Walking and Running of Children with Decreased Femoral Torsion
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measuring System and Procedure
2.3. Data Processing
2.4. Statistical Analysis
3. Results
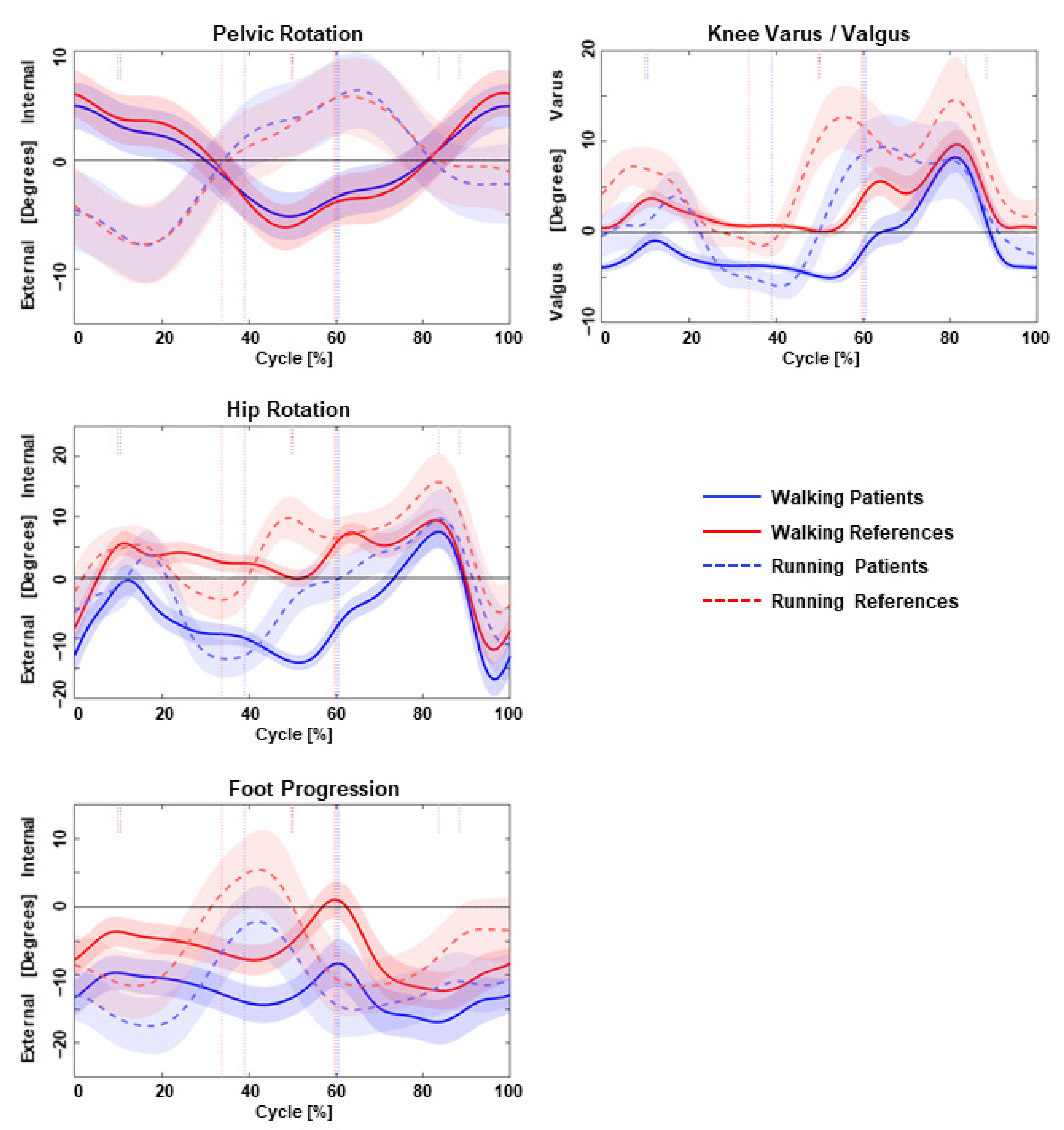
3.1. Kinematic Analysis during Walking and Running
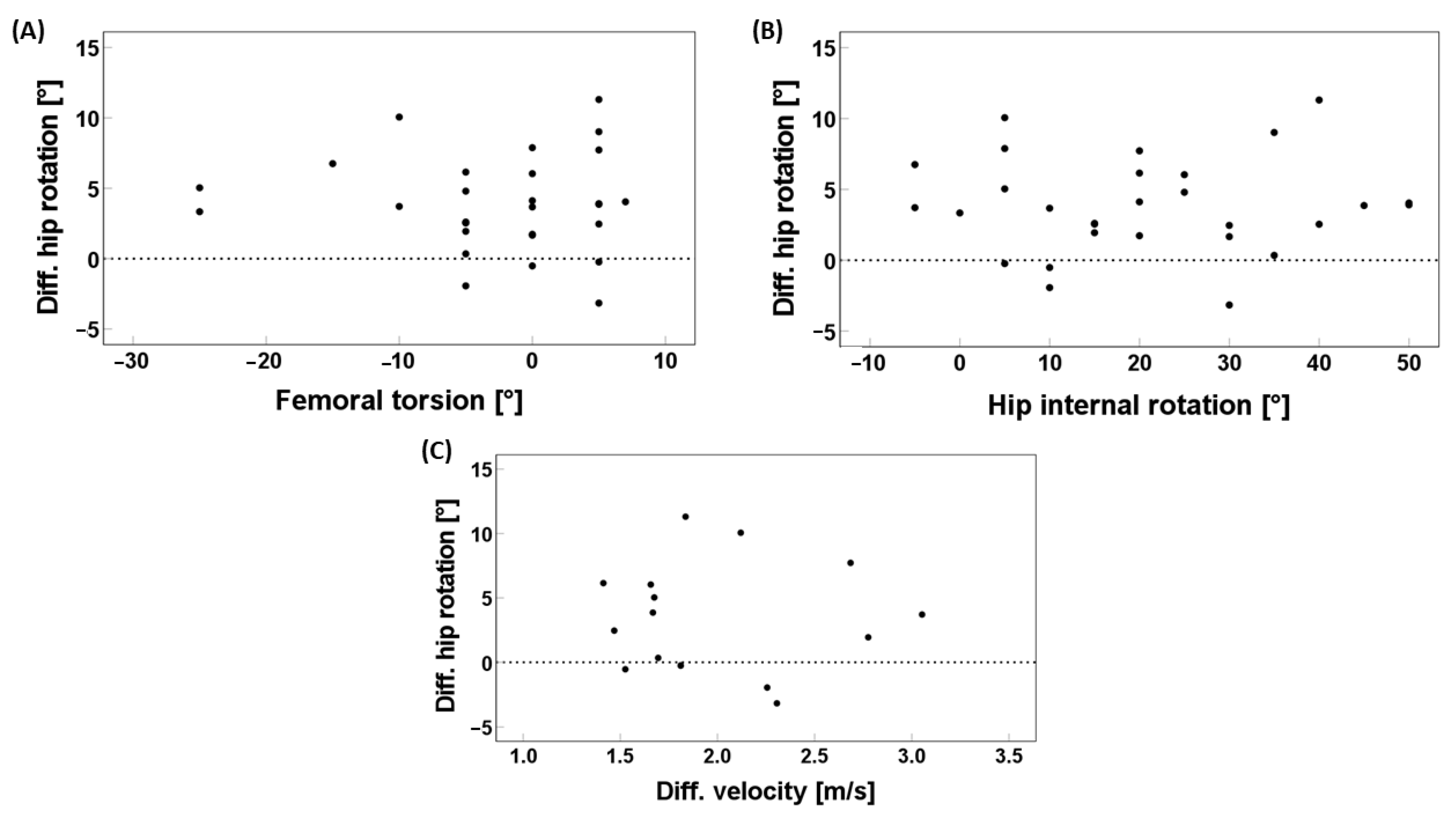
3.2. Comparison of Running–Walking Differences between Patients and Controls
4. Discussion
Limitations and Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gruskay, J.A.; Fragomen, A.T.; Rozbruch, S.R. Idiopathic Rotational Abnormalities of the Lower Extremities in Children and Adults. JBJS Rev. 2019, 7, E3. [Google Scholar] [CrossRef] [PubMed]
- Nourai, M.H.; Fadaei, B.; Maleki Rizi, A. In-Toeing and out-Toeing Gait Conservative Treatment; Hip Anteversion and Retroversion: 10-Year Follow-Up. J. Res. Med. Sci. 2015, 20, 1084. [Google Scholar] [CrossRef] [PubMed]
- Mittag, U.; Kriechbaumer, A.; Rittweger, J. Torsion—An Underestimated Form Shaping Entity in Bone Adaptation? J. Musculoskelet. Neuronal Interact. 2018, 18, 407. [Google Scholar] [PubMed]
- Scorcelletti, M.; Reeves, N.D.; Rittweger, J.; Ireland, A. Femoral Anteversion: Significance and Measurement. J. Anat. 2020, 237, 811. [Google Scholar] [CrossRef] [PubMed]
- Staheli, L.T. In-Toeing and out-Toeing in Children. J. Fam. Pract. 1983, 16, 1005–1011. [Google Scholar] [PubMed]
- Lerch, T.D.; Eichelberger, P.; Baur, H.; Schmaranzer, F.; Liechti, E.F.; Schwab, J.M.; Siebenrock, K.A.; Tannast, M. Prevalence and Diagnostic Accuracy of In-Toeing and out-Toeing of the Foot for Patients with Abnormal Femoral Torsion and Femoroacetabular Impingement: Implications for Hip Arthroscopy and Femoral Derotation Osteotomy. Bone Jt. J. 2019, 101-B, 1218–1229. [Google Scholar] [CrossRef]
- Galbraith, R.T.; Gelberman, R.H.; Hajek, P.C.; Baker, L.A.; Sartoris, D.J.; Rab, G.T.; Cohen, M.S.; Griffin, P.P. Obesity and Decreased Femoral Anteversion in Adolescence. J. Orthop. Res. 1987, 5, 523–528. [Google Scholar] [CrossRef] [PubMed]
- Murray, A.W.; Wilson, N.I.L. Changing Incidence of Slipped Capital Femoral Epiphysis: A Relationship with Obesity? J. Bone Jt. Surg. Ser. B 2008, 90, 92–94. [Google Scholar] [CrossRef]
- Dreher, T. Gait Analysis May Identify Femoral Retroversion. Gait Posture 2017, 57, 375–376. [Google Scholar] [CrossRef]
- Svenningsen, S.; Apalset, K.; Terjesen, T.; Anda, S. Regression of Femoral Anteversion. A Prospective Study of Intoeing Children. Acta Orthop. Scand. 1989, 60, 170–173. [Google Scholar] [CrossRef]
- Hatem, M.; Khoury, A.N.; Erickson, L.R.; Jones, A.L.; Martin, H.D. Femoral Derotation Osteotomy Improves Hip and Spine Function in Patients with Increased or Decreased Femoral Torsion. Arthrosc. J. Arthrosc. Relat. 2020, 37, 111–123. [Google Scholar] [CrossRef]
- Mooney, J.F. Lower Extremity Rotational and Angular Issues in Children. Pediatr. Clin. N. Am. 2014, 61, 1175–1183. [Google Scholar] [CrossRef] [PubMed]
- Sass, P.; Hassan, G. Lower Extremity Abnormalities in Children. Am. Fam. Physician 2003, 68, 461–468. [Google Scholar] [PubMed]
- Approach to the Child with Out-Toeing—UpToDate. Available online: https://www.uptodate.com/contents/approach-to-the-child-with-out-toeing (accessed on 8 September 2023).
- Schmaranzer, F.; Kallini, J.R.; Ferrer, M.G.; Miller, P.E.; Wylie, J.D.; Kim, Y.J.; Novais, E.N. How Common Is Femoral Retroversion and How Is It Affected by Different Measurement Methods in Unilateral Slipped Capital Femoral Epiphysis? Clin. Orthop. Relat. Res. 2021, 479, 947–959. [Google Scholar] [CrossRef] [PubMed]
- Lerch, T.D.; Kaim, T.; Hanke, M.S.; Schmaranzer, F.; Steppacher, S.D.; Busch, J.D.; Novais, E.N.; Ziebarth, K. Assessment of Femoral Retroversion on Preoperative Hip Magnetic Imaging in Patients with Slipped Capital Femoral Epiphysis: Theoretical Implications for Hip Impingement Risk Estimation. J. Child. Orthop. 2023, 17, 116. [Google Scholar] [CrossRef] [PubMed]
- Stevens, P.M.; Anderson, L.; MacWilliams, B.A. Femoral Shaft Osteotomy for Obligate Outward Rotation Due to SCFE. Strateg. Trauma Limb Reconstr. 2017, 12, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Rerucha, C.M.; Dickison, C.; Baird, D.C. Lower Extremity Abnormalities in Children. Am. Fam. Physician 2017, 96, 226–233. [Google Scholar] [PubMed]
- Tönnis, D.; Heinecke, A. Acetabular and Femoral Anteversion: Relationship with Osteoarthritis of the Hip. J. Bone Jt. Surg. Am. 1999, 81, 1747–1770. [Google Scholar] [CrossRef]
- Ganz, R.; Parvizi, J.; Beck, M.; Leunig, M.; Nötzli, H.; Siebenrock, K.A. Femoroacetabular Impingement: A Cause for Osteoarthritis of the Hip. Clin. Orthop. Relat. Res. 2003, 417, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Audenaert, E.A.; Peeters, I.; Vigneron, L.; Baelde, N.; Pattyn, C. Hip Morphological Characteristics and Range of Internal Rotation in Femoroacetabular Impingement. Am. J. Sports Med. 2012, 40, 1329–1336. [Google Scholar] [CrossRef]
- Ito, K.; Minka, M.A.; Leunig, M.; Werlen, S.; Ganz, R. Femoroacetabular Impingement and the Cam-Effect. A MRI-Based Quantitative Anatomical Study of the Femoral Head-Neck Offset. J. Bone Jt. Surg. Br. 2001, 83, 171–176. [Google Scholar] [CrossRef][Green Version]
- Grisch, D.; Dreher, T. Torsion and Torsional Development of the Lower Extremities. Orthopade 2019, 48, 523–530. [Google Scholar] [CrossRef] [PubMed]
- Radler, C.; Kranzl, A.; Manner, H.M.; Höglinger, M.; Ganger, R.; Grill, F. Torsional Profile versus Gait Analysis: Consistency between the Anatomic Torsion and the Resulting Gait Pattern in Patients with Rotational Malalignment of the Lower Extremity. Gait Posture 2010, 32, 405–410. [Google Scholar] [CrossRef] [PubMed]
- Wren, T.A.L.; Tucker, C.A.; Rethlefsen, S.A.; Gorton, G.E.; Õunpuu, S. Clinical Efficacy of Instrumented Gait Analysis: Systematic Review 2020 Update. Gait Posture 2020, 80, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Bruderer-Hofstetter, M.; Fenner, V.; Payne, E.; Zdenek, K.; Klima, H.; Wegener, R. Gait Deviations and Compensations in Pediatric Patients with Increased Femoral Torsion. J. Orthop. Res. 2014, 33, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Alexander, N.; Studer, K.; Lengnick, H.; Payne, E.; Klima, H.; Wegener, R. The Impact of Increased Femoral Antetorsion on Gait Deviations in Healthy Adolescents. J. Biomech. 2019, 86, 167–174. [Google Scholar] [CrossRef] [PubMed]
- Wilczyński, B.; Zorena, K.; Ślęzak, D. Dynamic Knee Valgus in Single-Leg Movement Tasks. Potentially Modifiable Factors and Exercise Training Options. A Literature Review. Int. J. Environ. Res. Public Health 2020, 17, 8208. [Google Scholar] [CrossRef] [PubMed]
- Sudlow, A.; Galantine, P.; Vercruyssen, F.; Peyrot, N.; Raymond, J.J.; Duché, P. Which Factors Influence Running Gait in Children and Adolescents? A Narrative Review. Int. J. Environ. Res. Public Health 2023, 20, 4621. [Google Scholar] [CrossRef] [PubMed]
- Dicharry, J. Kinematics and Kinetics of Gait: From Lab to Clinic. Clin. Sports Med. 2010, 29, 347–364. [Google Scholar] [CrossRef]
- Dugan, S.A.; Bhat, K.P. Biomechanics and Analysis of Running Gait. Phys. Med. Rehabil. Clin. N. Am. 2005, 16, 603–621. [Google Scholar] [CrossRef]
- Franz, J.R.; Paylo, K.W.; Dicharry, J.; Riley, P.O.; Kerrigan, D.C. Changes in the Coordination of Hip and Pelvis Kinematics with Mode of Locomotion. Gait Posture 2009, 29, 494–498. [Google Scholar] [CrossRef]
- Perpiñá-Martínez, S.; Arguisuelas-Martínez, M.D.; Pérez-Domínguez, B.; Nacher-Moltó, I.; Martínez-Gramage, J. Differences between Sexes and Speed Levels in Pelvic 3D Kinematic Patterns during Running Using an Inertial Measurement Unit (IMU). Int. J. Environ. Res. Public Health 2023, 20, 3631. [Google Scholar] [CrossRef] [PubMed]
- Shultz, S.P.; D’Hondt, E.; Fink, P.W.; Lenoir, M.; Hills, A.P. The Effects of Pediatric Obesity on Dynamic Joint Malalignment during Gait. Clin. Biomech. 2014, 29, 835–838. [Google Scholar] [CrossRef] [PubMed]
- Bailly, R.; Pons, C.; Haes, A.C.; Nguyen, L.; Thepaut, M.; Houx, L.; Lempereur, M.; Brochard, S. Bone Deformities through the Prism of the International Classification of Functioning, Disability and Health in Ambulant Children with Cerebral Palsy: A Systematic Review. Children 2024, 11, 257. [Google Scholar] [CrossRef]
- Powers, C.M. The Influence of Abnormal Hip Mechanics on Knee Injury: A Biomechanical Perspective. J. Orthop. Sports Phys. Ther. 2010, 40, 42–51. [Google Scholar] [CrossRef]
- Cordier, W.; Katthagen, B.D. Femoral Torsional Deformities. Orthopade 2000, 29, 795–801. [Google Scholar] [CrossRef] [PubMed]
- McGinley, J.L.; Baker, R.; Wolfe, R.; Morris, M.E. The Reliability of Three-Dimensional Kinematic Gait Measurements: A Systematic Review. Gait Posture 2009, 29, 360–369. [Google Scholar] [CrossRef]
- Reinschmidt, C.; Van Den Bogert, A.J.; Nigg, B.M.; Lundberg, A.; Murphy, N. Effect of Skin Movement on the Analysis of Skeletal Knee Joint Motion during Running. J. Biomech. 1997, 30, 729–732. [Google Scholar] [CrossRef]
| Groups | Patients | Controls | Patients | Controls | Patients/Controls | Patients/Controls | ||
|---|---|---|---|---|---|---|---|---|
| Conditions Parameters | WALK (Mean ± SD) | RUN (Mean ± SD) | WALK (Mean ± SD) | RUN (Mean ± SD) | RUN/WALK (p Value) | RUN/WALK (p Value) | WALK (p Value) | RUN (p Value) |
| Mean pelvic rotation (°) Internal(+)/external rotation(−) | −0.06 ± 2.72 | −0.38 ± 2.63 | 0.07 ± 1.05 | −0.53 ± 2.04 | 0.008 * | <0.001 * | 0.474 | 0.216 |
| ROM pelvic rotation (°) Internal(+)/external rotation(−) | 12.38 ± 3.96 | 17.49 ± 4.04 | 14.33 ± 3.86 | 17.99 ± 5.54 | 0.150 | 0.103 | 0.231 | 0.529 |
| Mean hip rotation (°) Internal(+)/external rotation(−) | −8.80 ± 8.08 | −4.96 ± 9.00 | 2.67 ± 5.92 | 2.69 ± 8.21 | 0.680 | 0.936 | <0.001 * | 0.539 |
| Peak hip external rotation (°) Internal(+)/external rotation(−) | −17.08 ± 7.80 | −17.16 ± 8.84 | −7.78 ± 6.40 | −6.75 ± 7.46 | 0.999 | 0.777 | 0.004 * | 0.503 |
| Peak hip extension (°) Flexion(+)/extension(−) | −6.64 ± 5.65 | −4.56 ± 6.75 | −10.45 ± 6.29 | −9.02 ± 6.82 | 0.310 | 0.707 | 0.071 | 0.292 |
| Peak knee valgus (°) Varus(+)/Valgus(−) | −6.55 ± 3.24 | −7.07 ± 3.73 | −1.27 ± 1.93 | −1.95 ± 3.81 | 0.741 | 0.543 | 0.001 * | 0.034 * |
| Peak foot DF (°) Dorsi(+)/plantarflexion(−) | 13.23 ± 3.02 | 23.57 ± 3.94 | 14.78 ± 3.04 | 26.63 ± 3.93 | <0.001 * | <0.001 * | 0.179 | 0.052 |
| Peak foot PA (°) In(+)/out-toeing(−) | −11.31 ± 9.08 | −15.40 ± 5.95 | −6.12 ± 4.65 | −10.59 ± 6.60 | 0.145 | 0.034 * | 0.037 * | 0.107 |
| Groups Conditions Parameters | Patients RUN-WALK (Mean ± SD) | Controls RUN-WALK (Mean ± SD) | Δ Patients/Δ Controls (p Value) |
|---|---|---|---|
| Δ mean pelvic rotation (°) Internal(+)/external rotation(−) | −0.32 ± 1.88 | −0.61 ± 1.61 | 0.179 |
| Δ ROM pelvic rotation (°) Internal(+)/external rotation(−) | 5.11 ± 5.84 | 3.67 ± 4.67 | 0.601 |
| Δ mean hip rotation (°) Internal(+)/external(−)rotation | 3.84 ± 3.40 | 0.02 ± 4.30 | 0.005 * |
| Δ peak hip external rotation (°) Internal(+)/external(−)rotation | −0.09 ± 3.17 | 1.03 ± 5.12 | 0.490 |
| Δ peak hip extension (°) Flexion(+)/extension(−) | 2.08 ± 4.74 | 1.43 ± 3.38 | 0.778 |
| Δ peak knee valgus (°) Varus(+)/Valgus(−) | −0.52 ± 1.77 | −0.67 ± 2.88 | 0.944 |
| Δ peak foot DF (°) Dorsi(+)/plantarflexion(−) | 10.34 ± 4.30 | 11.85 ± 4.34 | 0.357 |
| Δ peak foot PA (°) In(+)/out(−)-toeing | −4.08 ± 6.64 | −4.47 ± 4.19 | 0.902 |
| Δ mean velocity (m/s) | 2.00 ± 0.51 | 2.28 ± 0.35 | 0.104 |
| Variables | Regression Coefficient B | p Value | Patients (Mean ± SD) | Controls (Mean ± SD) |
|---|---|---|---|---|
| Total hip rotation (°) | 0.009 | 0.832 | 89.83 ± 16.39 | 91.82 ± 16.80 |
| Hip external rotation (°) | 0.003 | 0.939 | 69.14 ± 14.34 | 43.64 ± 14.57 |
| Hip internal rotation (°) | 0.003 | 0.939 | 20.69 ± 15.74 | 48.18 ± 10.86 |
| Hip extension (°) | 0.124 | 0.415 | 11.90 ± 4.31 | 14.32 ± 4.70 |
| Femoral torsion (°) | −0.021 | 0.789 | −2.69 ± 8.27 | 15.45 ± 5.33 |
| Tibia torsion (°) | −0.258 | 0.024 * | −23.45 ± 5.53 | −20.55 ± 6.68 |
| Δ mean velocity RUN-WALK (m/s) | −0.254 | 0.914 | 2.00 ± 0.51 | 2.28 ± 0.35 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsagkaris, C.; Hamberg, M.E.; Villefort, C.; Dreher, T.; Krautwurst, B.K. Walking and Running of Children with Decreased Femoral Torsion. Children 2024, 11, 617. https://doi.org/10.3390/children11060617
Tsagkaris C, Hamberg ME, Villefort C, Dreher T, Krautwurst BK. Walking and Running of Children with Decreased Femoral Torsion. Children. 2024; 11(6):617. https://doi.org/10.3390/children11060617
Chicago/Turabian StyleTsagkaris, Christos, Marry E. Hamberg, Christina Villefort, Thomas Dreher, and Britta K. Krautwurst. 2024. "Walking and Running of Children with Decreased Femoral Torsion" Children 11, no. 6: 617. https://doi.org/10.3390/children11060617
APA StyleTsagkaris, C., Hamberg, M. E., Villefort, C., Dreher, T., & Krautwurst, B. K. (2024). Walking and Running of Children with Decreased Femoral Torsion. Children, 11(6), 617. https://doi.org/10.3390/children11060617





