Phenotypic Presentation of Children with Joint Hypermobility: Preclinical Signs
Abstract
1. Introduction
2. Methods
2.1. Data Collection Instrument
2.2. Examination of Sitting Positions
2.3. Examination of the GJH Utilizing BS
2.4. Identification of Occasional Occurrence of Joint Dislocations and Subluxations
2.5. Statistical Analysis
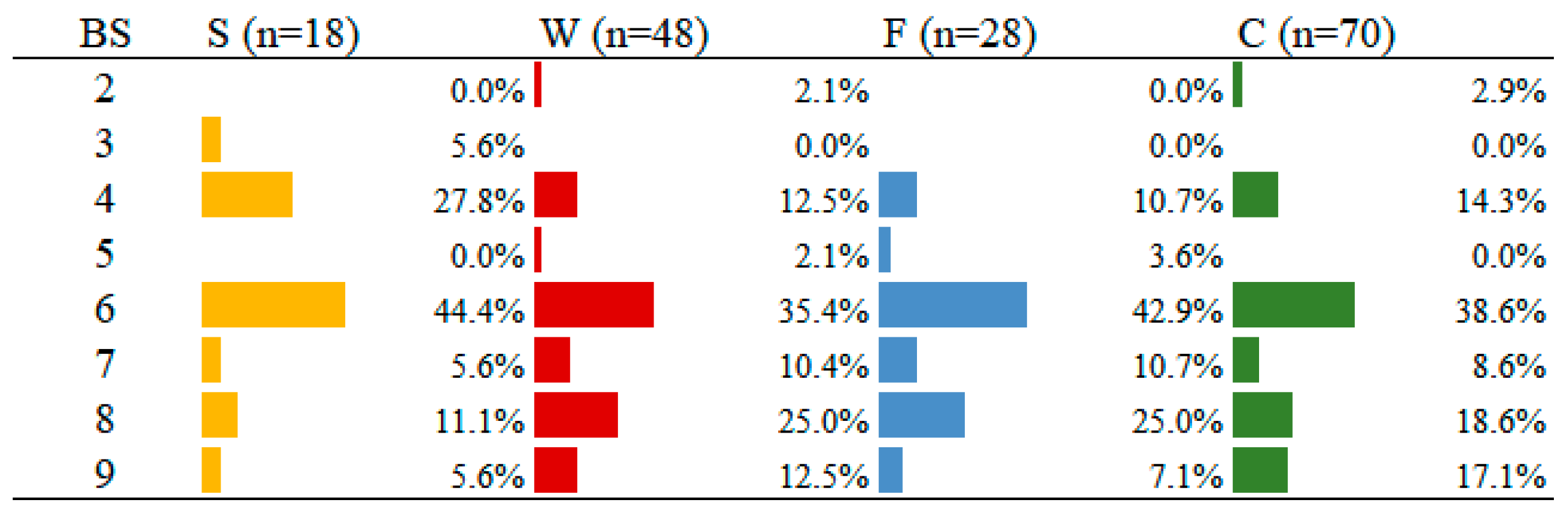
3. Results
3.1. Postures and Abilities in Sitting Position
3.2. Influence of Sex on BS
4. Discussion
5. Conclusions
Limitations of the Study
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grahame, R. Joint hypermobility and genetic collagen disorders: Are they related? Arch. Dis. Child. 1999, 80, 188–191. [Google Scholar] [CrossRef]
- Malfait, F.; Francomano, C.; Byers, P.; Belmont, J.; Berglund, B.; Black, J.; Bloom, L.; Bowen, J.M.; Brady, A.F.; Burrows, N.P.; et al. The 2017 International Classification of the Ehlers-Danlos Syndromes. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 8–26. [Google Scholar] [CrossRef] [PubMed]
- Lamari, N.M.; Chueire, A.G.; Cordeiro, J.A. Analysis of joint mobility patterns among preschool children. São Paulo Med. J. 2005, 123, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Stern, C.M.; Pepin, M.J.; Stoler, J.M.; Kramer, D.E.; Spencer, S.A.; Stein, C.J. Musculoskeletal Conditions in a Pediatric Population with Ehlers-Danlos Syndrome. J. Pediatr. 2017, 181, 261–266. [Google Scholar] [CrossRef]
- Lamari, M.M.; Lamari, N.M.; de Medeiros, M.P.; Giacomini, M.G.; Santos, A.B.; de Araújo Filho, G.M.; Goloni-Bertollo, E.M.; Pavarino, É.C. Generalized Joint Hypermobility: A Statistical Analysis Identifies Non-Axial Involvement in Most Cases. Children 2024, 11, 344. [Google Scholar] [CrossRef]
- Lamari, N.M.; Lamari, M.M. Characterization of brazilian children with joint hypermobility. Int. J. Physiatry 2016, 2, 011. [Google Scholar] [CrossRef]
- Tofts, L.J.; Simmonds, J.; Schwartz, S.B.; Richheimer, R.M.; O’Connor, C.; Elias, E.; Engelbert, R.; Cleary, K.; Tinkle, B.T.; Kline, A.D.; et al. Pediatric joint hypermobility: A diagnostic framework and narrative review. Orphanet J. Rare Dis. 2023, 18, 104. [Google Scholar] [CrossRef]
- Kirby, A.; Davies, R. Developmental Coordination Disorder and Joint Hypermobility Syndrome?—Overlapping disorders? Implications for research and clinical practice. Child Care Health Dev. 2007, 33, 513–519. [Google Scholar] [CrossRef] [PubMed]
- Castori, M.; Tinkle, B.; Levy, H.; Grahame, R.; Malfait, F.; Hakim, A. A framework for the classification of joint hypermobility and related conditions. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 148–157. [Google Scholar] [CrossRef] [PubMed]
- Beighton, P.; Solomon, I.; Soskolne, L. Articular mobility in an African population. Ann. Rheum. Dis. 1973, 32, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Juul-Kristensen, B.; Schmedling, K.; Rombaut, L.; Lund, H.; Engelbert, R.H.H. Measurement Properties of Clinical Assessment Methods for Classifying Generalized Joint Hypermobility-A Systematic Review. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175C, 116–147. [Google Scholar] [CrossRef] [PubMed]
- Grahame, R. Joint hypermobility: Emerging disease or illness behaviour? Clin. Med. 2013, 13 (Suppl. 6), s50–s52. [Google Scholar] [CrossRef] [PubMed]
- Castori, M. Deconstructing and reconstructing joint hypermobility on an evo-devo perspective. Rheumatology 2021, 60, 2537–2544. [Google Scholar] [CrossRef] [PubMed]
- Purvis, T. Mecânica Articular I. Traduzido por Mariane M. Franceschi Malucelli; RTS Brasil: Curitiba, Brazil, 2017; Volume 1. [Google Scholar]
- Guedes, D.P. Crescimento e desenvolvimento aplicado à Educação Física e ao esporte. Rev. Bras. Educ. Física Esp. 2011, 25, 127–140. [Google Scholar] [CrossRef]
- Kłodowski, A.; Rantalainen, T. Multibody Approach to Musculoskeletal and Joint Loading. Arch. Comput. Methods Eng. 2015, 22, 237–267. [Google Scholar] [CrossRef]
- Pinheiro, M.B.; Avelar, B.S.; Teixeira-Salmela, L.F. Implicações clínicas das respostas dos tecidos musculares e conjuntivos ao estresse físico. Ter. Man. 2013, 11, 111–116. [Google Scholar]
- Levangie, P.K.; Norkin, C.C. Joint Structure and Function: A Comprehensive Analysis, 5th ed.; F. A. Davis Company: Philadelphia, PA, USA, 2011. [Google Scholar]
- Guedes, D.P.; Guedes, J.E.R.P. Crescimento Composição Corporal e Desempenho Motor: De Crianças e Adolescentes; CLR Balieiro: São Paulo, Brazil, 2000. [Google Scholar]
- Malina, R.M.; Bouchard, C. Atividade Física do Atleta Jovem: Do Crescimento à Maturação; Roca: São Paulo, Brazil, 2002. [Google Scholar]
- Matsudo, S.M.; Paschoal, V.C.P.; Amancio, O.M.S. Atividade Física e sua relação com o crescimento e a maturação biológica de crianças. Cad. Nutr. Soc. Bras. Aliment. Nutr. 1997, 14, 1–12. [Google Scholar]
- Galli, M.; Cimolin, V.; Vismara, L.; Grugni, G.; Camerota, F.; Celletti, C.; Albertini, G.; Rigoldi, C.; Capodaglio, P. The effects of muscle hypotonia and weakness on balance: A study on Prader-Willi and Ehlers-Danlos syndrome patients. Res. Dev. Disabil. 2011, 32, 1117–1121. [Google Scholar] [CrossRef] [PubMed]
- Galli, M.; Cimolin, V.; Rigoldi, C.; Castori, M.; Celletti, C.; Albertini, G.; Camerota, F. Gait strategy in patients with Ehlers-Danlos syndrome hypermobility type: A kinematic and kinetic evaluation using 3D gait analysis. Res. Dev. Disabil. 2011, 32, 1663–1668. [Google Scholar] [CrossRef]
- Rombaut, L.; Malfait, F.; De Wandele, I.; Cools, A.; Thijs, Y.; De Paepe, A.; Calders, P. Medication, surgery, and physiotherapy among patients with the hypermobility type of Ehlers-Danlos syndrome. Arch. Phys. Med. Rehabil. 2011, 92, 1106–1112. [Google Scholar] [CrossRef]
- Booshanam, D.S.; Cherian, B.; Joseph, C.P.; Mathew, J.; Thomas, R. Evaluation of posture and pain in persons with benign joint hypermobility syndrome. Rheumatol. Int. 2011, 31, 1561–1565. [Google Scholar] [CrossRef]
- Vařeková, R.; Vařeka, I.; Janura, M.; Svoboda, Z.; Elfmark, M. Evaluation of Postural Asymmetry and Gross Joint Mobility in Elite Female Volleyball Athletes. J. Hum. Kinet. 2011, 29, 5–13. [Google Scholar] [CrossRef] [PubMed]
- Scheper, M.C.; Juul-Kristensen, B.; Rombaut, L.; Rameckers, E.A.; Verbunt, J.; Engelbert, R.H. Disability in Adolescents and Adults Diagnosed with Hypermobility-Related Disorders: A Meta-Analysis. Arch. Phys. Med. Rehabil. 2016, 97, 2174–2187. [Google Scholar] [CrossRef] [PubMed]
- Chopra, P.; Tinkle, B.; Hamonet, C.; Brock, I.; Gompel, A.; Bulbena, A.; Francomano, C. Pain management in the Ehlers-Danlos syndromes. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 212–219. [Google Scholar] [CrossRef]
- Tibbo, M.E.; Wyles, C.C.; Houdek, M.T.; Wilke, B.K. Outcomes of Primary Total Knee Arthroplasty in Patients With Ehlers-Danlos Syndromes. J. Arthroplast. 2019, 34, 315–318. [Google Scholar] [CrossRef] [PubMed]
- Ericson, W.B., Jr.; Wolman, R. Orthopaedic management of the Ehlers-Danlos syndromes. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 188–194. [Google Scholar] [CrossRef]
- Lamari, M.M.; Lamari, N.M.; Araujo-Filho, G.M.; Medeiros, M.P.; Marques, V.R.P.; Pavarino, E.C. Psychosocial and motor characteristics of patients with hypermobility. Front. Psychiatry 2022, 12, 787822. [Google Scholar] [CrossRef] [PubMed]
- Sanders, J.O.; Qiu, X.; Lu, X.; Duren, D.L.; Liu, R.W.; Dang, D.; Menendez, M.E.; Hans, S.D.; Weber, D.R.; Cooperman, D.R. The Uniform Pattern of Growth and Skeletal Maturation during the Human Adolescent Growth Spurt. Sci. Rep. 2017, 7, 16705. [Google Scholar] [CrossRef] [PubMed]
- Lamari, N.; Beighton, P. Hypermobility in Medical Practice; Springer Nature: Berlin/Heidelberg, Germany, 2023. [Google Scholar]
- Engelbert, R.H.; Juul-Kristensen, B.; Pacey, V.; de Wandele, I.; Smeenk, S.; Woinarosky, N.; Sabo, S.; Scheper, M.C.; Russek, L.; Simmonds, J.V. The evidence-based rationale for physical therapy treatment of children, adolescents, and adults diagnosed with joint hypermobility syndrome/hypermobile Ehlers Danlos syndrome. Am. J. Med. Genet. C Semin. Med. Genet. 2017, 175, 158–167. [Google Scholar] [CrossRef] [PubMed]
- Norkin, C.C.; White, D.J. Medida do Movimento Articular: Manual de Goniometria. Artes. Medicas 1997, 2, 34–39. [Google Scholar]
- Thomson, A.; Skneeer Pierct, J. Fisioterapia de Tidy, 12th ed.; Livraria Ed Santos: São Paulo, Brazil, 1994; Volume 5, pp. 33–37. [Google Scholar]
- Jekel, J.F.; Elmore, J.G.; Katz, D.L. Epidemiologia, Bioestatística e Medicina Preventiva; Artmed: Porto Alegre, Brazil, 2002. [Google Scholar]
- Minitab, Inc. Minitab 16.2.2 [Software]; Minitab, Inc.: State College, PA, USA, 2010. [Google Scholar]
- Miller, S.M.C.; Lamari, M.M.; Lamari, N.M. Síndrome de Ehlers-Danlos -tipo hipermobilidade: Estratégias de inclusão. Arq. Ciênc. Saúde 2015, 22, 21–27. [Google Scholar] [CrossRef][Green Version]
- Romeo, D.M.; Venezia, I.; De Biase, M.; Ascione, F.; Lala, M.R.; Arcangeli, V.; Mercuri, E.; Brogna, C. Developmental Coordination Disorder and Joint Hypermobility in Childhood: A Narrative Review. Children 2022, 9, 1011. [Google Scholar] [CrossRef] [PubMed]
- Geuze, R.H. Postural Control in Children with Developmental Coordination Disorder. Neural Plast. 2005, 12, 183–196. [Google Scholar] [CrossRef] [PubMed]
- Casanova, E.L.; Baeza-Velasco, C.; Buchanan, C.B.; Casanova, M.F. The Relationship between Autism and Ehlers-Danlos Syndromes/Hypermobility Spectrum Disorders. J. Pers. Med. 2020, 10, 260. [Google Scholar] [CrossRef]
- Lamari, N.M.; Baeza-Velasco, C.; Araújo Filho, G.M.; Lamari, M.M.; Medeiros, M.P. Autism spectrum disorder and Ehlers-Danlos syndrome—Hypermobility type: A case report. Arch. Health Sci. 2021, 28, 46–48. [Google Scholar] [CrossRef]
- Alter, M.J. Ciência da Flexibilidade, 3rd ed.; Artmed: Porto Alegre, Brazil, 2010. [Google Scholar]
- Castori, M.; Camerota, F.; Celletti, C.; Grammatico, P.; Padua, L. Ehlers-Danlos syndrome hypermobility type and the excess of affected females: Possible mechanisms and perspectives. Am. J. Med. Genet. Part A 2010, 152A, 2406–2408. [Google Scholar] [CrossRef] [PubMed]
- Malek, S.; Reinhold, E.J.; Pearce, G.S. The Beighton Score as a measure of generalised joint hypermobility. Reumatol. Int. 2021, 41, 1707–1716. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, L.L.; Simmonds, J.; Pacey, V.; De Wandele, I.; Rombaut, L.; Williams, C.M.; Chan, C. International Perspectives on Joint Hypermobility: A Synthesis of Current Science to Guide Clinical and Research Directions. J. Clin. Rheumatol. 2022, 28, 314–320. [Google Scholar] [CrossRef]
- Nicholson, L.L.; Chan, C.; Tofts, L.; Pacey, V. Hypermobility syndromes in children and adolescents: Assessment, diagnosis and multidisciplinary management. Aust. J. Gen. Pract. 2022, 51, 409–414. [Google Scholar] [CrossRef] [PubMed]
- Winter, D.A. Biomechanics and Motor Control of Human Movement, 4th ed.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2009. [Google Scholar]
- Chiodelli, L.; Pacheco, A.B.; Missau, T.S.; Silva, A.M.T.; Corrêa, E.C.R. Influence of generalized joint hypermobility on temporomandibular joint, mastication and deglutition: A cross-sectional study. Rev. CEFAC 2015, 17, 890–898. [Google Scholar] [CrossRef]
- Kapandji, A.I. Fisiologia Articular. Vol. 3. Esquemas Comentados de Mecânica Humana, 6th ed.; Guanabara Koogan: São Paulo, Brazil, 2009. [Google Scholar]
- Whiting, W.C.; Zernicke, R.F. Biomechanics of Musculoskeletal Injury, 2nd ed.; Guanabara Koogan: Rio de Janeiro, Brazil, 2008. [Google Scholar]
- Williams, C.M.; Welch, J.J.; Scheper, M.; Tofts, L.; Pacey, V. Variability of joint hypermobility in children: A meta-analytic approach to set cut-off scores. Eur. J. Pediatr. 2024, 183, 3517–3529. [Google Scholar] [CrossRef] [PubMed]


| Group | n | Mean () | Standard Deviation (s) | CV (%) | Median | Range | p-Value Mann–Whitney U Test |
|---|---|---|---|---|---|---|---|
| Total | 124 | 6.70 | 1.76 | 26.2 | 7.0 | 2.0–9.0 | |
| Female | 74 | 6.95 | 1.73 | 24.9 | 7.0 | 2.0–9.0 | 0.046 |
| Male | 50 | 6.34 | 1.76 | 27.7 | 6.0 | 2.0–9.0 |
| Sex | BS ≤ 6 | BS > 6 | Total |
|---|---|---|---|
| Female | 29 (39.2%) | 45 (60.8%) | 74 |
| Male | 30 (60.0%) | 20 (40.0%) | 50 |
| p-value = 0.024 (Fisher’s test) | |||
| Sitting Position (n) | Female | Male |
|---|---|---|
| S (n = 18) | 11 (61.1%) | 07 (38.9%) |
| W (n = 48) | 29 (60.4%) | 19 (39.6%) |
| F (n = 28) | 17 (60.7%) | 11 (39.3%) |
| C (n = 70) | 38 (54.3%) | 32 (45.7%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lamari, M.M.; Lamari, N.M.; de Medeiros, M.P.; de Araújo Filho, G.M.; Santos, A.B.; Giacomini, M.G.; Marques, V.R.P.; Goloni-Bertollo, E.M.; Pavarino, É.C. Phenotypic Presentation of Children with Joint Hypermobility: Preclinical Signs. Children 2025, 12, 109. https://doi.org/10.3390/children12010109
Lamari MM, Lamari NM, de Medeiros MP, de Araújo Filho GM, Santos AB, Giacomini MG, Marques VRP, Goloni-Bertollo EM, Pavarino ÉC. Phenotypic Presentation of Children with Joint Hypermobility: Preclinical Signs. Children. 2025; 12(1):109. https://doi.org/10.3390/children12010109
Chicago/Turabian StyleLamari, Mateus Marino, Neuseli Marino Lamari, Michael Peres de Medeiros, Gerardo Maria de Araújo Filho, Adriana Barbosa Santos, Matheus Gomes Giacomini, Vitor Roberto Pugliesi Marques, Eny Maria Goloni-Bertollo, and Érika Cristina Pavarino. 2025. "Phenotypic Presentation of Children with Joint Hypermobility: Preclinical Signs" Children 12, no. 1: 109. https://doi.org/10.3390/children12010109
APA StyleLamari, M. M., Lamari, N. M., de Medeiros, M. P., de Araújo Filho, G. M., Santos, A. B., Giacomini, M. G., Marques, V. R. P., Goloni-Bertollo, E. M., & Pavarino, É. C. (2025). Phenotypic Presentation of Children with Joint Hypermobility: Preclinical Signs. Children, 12(1), 109. https://doi.org/10.3390/children12010109






