Investigation of Dental and Oral Health in Children and Adolescents with Special Support Needs from a Child and Adolescent Psychiatric Perspective
Abstract
1. Introduction
Aim of the Study
2. Materials and Methods
2.1. Survey via Online and Paper Questionnaires
2.2. Data Analysis Methods
3. Results
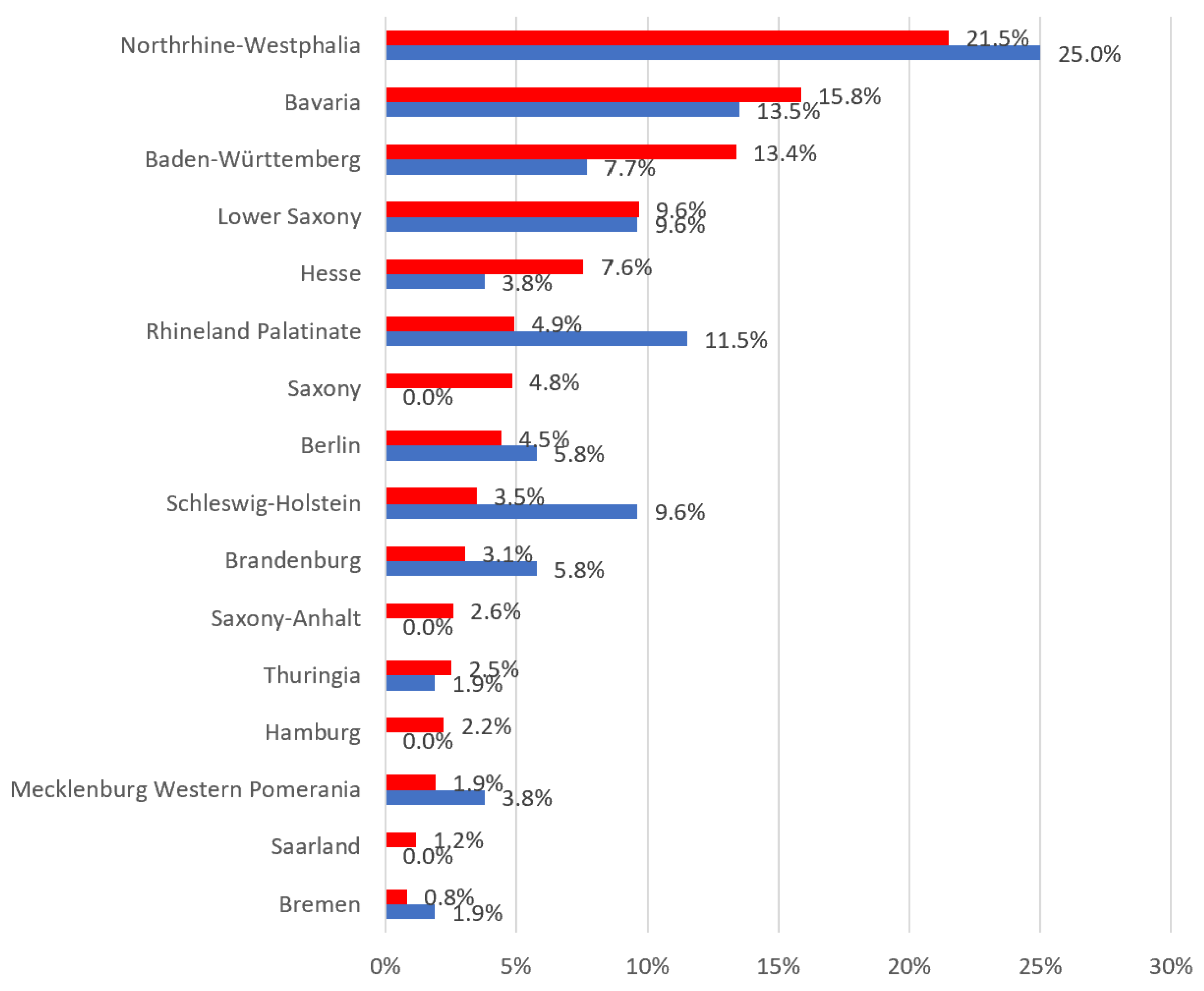
3.1. Sociodemographic Data
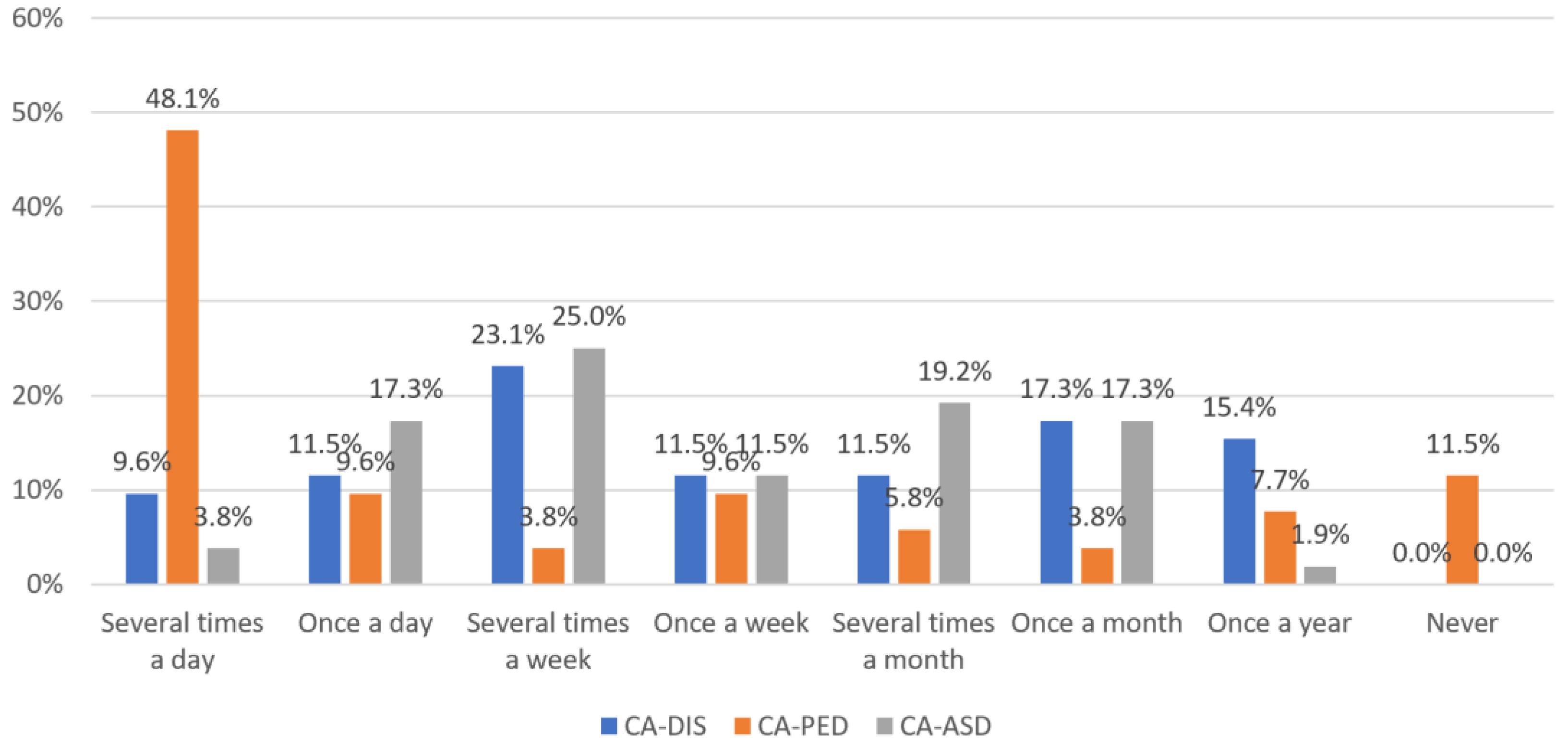
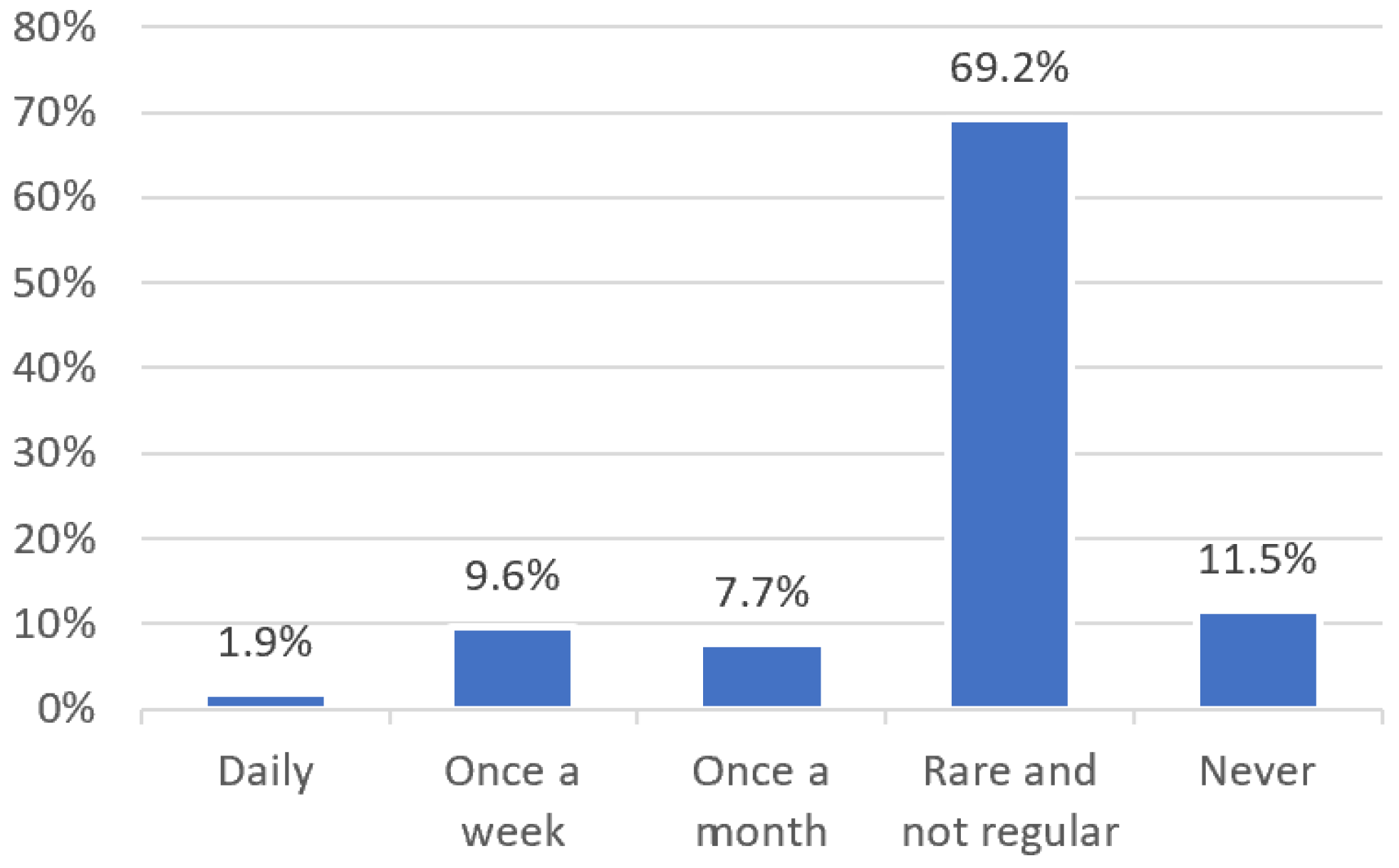
3.2. Relevance of Dental and Oral Health in Child and Adolescent Psychiatric Therapy
- Disorder-Specific Indication: “Primarily in patients with depressive and/or psychotic disorders due to neglect of personal hygiene”
- Patient Concerns: “I don’t specifically inquire about dental health. However, if problems are reported to me, I address them” and “Children and adolescents with dental phobia often seek certification for dental surgery under general anesthesia”
- Lack of Consideration of Dental and Oral Health in Daily Practice: “The topic is primarily discussed with pediatricians, less frequently in CAPPS practices, despite frequent fears and psychosomatic symptoms” and “We have not considered this aspect frequently enough.”
3.3. Explanatory Factors for Poor Oral Health in Children and Adolescents with Special Support Needs
- Behavioral Causes: A lack of cooperation and compliance (21x), inadequate dental care (10x), unhealthy eating and drinking habits (7x), a lack of understanding or insight into dental hygiene importance (6x), a lack of self-care (5x), a lack of independence (2x), a lack of knowledge (2x), low perseverance (1x), general deficits in personal hygiene (1x), unpleasant sensations during toothbrushing (1x)
- Illness-Related Causes: Dental phobia (11x), altered motor skills (e.g., only drinking from a bottle, poor chewing) or disease-related malocclusion (8x), motor difficulties (5x), altered saliva flow (3x), genetic predispositions (2x), reduced pain tolerance (2x), a lack of body awareness (1x), bruxism (1x)
- High Psychosocial Burden on the Family System: Overwhelming of caregivers (5x), a lack of healthcare by caregivers (4x), low priority given to dental health (4x), dental visits perceived as too burdensome (3x), a lack of care and guidance by caregivers (2x), financial burdens (1x) Insufficient Support and Care from the Support System: Inadequate support for caregivers (3x), dental co-treatment or assessment often neglected (1x), dental health often given low priority (1x), dental visits deemed too burdensome (1x)
- Communication Barriers: A lack of or very difficult patient-side communication (e.g., language) (7x)
3.4. Desires and Suggestions for Improving Dental Patient Care and Collaboration
- Expand Cooperation and Networks: Share more information about specialized treatment options or specialized dentists (3x), Enhance region-specific networking on dental health (2x), Enable Research and Education: Provide specific education for CAPPS (2x), Offer specific training for dentists (2x), Expand scientific engagement at the interface of child and adolescent psychiatry and dentistry (2x)
- Structural Changes in Daily Practice: Offer larger time slots where possible (5x), Acquire noiseless drills and low-stimulus treatment rooms (1x)
4. Discussion
5. Strengths and Limitations of the Methodology, Implementation and Data Analysis
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Statistisches Bundesamt. Behinderte Menschen: Schwerbehinderte Menschen am Jahresende. Available online: https://www.destatis.de/DE/Themen/Gesellschaft-Umwelt/Gesundheit/Behinderte-Menschen/Tabellen/geschlecht-behinderung.html (accessed on 9 March 2024).
- Bundespsychotherapeutenkammer. Fast 20 Prozent Erkranken an Einer Psychischen Störung: BPtK-Faktenblatt “Psychische Erkrankungen bei Kindern und Jugendlichen”. Available online: https://bptk.de/pressemitteilungen/fast-20-prozent-erkranken-an-einer-psychischen-stoerung (accessed on 9 March 2024).
- Ravens-Sieberer, U.; Otto, C.; Kriston, L.; Rothenberger, A.; Döpfner, M.; Herpertz-Dahlmann, B.; Barkmann, C.; Schön, G.; Hölling, H.; Schulte-Markwort, M.; et al. The longitudinal BELLA study: Design, methods and first results on the course of mental health problems. Eur. Child Adolesc. Psych. 2015, 24, 651–663. [Google Scholar] [CrossRef]
- Klipker, K.; Baumgarten, F.; Göbel, K.; Lampert, T.; Hölling, H. Psychische Auffälligkeiten bei Kindern und Jugendlichen in Deutschland—Querschnittergebnisse aus KiGGS Welle 2 und Trends. J. Health Monit. 2018, 3, 37–45. [Google Scholar] [CrossRef]
- Schmidt, P.; Egermann, M.; Sauerland, C.; Schulte, A.G. Caries Experience of Adults with Intellectual Disability in the Western Part of Germany. J. Clin. Med. 2021, 10, 2602. [Google Scholar] [CrossRef]
- Schulte, A.G.; Schmidt, P. Mundgesundheit bei Menschen mit Behinderung in Deutschland—Eine Literaturübersicht. Bundesgesundheitsblatt-Gesund. 2021, 64, 793–801. [Google Scholar] [CrossRef]
- Schüler, I.M.; Dziwak, M.; Schmied, K.; Lehmann, T.; Heinrich-Weltzien, R. Mundgesundheit von Kindern und Jugendlichen mit geistiger Behinderung und psychoemotionalen Störungen aus Niedersachsen und Thüringen. Gesundheitswesen 2019, 81, 207–214. [Google Scholar] [CrossRef]
- Wilson, N.J.; Lin, Z.; Villarosa, A.; George, A. Oral health status and reported oral health problems in people with intellectual disability: A literature review. J. Intellect. Dev. Dis. 2019, 44, 292–304. [Google Scholar] [CrossRef]
- Zucoloto, M.L.; Maroco, J.; Campos, J.A.D.B. Impact of oral health on health-related quality of life: A cross-sectional study. BMC Oral Health 2016, 16, 55:1–55:6. [Google Scholar] [CrossRef]
- Heinrich-Weltzien, R.; Wagner, A.; Micheelis, W. Fachwissen und subjektive Behandlung von Kindern mit Behinderungen: Eine Befragung der Thüringer Zahnärzteschaft. Oralprophylaxe Kinderzahnheilkd. 2013, 35, 81–88. [Google Scholar]
- Schmidt, P.; Reis, D.; Schulte, A.G.; Fricke, O. Self-Assessment of Knowledge on the Treatment of Children and Adolescents with Special Care Needs: Results of a Survey amongst German Dentists with Key Expertise in Paediatric Dentistry. J. Pers. Med. 2022, 12, 1173. [Google Scholar] [CrossRef] [PubMed]
- Casamassimo, P.S.; Seale, N.S.; Ruehs, K. General Dentists’ Perceptions of Educational and Treatment Issues Affecting Access to Care for Children with Special Health Care Needs. J. Dent. Educ. 2004, 68, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Dao, L.P.; Zwetchkenbaum, S.; Inglehart, M.R. General Dentists and Special Needs Patients: Does Dental Education Matter? J. Dent. Educ. 2005, 69, 1107–1115. [Google Scholar] [CrossRef]
- Schmidt, P.; Egermann, M.; Ehlers, J.P.; Schulte, A.G. A five-year cohort study on German dental students: Self-assessment in regard to previous experience and attitude toward patients with different types of disability. Spec. Care Dentist. 2023, 43, 829–838. [Google Scholar] [CrossRef]
- Reis, D.; Fricke, O.; Schulte, A.G.; Schmidt, P. Is examining children and adolescents with autism spectrum disorders a challenge?-Measurement of Stress Appraisal (SAM) in German dentists with key expertise in paediatric dentistry. PLoS ONE 2022, 17, e0271406. [Google Scholar] [CrossRef] [PubMed]
- Weil, T.N.; Bagramian, R.A.; Inglehart, M.R. Treating patients with autism spectrum disorder--SCDA members’ attitudes and behavior. Spec. Care Dentist. 2011, 31, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Schüler, I.M.; Bock, B.; Heinrich-Weltzien, R.; Bekes, K.; Rudovsky, M.; Filz, C.; Ligges, C. Status and perception of oral health in 6-17-year-old psychiatric inpatients-randomized controlled trial. Clin. Oral Investig. 2017, 21, 2749–2759. [Google Scholar] [CrossRef] [PubMed]
- Machetanz, E. Probleme zahnärztlicher Behandlung bei geistig und seelisch gestörten Kindern unter dem Aspekt der Jugendpsychiatrie. Zahnärztl. Mitt. 1977, 67, 864–870. [Google Scholar] [PubMed]
- Döring, N.; Bortz, J.; Pöschl, S.; Werner, C.S.; Schermelleh-Engel, K.; Gerhard, C.; Gäde, J.C. Forschungsmethoden und Evaluation in den Sozial- und Humanwissenschaften, 5th ed.; Springer: Berlin/Heidelberg, Germany, 2016; ISBN 978-3-642-41089-5. [Google Scholar]
- Mayring, P. Qualitative Inhaltsanalyse: Grundlagen und Techniken, 13th ed.; Beltz: Weinheim, Basel, Germany, 2022; ISBN 978-3-407-25898-4. [Google Scholar]
- Kassenärztliche Bundesvereinigung. Gesundheitsdaten: Vertragsärztliche Versorgung. Available online: https://gesundheitsdaten.kbv.de/cms/html/16392.php (accessed on 9 March 2024).
- Jones, J.; Roberts, E.; Cockrell, D.; Higgins, D.; Sharma, D. Barriers to Oral Health Care for Autistic Individuals-A Scoping Review. Healthcare 2024, 12, 103. [Google Scholar] [CrossRef] [PubMed]
- Sami, W.; Ahmad, M.S.; Shaik, R.A.; Miraj, M.; Ahmad, S.; Molla, M.H. Oral Health Statuses of Children and Young Adults with Autism Spectrum Disorder: An Umbrella Review. J. Clin. Med. 2023, 13, 59. [Google Scholar] [CrossRef] [PubMed]
- Hasell, S.; Hussain, A.; Da Silva, K. The Oral Health Status and Treatment Needs of Pediatric Patients Living with Autism Spectrum Disorder: A Retrospective Study. Dent. J. 2022, 10, 224. [Google Scholar] [CrossRef]
- Biasotto, M.; Poropat, A.; Porrelli, D.; Ottaviani, G.; Rupel, K.; Preda, M.T.B.; Di Lenarda, R.; Gobbo, M. Dental Treatment in Special Needs Patients and Uncooperative Young Children: A Retrospective Study. Medicina 2024, 60, 91. [Google Scholar] [CrossRef]
- Bossù, M.; Trottini, M.; Corridore, D.; Di Giorgio, G.; Sfasciotti, G.L.; Palaia, G.; Ottolenghi, L.; Polimeni, A.; Di Carlo, S. Oral Health Status of Children with Autism in Central Italy. Appl. Sci. 2020, 10, 2247. [Google Scholar] [CrossRef]
- Pimentel Júnior, N.S.; de Barros, S.G.; de Jesus Filho, E.; Vianna, M.I.P.; Santos, C.M.L.; Cangussu, M.C.T. Oral health-care practices and dental assistance management strategies for people with autism spectrum disorder: An integrative literature review. Autism 2024, 28, 529–539. [Google Scholar] [CrossRef] [PubMed]
- Corridore, D.; Zumbo, G.; Corvino, I.; Guaragna, M.; Bossù, M.; Polimeni, A.; Vozza, I. Prevalence of oral disease and treatment types proposed to children affected by Autistic Spectrum Disorder in Pediatric Dentistry: A Systematic Review. Clin. Ter. 2020, 171, e275–e282. [Google Scholar] [CrossRef] [PubMed]
- Uliana, J.C.; Del’ Agnese, C.C.; Antoniazzi, R.P.; Kantorski, K.Z. Autistic individuals have worse oral status than neurotypical controls: A systematic review and meta-analysis of observational studies. Clin. Oral Investig. 2024, 28, 137. [Google Scholar] [CrossRef] [PubMed]
- Verma, A.; Priyank, H.; Viswanath, B.; Bhagat, J.K.; Purbay, S.; V, M.; Shivakumar, S. Assessment of Parental Perceptions of Socio-Psychological Factors, Unmet Dental Needs, and Barriers to Utilise Oral Health Care in Autistic Children. Cureus 2022, 14, e27950. [Google Scholar] [CrossRef]
- Alqahtani, A.S.; Gufran, K.; Alsakr, A.; Alnufaiy, B.; Al Ghwainem, A.; Bin Khames, Y.M.; Althani, R.A.; Almuthaybiri, S.M. Oral Healthcare Practices and Awareness among the Parents of Autism Spectrum Disorder Children: A Multi-Center Study. Children 2023, 10, 978. [Google Scholar] [CrossRef]
- Kassenärztliche Vereinigung Nordrhein. Die 100 häufigsten ICD-10-Schlüssel und Kurztexte (nach Fachgruppen): 2. Quartal 2022. Available online: https://www.kvno.de/fileadmin/shared/pdf/online/verordnungen/morbiditaetsstatistik/100icd_22-2.pdf (accessed on 25 September 2023).
- Schmidt, P.; Reis, D.; Schulte, A.G.; Fricke, O. Zahnmedizinische Diagnoseprävalenzen bei Kindern, Jugendlichen und jungen Erwachsenen mit psychischen Störungen im Vergleich zu Gesunden-Analyse und Abschätzung kassenärztlicher Abrechnungsdaten (2019). Psychother. Psychosom. Med. Psychol. 2022, 73, 130–138. [Google Scholar] [CrossRef]
- Bundesärztekammer. (Muster-)Fachlich Empfohlene Weiterbildungspläne: Fachlich Empfohlener Weiterbildungsplan für den/die Facharzt für Kinder- und Jugendpsychiatrie und -Psychotherapie. Available online: https://www.bundesaerztekammer.de/fileadmin/user_upload/BAEK/Themen/Aus-Fort-Weiterbildung/Weiterbildung/FEWP/FA_SP-WB/20201112_13_FEWP_KJPP.pdf (accessed on 17 September 2023).
- Ärztekammer Westfalen-Lippe. Weiterbildungsordnung der Ärztekammer Westfalen-Lippe vom 02. April 2022 inkl. Richtlinien über den Inhalt der Weiterbildung. Available online: https://www.aekwl.de/fileadmin/user_upload/aekwl/weiterbildung/Aenderungsfassung_April_2022_-_WO_AEKWL_01.07.2023.pdf (accessed on 17 September 2023).
- Izat, Y. Körperliche Diagnostik in der Kinder- und Jugendpsychiatrie. In Psychiatrie und Psychotherapie des Kindes- und Jugendalters; Fegert, J., Resch, F., Plener, P., Kaess, M., Döpfner, M., Konrad, K., Legenbauer, T., Eds.; Springer: Berlin/Heidelberg, Germany, 2019; pp. 1–7. ISBN 978-3-662-49289-5. [Google Scholar]
| Description of the Sample | Frequencies = 52 | |
|---|---|---|
| Gender | ||
| male | 14 | 26.9% |
| female | 38 | 73.1% |
| Age | ||
| <35 years old | - | - |
| 35–44 years old | 5 | 9.6% |
| 45–54 years old | 11 | 21.2% |
| 55–64 years old | 30 | 57.7% |
| >65 years old | 6 | 11.5% |
| Professional experience (in years) | ||
| less than 5 years | 1 | 1.9% |
| 5–10 years | 2 | 3.8% |
| 11–15 years | 7 | 13.5% |
| 16–20 years | 10 | 19.2% |
| more than 20 years | 32 | 61.5% |
| Current field of activity | ||
| established in own practice | 39 | 75% |
| employed in a hospital as a CAPP | 4 | 7.7% |
| employed as a CAPP in a university clinic | 3 | 5.8% |
| employed in a care center (MVZ) as a CAPP | 3 | 5.8% |
| employed as a CAPP in a practice | 2 | 3.8% |
| employed as an assistant doctor in a practice | 1 | 1.9% |
| Local–regional situation | ||
| village location | 10 | 19.2% |
| urban location | 42 | 80.8% |
| Type of insurance of the patients | ||
| statutorily insured | 90%–95% | |
| privately insured | 5%–10% | |
| Wheelchair-accessible practice | ||
| rooms are wheelchair-accessible | 35 | 67.3% |
| rooms are wheelchair-accessible-furnished | 26 | 50% |
| Dental Anxiety | Teeth and Dental Health | Teeth and Nutrition | Toothache | Teeth and Self-Harm | Dental Aesthetics | Others | |
|---|---|---|---|---|---|---|---|
| CA-DIS | 80.8% (42) | 53.6% (28) | 40.4% (21) | 26.9% (14) | 26.9% (14) | 15.4% (8) | 7.7% (4) |
| CA-PED | 71.2% (37) | 46.2% (24) | 38.5% (20) | 25.0% (13) | 17.3% (9) | 21.2% (11) | 15.4% (8) |
| CA-ASS | 82.7% (43) | 52.0% (27) | 30.8% (16) | 23.1% (12) | 21.2% (11) | 11.5% (6) | 7.7% (4) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fornefeld, D.; Fricke, O.; Schulte, A.G.; Schmidt, P. Investigation of Dental and Oral Health in Children and Adolescents with Special Support Needs from a Child and Adolescent Psychiatric Perspective. Children 2024, 11, 355. https://doi.org/10.3390/children11030355
Fornefeld D, Fricke O, Schulte AG, Schmidt P. Investigation of Dental and Oral Health in Children and Adolescents with Special Support Needs from a Child and Adolescent Psychiatric Perspective. Children. 2024; 11(3):355. https://doi.org/10.3390/children11030355
Chicago/Turabian StyleFornefeld, Dustin, Oliver Fricke, Andreas G. Schulte, and Peter Schmidt. 2024. "Investigation of Dental and Oral Health in Children and Adolescents with Special Support Needs from a Child and Adolescent Psychiatric Perspective" Children 11, no. 3: 355. https://doi.org/10.3390/children11030355
APA StyleFornefeld, D., Fricke, O., Schulte, A. G., & Schmidt, P. (2024). Investigation of Dental and Oral Health in Children and Adolescents with Special Support Needs from a Child and Adolescent Psychiatric Perspective. Children, 11(3), 355. https://doi.org/10.3390/children11030355








