Dynamic Gait Analysis in Paediatric Flatfeet: Unveiling Biomechanical Insights for Diagnosis and Treatment
Abstract
1. Introduction
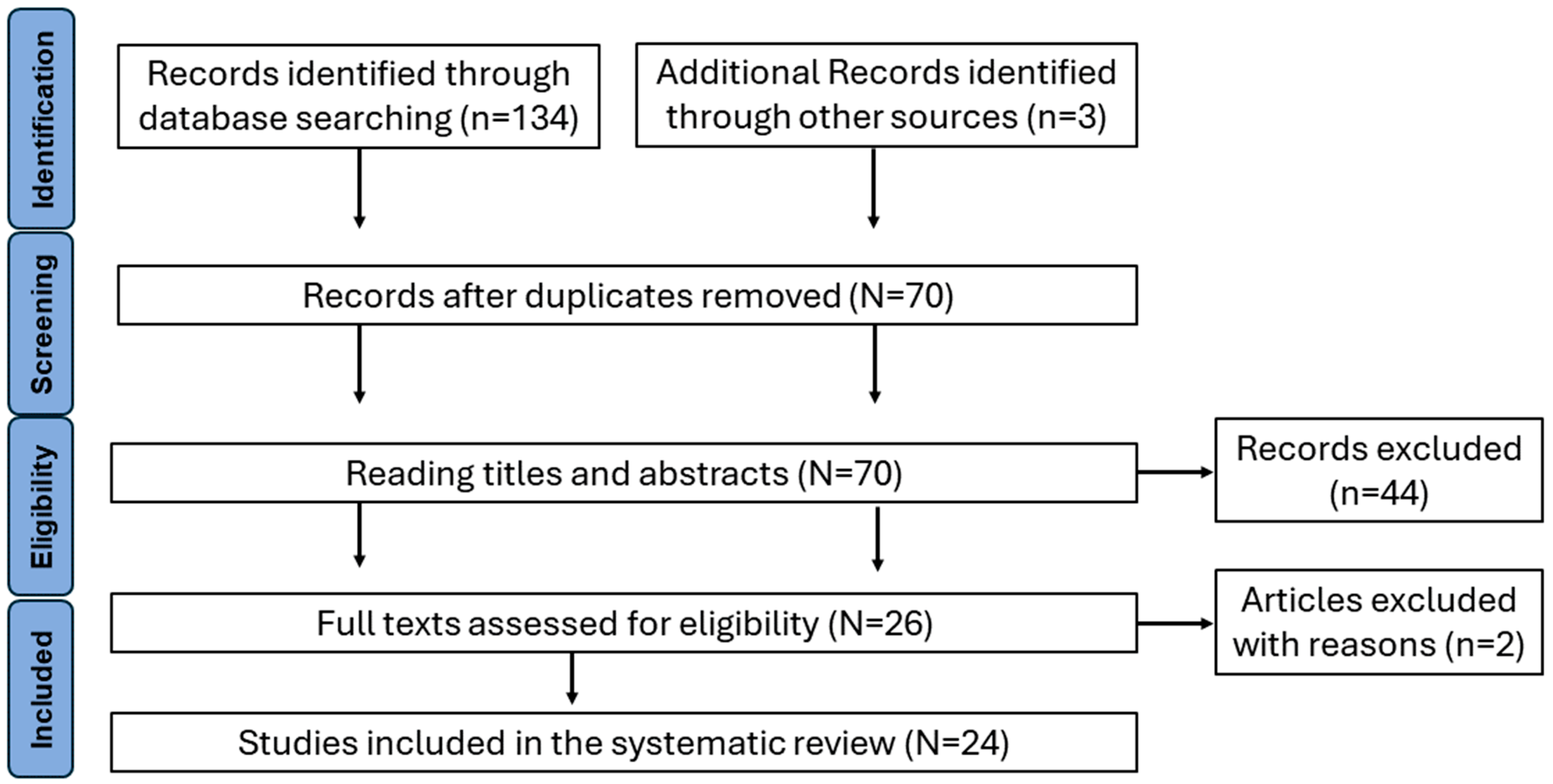
2. Methods
2.1. Inclusion and Exclusion Criteria
2.2. Search Strategy
2.3. Study Selection
2.4. Data Extraction and Management
3. Results
3.1. Population
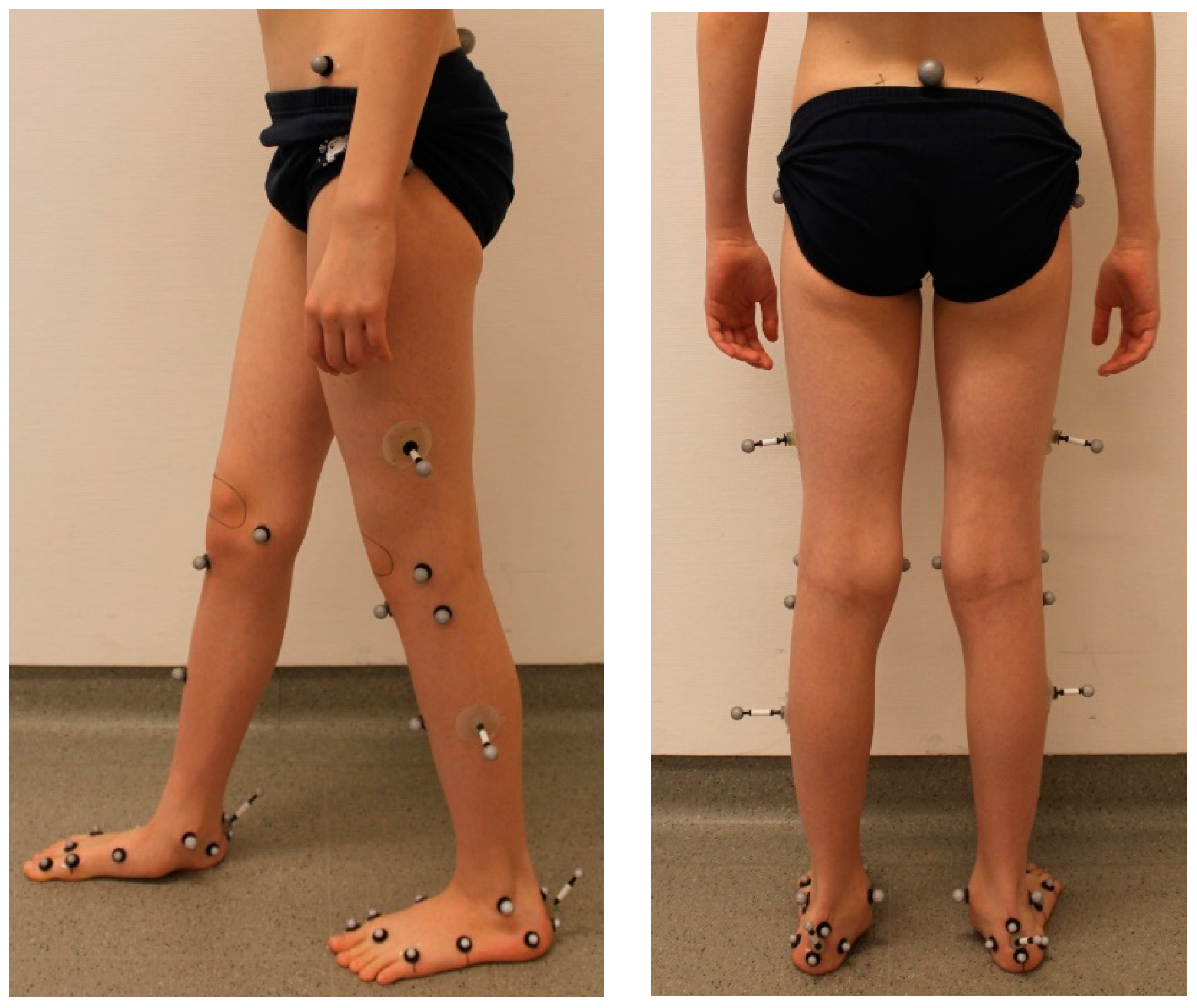
3.2. Technology and Human Model
3.3. Footwear and Movement
3.4. Purpose and Main Outcome
- Comparative analysis between FFF and Typically Developed Feet (TDF);
- Classification of foot types;
- Examination of the relationship between foot characteristics and clinical measures;
- Assessment of the effectiveness of interventions.
3.4.1. Comparative Analysis between Flexible Flat Feet and Typically Developed Feet
3.4.2. Classification of Foot Types
3.4.3. Relation with Clinical Measures
3.4.4. Effects of Interventions
4. Discussion
4.1. Population
4.2. Technology and Human Model
4.3. Footwear and Movement
4.4. Purpose and Main Outcome
4.4.1. Comparative Analysis between Flexible Flat Feet and Typically Developed Feet
4.4.2. Classification of Foot Types
4.4.3. Relation with Clinical Measures
4.4.4. Effects of Interventions
4.5. Challenges and Future Directions
5. Conclusions
Funding
Conflicts of Interest
References
- Bauer, K.; Mosca, V.S.; Zionts, L.E. What’s New in Pediatric Flatfoot? J. Pediatr. Orthop. 2016, 36, 865–869. [Google Scholar] [CrossRef] [PubMed]
- Bosch, K.; Gerß, J.; Rosenbaum, D. Development of healthy children’s feet—Nine-year results of a longitudinal investigation of plantar loading patterns. Gait Posture 2010, 32, 564–571. [Google Scholar] [CrossRef] [PubMed]
- Pfeiffer, M.; Kotz, R.; Ledl, T.; Hauser, G.; Sluga, M. Prevalence of Flat Foot in Preschool-Aged Children. Pediatrics 2006, 118, 634–639. [Google Scholar] [CrossRef]
- Benedetti, M.G.; Ceccarelli, F.; Berti, L.; Luciani, D.; Catani, F.; Boschi, M.; Giannini, S. Diagnosis of Flexible Flatfoot in Children: A Systematic Clinical Approach. Orthopedics 2011, 34, 94. [Google Scholar] [CrossRef] [PubMed]
- Böhm, H.; Dussa, C.U. Clinical, Radiographic and Gait Parameters Associated with Medial Arch Pain in the Flexible Pediatric Flatfoot. J. Foot Ankle Surg. 2023, 62, 637–643. [Google Scholar] [CrossRef]
- Westberry, D.E.; Davids, J.R.; Anderson, J.P.; Pugh, L.I.; Davis, R.B.; Hardin, J.W. The operative correction of symptomatic flat foot deformities in children. Bone Jt. J. 2013, 95, 706–713. [Google Scholar] [CrossRef]
- MacInnes, P.; Lewis, T.L.; Griffin, C.; Martinuzzi, M.; Shepherd, K.L.; Kokkinakis, M. Surgical management of pes planus in children with cerebral palsy: A systematic review. J. Child. Orthop. 2022, 16, 333–346. [Google Scholar] [CrossRef] [PubMed]
- Dussa, C.U.; Boehm, H.; Doederlein, L.; Forst, R.; Fujak, A. Does an overcorrected clubfoot caused by surgery or by the Ponseti method behave differently? Gait Posture 2020, 77, 308–314. [Google Scholar] [CrossRef] [PubMed]
- Frances, J.M.; Feldman, D.S. Management of idiopathic and nonidiopathic flatfoot. Instr. Course Lect. 2015, 64, 429–440. [Google Scholar]
- Bourdet, C.; Seringe, R.; Adamsbaum, C.; Glorion, C.; Wicart, P. Flatfoot in children and adolescents. Analysis of imaging findings and therapeutic implications. Orthop. Traumatol. Surg. Res. 2013, 99, 80–87. [Google Scholar] [CrossRef]
- Lau, B.C.; Allahabadi, S.; Palanca, A.; Oji, D.E. Understanding Radiographic Measurements Used in Foot and Ankle Surgery. J. Am. Acad. Orthop. Surg. 2022, 30, e139–e154. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, D. Assessing Pediatric Foot Deformities by Pedobarography. In Handbook of Human Motion; Springer International Publishing: Cham, Switzerland, 2016; pp. 1–15. [Google Scholar] [CrossRef]
- Leardini, A.; Caravaggi, P.; Theologis, T.; Stebbins, J. Multi-segment foot models and their use in clinical populations. Gait Posture 2019, 69, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Caravaggi, P.; Lullini, G.; Berti, L.; Giannini, S.; Leardini, A. Functional evaluation of bilateral subtalar arthroereisis for the correction of flexible flatfoot in children: 1-year follow-up. Gait Posture 2018, 64, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Das, S.P.; Das, P.B.; Bsc, G.S.; Sahu, M.C. Effectiveness of surgically treated symptomatic plano-valgus deformity by the calcaneo stop procedure according to radiological, functional and gait parameters. J. Taibah Univ. Med. Sci. 2017, 12, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Papamerkouriou, Y.-M.; Rajan, R.; Chaudhry, S.; Kodumuri, P.; Evans, H.; Kerr, M. Prospective Early Clinical, Radiological, and Kinematic Pedobarographic Analysis Following Subtalar Arthroereises for Paediatric Pes Planovalgus. Cureus 2019, 11, e6309. [Google Scholar] [CrossRef] [PubMed]
- Twomey, D.; McIntosh, A.; Simon, J.; Lowe, K.; Wolf, S. Kinematic differences between normal and low arched feet in children using the Heidelberg foot measurement method. Gait Posture 2010, 32, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Twomey, D.; McIntosh, A. The effects of low arched feet on lower limb gait kinematics in children. Foot 2012, 22, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Shih, Y.-F.; Chen, C.-Y.; Chen, W.-Y.; Lin, H.-C. Lower extremity kinematics in children with and without flexible flatfoot: A comparative study. BMC Musculoskelet. Disord. 2012, 13, 31. [Google Scholar] [CrossRef] [PubMed]
- Hösl, M.; Böhm, H.; Multerer, C.; Döderlein, L. Does excessive flatfoot deformity affect function? A comparison between symptomatic and asymptomatic flatfeet using the Oxford Foot Model. Gait Posture 2014, 39, 23–28. [Google Scholar] [CrossRef]
- Ramakrishnan, H.; Kadaba, M. On the estimation of joint kinematics during gait. J. Biomech. 1991, 24, 969–977. [Google Scholar] [CrossRef]
- Kothari, A.; Dixon, P.C.; Stebbins, J.; Zavatsky, A.B.; Theologis, T. Motion Analysis to Track Navicular Displacements in the Pediatric Foot: Relationship with Foot Posture, Body Mass Index, and Flexibility. Foot Ankle Int. 2014, 35, 929–937. [Google Scholar] [CrossRef]
- Portinaro, N.; Leardini, A.; Panou, A.; Monzani, V.; Caravaggi, P. Modifying the Rizzoli foot model to improve the diagnosis of pes-planus: Application to kinematics of feet in teenagers. J. Foot Ankle Res. 2014, 7, 57. [Google Scholar] [CrossRef]
- Kerr, C.; Stebbins, J.; Theologis, T.; Zavatsky, A. Static postural differences between neutral and flat feet in children with and without symptoms. Clin. Biomech. 2015, 30, 314–317. [Google Scholar] [CrossRef]
- Kothari, A.; Dixon, P.; Stebbins, J.; Zavatsky, A.; Theologis, T. The relationship between quality of life and foot function in children with flexible flatfeet. Gait Posture 2015, 41, 786–790. [Google Scholar] [CrossRef]
- Kothari, A.; Dixon, P.; Stebbins, J.; Zavatsky, A.; Theologis, T. Are flexible flat feet associated with proximal joint problems in children? Gait Posture 2016, 45, 204–210. [Google Scholar] [CrossRef] [PubMed]
- Pothrat, C.; Authier, G.; Viehweger, E.; Berton, E.; Rao, G. One- and multi-segment foot models lead to opposite results on ankle joint kinematics during gait: Implications for clinical assessment. Clin. Biomech. 2015, 30, 493–499. [Google Scholar] [CrossRef]
- Krautwurst, B.K.; Wolf, S.I.; Dreher, T. Three-dimensional evaluation of heel raise test in pediatric planovalgus feet and normal feet. Gait Posture 2016, 48, 146–151. [Google Scholar] [CrossRef]
- Jafarnezhadgero, A.A.; Shad, M.M.; Majlesi, M. Effect of foot orthoses on the medial longitudinal arch in children with flexible flatfoot deformity: A three-dimensional moment analysis. Gait Posture 2017, 55, 75–80. [Google Scholar] [CrossRef]
- Kim, H.Y.; Shin, H.S.; Ko, J.H.; Cha, Y.H.; Ahn, J.H.; Hwang, J.Y. Gait Analysis of Symptomatic Flatfoot in Children: An Observational Study. CiOS Clin. Orthop. Surg. 2017, 9, 363–373. [Google Scholar] [CrossRef]
- Caravaggi, P.; Sforza, C.; Leardini, A.; Portinaro, N.; Panou, A. Effect of plano-valgus foot posture on midfoot kinematics during barefoot walking in an adolescent population. J. Foot Ankle Res. 2018, 11, 55. [Google Scholar] [CrossRef]
- Jafarnezhadgero, A.; Madadi-Shad, M.; Alavi-Mehr, S.M.; Granacher, U. The long-term use of foot orthoses affects walking kinematics and kinetics of children with flexible flat feet: A randomized controlled trial. PLoS ONE 2018, 13, e0205187. [Google Scholar] [CrossRef] [PubMed]
- Kerr, C.; Zavatsky, A.; Theologis, T.; Stebbins, J. Kinematic differences between neutral and flat feet with and without symptoms as measured by the Oxford foot model. Gait Posture 2019, 67, 213–218. [Google Scholar] [CrossRef] [PubMed]
- Böhm, H.; Oestreich, C.; Rethwilm, R.; Federolf, P.; Döderlein, L.; Fujak, A.; Dussa, C.U. Cluster analysis to identify foot motion patterns in children with flexible flatfeet using gait analysis—A statistical approach to detect decompensated pathology? Gait Posture 2019, 71, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Böhm, H.; Döderlein, L.; Fujak, A.; Dussa, C.U. Is there a correlation between static radiographs and dynamic foot function in pediatric foot deformities? Foot Ankle Surg. 2020, 26, 801–809. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.Y.; Cha, Y.H.; Lee, J.S.; Kil, K.-M.; Choy, W.S. Changes in Gait and Radiographic and Clinical Results of Calcaneal Lengthening Osteotomy in Children with Idiopathic Flexible Flatfoot. Clin. Orthop. Surg. 2020, 12, 386–395. [Google Scholar] [CrossRef] [PubMed]
- Byrnes, S.K.; Wearing, S.; Böhm, H.; Dussa, C.U.; Horstmann, T. Effects of idiopathic flatfoot deformity on knee adduction moments during walking. Gait Posture 2021, 84, 280–286. [Google Scholar] [CrossRef] [PubMed]
- Stief, F.; Böhm, H.; Michel, K.; Schwirtz, A.; Döderlein, L. Reliability and Accuracy in Three-Dimensional Gait Analysis: A Comparison of Two Lower Body Protocols. J. Appl. Biomech. 2013, 29, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Boryczka-Trefler, A.; Kalinowska, M.; Szczerbik, E.; Stępowska, J.; Łukaszewska, A.; Syczewska, M. Effect of Plano-Valgus Foot on Lower-Extremity Kinematics and Spatiotemporal Gait Parameters in Children of Age 5–9. Diagnostics 2022, 12, 2. [Google Scholar] [CrossRef] [PubMed]
- Pourghazi, F.; Nabian, M.H.; Bakht, S.S.; Laripour, R.; Zoshk, M.Y. Changes in gait pattern and quality of life of adolescents with flexible flat foot after Calcaneal Lengthening Osteotomy. Foot 2023, 57, 101962. [Google Scholar] [CrossRef]
- Cote, K.P.; E Brunet, M.; Gansneder, B.M.; Shultz, S.J. Effects of Pronated and Supinated Foot Postures on Static and Dynamic Postural Stability. J. Athl. Train 2005, 40, 41–46. [Google Scholar]
- Bok, S.-K.; Kim, B.-O.; Lim, J.-H.; Ahn, S.-Y. Effects of Custom-Made Rigid Foot Orthosis on Pes Planus in Children over 6 Years Old. Ann. Rehabil. Med. 2014, 38, 369. [Google Scholar] [CrossRef] [PubMed]
- Butler, R.J.; Hillstrom, H.; Song, J.; Richards, C.J.; Davis, I.S. Arch Height Index Measurement System: Establishment of Reliability and Normative Values. J. Am. Podiatr. Med. Assoc. 2008, 98, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Davis, R.B.; Õunpuu, S.; Tyburski, D.; Gage, J.R. A gait analysis data collection and reduction technique. Hum. Mov. Sci. 1991, 10, 575–587. [Google Scholar] [CrossRef]
- Sarrafian, S.K. Functional Characteristics of the Foot and Plantar Aponeurosis under Tibiotalar Loading. Foot Ankle 1987, 8, 4–18. [Google Scholar] [CrossRef] [PubMed]
- Seringe, R.; Wicart, P. The talonavicular and subtalar joints: The “calcaneopedal unit” concept. Orthop. Traumatol. Surg. Res. 2013, 99, S345–S355. [Google Scholar] [CrossRef] [PubMed]
- Basmajian, J.V.; Stecko, G. The Role of Muscles in Arch Support of the Foot. J. Bone Jt. Surg. 1963, 45, 1184–1190. [Google Scholar] [CrossRef]
- Sonia, J.; Nadia, L.; Manel, A.; Samia, F.; Mohamed, B.R.; Walid, O.; Afif, Z.; Faycel, K. Children Flat Foot and Lower Limb Rotational Profile: A Cross-Sectional Descriptive Study. Open J. Orthop. 2015, 5, 326–335. [Google Scholar] [CrossRef]
- Mann, R.; Inman, V.T. Phasic Activity of Intrinsic Muscles of the Foot. J. Bone Jt. Surg. 1964, 46, 469–481. [Google Scholar] [CrossRef]
- Jankowicz-Szymanska, A.; Mikolajczyk, E. Genu Valgum and Flat Feet in Children With Healthy and Excessive Body Weight. Pediatr. Phys. Ther. 2016, 28, 200–206. [Google Scholar] [CrossRef]
- Shultz, S.P.; D’Hondt, E.; Fink, P.W.; Lenoir, M.; Hills, A.P. The effects of pediatric obesity on dynamic joint malalignment during gait. Clin. Biomech. 2014, 29, 835–838. [Google Scholar] [CrossRef]
- Guichet, J.-M.; Javed, A.; Russell, J.; Saleh, M. Effect of the Foot on the Mechanical Alignment of the Lower Limbs. Clin. Orthop. Relat. Res. 2003, 415, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Blackwood, C.B.; Yuen, T.J.; Sangeorzan, B.J.; Ledoux, W.R. The Midtarsal Joint Locking Mechanism. Foot Ankle Int. 2005, 26, 1074–1080. [Google Scholar] [CrossRef] [PubMed]
- Richie, D.H., Jr. Comparative Anatomy and Introduction to the Twisted Plate Mechanism. In Pathomechanics of Common Foot Disorders; Springer International Publishing: Cham, Switzerland, 2021; pp. 1–43. [Google Scholar] [CrossRef]
- Mosca, V.S. Flexible flatfoot in children and adolescents. J. Child. Orthop. 2010, 4, 107–121. [Google Scholar] [CrossRef] [PubMed]
- Labovitz, J.M. The Algorithmic Approach to Pediatric Flexible Pes Planovalgus. Clin. Podiatr. Med. Surg. 2005, 23, 57–76. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Chen, L.; Yu, J.; Zhang, C.; Huang, J.-Z.; Wang, X.; Ma, X. Mid-term Results of Subtalar Arthroereisis with Talar-Fit Implant in Pediatric Flexible Flatfoot and Identifying the Effects of Adjunctive Procedures and Risk Factors for Sinus Tarsi Pain. Orthop. Surg. 2021, 13, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Buldt, A.K.; Murley, G.S.; Butterworth, P.; Levinger, P.; Menz, H.B.; Landorf, K.B. The relationship between foot posture and lower limb kinematics during walking: A systematic review. Gait Posture 2013, 38, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Horsak, B.; Eichmann, A.; Lauer, K.; Prock, K.; Krondorfer, P.; Siragy, T.; Dumphart, B. Concurrent validity of smartphone-based markerless motion capturing to quantify lower-limb joint kinematics in healthy and pathological gait. J. Biomech. 2023, 159, 111801. [Google Scholar] [CrossRef] [PubMed]
- Vafadar, S.; Skalli, W.; Bonnet-Lebrun, A.; Assi, A.; Gajny, L. Assessment of a novel deep learning-based marker-less motion capture system for gait study. Gait Posture 2022, 94, 138–143. [Google Scholar] [CrossRef]
- Herrewegen, I.V.D.; Cuppens, K.; Broeckx, M.; Barisch-Fritz, B.; Sloten, J.V.; Leardini, A.; Peeraer, L. Dynamic 3D scanning as a markerless method to calculate multi-segment foot kinematics during stance phase: Methodology and first application. J. Biomech. 2014, 47, 2531–2539. [Google Scholar] [CrossRef]

| Author, Year of Publication | Population of Idiopathic FFF | Models and Movement Conditions | Purpose | Main Results |
|---|---|---|---|---|
| Twomey et al., 2010 [17] | N = 27, age = 11.2 ± 1.2 years, asymptomatic, navicular height during stance phase < 20 mm. Selected from a sample of 94 feet recruited for another study without further information. | Heidelberg, BFSSS. | Comparative analysis between FFF and TDF. | Foot: Increased forefoot supination throughout the whole gait cycle. Lower body: N/A Kinetics: N/A |
| Twomey et al., 2012 [18] | N = 12, age = 12.2 ± 0.4 [11,12] years, asymptomatic, navicular height during stance phase < 20 mm. Subsample from above study. | PiG, BFSSS | Comparative analysis between FFF and TDF. | Foot: N/A Lower body: Increased external hip rotation and greater knee valgus angle in the low arched foot compared to TDF controls. Kinetics: N/A |
| Shih et al., 2012 [19] | N = 20, age = 9.7 ± 0.9 years. The FFF was defined by the Feiss line. Elementary school children. | Electromagnetic tracking, participants wore the same indoor shoes, walking speed was not reported. | Comparative analysis between FFF and TDF. | Foot: No differences in calcaneal angles between FFF and TDF controls. Lower body: Increased hip rotation range from initial contact to peak internal rotation and increased peak knee internal rotation compared to TDF. Kinetics: N/A |
| Hösl et al., 2014 [20] | N = 21, age = 11.0 ± 2.6 years, asymptomatic. N = 14, Age = 11.6 ± 2.0 years. Symptomatic. Patients presented to the clinics because of their FFF. | OFM, Modified PiG [21], BFSSS. | Classification of foot types symptomatic and asymptomatic FFF and TDF. | Foot: No differences in foot kinematics between symptomatic and asymptomatic feet. FFF showed increased eversion, and reduced DF of the rearfoot to tibia and increased DF, supination and abduction of the forefoot to the rearfoot compared to TDF controls Lower body: No differences in foot progression. Kinetics: During loading response Asymptomatic FFF absorbed more energy than TDF. The generated ankle joint energy at push-off showed a significant reduction in symptomatic vs. asymptomatic feet. |
| Kothari et al., 2014 [22] | N = 25, age = [8–15] years. FFF N = 25 Age 11.1 [10.0–12.2] TDF N = 26 Age 12.4 [9.4–13.9] (Same selection method as my other papers) Did not go into symptoms. | OFM with an additional navicular marker added. | Comparative analysis between FFF and TDF regarding navicular motion in different activities. | Foot: Flatfeet demonstrated reduced navicular drift compared to neutral footed children. No difference was observed in navicular drop between groups. Lower body: N/A Kinetics: N/A |
| Portinario et al., 2014 [23] | N = 10, age = 13.1 ± 0.8 years. Patients presented to the clinics because of their FFF but did not require surgical interventions. | Rizzoli, BFSSS. | Examination of the relationship between foot characteristics and clinical observation of rearfoot valgus to optimize the Rizzoli model for use in FFF. | Foot: To improve the correspondence with clinical observation of a valgus orientation of the calcaneus, an additional marker of the attachment area of the Achilles tendon was added. However, in 25% of patients this did not match the clinical observation of rearfoot valgus. A clearer definition of the position of this marker should be defined. Lower body: N/A Kinetics: N/A |
| Kerr et al., 2015 [24] | N = 15, age = 11.5 ± 2.2 years, symptomatic. Selected from patients records in the gait lab. N = 29, age 10.7 ± 3.5 [5–18] years, asymptomatic. They were recruited as part of a larger study to describe typical gait in children without further information. | OFM, barefoot static weightbearing. | Classification of foot types. Asymptomatic and symptomatic FFF. | Foot: Hindfoot eversion and forefoot abduction were much greater in the symptomatic population. Lower body: N/A Kinetics: N/A |
| Kothari et al., 2015 [25] | N = 42, age = 11.9 ± 2.0 years. Children were recruited from the paediatric orthopaedic clinic, orthotic clinic and from the community. | OFM, BFSSS. | Examination of the relationship between foot characteristics and quality of life. | Foot: Increased hindfoot eversion and forefoot supination during gait in FFF compared to TDF. Both parameters are also strongly related to lower quality of life scores. Lower body: N/A Kinetics: N/A |
| Kothari et al., 2016 [26] | N = 48, age = [8–15] years. The majority were recruited from the orthopaedic clinic and were referred because of their FFF. | PiG, BFSSS. | Examination of the relationship between foot characteristics and pain, finding predictors of hip and knee pain. | No kinematic or kinetic parameters associated with a flat foot posture were related to increased proximal joint pain but relations between FFF and various leg and kinetic parameters were shown. Foot: N/A Lower body: A flatter foot posture was associated with increased peak external pelvis rotation in late stance and was also associated with increased knee valgus in midstance. Kinetics: The flat foot posture was significantly associated with a reduction in the second peak of the vertical GRF, which concomitantly reduced late stance hip extension and knee varus and rotation moments. |
| Pothrat et al., 2015 [27] | N = 9, age = 8.2 ± 3.4 years Recruited children had a rearfoot valgus > 4° and a medial arch flattening when standing. | OFM and PiG, BFSSS. | Examination of the relationship between foot characteristics of ankle dorsiflexion of a single segment PiG model to amulltisegment OFM. | Foot: PiG Model showed at heelstrike ankle dorsiflexion and varus, whereas OFM showing plantar flexion and valgus. Lower body: N/A Kinetics: N/A |
| Krautwurst et al., 2016 [28] | N = 16, age = 6.4 ± 2.3 years, painless. N = 10, age = 8.0 ± 2.5 years, painful. They were presented to the clinics because of their FFF. | Heidelberg, barefoot heel raise test. | Examination of the relationship between foot characteristics during the heel raise test to distinguish pain free from painful feet. | Foot: No significant differences were found between the painful and painless groups. Lower body: N/A Kinetics: N/A |
| Jafarnezhadgero et al., 2017 [29] | N = 14, age = 10.2 ± 1.4 [8–12] years. Navicular drop > 10 mm. | PiG, participants wore the same sport shoes, at self-selected walking speed. | Assessment of the effectiveness of orthotic interventions on moments of ankle, knee, and hip joints. | Foot: N/A Lower body: N/A Kinetics: Foot orthoses can decrease the ankle evertor moment, knee and hip abductor moments, and hip flexor moment in the dominant lower limb. |
| Kim et al., 2017 [30] | N = 26, age = 9.5 [7–13] years. Recruited from the outpatient clinic. | Helen Hayes, Orthotrack software 6.6 (Motion Analysis Corp., Santa Rosa, CA, USA), BFSSS. | Comparative analysis between FFF and TDF that were healthy university students with a mean age of 21.3 years. | Foot: N/A Lower body: The range of plantarflexion during push-off was significantly reduced in the FFF compared to TDF controls. At midstance, the knee was significantly more flexed in FFF compared to TDF controls. Kinetics: The mean GRF during the push-off phase was significantly lower for FFF compared to TDF. This concomitantly reduced the mean ankle moment and power |
| Caravaggi et al., 2018 [31] | N = 20, age = 13.3 ± 0.8 years. Presented to the clinics because of their FFF. | Rizzoli, BFSSS. | Comparative analysis between FFF and TDF in midfoot kinematics. | Foot: The midtarsal joint was more dorsiflexed, everted, and abducted In FFF than TDF controls. and showed reduced sagittal-plane RoM. The tarso-metarsal joint was more plantarflexed and adducted, and showed larger frontal-plane RoM. The medial longitudinal arch showed larger RoM and was lower throughout the stance phase of the gait cycle. Lower body: N/A Kinetics: N/A |
| Caravaggi et al., 2018 [14] | N = 13, age = 11.3 ± 1.6 years at surgery. Scheduled for surgery because of their FFF. | Rizzoli, BFSSS. | Assessment of the effectiveness of surgical interventions. Two different arthroereisis implants were compared. | Foot: Both implants appear effective in restoring physiological alignment of the rearfoot; however, the endo-orthotic implant appeared more effective in restoring a more correct frontal-plane mobility of foot joints. Lower body: Knee valgus in stance was not different to TDF Kinetics: The second peak of the GRF is reduced in FFF preoperatively, whereas the first peak was increased compared to TDF. |
| Jafarnezhadgero et al., 2018 [32] | N = 30, age = [8–12] years. Separated into N = 15, orthoses, 10.5 ± 1.4 years, and N = 15 controls 10.4 ± 1.5 years. Recruited from orthopaedic specialists in the local community. Navicular drop > 10 mm, rearfoot eversion > 4° and arch height index < 0.31. | PiG, participants wore the same sport shoes, at self-selected walking speed. | Assessment of the effectiveness of orthotic interventions. In a randomized controlled study, the effects of 4-month treatment with arch support foot orthoses were compared to a placebo condition. | Foot: N/A Lower body: Improvements after 4 months in walking kinematics in maximum ankle internal rotation angle, maximum knee external, and internal rotation angles. Kinetics: Significant lower vertical GRF at push off between FFF and TDF at baseline. First peak of GRF was significantly reduced following 4-month orthotic therapy. |
| Kerr et al., 2019 [33] | N = 19, age = 11.4 ± 2.2 years, symptomatic, recruited from the paediatric orthopaedic clinic. N = 17, age = 9.6 ± 3.2 years, asymptomatic, recruited from the community. | OFM, BFSSS. | Classification of foot types in asymptomatic vs symptomatic FFF. | Foot: The symptomatic group having significantly increased forefoot abduction throughout the stance phase compared to the asymptomatic group. Lower body: The symptomatic FFF group exhibited significant differences compared to the TDF group, showing increased knee flexion angle by 5° and elevated knee valgus angle by 3° at midstance. Kinetics: N/A |
| Böhm et al., 2019 [34] | N = 129, age = 11.7 ± 2.1 years Patients presented to the clinics because of their FFF. | OFM, BFSSS. | Mathematical classification of foot types using 3D-foot kinematics. | Foot: Two clusters of feet could be identified, interpreted as compensated and decompensated feet. Hindfoot to tibia inversion at push-off was the most important discriminator for compensated feet. Deviations of decompensated FFF compared to TDF could be observed in all 3 planes and rearfoot to tibia and forefoot to rearfoot with the largest deviations in the frontal plane rearfoot eversion and forefoot supination. Lower body: N/A Kinetics: N/A |
| Böhm et al., 2020 [35] | N = 204, age = 11.7 ± 1.9 years Patients presented to the clinics because of their FFF. | OFM, BFSSS. | Examination of the relationship between foot characteristics and radiography. | Foot: Three-dimensional foot kinematics showed little to no relation to radiographic measures. Lower body: N/A Kinetics: N/A |
| Kim et al., 2020 [36] | N = 22, 10.8 ± 1.51 years at surgery. Scheduled for surgery because of their FFF. | Helen Hayes, Orthotrack software (Motion Analysis Corp.), BFSSS. | Assessment of the effectiveness of surgical interventions. Calcaneal lengthening procedure was analysed before and 1 year following surgery. | Foot: Ankle valgus angle in the coronal plane was reduced from 35.5° preoperatively to 16.6° postoperatively. Lower body: The preoperative foot progression angle of 20° was normalized to 14° postoperatively. Kinetics: The push-off moment increased from 0.66 Nm/kg preoperatively to 0.83 Nm/kg postoperatively |
| Byrnes et al., 2021 [37] | N = 103, age = 11.7 ± 2.3 years. Patients presented to the clinics because of their FF. Of those N = 19, 11.3 ± 1.9 years underwent surgeries and follow up. | OFM, Modified PiG [38], BFSSS. | Examination of the relationship between foot characteristics with the knee adduction moments (KAM). | Foot: N/A Lower body: Knee valgus angle was not significantly different between FFF and TDF controls. It should be mentioned that children with knee varus/valgus deformities and in- and out-toeing were excluded from the study. Kinetics: Lateral calcaneal shift and arch height correlated with KAM. Only the change in lateral calcaneal shift correlated to the change in KAM following surgery. Children with FFF hat significantly lower peak KAM in the first and second half of stance compared to TDF. |
| Boryczka-Trefler et al., 2022 [39] | N = 49, Age= 6.4 [5.0–10.4] years Presented to the outpatient clinic with an established clinical FFF. | PiG, BFSSS. | Comparative analysis between FFF and TDF: Does the method (static vs. dynamic) of assessing FFF severity influence lower limb kinematic differences compared to TDF? | Only the discrimination by dynamic arch index of >0.27 leads to the following significant differences during walking: Foot: N/A Lower body: The pelvic rotation and ankle ROM was smaller in more severe flatfeet. Kinetics: The maximal values of vertical GRF components in the middle of stance were larger and during push-off were smaller in FFF than in TDF. |
| Böhm and Dussa 2023 [5] | N = 177, age = 11.8 ± 2.2 [7–17] years. Presented to the clinics because of their FFF. Of those N = 31, 11.2 ± 1.4 years underwent arthroereisis surgeries and follow up. | OFM, BFSSS. | Examination of the relationship between foot characteristics and medial arch pain and the relation to the reduction in pain following surgical treatment. | Foot: Pain was perceived in 52% of the feet, of these, 74% was in the medial arch. The calcaneal lateral shift during walking showed a significant difference between the no pain and pain groups and was associated with the reduction in pain following surgery. Lower body: N/A Kinetics: N/A |
| Pourghazi et al., 2023 [40] | N = 7, age = 12.2 ± 2.9 years, Scheduled for surgery because of their FFF. | OFM, BFSSS. | Assessment of the effectiveness of surgical intervention calcaneal lengthening osteotomy before and 6 months after surgery. | Foot: Not reported because of volatile results, e.g., ankle varus in FFF and valgus in TDF. Lower body: External foot progression angle was improved from 11.3 ± 6 to 16.2 ± 7.1 after surgery. The (1 maximum plantar flexion decreased. Kinetics: Peak ankle moments and powers of FFF patients are significantly smaller than TDF. Following surgery ankle moment and power were not significantly different. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Böhm, H.; Stebbins, J.; Kothari, A.; Dussa, C.U. Dynamic Gait Analysis in Paediatric Flatfeet: Unveiling Biomechanical Insights for Diagnosis and Treatment. Children 2024, 11, 604. https://doi.org/10.3390/children11050604
Böhm H, Stebbins J, Kothari A, Dussa CU. Dynamic Gait Analysis in Paediatric Flatfeet: Unveiling Biomechanical Insights for Diagnosis and Treatment. Children. 2024; 11(5):604. https://doi.org/10.3390/children11050604
Chicago/Turabian StyleBöhm, Harald, Julie Stebbins, Alpesh Kothari, and Chakravarthy Ughandar Dussa. 2024. "Dynamic Gait Analysis in Paediatric Flatfeet: Unveiling Biomechanical Insights for Diagnosis and Treatment" Children 11, no. 5: 604. https://doi.org/10.3390/children11050604
APA StyleBöhm, H., Stebbins, J., Kothari, A., & Dussa, C. U. (2024). Dynamic Gait Analysis in Paediatric Flatfeet: Unveiling Biomechanical Insights for Diagnosis and Treatment. Children, 11(5), 604. https://doi.org/10.3390/children11050604






