of phases | 0.76 (0.69−0.83) | 0.49 (0.24−0.36) | <0.001 | |||
| Any | 259 (37.9) | 76 (28.5) | 0.006 | |||
| NECT only * | 11 (4.2) | 4 (5.3) | 1.000 | |||
| CECT only * | 0 (0) | 68 (89.5) | <0.001 | |||
| Both * | 249 (96.1) | 4 (5.3) | <0.001 | |||
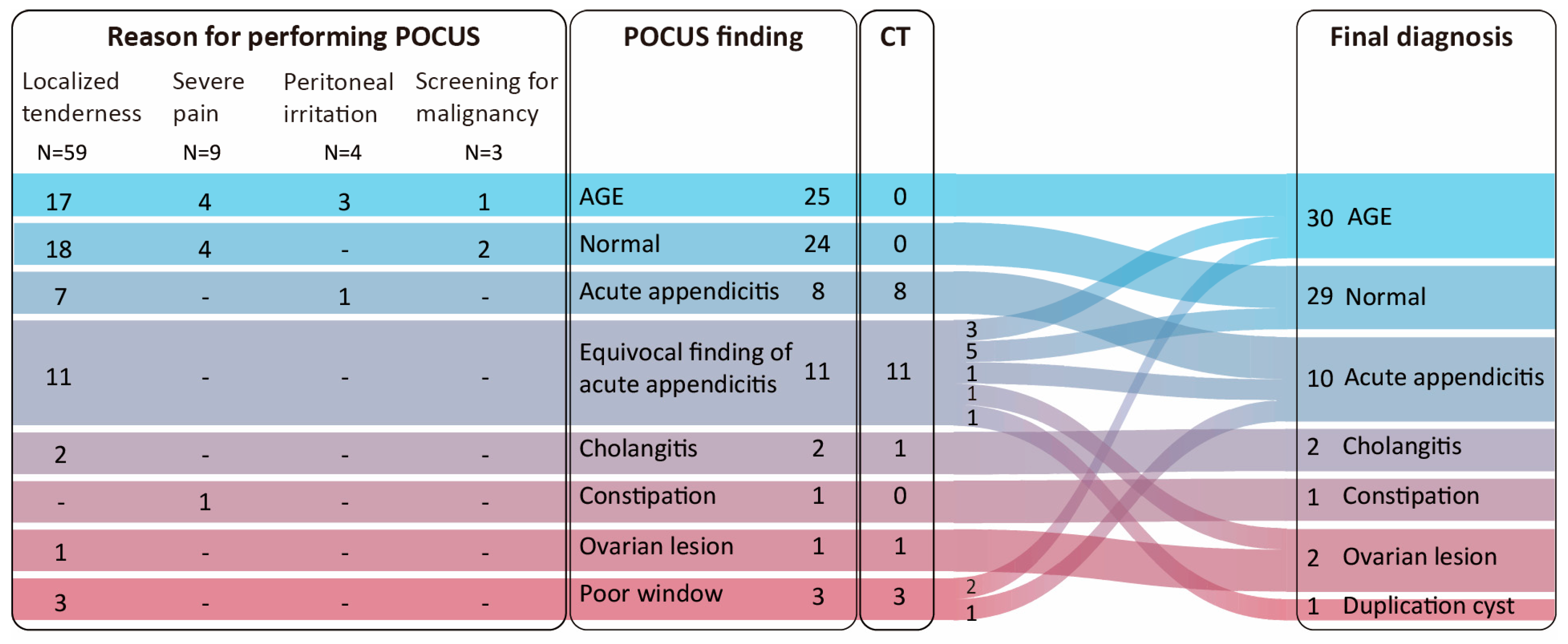
| POCUS | 1 (0.1) | 75 (28.0) | <0.001 | |||
| RADUS | 2 (0.3) | 10 (3.7) | <0.001 | |||
| Imaging Tests | Variables | B | SE | Wals | p Value | OR |
|---|---|---|---|---|---|---|
| Any image testing | Intercept | 1.13 | 0.23 | 23.0 | <0.001 | 3.1 |
| X-ray | Tenderness | 1.55 | 0.50 | 9.6 | 0.002 | 4.7 |
| Intercept | 0.32 | 0.33 | 0.9 | 0.332 | 1.4 | |
| POCUS | PED (vs. AED) | 3.25 | 1.10 | 8.8 | 0.003 | 25.8 |
| Tenderness | 1.98 | 0.89 | 5.0 | 0.025 | 7.3 | |
| Intercept | −3.51 | 1.08 | 10.5 | 0.001 | 0.03 | |
| CT | Vomiting | −1.49 | 0.62 | 5.7 | 0.017 | 0.23 |
| Tenderness | 1.81 | 0.56 | 10.4 | 0.001 | 6.1 | |
| Intercept | −1.69 | 0.49 | 12.0 | 0.001 | 0.18 | |
| Admission required | Rebound tenderness | 2.98 | 1.08 | 7.6 | 0.006 | 19.73 |
| Tenderness | 4.34 | 0.89 | 23.8 | 0.000 | 76.4 | |
| Intercept | −3.62 | 0.72 | 25.5 | 0.000 | 0.03 |
| Sensitivity | Specificity | PPV | NPV | Accuracy | |
|---|---|---|---|---|---|
| Actionable abdomen | 93.3 | 81.0 | 53.8 | 98.1 | 83.3 |
| Surgical abdomen | 91.7 | 84.8 | 52.4 | 98.2 | 85.9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chun, M.K.; Yoo, R.; Lim, S.-y.; Kim, D.; Han, J.; Choi, S.J.; Lee, J.-Y.; Lee, J.S.; Park, J.S. Lesson from a Single Pediatric Emergency Department: Potentially Applicable Radiation-Minimizing Practices for Non-Traumatic Abdominal Pain in Adolescents. Children 2025, 12, 1306. https://doi.org/10.3390/children12101306
Chun MK, Yoo R, Lim S-y, Kim D, Han J, Choi SJ, Lee J-Y, Lee JS, Park JS. Lesson from a Single Pediatric Emergency Department: Potentially Applicable Radiation-Minimizing Practices for Non-Traumatic Abdominal Pain in Adolescents. Children. 2025; 12(10):1306. https://doi.org/10.3390/children12101306
Chicago/Turabian StyleChun, Min Kyo, Reenar Yoo, Soo-young Lim, Dahyun Kim, Jeeho Han, Seung Jun Choi, Jeong-Yong Lee, Jong Seung Lee, and Jun Sung Park. 2025. "Lesson from a Single Pediatric Emergency Department: Potentially Applicable Radiation-Minimizing Practices for Non-Traumatic Abdominal Pain in Adolescents" Children 12, no. 10: 1306. https://doi.org/10.3390/children12101306
APA StyleChun, M. K., Yoo, R., Lim, S.-y., Kim, D., Han, J., Choi, S. J., Lee, J.-Y., Lee, J. S., & Park, J. S. (2025). Lesson from a Single Pediatric Emergency Department: Potentially Applicable Radiation-Minimizing Practices for Non-Traumatic Abdominal Pain in Adolescents. Children, 12(10), 1306. https://doi.org/10.3390/children12101306







