Morphometric Analysis of the Infraorbital Foramen in Children and Adolescents with Unilateral Cleft Lip and Palate: A CBCT Study
Abstract
Highlights
- On the cleft side (CS), the distances of IOF-IOM, IOF-SOM, IOF-S, IOF-N, IOF-LAP, and IOF-M were found to be significantly shorter than those on the non-cleft side (NCS). Conversely, the distances of IOF-ANS and IOF-J were significantly longer on the CS than on the NCS.
- No significant differences were observed between the CS and NCS regarding the IOF-TM and IOF-STT distances.
- On the CS, compared to the NCS, the injection site for inferior nerve block (INB) should be planned slightly more superior and medial.
- In INB applications, it has been clearly demonstrated that the standard needle depth can be used safely on both sides.
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethical Approval
2.2. Sample Size and Criteria
- Cleft side (CS),
- Non-cleft side (NCS).
- Confirmed diagnosis of nonsyndromic UCLP,
- Age between 6 and 18 years,
- Individuals who underwent primary lip repair before the age of one and hard palate repair before the age of three,
- Individuals who have not received orthodontic treatment,
- Availability of diagnostic-quality CBCT images,
- Clear visibility of anatomical landmarks in the infraorbital region bilaterally,
- Presence of bilateral cleft lip and/or palate,
- Any syndromic condition associated with craniofacial anomalies,
- History of facial trauma or prior orthognathic/facial surgery,
- Presence of developmental anomalies affecting the infraorbital region,
- Poor image quality or significant artifacts on CBCT scans.
2.3. CBCT Imaging Procedure
2.4. Evaluation of Diameters and Shape of Infraorbital Foramen
2.5. Evaluation of the Distance of the Infraorbital Foramen from Reference Anatomical Landmarks
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- The most common morphological shape of the IOF in both the CS and NCS is the V-oval form.
- No significant differences were found between the CS and NCS in both vertical and horizontal diameters.
- On the CS, the distances between the IOF-IOM, IOF-SOM, IOF-S, IOF-N, IOF-LAP, and IOF-M were significantly shorter than those on to the NCS.
- Conversely, the distances between the IOF-ANS and IOF-J were significantly longer on the CS than on the NCS.
- There were no significant differences between the two groups regarding the distances from the IOF-TM and the IOF-STT.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Martinelli, M.; Palmieri, A.; Carinci, F.; Scapoli, L. Non-syndromic cleft palate: An overview on human genetic and environmental risk factors. Front. Cell Dev. Biol. 2020, 8, 592271. [Google Scholar] [CrossRef]
- Wang, M.; Meng, R.; Wang, Z.; Liu, D.; Huang, H.; Kang, C.; Li, H.; Wu, T.; Zhan, S. Prevalence of oral clefts among live births in Gansu Province, China. Int. J. Environ. Res. Public. Health 2018, 15, 380. [Google Scholar] [CrossRef]
- Rychlik, D.; Wójcicki, P.; Koźlik, M. Osteoplasty of the alveolar cleft defect. Adv. Clin. Exp. Med. 2012, 21, 255–262. [Google Scholar]
- Paradowska-Stolarz, A.; Mikulewicz, M.; Duś-Ilnicka, I. Current concepts and challenges in the treatment of cleft lip and palate patients—A comprehensive review. J. Pers. Med. 2022, 12, 2089. [Google Scholar] [CrossRef]
- Wójcicki, P.; Koźlik, M.J.; Wójcicka, K. Genetic factors in selected complex congenital malformations with cleft defect. Adv. Clin. Exp. Med. Off. Organ. Wroc. Med. Univ. 2016, 25, 977–987. [Google Scholar] [CrossRef] [PubMed]
- Askarian, S.; Gholami, M.; Khalili-Tanha, G.; Tehrani, N.C.; Joudi, M.; Khazaei, M.; Ferns, G.A.; Hassanian, S.M.; Avan, A.; Joodi, M. The genetic factors contributing to the risk of cleft lip-cleft palate and their clinical utility. Oral. Maxillofac. Surg. 2023, 27, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Parveen, S.; Husain, A.; Johns, G.; Mascarenhas, R.; Reddy, S.G. Three-dimensional analysis of craniofacial structures of individuals with nonsyndromic unilateral complete cleft lip and palate. J. Craniofacial Surg. 2021, 32, e65–e69. [Google Scholar] [CrossRef] [PubMed]
- Ozdemir, S.A.; Esenlik, E. Three-dimensional soft-tissue evaluation in patients with cleft lip and palate. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2018, 24, 8608. [Google Scholar] [CrossRef]
- Haylaz, E.; Kalabalık, F.; Cicek, O.; Gümüşsoy, İ.; Aytuğar, E. Comparative CBCT Analysis of Maxillofacial Skeletal Structures in Patients with Unilateral Cleft Lip and Palate and Non-Cleft Individuals. Diagnostics 2024, 14, 2555. [Google Scholar] [CrossRef]
- Ye, B.; Wu, Y.; Zhou, Y.; Jing, H.; Hu, J.; Zhang, G. A comparative cephalometric study for adult operated cleft palate and unoperated cleft palate patients. J. Cranio-Maxillofac. Surg. 2015, 43, 1218–1223. [Google Scholar] [CrossRef] [PubMed]
- Zheng, J.; Sun, Y.; Yang, Z.; Guo, D.; Ren, M.; Jiang, Y.; Yuan, W. Comparison of craniomaxillofacial morphology in children with unilateral cleft lip and palate treated with/without presurgical nasoalveolar molding-a retrospective study with a mean age of 5 years. Clin. Oral. Investig. 2024, 28, 326. [Google Scholar] [CrossRef] [PubMed]
- Nelke, K.; Janeczek, M.; Małyszek, A.; Łukaszewski, M.; Frydrych, M.; Kulus, M.; Dąbrowski, P.; Łuczak, K.; Pawlak, W.; Gogolewski, G. Facial Foramen Diagnostic and Surgical Role as Reference Points in Asymmetries—Cone-Beam Computed Tomography Preliminary Study. J. Clin. Med. 2025, 14, 463. [Google Scholar] [CrossRef]
- Razak, T.N.A.; AC, L.R.; Narayanan, V.; Gurram, P.; Vivek, N. Morphometric Analysis of the Infraorbital Canal, Groove, and Foramen in the Indian Population: A Retrospective Analytical Study. Cureus 2024, 16, e72367. [Google Scholar] [CrossRef] [PubMed]
- Aryanezhad, S.S.; Jafari-Pozve, N.; Abrishami, M.; Arianezhad, S.M. Investigating the anatomy and location of the infraorbital canal in relation to the adjacent structures in cone beam computed tomography (CBCT) images. J. Maxillofac. Oral. Surg. 2024, 24, 542–556. [Google Scholar] [CrossRef] [PubMed]
- Thilakumara, I.; Hettiarachchi, P.; Jayasinghe, R.; Fonseka, M.; Jayasinghe, R.D.; Nanayakkara, C. Morphometric Analysis of Infraorbital Foramen Using Cone Beam Computed Tomography in a Cohort of Sri Lankan Adults. Int. J. Morphol. 2021, 39, 489–496. [Google Scholar] [CrossRef]
- Gumussoy, I.; Haylaz, E.; Duman, S.B.; Kalabalık, F.; Eren, M.C.; Say, S.; Celik, O.; Bayrakdar, I.S. Automatic Segmentation of the Infraorbital Canal in CBCT Images: Anatomical Structure Recognition Using Artificial Intelligence. Diagnostics 2025, 15, 1713. [Google Scholar] [CrossRef]
- Orhan, K.; Misirli, M.; Aksoy, S.; Hincal, U.S.E.; Ormeci, T.; Arslan, A. Morphometric analysis of the infraorbital foramen, canal and groove using cone beam CT: Considerations for creating artificial organs. Int. J. Artif. Organs 2016, 39, 28–36. [Google Scholar] [CrossRef]
- Allam, A.E.-S.; Khalil, A.A.F.; Eltawab, B.A.; Wu, W.-T.; Chang, K.-V. Ultrasound-Guided Intervention for Treatment of Trigeminal Neuralgia: An Updated Review of Anatomy and Techniques. Pain. Res. Manag. 2018, 2018, 5480728. [Google Scholar] [CrossRef]
- Shi, B.; Losee, J.E. The impact of cleft lip and palate repair on maxillofacial growth. Int. J. Oral. Sci. 2015, 7, 14–17. [Google Scholar] [CrossRef]
- Guerrero, C.A. Cleft lip and palate surgery: 30 years follow-up. Ann. Maxillofac. Surg. 2012, 2, 153–157. [Google Scholar] [CrossRef] [PubMed]
- Haghnegahdar, A.; Khojastepour, L.; Naderi, A. Evaluation of infraorbital canal in cone beam computed tomography of maxillary sinus. J. Dent. 2018, 19, 41. [Google Scholar]
- Zdilla, M.J.; Russell, M.L.; Koons, A.W. Infraorbital foramen location in the pediatric population: A guide for infraorbital nerve block. Pediatr. Anesth. 2018, 28, 697–702. [Google Scholar] [CrossRef] [PubMed]
- Suresh, S.; Voronov, P.; Curran, J. Infraorbital nerve block in children: A computerized tomographic measurement of the location of the infraorbital foramen. Reg. Anesth. Pain. Med. 2006, 31, 211–214. [Google Scholar] [CrossRef]
- Jamilian, A.; Lucchese, A.; Darnahal, A.; Kamali, Z.; Perillo, L. Cleft sidedness and congenitally missing teeth in patients with cleft lip and palate patients. Prog. Orthod. 2016, 17, 14. [Google Scholar] [CrossRef]
- Suresh, S.; Voronov, P. Head and neck blocks in infants, children, and adolescents. Pediatr. Anesth. 2012, 22, 81–87. [Google Scholar] [CrossRef] [PubMed]
- Malherbe, V.; Bosenberg, A.T.; Lomeli, A.L.; Neser, C.; Pienaar, C.H.; Madaree, A. Regional anaesthesia for cleft lip surgery in a developing world setting. S. Afr. J. Surg. 2014, 52, 108–110. [Google Scholar] [CrossRef]
- Wang, H.; Liu, G.; Fu, W.; Li, S.t. The effect of infraorbital nerve block on emergence agitation in children undergoing cleft lip surgery under general anesthesia with sevoflurane. Pediatr. Anesth. 2015, 25, 906–910. [Google Scholar] [CrossRef]
- Saeedi, O.J.; Wang, H.; Blomquist, P.H. Penetrating globe injury during infraorbital nerve block. Arch. Otolaryngol.–Head Neck Surg. 2011, 137, 396–397. [Google Scholar] [CrossRef]
- Dağıstan, S.; Miloğlu, Ö.; Altun, O.; Umar, E. Retrospective morphometric analysis of the infraorbital foramen with cone beam computed tomography. Niger. J. Clin. Pract. 2017, 20, 1053–1064. [Google Scholar]
- Aggarwal, A.; Kaur, H.; Gupta, T.; Tubbs, R.S.; Sahni, D.; Batra, Y.; Sondekoppam, R.V. Anatomical study of the infraorbital foramen: A basis for successful infraorbital nerve block. Clin. Anat. 2015, 28, 753–760. [Google Scholar] [CrossRef]
- Nanayakkara, D.; Peiris, R.; Mannapperuma, N.; Vadysinghe, A. Morphometric analysis of the infraorbital foramen: The clinical relevance. Anat. Res. Int. 2016, 2016, 7917343. [Google Scholar] [CrossRef]
- Tan, S.P.; Allareddy, V.; Bruun, R.A.; Mulliken, J.B.; Sullivan, S.R.; Peguero, O.J., Jr.; Cooper, J.S.; Padwa, B.L.; Gerlein, E.J.; Cook, E.F. Effect of infant surgical orthopedic treatment on facial growth in preadolescent children with unilateral and bilateral complete cleft lip and palate. Oral. Surg. Oral. Med. Oral. Pathol. Oral. Radiol. 2015, 120, 291–298. [Google Scholar] [CrossRef] [PubMed]
- Naqvi, Z.A.; Shivalinga, B.; Ravi, S.; Munawwar, S.S. Effect of cleft lip palate repair on craniofacial growth. J. Orthod. Sci. 2015, 4, 59–64. [Google Scholar] [CrossRef]
- Ukoha, U.U.; Umeasalugo, K.E.; Udemezue, O.O.; Nzeako, H.C.; Ndukwe, G.U.; Nwankwo, P.C. Anthropometric measurement of infraorbital foramen in south-east and south-south Nigeria. Natl. J. Med. Res. 2014, 4, 225–227. [Google Scholar]
- Hwang, S.H.; Kim, S.W.; Park, C.S.; Kim, S.W.; Cho, J.H.; Kang, J.M. Morphometric analysis of the infraorbital groove, canal, and foramen on three-dimensional reconstruction of computed tomography scans. Surg. Radiol. Anat. 2013, 35, 565–571. [Google Scholar] [CrossRef]
- Bjelakovic, M.D.; Popovic, J.; Stojanov, D.; Dzopalic, T.; Ignjatovic, J. Morphometric characteristics of the ınfraorbital foramen on volumerendered CT scans. RAD Assoc. J. 2017, 2, 204–206. [Google Scholar]
- Chrcanovic, B.R.; Abreu, M.H.N.G.; Custódio, A.L.N. A morphometric analysis of supraorbital and infraorbital foramina relative to surgical landmarks. Surg. Radiol. Anat. 2011, 33, 329–335. [Google Scholar] [CrossRef]
- Sundareswaran, S.; Nipun, C. Bridging the gap: Sella turcica in unilateral cleft lip and palate patients. Cleft Palate-Craniofacial J. 2015, 52, 597–604. [Google Scholar] [CrossRef]
- Kochhar, A.S.; Nucci, L.; Sidhu, M.S.; Prabhakar, M.; Grassia, V.; Perillo, L.; Kochhar, G.K.; Bhasin, R.; Dadlani, H.; d’Apuzzo, F. Reliability and reproducibility of landmark identification in unilateral cleft lip and palate patients: Digital lateral vis-a-vis CBCT-derived 3D cephalograms. J. Clin. Med. 2021, 10, 535. [Google Scholar] [CrossRef]
- Tekemen, Ş.; Özer, C.M.; Atalar, K.; Kayatekin, A.Z.Y. Evaluation of Foramen Infraorbitale by Three Dimensional Reconstruction Method. Batı Karadeniz Tıp Derg. 2021, 5, 94–100. [Google Scholar] [CrossRef]
- Vaezi, M.; Karagah, A.; Damghani, F.T.; Tofangchiha, M.; Alizadeh, A.; Reda, R.; Testarelli, L. Morphometric analysis of the infraorbital groove, canal, and foramen on computed tomography scans of an Iranian population. Odovtos Int. J. Dent. Sci. 2025, 27, 139–152. [Google Scholar]
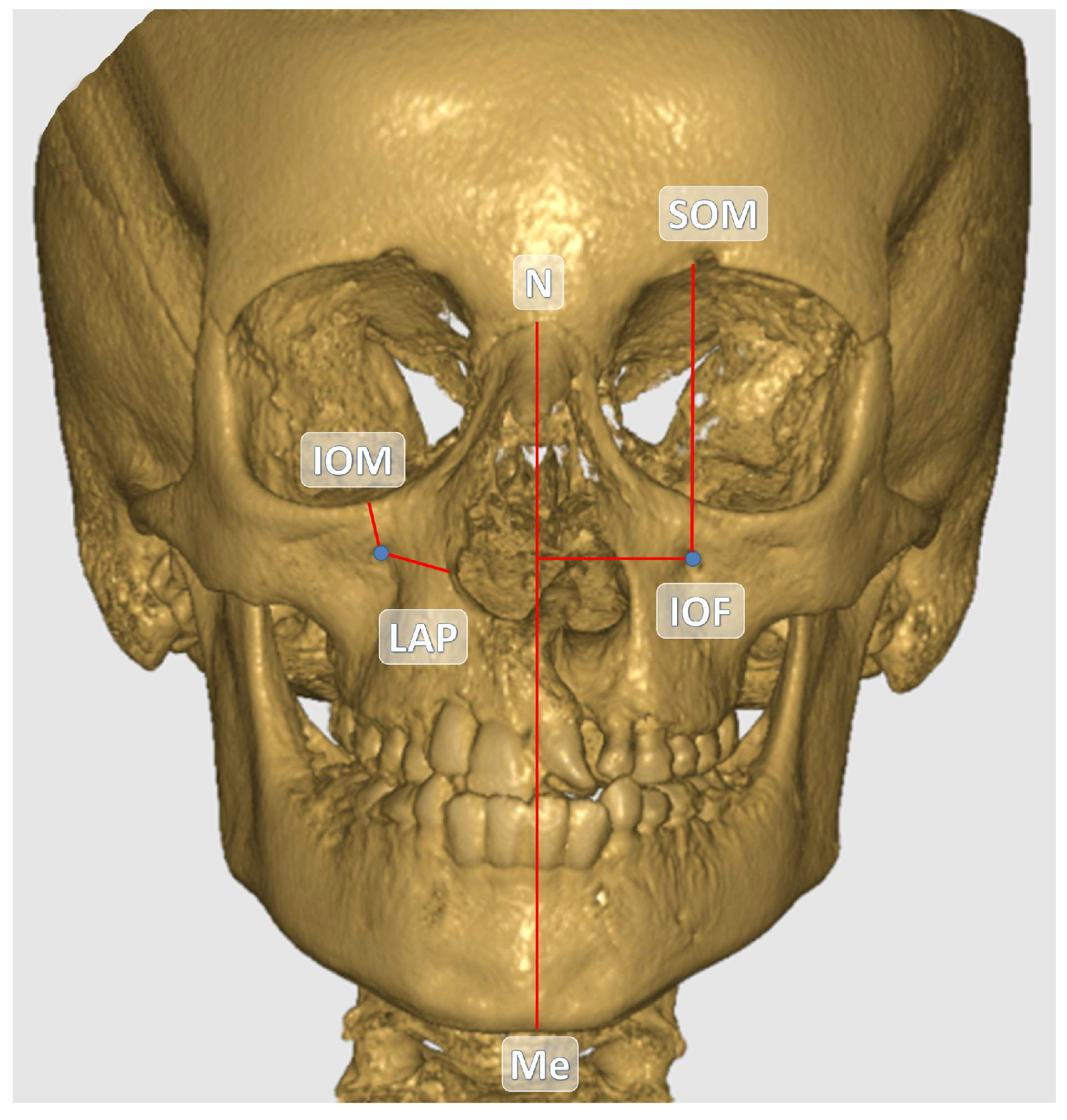


| Abbreviation | Description |
|---|---|
| IOF-SOM | Distance between the center of the infraorbital foramen and the upper margin of the orbit in coronal sections. |
| IOF-IOM | Distance between the center of the infraorbital foramen and the lower margin of the orbit in coronal sections. |
| IOF-N | Distance between the center of the infraorbital foramen and the nasion in coronal sections. |
| IOF-ANS | Distance between the center of the infraorbital foramen and the spina nasalis anterior in coronal sections. |
| IOF-TM | Distance between the center of the infraorbital foramen and the tuber maxilla in coronal sections. The highest point of the alveolar bone at the cemento-enamel border of the upper jaw 1st molar tooth was taken as reference. |
| IOF-S | Distance between the center of the infraorbital foramen and the sella in sagittal sections. |
| IOF-LAP | Distance between the center of the infraorbital foramen and the lateral margin of the aperture piriformis in coronal sections. |
| IOF-STT | Distance between the center of the infraorbital foramen and the soft tissue thickness in sagittal sections. |
| IOF-J | Distance between the center of the infraorbital foramen and the jugale point on coronal sections. |
| IOF-M | Distance between the center of the infraorbital foramen and the midline on coronal sections. The midline was determined by reference to the line connecting the nasion and menton points. |
| Gender | N | % |
| Male | 33 | 68.75 |
| Female | 15 | 31.25 |
| Total | 48 | 100 |
| Age | Mean ± SD | Min.–Max. |
| Male | 13.55 ± 2.29 | 9.9–17.9 |
| Female | 13.90 ± 2.58 | 9.0–17.8 |
| Total | 13.66 ± 2.36 | 9.0–17.9 |
| Shape | Cleft Side N (%) | Non-Cleft Side N (%) | Total N (%) |
| H-oval | 8 (16.7) | 10 (20.8) | 18 (18.8) |
| V-oval | 30 (62.5) | 28 (58.3) | 58 (60.4) |
| Round | 10 (20.8) | 10 (20.8) | 20 (20.8) |
| Total | 48 (100.0) | 48 (100.0) | 96 (100.0) |
| Cleft Side | Non-Cleft Side | ||||||
|---|---|---|---|---|---|---|---|
| Measurements | Min. | Max. | Mean ± SD | Min. | Max. | Mean ± SD | p Value |
| Horizontal Diameter | 1.30 | 4.30 | 2.75 ± 0.61 | 1.51 | 4.26 | 2.80 ± 0.55 | 0.607 |
| Vertical Diameter | 1.49 | 4.34 | 3.19 ± 0.64 | 1.76 | 4.21 | 3.22 ± 0.46 | 0.804 |
| IOF-IOM | 4.73 | 11.02 | 7.56 ± 1.36 | 4.76 | 11.22 | 8.06 ± 1.60 | 0.005 * |
| IOF-SOM | 38.07 | 48.99 | 42.54 ± 1.99 | 38.55 | 49.49 | 42.98 ± 2.18 | 0.032 * |
| IOF-ANS | 26.07 | 39.92 | 33.36 ± 3.06 | 21.00 | 41.17 | 31.13 ± 3.53 | <0.001 * |
| IOF-S | 53.46 | 70.29 | 60.20 ± 3.76 | 53.60 | 69.55 | 61.00 ± 4.07 | 0.006 * |
| IOF-N | 39.44 | 49.35 | 43.95 ± 2.66 | 39.32 | 50.70 | 44.61 ± 2.60 | <0.024 * |
| IOF-J | 17.68 | 30.30 | 22.27 ± 2.72 | 15.70 | 25.86 | 21.25 ± 2.28 | 0.001 * |
| IOF-TM | 23.19 | 42.01 | 31.15 ± 4.75 | 23.89 | 41.34 | 30.85 ± 4.78 | 0.379 |
| IOF-LAP | 11.44 | 21.73 | 15.29 ± 2.22 | 11.38 | 20.18 | 16.07 ± 1.92 | 0.013 * |
| IOF-M | 21.51 | 31.63 | 26.34 ± 2.26 | 22.64 | 33.44 | 27.73 ± 2.30 | <0.001 * |
| IOF-STT | 8.48 | 15.82 | 11.49 ± 1.74 | 8.47 | 15.07 | 11.47 ± 1.65 | 0.914 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haylaz, E.; Kalabalık, F.; Gumussoy, I.; Duman, S.B.; Eren, M.C.; Say, S.; Akarçay, F.O.; Aytuğar, E. Morphometric Analysis of the Infraorbital Foramen in Children and Adolescents with Unilateral Cleft Lip and Palate: A CBCT Study. Children 2025, 12, 1289. https://doi.org/10.3390/children12101289
Haylaz E, Kalabalık F, Gumussoy I, Duman SB, Eren MC, Say S, Akarçay FO, Aytuğar E. Morphometric Analysis of the Infraorbital Foramen in Children and Adolescents with Unilateral Cleft Lip and Palate: A CBCT Study. Children. 2025; 12(10):1289. https://doi.org/10.3390/children12101289
Chicago/Turabian StyleHaylaz, Emre, Fahrettin Kalabalık, Ismail Gumussoy, Suayip Burak Duman, Muhammet Can Eren, Seyda Say, Furkan Osman Akarçay, and Emre Aytuğar. 2025. "Morphometric Analysis of the Infraorbital Foramen in Children and Adolescents with Unilateral Cleft Lip and Palate: A CBCT Study" Children 12, no. 10: 1289. https://doi.org/10.3390/children12101289
APA StyleHaylaz, E., Kalabalık, F., Gumussoy, I., Duman, S. B., Eren, M. C., Say, S., Akarçay, F. O., & Aytuğar, E. (2025). Morphometric Analysis of the Infraorbital Foramen in Children and Adolescents with Unilateral Cleft Lip and Palate: A CBCT Study. Children, 12(10), 1289. https://doi.org/10.3390/children12101289





