Development and Validation of a Realistic Neonatal Intestinal Jejunoileal Atresia Simulator for the Training of Pediatric Surgeons
Abstract
1. Introduction
2. Methods
2.1. Conceptualization and Preliminary Design of the Model
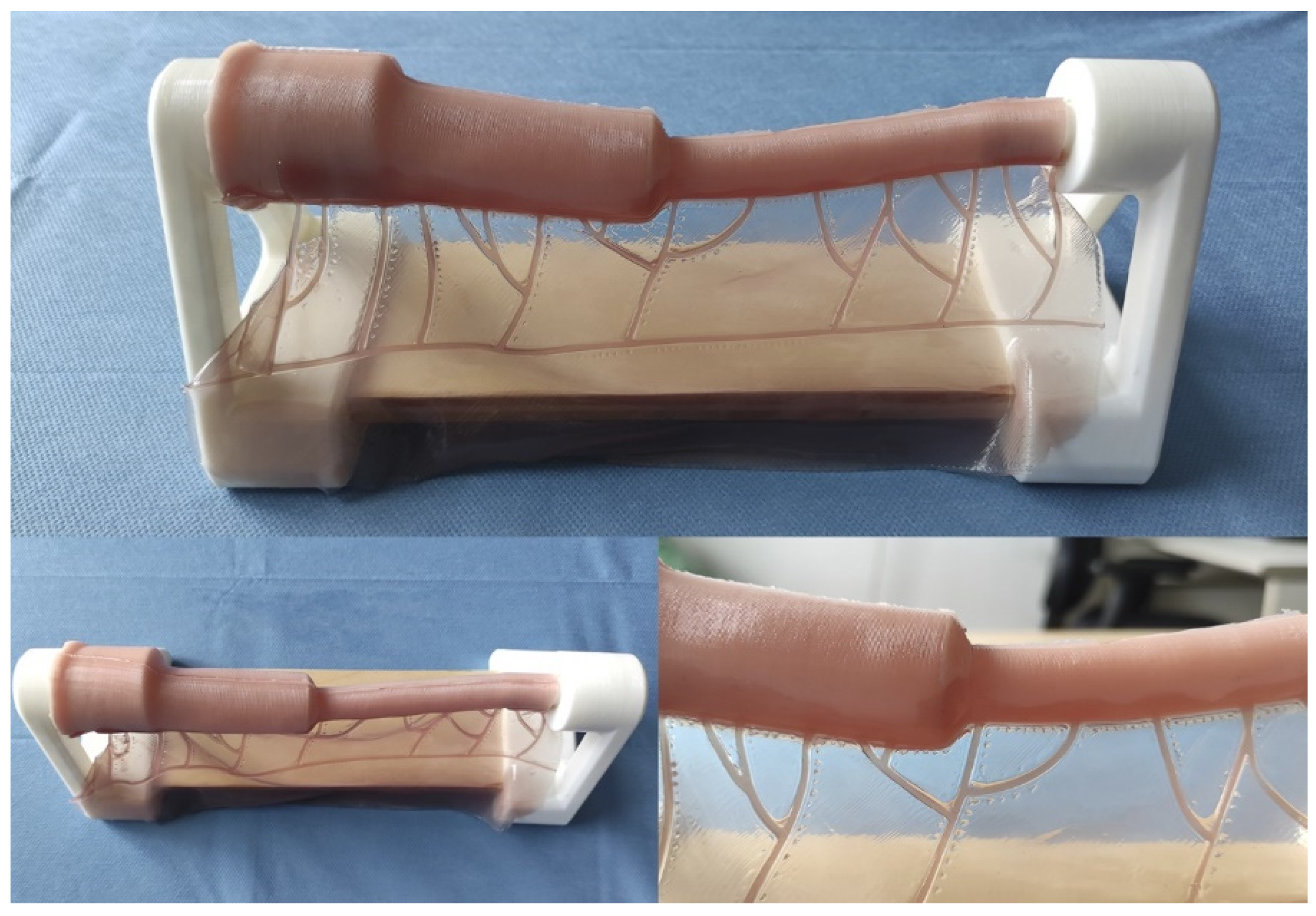
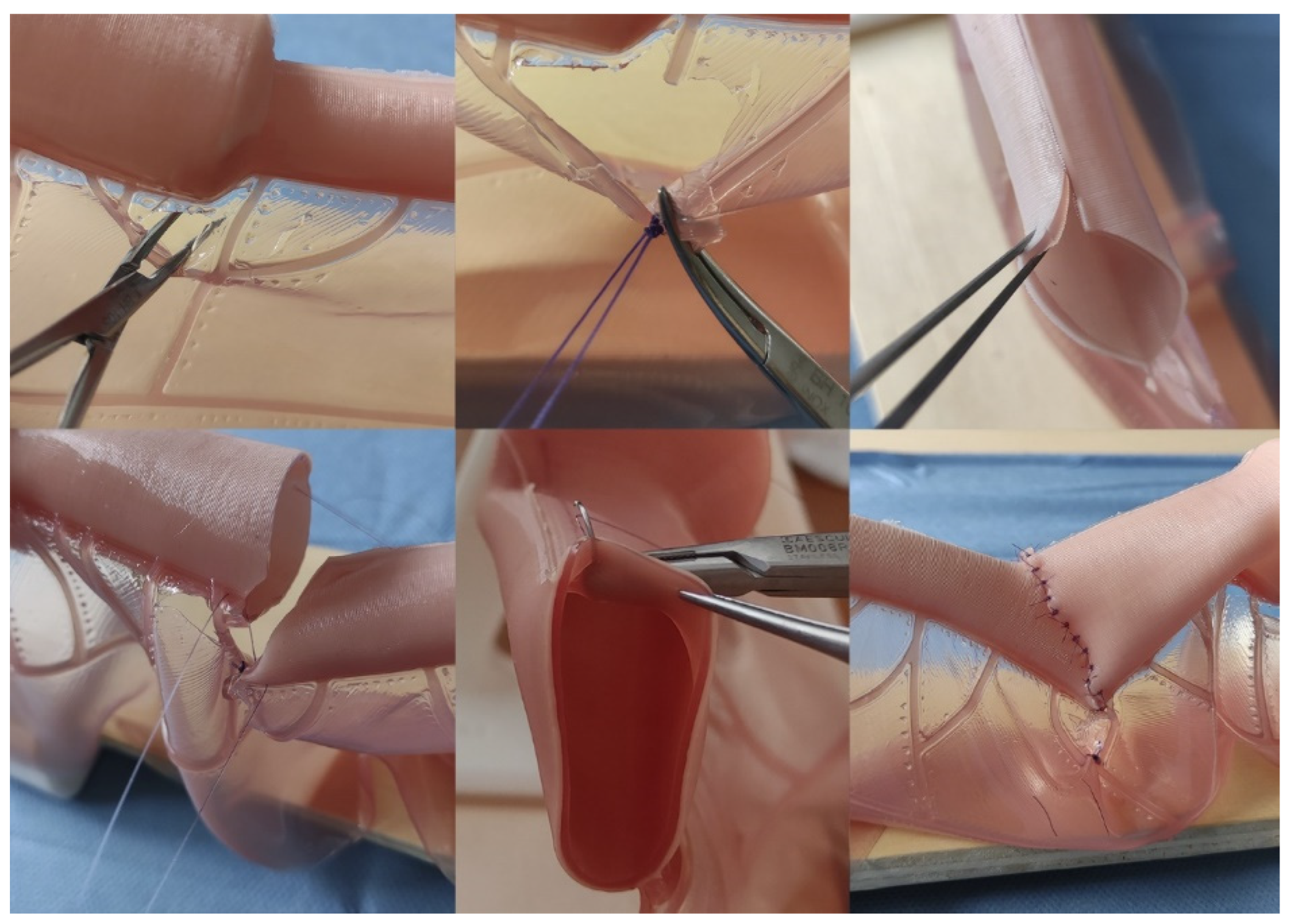
2.2. Model Production Methodology
2.3. The Final Version of the Model
2.4. Validation
2.5. Statistical Analysis
3. Results
3.1. Construct Validity
3.2. Face Validity
3.3. Content Validity
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Industrial Property
Acknowledgments
Conflicts of Interest
References
- Tovar, J.A. Pediatric Surgery remains the only true General Surgery. Porto Biomed. J. 2017, 2, 143–144. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Cummins, C.B.; Bowen-Jallow, K.A.; Tran, S.; Radhakrishnan, R.S. Education of pediatric surgery residents over time: Examining 15 years of case logs. J. Pediatr. Surg. 2021, 56, 85–98. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- ESHRE Capri Workshop Group. Europe the continent with the lowest fertility. Hum. Reprod. Update 2010, 16, 590–602. [Google Scholar] [CrossRef] [PubMed]
- Raboei, E.H. The role of the pediatric surgeon in the perinatal multidisciplinary team. Eur. J. Pediatr. Surg. 2008, 18, 313–317. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Xu, X.; Wang, X.; Zhao, L.; Lv, Y.; Chen, K. Laparoscopic versus open repair of congenital duodenal obstruction: A systematic review and meta-analysis. Pediatr. Surg. Int. 2022, 38, 1507–1515. [Google Scholar] [CrossRef] [PubMed]
- Lacher, M.; Barthlen, W.; Eckoldt, F.; Fitze, G.; Fuchs, J.; Hosie, S.; Kaiser, M.M.; Meyer, T.; Muensterer, O.J.; Reinshagen, K.; et al. Operative Volume of Newborn Surgery in German University Hospitals: High Volume Versus Low Volume Centers. Eur. J. Pediatr. Surg. 2022, 32, 391–398. [Google Scholar] [CrossRef] [PubMed]
- Sømme, S.; Shahi, N.; McLeod, L.; Torok, M.; McManus, B.; Ziegler, M.M. Neonatal surgery in low- vs. high-volume institutions: A KID inpatient database outcomes and cost study after repair of congenital diaphragmatic hernia, esophageal atresia, and gastroschisis. Pediatr. Surg. Int. 2019, 35, 1293–1300. [Google Scholar] [CrossRef] [PubMed]
- Farooqui, Z.; Cortez, A.R.; Potts, J.R., III; Tiao, G.M.; von Allmen, D.; Quillin, R.C., 3rd; Bondoc, A.J.; Garrison, A.P. 10 Year Analysis of Pediatric Surgery Fellowship Match and Operative Experience: Concerning Trends? Ann. Surg. 2023, 277, e475–e482. [Google Scholar] [CrossRef] [PubMed]
- Jhala, T.; Zundel, S.; Szavay, P. Surgical simulation of pediatric laparoscopic dismembered pyeloplasty: Reproducible high-fidelity animal-tissue model. J. Pediatr. Urol. 2021, 17, 833.e1–833.e4. [Google Scholar] [CrossRef] [PubMed]
- Gandra de Meira, M.L.; Buraschi Antunes, R.; de Oliveira Zani, V.; Dutra de Oliveira, G.; Generoso, D.; Ortolan, E.V.P.; Lourenção, P.L.T.A. Developing an Animal Model for Swenson Transanal Endorectal Pull-Through: A New Possibility for Training and Research Purposes. J. Investig. Surg. 2024, 37, 2376548. [Google Scholar] [CrossRef] [PubMed]
- Esposito, C.; Escolino, M.; Draghici, I.; Cerulo, M.; Farina, A.; De Pascale, T.; Cozzolino, S.; Settimi, A. Training Models in Pediatric Minimally Invasive Surgery: Rabbit Model Versus Porcine Model: A Comparative Study. J. Laparoendosc. Adv. Surg. Tech. A 2016, 26, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, S.; Miyano, G.; Tanaka, M.; Ikegami, M.; Kato, H.; Seo, S.; Ochi, T.; Koga, H.; Lane, G.J.; Takahashi, M.; et al. Cadaver Training for Minimally Invasive Pediatric Surgery: A Preliminary Report. J. Laparoendosc. Adv. Surg. Tech. A 2021, 31, 1485–1490. [Google Scholar] [CrossRef] [PubMed]
- Arredondo Montero, J.; Pérez Riveros, B.P.; Bueso Asfura, O.E.; Martín-Calvo, N.; Pueyo, F.J.; López de Aguileta Castaño, N. Development and validation of a realistic type III esophageal atresia simulator for the training of pediatric surgeons. Pediatr. Surg. Int. 2024, 40, 251. [Google Scholar] [CrossRef] [PubMed]
- Joosten, M.; de Blaauw, I.; Botden, S.M. Validated simulation models in pediatric surgery: A review. J. Pediatr. Surg. 2022, 57, 876–886. [Google Scholar] [CrossRef] [PubMed]
- Deonarain, A.R.; Harrison, R.V.; Gordon, K.A.; Looi, T.; Agur, A.M.R.; Estrada, M.; Wolter, N.E.; Propst, E.J. Synthetic Simulator for Surgical Training in Tracheostomy and Open Airway Surgery. Laryngoscope 2021, 131, E2378–E2386. [Google Scholar] [CrossRef] [PubMed]
- Takazawa, S.; Nishi, A.; Ishimaru, T.; Takahashi, M.; Sunouchi, T.; Kikuchi, K.; Koyama, R. Face and construct validity assessment of training models for intestinal anastomosis in low-birth-weight infants. Pediatr. Surg. Int. 2021, 37, 1765–1772. [Google Scholar] [CrossRef] [PubMed]
- Evetts, A.A.; Shkrum, M.J.; Tugaleva, E. Postmortem Body and Organ Measurements in Neonates and Infants: A Review of Reference Resources Used by Ontario Pathologists (Part 1). Am. J. Forensic Med. Pathol. 2016, 37, 179–182. [Google Scholar] [CrossRef] [PubMed]
- Evetts, A.M.; Shkrum, M.J.; Tugaleva, E. A New Reference Source for Postmortem Body Measurements and Organ Weights in Neonates and Infants: A Statistical Analysis Based on Sudden Death Classification (Part 2). Am. J. Forensic Med. Pathol. 2018, 39, 285–303. [Google Scholar] [CrossRef] [PubMed]
- Lap, C.C.; Voskuilen, C.S.; Pistorius, L.R.; Mulder, E.J.H.; Visser, G.H.A.; Manten, G.T.R. Reference curves for the normal fetal small bowel and colon diameters; their usefulness in fetuses with suspected dilated bowel. J. Matern. Fetal Neonatal Med. 2020, 33, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Gao, J.; Margonis, G.A.; Wang, J.J.; Yi, J.; Weng, X.; Lin, C.; Wang, W. Comparative Analysis of 2D and 3D Training Models for Emergency Appendectomy Among Surgical Residents: A Randomized Controlled Study. J. Gastrointest. Surg. 2024. [Google Scholar] [CrossRef] [PubMed]
- Recker, F.; Schremmer, T.; Berg, C.; Schäfer, V.S.; Strizek, B.; Jimenez-Cruz, J. Advancement of 3D printing technology for the development of a training model in US-guided vesicoamniotic shunting for early LUTO therapy. Acta Obstet. Gynecol. Scand. 2024, 103, 1550–1557. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Amstutz, C.; Ilic, M.; Fontaine, N.; Siegenthaler, L.; Illi, J.; Haeberlin, A.; Zurbuchen, A.; Burger, J. Development of a patient-specific model of the human coronary system for percutaneous transluminal coronary angioplasty balloon catheter training and testing. Biomed. Eng. Online 2024, 23, 89. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ntakakis, G.; Plomariti, C.; Frantzidis, C.; Antoniou, P.E.; Bamidis, P.D.; Tsoulfas, G. Exploring the use of virtual reality in surgical education. World J. Transplant. 2023, 13, 36–43. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]

| Item | Experts (n = 11) | Non-Experts (n = 9) | p-Value |
|---|---|---|---|
| Decides to ligate the mesenteric vessels before sectioning (% Yes) | 72.7 | 55.6 | 0.64 |
| Ligates the mesenteric vessels without tearing them (% Yes) | 45.5 | 22.2 | 0.37 |
| Ligates the mesenteric vessels without grasping any of them with the forceps (% Yes) | 63.6 | 22.2 | 0.09 |
| Does not produce damage to mesenteric vessels during the whole process (% Yes) | 72.7 | 44.4 | 0.36 |
| Correctly identifies the mesenteric section area and vascular boundaries of the intestinal segment to be resected (% Yes) | 81.8 | 77.8 | 0.99 |
| Sections bowel accurately, without deviation (% Yes) | 81.8 | 33.3 | 0.07 |
| Resects only the essential amount of affected intestine (<2 cm from the beginning of the healthy intestine in each segment) (% Yes) | 100 | 66.7 | 0.07 |
| Adequately spatulates intestinal loop (Benson technique) (% Yes) | 72.7 | 33.3 | 0.18 |
| Adequately calculates the section length of the antimesenteric border (Nixon technique) (% Yes) | 100 | 22.2 | 0.01 |
| Start anastomosis with side sutures and reference them (% Yes) | 90.0 | 100 | 0.99 |
| In general, sutures are seromuscular (% Yes) | 100 | 88.9 | 0.45 |
| Sutures are generally equidistant from each other (% Yes) | 100 | 88.9 | 0.45 |
| In general, the entry points of the suture in relation to the free margin are equidistant (% Yes) | 100 | 88.9 | 0.45 |
| In general, hand-made knots are performed correctly (“surgeon’s knot”) (% Yes) | 100 | 100 | 0.99 |
| In general, knots are performed correctly using the Mayo holder (% Yes) | 100 | 100 | 0.99 |
| Does not leave overlapping anastomotic edges (% Yes) | 36.4 | 22.2 | 0.64 |
| Does not tear serosa (% Yes) | 45.5 | 66.7 | 0.41 |
| Correctly repositions lateral references before intestinal rotation (% Yes) | 81.8 | 66.7 | 0.62 |
| Adequately rotates the anastomosis without damaging the mesentery or the bowel (% Yes) | 63.6 | 44.4 | 0.65 |
| Number of sutures employed (average) | 3 | 2.7 | 0.25 |
| Completes procedure in <45 min (% Yes) | 90.9 | 33.3 | 0.02 |
| Average time to complete the procedure (only takes into account those who completed the procedure) (minutes) | 41 (3.70) (n = 10) * | 42 (5.15) (n = 3) * | 0.61 |
| Item | Mean Score (Experts) N = 11 |
|---|---|
| The intestinal diameter of the model resembles that of neonatal intestinal atresia. | 2.7 |
| The intestinal thickness of the model resembles that of neonatal intestinal atresia. | 3.0 |
| The mesentery resembles that of a real neonatal intestine. | 2.4 |
| Mesentery vessels are adequately represented. | 3.2 |
| The layers of the model realistically simulate a real neonatal intestine. | 3.4 |
| Visually, the model material resembles a real neonatal intestine. | 3.5 |
| The model’s feel (wet and slippery) resembles a real neonatal intestine. | 2.8 |
| The texture and consistency of the model when the suture needle passes through it is similar to that of a real neonatal intestine. | 3.3 |
| The sensation of suturing the model’s strands together is similar to that of a real neonatal intestine. | 3.1 |
| The model reproduces the surgical dimensions of a neonatal abdominal field. | 2.3 |
| The spatial positioning of the model resembles that of a surgical field. | 2.5 |
| The model allows the mobility of the structures to be similar to reality. | 2.9 |
| In general, the execution of the surgical technique for the correction of neonatal intestinal atresia on the model resembles reality | 3.0 |
| This model is USEFUL for LEARNING the surgical technique for correcting intestinal atresia. | 3.6 |
| This model is USEFUL for TRAINING the surgical technique for correcting intestinal atresia. | 3.5 |
| This model allows realistic simulation of the Benson anastomotic congruency technique (spatulation of the distal anastomotic end). | 3.6 |
| This model allows a realistic simulation of Nixon’s anastomotic congruence technique (longitudinal opening of the antimesenteric edge of the distal anastomotic end). | 3.6 |
| This model allows a realistic simulation of an end-to-end intestinal anastomosis with discordant caliber ends. | 3.5 |
| This model allows the acquisition of transferable surgical skills to the actual surgical field. | 3.5 |
| This model realistically reproduces the level of difficulty of the procedure. | 3.1 |
| MEAN SCORE | 3.1 |
| Item | Mean Score (Experts) N = 11 | Mean Score (Non-Experts) N = 9 | p-Value |
|---|---|---|---|
| This model helps the user to understand the surgical technique. | 3.9 | 3.4 | 0.17 |
| This model helps the user to understand the spatial arrangement of the intestine and mesentery in a neonate. | 3.3 | 3.4 | 0.74 |
| This model helps the user learn how to handle the neonatal bowel and mesenteric structures in a surgical context. | 2.7 | 3.2 | 0.33 |
| This model helps the user understand how intestinal tissue responds to being handled in surgery. | 3.0 | 3.1 | 0.74 |
| This model allows you to LEARN different surgical techniques. | 3.6 | 3.6 | 0.88 |
| This model allows TRAINING different surgical techniques. | 3.5 | 3.6 | 0.84 |
| This model allows to EVALUATE the user’s surgical technique. | 2.9 | 3.1 | 0.56 |
| This model allows users to measure their ability to perform corrective surgery for neonatal intestinal atresia. | 3.1 | 3.2 | 0.67 |
| This model helps the user to be better prepared when performing corrective surgery for intestinal atresia in a neonate for the first time. | 3.5 | 3.6 | 0.93 |
| This model increases the user’s confidence before performing corrective surgery for intestinal atresia in a neonate. | 3.5 | 3.4 | 0.59 |
| MEAN SCORE | 3.3 (0.38) * | 3.4 (0.18) * | 0.74 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arredondo Montero, J.; Pérez Riveros, B.P.; Bueso Asfura, O.E.; Martín Calvo, N.; Pueyo, F.J.; López de Aguileta Castaño, N. Development and Validation of a Realistic Neonatal Intestinal Jejunoileal Atresia Simulator for the Training of Pediatric Surgeons. Children 2024, 11, 1109. https://doi.org/10.3390/children11091109
Arredondo Montero J, Pérez Riveros BP, Bueso Asfura OE, Martín Calvo N, Pueyo FJ, López de Aguileta Castaño N. Development and Validation of a Realistic Neonatal Intestinal Jejunoileal Atresia Simulator for the Training of Pediatric Surgeons. Children. 2024; 11(9):1109. https://doi.org/10.3390/children11091109
Chicago/Turabian StyleArredondo Montero, Javier, Blanca Paola Pérez Riveros, Oscar Emilio Bueso Asfura, Nerea Martín Calvo, Francisco Javier Pueyo, and Nicolás López de Aguileta Castaño. 2024. "Development and Validation of a Realistic Neonatal Intestinal Jejunoileal Atresia Simulator for the Training of Pediatric Surgeons" Children 11, no. 9: 1109. https://doi.org/10.3390/children11091109
APA StyleArredondo Montero, J., Pérez Riveros, B. P., Bueso Asfura, O. E., Martín Calvo, N., Pueyo, F. J., & López de Aguileta Castaño, N. (2024). Development and Validation of a Realistic Neonatal Intestinal Jejunoileal Atresia Simulator for the Training of Pediatric Surgeons. Children, 11(9), 1109. https://doi.org/10.3390/children11091109








