Abstract
Background and Objectives: There is no standardised approach to toilet training in children. This study aimed to determine the factors affecting the duration of toilet training in children aged 0–5 years and to develop a tool to assess the child’s readiness to start toilet training. Materials and Methods: This cross-sectional study was conducted on 409 children aged 0–5 years. Social, economic, behavioural, and developmental characteristics that are effective in toilet training in healthy children were evaluated. A scale assessing children’s readiness for toilet training (Toilet Training Readiness Scale-TTRS) was developed and content validated. Results: The mean age of the 409 children included in this study was 44.69 ± 13.07 months (min = 4; max = 60 months). The mean age of initiation of toilet training was 26.8 months. Most frequently, urine and faeces trainings were started together (52.1%). In the logistic regression analysis performed to evaluate the factors affecting the duration of toilet training, it was found that the TTRS score, mother’s employment status, family type, child’s first reaction, toilet type, and continuity of training were important predictors. The duration of toilet training showed a weak negative correlation with the scores obtained from the TTRS and the number of children in the family but a weak positive correlation with the age at the beginning of toilet training. The TTRS scores were inversely proportional to the duration of toilet training. Conclusions: Family characteristics, socioeconomic conditions, and readiness of the child for and no interruption in toilet training are important in completing toilet training in a short time and successfully. If a child-focused approach is adopted, evaluating the child from this point of view and initiating the training at the appropriate time may help to complete a more successful and shorter toilet training. We recommend that the scale we have developed be studied in other studies and different groups.
1. Introduction
Toilet training is defined as the child being aware of the need to pass urine and faeces and being able to initiate the action without being reminded or prepared by the parents [1,2]. Generally, starting before 2 years (24 months) of age is not recommended [1].
The preparation skills and physical development the child requires to undertake successful toileting, usually occur between 18 months and 2.5 years of age. Current acceptance worldwide is that toilet training should be introduced to children between the ages of 2 and 3 years [1]. The American Academy of Paediatrics and the Canadian Paediatric Society report that the most physiologically, cognitively, and behaviourally appropriate time to start toilet training is between 18 and 24 months [3,4]. In children with typical development, the skills of recognising people, imitation, controlling simple stimuli and developing autonomy are completed between the ages of 2 and 3 years. Whether the children are ready for toilet training can be deducted from their cognitive and psychological reactions to their parents [5,6]. The readiness can be evaluated via physical, cognitive, and emotional aspects. Physical signs encompass a child’s physiological and motor abilities like control of sphincters and ability to perform gross motor skills such as walking, sitting, and squatting comfortably. Cognitive development accelerates as children begin to explore the outside world and themselves, these cognitive signs include understanding what is said, following simple instructions, and being able to say words related to the bathroom (toilet, sink, soap, toilet paper, etc.). Emotional aspects are signs such as the child being uncomfortable when his/her nappy is dirty, asking for it to be changed or trying to take it off himself/herself, wanting to be liked by the parents, striving to get reward or praise, turning towards the toilet or bathroom when he/she needs to use the toilet and wanting to use it [5,6,7]. Studies on toilet training in children are limited in the literature. However, many parents need guidance from their physicians on how best to fulfil this training. Psychological theories, paediatric recommendations, and parental practices related to toilet training have changed considerably in the last century [8]. In the last 50 years, the ages of initiation and completion of toilet training for children with normal neuropsychomotor development have been delayed from 18 months to 24–36 months and from 24 months to 36–39 months, respectively [9,10]
At the beginning of the twentieth century, toilet training, which was expected to develop naturally in line with the mother’s instincts, underwent a sharp transformation with the development of the behaviourist approach [11]. Two main classifications of toilet training have been used: the child-focused approach and the structured behavioural approach. Most children were trained with the structured behavioural approach starting early, but by the time toilet training was completed, they were similar in age to those using the child-focused approach. In the few reported studies, success rates were better with the child-focused approach. The lowest success rate was reported with the daytime dampness alarm approach. There is no consensus on the best method to use, as this depends on parental preferences, expectations, and cultural differences [12].
The duration of toilet training is affected by multiple factors which can be grouped as follows:
- (a)
- Personal factors: sex and age of the child or the age and educational status of the parents and the psychological status of the child;
- (b)
- Socio-demographic factors: the family and environment where the child lives, the place of residence, and the socioeconomic status of the family;
- (c)
- Educators/caregivers: family or non-family members at home or nursery school; how much information the educator has about toilet training; and the attitude of the parents during toilet training;
- (d)
- Methods and tools: the style of the toilet, i.e., Western (also named as sitting or flush toilet) versus Oriental (also known as squat); location of the toilet: inside or outside the house; and the methods and tools used in toilet training.
Health conditions such as chronic diseases may render the process more difficult [13,14,15].
In this study, it was aimed to determine the cognitive, behavioural, and sociocultural factors affecting the duration of toilet training in children aged 0–5 years who applied to the social paediatrics outpatient clinic in a university hospital and to develop a scale, i.e., a form that will assess the child’s readiness to start toilet training that can help clinicians during the counselling process given to families.
2. Materials and Methods
2.1. Study Type, Place, and Time
This cross-sectional study conducted between April 2023 and April 2024 included the mothers of children between 0 and 60 months of age who had completed toilet training with their children or whose toilet training was still ongoing and who applied to the child health follow-up outpatient clinic of the Department of Social Paediatrics at the Faculty of Medicine of Çukurova University in Adana, Turkey.
2.2. Sampling
The sample size analysis with d = 0.1, 1 − β = 0.95, and α = 0.01 revealed the minimum sample size to be reached in the study as 391. Participants were reached using a convenience sampling method. The questionnaire form was filled face-to-face, and the evaluation of each participant took an average of 30 min. This study was completed with 409 participants.
-Inclusion criteria: parents of children born at term and children who did not have any chronic diseases were included in this study after having signed a written consent form;
-Exclusion criteria: children with a history of premature birth, physical or mental disability, and anomalies that might affect bladder function and anal emptying were excluded from this study.
2.3. Ethics
Ethical approval was obtained from the Non-interventional Clinical Research Ethics Committee of the Faculty of Medicine at Çukurova University (decree no: 16, meeting no: 111, dated 21 May 2021).
2.4. Questionnaire Form
The form consisted of questions regarding the sociodemographic characteristics of mothers and children, in addition to the scale designed to determine the signs of children’s readiness for toilet training and the attitudes and behaviours of mothers towards this training.
Although there is no consensus on when a child is considered fully trained, it is defined as when he/she is aware of his/her own need to eliminate urine and stool and initiates the act without being remembered or prepared by parents or caregivers. In our study, while questioning the completion of toilet training, we took into consideration whether the child spent the night dry, whether the child went to the toilet by controlling faeces and urine during the day and whether the child was completely weaned from the nappy [2].
2.5. Toilet Training Readiness Scale (TTRS)
The scale we have developed consists of 10 content-validated questions that aim to evaluate children’s readiness for toilet training physiologically, cognitively, and psychologically [5].
Content Validity
- Creating an Item Pool:
A questionnaire consisting of 15 questions evaluating the developmental characteristics of a child was created by the researchers based on their clinical observations and the literature to evaluate the readiness of children for toilet training [16,17]. The items were expressed as positive or negative, and the scale items were expressed in understandable language. Care was taken not to have more than one meaning in an item. The answers to the statements used in the scale consisted of “yes” or “no”.
- Content Validity (Expert Opinion)
Validity is a concept related to the extent to which the instrument (which is a scale in our study) accurately measures the desired characteristic in question. The content validity is the indicator of whether the items constituting the instrument are sufficient in terms of quantity and quality to measure the behaviour in question. One of the frequently used methods to test content validity is seeking expert opinions [18]. In our study, the 15-item draft scale was sent to five faculty member paediatricians. How this number was calculated is explained below.
- Calculation of Content Validity Ratio (CVR) and Content Validity Index (CVI)
The content validity ratio (CVR) is an internationally recognised item statistic to determine content validity; in other terms, it is used to decide whether to include or reject an individual item in any measurement tool [15]. It is calculated with the following formula:
where Nu indicates the number of experts who evaluated the item as “essential”, and N indicates the total number of experts who expressed any opinion (“essential”, “useful, but not essential”, or “not necessary” on this item. The CVR has a value between −1 (perfect disagreement) and +1 (perfect agreement). If all participants rate any item in the scale as “essential”, the CVR value of that item becomes 1. If the CVR takes a 0 (zero) or negative (less than zero) value, it means that the item with such a value does not have content validity, and all such items in the scale are promptly eliminated [19,20,21]. Ayre and Scally (2014) pointed out that if the number of experts participating in the study increased or decreased even by one person, the critical values of the CVRs would change and proposed a table to determine the critical (minimum acceptable) CVR (CVRcritical) by using different statistical analyses with α (Type I error probability) set to 0.05. To summarise, this table gave the minimum number of experts required to agree that an item was essential and thus which items should be included or discarded from the final instrument could be determined [20].
When the hypotheses proposed by Lawshe [21], Wilson et al. [19], and Ayre and Scally [20] were evaluated together, the common consensus was to use the aforementioned table of Ayre and Scally, where CVRcritical was reported as 1.00 when the panel included five experts and α = 0.05 is the significance level [21]. In our study, 5 items were removed because they had zero or negative values with a resulting total of 10 items being accepted in terms of content validity in the final version of our scale. The content validity index (CVI) is the mean of CVRs of all the items included in the tool [22]. Assuming that the draft scale used in our study had a single dimension, the CVI value for 10 items was calculated as 1 for a single dimension. Since CVI = 1, the scale could be assessed as valid in terms of content. The questions of the scale are given in Table 1. After the content was validated, the scale was administered to the families. Parents were asked to answer “yes” or “no” to each question. The answer “yes” was scored as “1 point” while “no” was scored as “0 points”. Thus, the total score on the scale ranged between 0 and 10. Increased scores were interpreted in favour of more likely readiness for toilet training. The reliability analysis revealed a Cronbach alpha value of 0.567.

Table 1.
Toilet Training Readiness Scale questions.
2.6. Statistical Analyses
SPSS 20.0 (IBM Corp., Armonk, NY, USA) and JAMOVI 2.3 [23] software were used for data analysis. The chi-square test, binary logistic regression, multinominal logistic regression, mediation, Spearman correlation, and ROC analyses were used. A p < 0.05 value was considered statistically significant.
3. Findings
The mean age of the 409 children included in our study was 44.69 ± 13.07 months (min = 4; max = 60). The mean age for toilet training initiation was 26.8 months. Females constituted 50.6% of the children. Sociodemographic data of the children and their families are given in Table 2.

Table 2.
Characteristics of children and families.
A total of 66.7% of the mothers started toilet training because they thought that their child was ready. Most frequently, trainings were started together for both urine and faeces (52.1%). The duration of training was 2–7 days for 24.4% of the children and 8–15 days for 27.9%. Most of the children were enthusiastic on the first attempt (64.1%). The most preferred toilet type was the Oriental (also known as squat) style. Other information about the toilet training process of the families is given in Table 3.

Table 3.
Distribution of characteristics related to toilet training.
A significant logistic regression model (Forward LR method) was constructed (omnibus test p < 0.001). The explanatory power of the model was 27.3%, and the accuracy rate was 72.8%. Among the variables included in the model, TTRS score, mother’s employment status, family type, child’s first reaction, toilet type, and continuity of training were found to be significant. The probability of completion of toilet training in less than 15 days was found to be 2.69-times higher in children with mothers who were employed, 2.09-times higher for those who lived in nuclear families, 2.79-times higher for children whose first reaction was enthusiastic, 6.89-times higher for those who used a Western-style toilet, 3.68-times higher for those trained in the Oriental style, 3.86-times higher for potty users, and 4.22-times higher for those whose toilet training was not interrupted. Each one-unit increase in the TTRS score increased by 1.30 times the probability of the duration of toilet training being shorter than 2 weeks (Table 4).

Table 4.
Logistic regression analysis for prediction of toilet training duration *.
When the correlations between the TTRS score and duration of toilet training, mother’s age, number of children, and age at the beginning of toilet training were examined, TTRS scores were found to show a significant weak correlation in the negative direction with the duration of toilet training or with the number of children but a significant weak correlation in the positive direction with the age at the beginning of toilet training. There was also a weak positive correlation between the number of children and the duration of toilet training (Table 5). The optimum cut-off value for the TTRS developed in our study was found to be 6 (Table 6, Figure 1).

Table 5.
Various correlations with Toilet Training Readiness Scale scores *.

Table 6.
Optimum cut-off values of Toilet Training Readiness Scale scores.
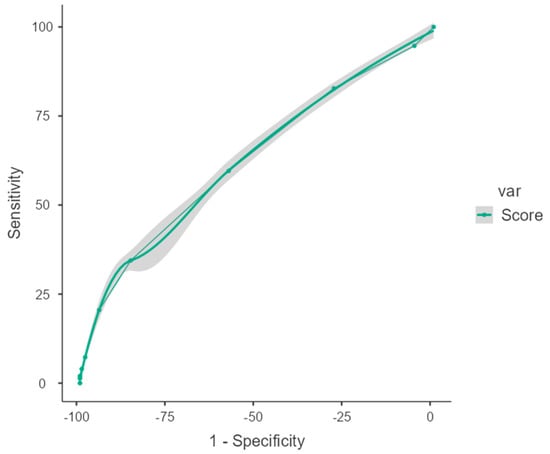
Figure 1.
ROC analysis of Toilet Training Readiness Scale scores (area under the curve).
The scores obtained from the Toilet Training Readiness Scale were classified according to the optimum cut-off value that we found in our study, and their effect on the duration of toilet training was evaluated. It was found that the probability of completing toilet training in a period longer than 1 month increased by 5.43 times in children who had a score below 6 (Table 7).

Table 7.
Multinomial logistic regression analysis predicting the duration of toilet training.
4. Discussion
Although toilet training is a challenging experience for parents and children, it constitutes one of the most important developmental stages of childhood. The initiation and completion of toilet training is under the influence of many facilitating and inhibiting factors [24]. In this study, the factors that are effective in toilet training in children aged 0–5 years were evaluated, and a scale was developed to assess the child’s readiness for toilet training (TTRS; Toilet Training Readiness Scale). In our study, the mean age at toilet training initiation was 26.8 months. The important predictors of the duration of toilet training in children were TTRS score, mother’s employment status, family type, child’s first reaction, toilet type, and continuity of training. There was a significant weak negative correlation between the TTRS score and the duration of toilet training, while there was a significant weak positive correlation with the age at toilet training initiation.
In the study conducted by Koç et al., the mean age of initiation of toilet training was 22.05 ± 6.73 months. The completion age was later in infants whose mothers had 12 years or more of education compared to the others, and the earliest completion age was observed in families using the punishment method. The duration of education was found to be longer in families living in rural and semi-urban settlements, in mothers with less than 5 years of education, in unemployed mothers, in children living in houses without indoor bathrooms, and in families using reusable washable nappies [14]. In the study conducted by Netto et al., it was found that prematurity and mothers working away from the home delayed toilet training [25]. In our study, it was found that the working status of the mother was significantly impactful, and the duration of toilet training was shorter in working mothers. This may be related to the social change over time. It may be related to working women being more conscious or sharing experiences and exchanging ideas with other mothers on these issues and being aware of correct practices. The fact that working mothers spend less but more productive time with their children than non-working mothers may also be one of the explanatory factors of this situation. In the study conducted by Önen et al., the duration of toilet training in children under five years of age was found to be lower in families with low-income levels and children living in nuclear families. The duration of toilet training was found to be longer in those who started toilet training before 18 months of age or later than 30 months, in those living in slums, and in those who experienced an event affecting their psychology compared to other groups [26]. Mrad et al. examined the effect of the child-focused toilet training method approach in children with Down syndrome and children with normal psychomotor development and found that the duration of toilet training was longer in children with Down syndrome [27]. In a cohort study conducted by Mota et al. on a total of 3281 children born in Brazil, it was found that mothers with a longer education period and from higher social class weaned their children from nappies later. The probability of nappy weaning increased when the number of children living at home was higher (RR = 1.32) and the child could communicate the need to go to the toilet to others (RR = 11.74) [28]. In the study conducted by Kural and Köse, it was found that the ages of children who encountered problems in toilet training were higher than those without problems. The rate of problems in toilet training in boys was found to be statistically significantly higher than that in girls. The rate of problems in toilet training of preterm children was higher than that of term children. Refusal of toilet training was found to be significantly higher in children with developmental language and speech delays [29]. The common finding of our study and these studies was the relationship between child development and toilet training success. There were no consistent findings between socioeconomic factors and toilet training, and the period in which the studies were conducted and the social characteristics might explain this. However, it is noteworthy that there was a close relationship between the developmental characteristics of the child and the duration and success of toilet training.
In the study conducted by Blum et al., advanced age at the beginning of toilet training, refusal to defecate and constipation were found to be predictors of the tendency to complete toilet training at a later age [30]. Vermendal et al. compared gradual child-focused education and structured endpoint-focused toilet training in healthy children. It was emphasised that there was no consensus on the most appropriate age to start toilet training or the expected average age to complete the training in the literature reviewed, where studies focusing on this subject were very few. Recent studies showed that children completed toilet training much later than previous generations. It was reported that the child started training between 24 and 36 months, and the current trend was completed later than previous generations [31]. In the study conducted by Kaerts et al., signs of readiness for toilet training were analysed, and 21 signs of readiness were identified: the child 1. could imitate behaviour, 2. could sit steadily and without assistance, 3. could walk without assistance, 4. could pick up small objects, 5. could say “no” as a sign of independence, 6. had voluntary control over bowel and bladder reflex actions, 7. could understand and respond to instructions, questions, or explanations and fulfil simple commands, 8. could express the need to evacuate through non-verbal communication (imitation, posture, or gestures, such as going to the toilet or grabbing the potty) or words, 9. could often indicate his/her trousers to be wet/dirty, 10. enjoyed putting things in containers, 11. had awareness of bladder sensations and the need to urinate, 12. understood toilet-related words and had a sufficient vocabulary of his/her own, 13. wanted to participate in toilet training, cooperated and showed interest in toilet training, 14. had a larger bladder capacity, 15. insisted on completing tasks without help and was proud of new skills, 16. wanted the potty to be clean and was uncomfortable with wet or dirty nappies, 17. wanted to wear adult clothes, 18. could pull his/her clothes up and down, 19. stayed overnight without bowel movements, 20. began to put things back where they belonged, and 21. the child could sit still on the potty for 5–10 min. The researchers emphasised that there was no consensus on which or how many signs of readiness to use. According to the signs of readiness, the moment of initiating toilet training can vary greatly. More studies were needed to define which readiness signs were the most important and how they could be easily detected [6].
Although there are various methods of toilet training, it is not clear when the right time to start training is, and this varies from child to child. There are many signs indicating that children are ready for toilet training. However, there is no consensus on any of them, and there is no clear attitude on deciding which one is the most important. Based on this, in our study, a child-centred scale was developed to objectively determine the readiness of children for toilet training where multiple signs were evaluated. The increase in the scores obtained from this scale was found to be associated with the shortness of toilet training. Scores of 6 and above indicated that the child was ready to start and successfully complete toilet training. It was found that the probability of completing toilet training in a longer period of time (more than one month) increased by 5.43 times in children who scored below 6 on the scale. In addition, the 10th item on the scale, “My child feels discomfort after defecating in his/her nappy/diaper” was found to be the most important predictor of toilet training success. Preparation for initiation of toilet training depends on the individual situation of the child [16]. There is no right age for giving toilet training to a child; the scale developed in our study may help clinicians to objectively evaluate whether healthy children aged 0–5 years are ready for toilet training.
Toilet training is a universal challenge for children, parents, and doctors. Although parents and physicians have addressed this issue for generations, there is still no consensus on the best method or even a standardised definition of toilet training. This uncertainty is partly due to the wide range of parental preferences and expectations regarding toilet training. In addition, few studies compared the effectiveness of different strategies, which limited the ability of physicians to make evidence-based recommendations. For these reasons, toilet training remains a complex behavioural and developmental stage with a variety of acceptable approaches and methods [32]. Many toilet training methods are available. The American Academy of Paediatrics recommends a child-centred approach for toilet training, which means that it should be started when the child is physically and psychologically ready [5,10,33], which is also the main approach in our study.
In the follow-up of healthy children, caregivers of children under 5 years of age should be informed about the importance of toilet training, clues indicating readiness for toilet training, and positive approaches/methods. The results of our study allow these evaluations to be made more objectively. There is no consensus on the criteria for preparation for and success of toilet training. Our study will guide the literature and parents and health professionals in terms of evaluating the readiness for toilet training in children under 5 years of age.
Although the readiness of healthy children for toilet training was evaluated from a neuropsychomotor perspective in our study, sometimes a delay in toilet training may be a harbinger of abnormal conditions. Further consideration of parent–child communication, children’s development and level of toilet skills may contribute to the development of toilet training approaches that better meet the needs of families of children with disorders such as autism spectrum disorder [34,35].
5. Conclusions
Our results show that family characteristics, socioeconomic and cultural conditions, signs of readiness in the child’s physical and mental development, and the absence of interruption in toilet training are important in completing toilet training shortly and successfully. If a child-oriented approach is adopted, evaluating the child in this respect and starting education at the appropriate time may help to complete a more successful and shorter toilet training. A score of 6 and above obtained on the scale we developed indicates that the child is physically and mentally ready for toilet training. Children who score below 6 on the scale are 5.4 times more likely to complete toilet training in more than 1 month. We recommend that the validity of the scale we developed—Toilet Training Readiness Scale—be investigated in clinics in different cultures and societies also including children with physical or mental development problems and that our results be compared with other studies.
Author Contributions
Conceptualization, A.B, B.M., H.D., S.B., A.K. and N.E.; methodology, A.B., B.M., H.D., S.B., A.K. and N.E.; software, A.B., B.M. and H.D.; formal analysis, A.B., B.M., H.D., S.B., A.K. and N.E.; investigation, A.B. and B.M.; resources, A.B.; data curation, A.B., B.M. and H.D.; validation, A.B., B.M. and H.D.; writing—original draft preparation, A.B., B.M., H.D. and S.B.; writing—review and editing, A.B., B.M., H.D., S.B., A.K. and N.E.; visualisation, B.M.; supervision, A.B., B.M. and H.D.; project administration, A.B. All authors have read and agreed to the published version of the manuscript.
Funding
This study has not received any financial support.
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki and approved by the Ethical Review Board for Non-interventional Studies of Cukurova University Faculty of Medicine, Adana, Türkiye (Date 21 May 2021-Meeting No:111-Decree No:16). All participants gave written informed consent to participate in this study.
Informed Consent Statement
Informed consent was obtained from all patients and their relatives for the data used in this study.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Luxem, M.; Christophersen, E. Behavioral toilet training in early childhood: Research, practice, and implications. J. Dev. Behav. Pediatr. 1994, 15, 370–378. [Google Scholar] [CrossRef]
- Mota, D.M.; Barros, A.J.D. Toilet training: Methods, parental expectations and associated dysfunctions. J. De Pediatr. 2008, 84, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Clifford, T.; Gorodzinsky, F.P. Toilet learning: Anticipatory guidance with a child-oriented approach. Paediatr. Child Health 2000, 5, 333–335. [Google Scholar] [CrossRef][Green Version]
- Stadtler, A.C.; Gorski, P.A.; Brazelton, T.B. Toilet Training Methods, Clinical Interventions, and Recommendations. Pediatrics 1999, 103, 1359–1361. [Google Scholar] [CrossRef] [PubMed]
- Brazelton, T.B. A child-oriented approach to toilet training. Pediatrics 1962, 29, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Kaerts, N.; Van Hal, G.; Vermandel, A.; Wyndaele, J. Readiness signs used to define the proper moment to start toilet training: A review of the literature. Neurourol. Urodyn. 2012, 31, 437–440. [Google Scholar] [CrossRef]
- Wilson, D. Family-Centered Care of The Young Child. In Wong’s Nursing Care of Infants and Children; Hockenberry, M.J., Wilson, D., Eds.; Mosby: St. Louis, MI, USA, 2011; pp. 564–567. [Google Scholar]
- Martin, J.A.; King, D.R.; Maccoby, E.E.; Jacklin, C.N. Secular trends and individual differences in toilet-training progress. J. Pediatr. Psychol. 1984, 9, 457–468. [Google Scholar] [CrossRef] [PubMed]
- Tarhan, H.; Çakmak, Ö.; Akarken, İ.; Ekin, R.G.; Ün, S.; Uzelli, D.; Helvacı, M.; Aksu, N.; Yavaşcan, Ö.; Mutlubaş Özsan, F. Toilet training age and influencing factors: A multicenter study. Turk. J. Pediatr. 2015, 57, 172–176. [Google Scholar]
- Colaco, M.; Johnson, K.; Schneider, D.; Barone, J. Toilet Training Method Is Not Related to Dysfunctional Voiding. Clin. Pediatr. 2013, 52, 49–53. [Google Scholar] [CrossRef]
- Stendler, C.B. Sixty years of child training practices; revolution in the nursery. J. Pediatr. 1950, 36, 122–134. [Google Scholar] [CrossRef]
- de Carvalho Mrad, F.C.; da Silva, M.E.; Moreira Lima, E.; Bessa, A.L.; de Bessa Junior, J.; Netto, J.M.B.; de Almeida Vasconcelos, M.M. Toilet training methods in children with normal neuropsychomotor development: A systematic review. J. Pediatr. Urol. 2021, 17, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Taubman, B.; Blum, N.J.; Nemeth, N. Stool toileting refusal: A prospective intervention targeting parental behavior. Arch. Pediatr. Adolesc. Med. 2003, 157, 1193–1196. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Koc, I.; Camurdan, A.D.; Beyazova, U.; Ilhan, M.N.; Sahin, F. Toilet training in Turkey: The factors that affect timing and duration in different sociocultural groups. Child Care Health Dev. 2008, 34, 475–481. [Google Scholar] [CrossRef] [PubMed]
- Frauman, A.C.; Brandon, D.H. Toilet training for the child with chronic illness. Pediatr. Nurs. 1996, 22, 469–472. [Google Scholar]
- Gorski, P.A. Toilet Training Guidelines: Parents-The Role of the Parents in Toilet Training. Pediatrics 1999, 103 (Suppl. S3), 1362–1363. [Google Scholar]
- American Academy of Family Physicians. Toilet Training: Information from Your Family Doctor. 2019. Available online: https://pubmed.ncbi.nlm.nih.gov/31613579/ (accessed on 7 July 2024).
- Büyüköztürk, Ş. Sosyal Bilimler Için Veri Analizi El Kitabı, 31st ed.; Pegem Akademi: Ankara, Turkey, 2024; Available online: www.pegem.net (accessed on 7 July 2024).
- Wilson, F.R.; Pan, W.; Schumsky, D.A. Recalculation of the Critical Values for Lawshe’s Content Validity Ratio. Meas. Eval. Couns. Dev. 2012, 45, 197–210. [Google Scholar] [CrossRef]
- Ayre, C.; Scally, A.J. Critical Values for Lawshe’s Content Validity Ratio. Meas. Eval. Couns. Dev. 2014, 47, 79–86. [Google Scholar] [CrossRef]
- Lawshe, C.H. A quantitative approach to content validity. Pers. Psychol. 1975, 28, 563–575. [Google Scholar] [CrossRef]
- DeVon, H.A.; Block, M.E.; Moyle-Wright, P.; Ernst, D.M.; Hayden, S.J.; Lazzara, D.J.; Savoy, S.M.; Kostas-Polston, E. A Psychometric Toolbox for Testing Validity and Reliability. J. Nurs. Scholarsh. 2007, 39, 155–164. [Google Scholar] [CrossRef]
- Jamovi 2.3. 2023. Available online: https://www.jamovi.org (accessed on 25 July 2023).
- Van Aggelpoel, T.; De Wachter, S.; Van Hal, G.; Van der Cruyssen, K.; Neels, H.; Vermandel, A. Parents’ views on toilet training: A cross-sectional study in Flanders. Nurs. Child. Young People 2018, 30, 30–35. [Google Scholar] [CrossRef]
- Netto, J.M.B.; de Paula, J.C.; Bastos, C.R.; Soares, D.G.; de Castro, N.C.T.; Sousa, K.K.D.V.; do Carmo, A.V.; de Miranda, R.L.; Mrad, F.C.C.; de Bessa, J., Jr. Personal and familial factors associated with toilet training. Int. Braz. J. Urol. Off. J. Braz. Soc. Urol. 2021, 47, 169. [Google Scholar] [CrossRef] [PubMed]
- Önen, S.; Aksoy, I.; Taşar, M.A.; Bilge, Y.D. Factors that affect toilet training in children. Med. J. Bakirkoy 2012, 8, 111–115. [Google Scholar] [CrossRef]
- Mrad, F.C.C.; Figueiredo, A.A.; Bessa, J., Jr.; Bastos Netto, J.M. Prolonged toilet training in children with Down syndrome: A case-control study. J. Pediatr. 2018, 94, 286–292. [Google Scholar] [CrossRef]
- Mota, D.M.; Barros, A.J.D. Toilet training: Situation at 2 years of age in a birth cohort. J. Pediatr. 2008, 84, 455–462. [Google Scholar] [CrossRef]
- Kural, B.; Köse, S. Factors Affecting Toilet Training in Children: A 10 Year Experience. J. Child 2022, 22, 178–184. [Google Scholar]
- Blum, N.J.; Taubman, B.; Nemeth, N. Why is toilet training occurring at older ages? A study of factors associated with later training. J. Pediatr. 2004, 145, 107–111. [Google Scholar] [CrossRef]
- Vermandel, A.; Van Kampen, M.; Van Gorp, C.; Wyndaele, J.J. How to toilet train healthy children? A review of the literature. Neurourol. Urodyn. 2008, 27, 162–166. [Google Scholar] [CrossRef]
- Howell, D.M.; Wysocki, K.; Steiner, M.J. Toilet training. Pediatr. Rev. 2010, 31, 262–263. [Google Scholar] [CrossRef] [PubMed]
- Choby, B.A.; George, S.; Jacinto, S. Toilet Training. Am. Fam. Physician 2008, 78, 1059–1064. [Google Scholar]
- Simon, M.; Wilkes-Gillan, S.; Chen, Y.-W.R.; Cordier, R.; Cantrill, A.; Parsons, L.; Phua, J.J. Toilet training interventions for children with autism spectrum disorder: A systematic review. Res. Autism Spectr. Disord. 2022, 99, 102049. [Google Scholar] [CrossRef]
- Cagliani, R.R.; Snyder, S.K.; White, E.N. Classroom Based Intensive Toilet Training for Children with Autism Spectrum Disorder. J. Autism Dev. Disord. 2021, 51, 4436–4446. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).