Visual Acuity Thresholds in Preterm Newborns: An Experimental Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Sample
2.3. Visual Acuity Assessment
2.4. Statistical Analysis
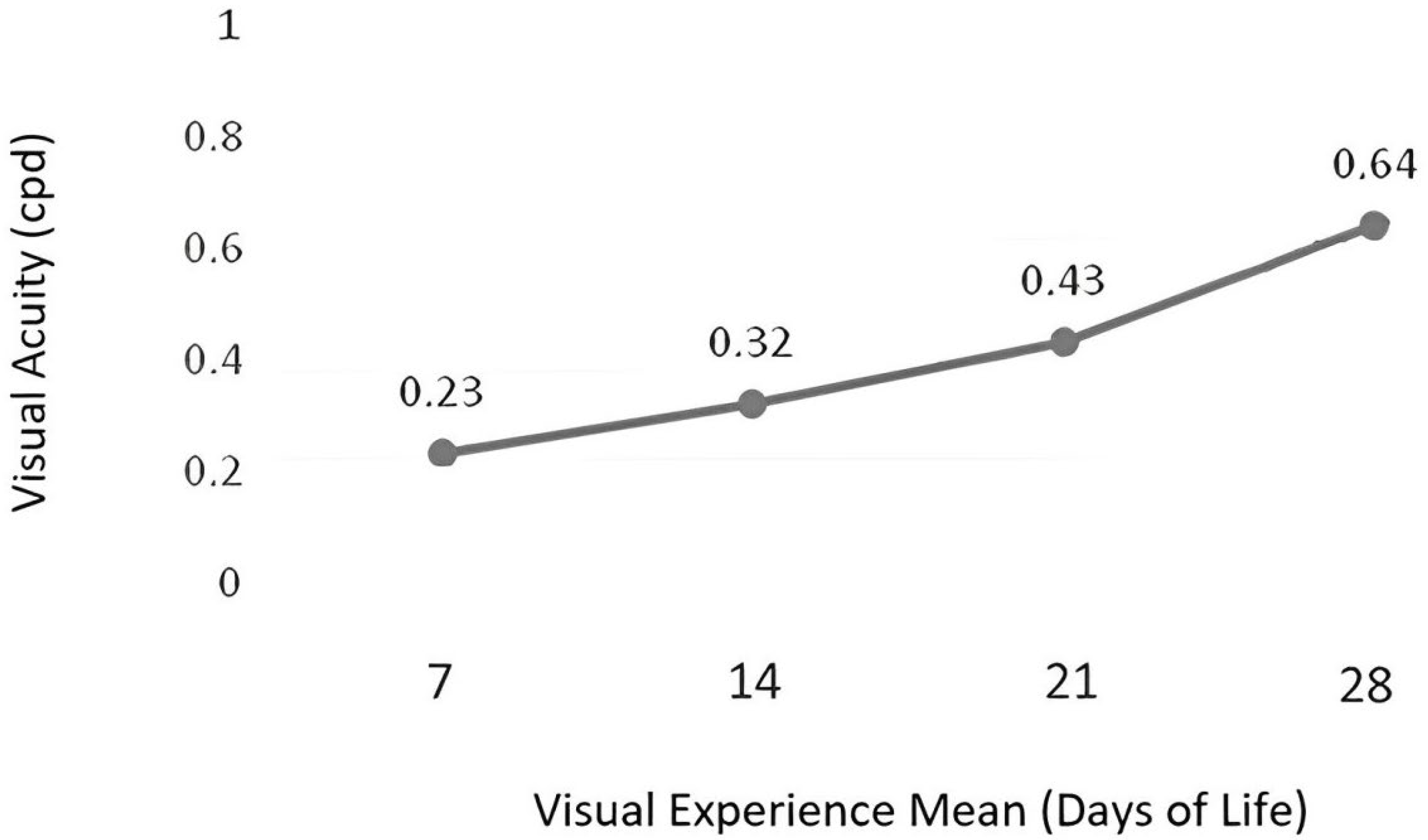
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Preston, K.L.; McDonald, M.; Sebris, S.L.; Dobson, V.; Teller, D.Y. Validation of the acuity card procedure for assessment of infants with ocular disorders. Ophthalmology 1987, 94, 644–653. [Google Scholar] [CrossRef]
- Duncan, A.F.; Matthews, M.A. Neurodevelopmental outcomes in early childhood. Clin. Perinatol. 2018, 45, 377–392. [Google Scholar] [CrossRef] [PubMed]
- Leung, M.P.; Thompson, B.; Black, J.; Dai, S.; Alsweiler, J.M. The effects of preterm birth on visual development. Clin. Exp. Optom. 2018, 101, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Kolb, H.; Kolb, H. How the retina works: Much of the construction of an image takes place in the retina itself through the use of specialized neural circuits. Am. Sci. 2003, 91, 28–35. [Google Scholar] [CrossRef]
- Lammertink, F.; Vinkers, C.H.; Tataranno, M.L.; Benders, M.J. Premature birth and developmental programming: Mechanisms of resilience and vulnerability. Front. Psychiatry 2021, 11, 531–571. [Google Scholar] [CrossRef]
- Holanda, N.S.O.; da Costa, L.D.O.; Sampaio, S.S.S.; Fonseca Filho, G.G.; Bezerra, R.B.; Azevedo, I.G.; Pereira, S.A. Screening for Autism Spectrum Disorder in Premature Subjects Hospitalized in a Neonatal Intensive Care Unit. Int. J. Environ. Res. Public Health 2020, 17, 7675. [Google Scholar] [CrossRef]
- Volpe, J.J. Confusions in nomenclature: Periventricular leukomalacia and white matter injury. Identical, distinct, or overlapping? Pediatr. Neurol. 2017, 73, 3–6. [Google Scholar] [CrossRef]
- Dubowitz, L.M.; Dubowitz, V.; Mercuri, E. The Neurological Assessment of the Preterm and Full-Term Newborn Infant; Spastics International Medical Publications: London, UK, 1981. [Google Scholar]
- Dubowitz, L.; Mercuri, E.; Dubowitz, V. An optimality score for the neurologic examination of the term newborn. J. Pediatr. 1998, 133, 406–416. [Google Scholar] [CrossRef]
- Dubowitz, L.M.; Dubowitz, V.; Morante, A. Visual function in the newborn: A study of preterm and full-term infants. Brain Dev. 1980, 2, 15–29. [Google Scholar] [CrossRef]
- Ricci, D.; Romeo, D.M.M.; Serrao, F.; Cesarini, L.; Gallini, F.; Cota, F.; Leone, D.; Zuppa, A.A.; Romagnoli, R.; Cowan, F.; et al. Application of a neonatal assessment of visual function in a population of low risk full-term newborn. Early Hum. Dev. 2008, 84, 277–280. [Google Scholar] [CrossRef]
- Mercuri, E.; Ricci, D.; Romeo, D.M. Neurological and visual assessments in very and late low-risk preterm infants. Early Hum. Dev. 2012, 88, 31–33. [Google Scholar] [CrossRef] [PubMed]
- Brémond-Gignac, D.; Copin, H.; Lapillonne, A.; Milazzo, S. Visual development in infants: Physiological and pathological mechanisms. Curr. Opin. Ophthalmol. 2011, 22, S1–S8. [Google Scholar] [CrossRef] [PubMed]
- Ellis, C.T.; Yates, T.S.; Skalaban, L.J.; Bejjanki, V.R.; Arcaro, M.J.; Turk-Browne, N.B. Retinotopic organization of visual cortex in human infants. Neuron 2021, 109, 2616–2626. [Google Scholar] [CrossRef]
- Birch, E. Looking to develop sight. Nature 2012, 487, 441–442. [Google Scholar] [CrossRef]
- Teller, D.Y.; Dobson, V.; Mayer, D.L. Reference and Instruction Manual: Teller Acuity Cards TM II (TAC II). 2019. Available online: https://eiiwebassets.s3.amazonaws.com/s/sterooptical/pdf/other-manuals/TAC_II_manual.pdf (accessed on 22 May 2024).
- Akoglu, H. User’s guide to correlation coefficients. Turk. J. Emerg. Med. 2018, 18, 91–93. [Google Scholar] [CrossRef]
- Ricci, D.; Romeo, D.M.; Serrao, F.; Gallini, F.; Leone, D.; Longo, M.; Albamonte, E.; Romeo, M.G.; Mazzone, D.; Romagnol, C.; et al. Early assessment of visual function in preterm infants: How early is early? Early Hum. Dev. 2010, 86, 29–33. [Google Scholar] [CrossRef]
- De Heering, A.; Turati, C.; Rossion, B.; Bulf, H.; Goffaux, V.; Simion, F. Newborns’ face recognition is based on spatial frequencies below 0.5 cycles per degree. Cognition 2008, 106, 444–454. [Google Scholar] [CrossRef]
- Graven, S.N. Early visual development: Implications for the neonatal intensive care unit and care. Clin. Perinatol. 2011, 38, 671–683. [Google Scholar] [CrossRef]
- Maurer, D.; Lewis, T.L.; Brent, H.P.; Levin, A.V. Rapid improvement in the acuity of infants after visual input. Science 1999, 286, 108–110. [Google Scholar] [CrossRef] [PubMed]
- Miranda, S.B.; Hack, M.; Fantz, R.L.; Fanaroff, A.A.; Klaus, M.H. Neonatal pattern vision: A predictor of future mental performance? J. Pediatr. 1977, 91, 642–647. [Google Scholar] [CrossRef]
- Graven, S.N.; Browne, J.V. Visual development in the human fetus, infant, and young child. Newborn Infant Nurs. Rev. 2008, 8, 194–201. [Google Scholar] [CrossRef]
- Dubowitz, L.M.; Mushin, J.; Morante, A.; Placzek, M. The maturation of visual acuity in neurologically normal and abnormal newborn infants. Behav. Brain Res. 1983, 10, 39–45. [Google Scholar] [CrossRef]
- Gagliardo, H.G.; Gonçalves, V.M.G.; Lima, M.C.M.P. A method to evaluate visual ability in infants. Arq. Neuro-Psiquiatr. 2004, 62, 300–306. [Google Scholar] [CrossRef]
- Tinelli, F.; Pei, F.; Guzzetta, A.; Bancale, A.; Mazzotti, S.; Baldassi, S.; Cioni, G. The assessment of visual acuity in children with periventricular damage: A comparison of behavioural and electrophysiological techniques. Vis. Res. 2008, 48, 1233–1241. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Koenig, K.P.; Rudney, S.G. Performance challenges for children and adolescents with difficulty processing and integrating sensory information: A systematic review. Am. J. Occup. Ther. 2010, 64, 430–442. [Google Scholar] [CrossRef]
- Mitchell, A.W.; Moore, E.M.; Roberts, E.J.; Hachtel, K.W.; Brown, M.S. Sensory processing disorder in children ages birth–3 years born prematurely: A systematic review. Am. J. Occup. Ther. 2015, 69, 6901220030p1–6901220030p11. [Google Scholar] [CrossRef] [PubMed]
- Messa, A.A.; Mattos, R.B.; Areco, K.C.; Sallum, J.M. Vision-related quality of life in children with retinopathy of prematurity. Arq. Bras. Oftalmol. 2015, 78, 224–228. [Google Scholar] [CrossRef][Green Version]
- Caldeira, V.A.; Oliver, F.C. Children with mental deficiency and interpersonal relationships in a community toy library. J. Hum. Growth Dev. 2007, 17, 98–110. [Google Scholar] [CrossRef][Green Version]
- Glass, P. Intensive Care Environment in Avery’s Neonatology: Pathophysiology & Management of the Newborn, 6th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2005; pp. 111–128. ISBN 0-7817-4643-4. [Google Scholar]
- Synnes, A.; Hicks, M. Neurodevelopmental Outcomes of Preterm Children at School Age and Beyond. Clin. Perinatol. 2018, 45, 393–408. [Google Scholar] [CrossRef]
- Brown, A.M.; Yamamoto, M. Visual acuity in newborn and preterm infants measured with grating acuity cards. Am. J. Ophthalmol. 1986, 102, 245–253. [Google Scholar] [CrossRef]
- Anderson, H.A.; Glasser, A.; Stuebing, K.K.; Manny, R.E. Minus lens stimulated accommodative lag as a function of age. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom. 2009, 86, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Lewis, T.L.; Maurer, D. Effects of early pattern deprivation on visual development. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom. 2009, 86, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Graziano, R.M.; Leone, C.R. Frequent ophthalmologic problems and visual development of preterm newborn infants. J. Pediatr. 2005, 81, S95–S100. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tham, E.H.; Loo, E.X.L.; Goh, A.; Teoh, O.H.; Yap, F.; Tan, K.H.; Godfrey, K.M.; Van Bever, H.; Lee, B.W.; Chong, Y.S.; et al. Phototherapy for neonatal hyperbilirubinemia and childhood eczema, rhinitis and wheeze. Pediatr. Neonatol. 2019, 60, 28–34. [Google Scholar] [CrossRef]
- Mondloch, C.J.; Lewis, T.L.; Levin, A.V.; Maurer, D. Infant face preferences after binocular visual deprivation. Int. J. Behav. Dev. 2013, 37, 148–153. [Google Scholar] [CrossRef]
- Nelson, C.A.; Zeanah, C.H.; Fox, N.A. How early experience shapes human development: The case of psychosocial deprivation. Neural Plast. 2019, 2019, 1676285. [Google Scholar] [CrossRef] [PubMed]
- Meredith, J.L.; Jnah, A.; Newberry, D. The NICU Environment: Infusing Single-Family Room Benefits into the Open-Bay Setting. Neonatal Netw. 2017, 36, 69–76. [Google Scholar] [CrossRef]
- Laudert, S.; Liu, W.F.; Blackington, S.; Perkins, B.; Martin, S.; MacMillan-York, E.; Handyside, J. Implementing potentially better practices to support the neurodevelopment of infants in the NICU. J. Perinatol. 2007, 27, S75–S93. [Google Scholar] [CrossRef]
- Esmaeilizadeh, M.; Shoja, M.; Shoja, E.; Shoja, M.; Nejat, H.; Oudi, D. Comparing the effects of continuous and cyclical lightings on weight gain and length of hospital stay among preterm neonates. Mod. Care J. 2016, 13, e8951. [Google Scholar] [CrossRef]
- Wachman, E.M.; Lahav, A. The effects of noise on preterm infants in the NICU. Arch. Dis. Child.-Fetal Neonatal Ed. 2011, 96, F305–F309. [Google Scholar] [CrossRef] [PubMed]

| Variables | Mean (SD)/Median (Q1–Q3) n = 42 | |
|---|---|---|
| Gestational age at birth (weeks) | 30 (±2.23) † | |
| Corrected gestational age (weeks) | 32 (30–36) | |
| Visual experience (days) * | 9 (1–57) | |
| Weight (grams) | 1290.20 (±267.10) † | |
| Apgar (first minute) | 8 (4–9) | |
| Apgar (fifth minute) | 9 (5–9) | |
| Frequency (% and N) | ||
| Type of delivery ** | Vaginal | 37.80% (14) |
| Cesarean | 62.20% (23) | |
| Gender | Male | 47.60% (20) |
| Female | 52.40% (22) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fagundes, R.B.B.; Silva, P.Y.F.; Barboni, M.T.S.; da Fonseca Filho, G.G.; Almeida, V.A.d.; Azevedo, I.G.; Pereira, S.A. Visual Acuity Thresholds in Preterm Newborns: An Experimental Study. Children 2024, 11, 1049. https://doi.org/10.3390/children11091049
Fagundes RBB, Silva PYF, Barboni MTS, da Fonseca Filho GG, Almeida VAd, Azevedo IG, Pereira SA. Visual Acuity Thresholds in Preterm Newborns: An Experimental Study. Children. 2024; 11(9):1049. https://doi.org/10.3390/children11091049
Chicago/Turabian StyleFagundes, Ruth Batista Bezerra, Pedro Ykaro Fialho Silva, Mirella Telles Salgueiro Barboni, Gentil Gomes da Fonseca Filho, Valeria Azevedo de Almeida, Ingrid Guerra Azevedo, and Silvana Alves Pereira. 2024. "Visual Acuity Thresholds in Preterm Newborns: An Experimental Study" Children 11, no. 9: 1049. https://doi.org/10.3390/children11091049
APA StyleFagundes, R. B. B., Silva, P. Y. F., Barboni, M. T. S., da Fonseca Filho, G. G., Almeida, V. A. d., Azevedo, I. G., & Pereira, S. A. (2024). Visual Acuity Thresholds in Preterm Newborns: An Experimental Study. Children, 11(9), 1049. https://doi.org/10.3390/children11091049






