Suspected Simple Appendicitis in Children: Should We Use a Nonoperative, Antibiotic-Free Approach? An Observational Study
Abstract
1. Introduction
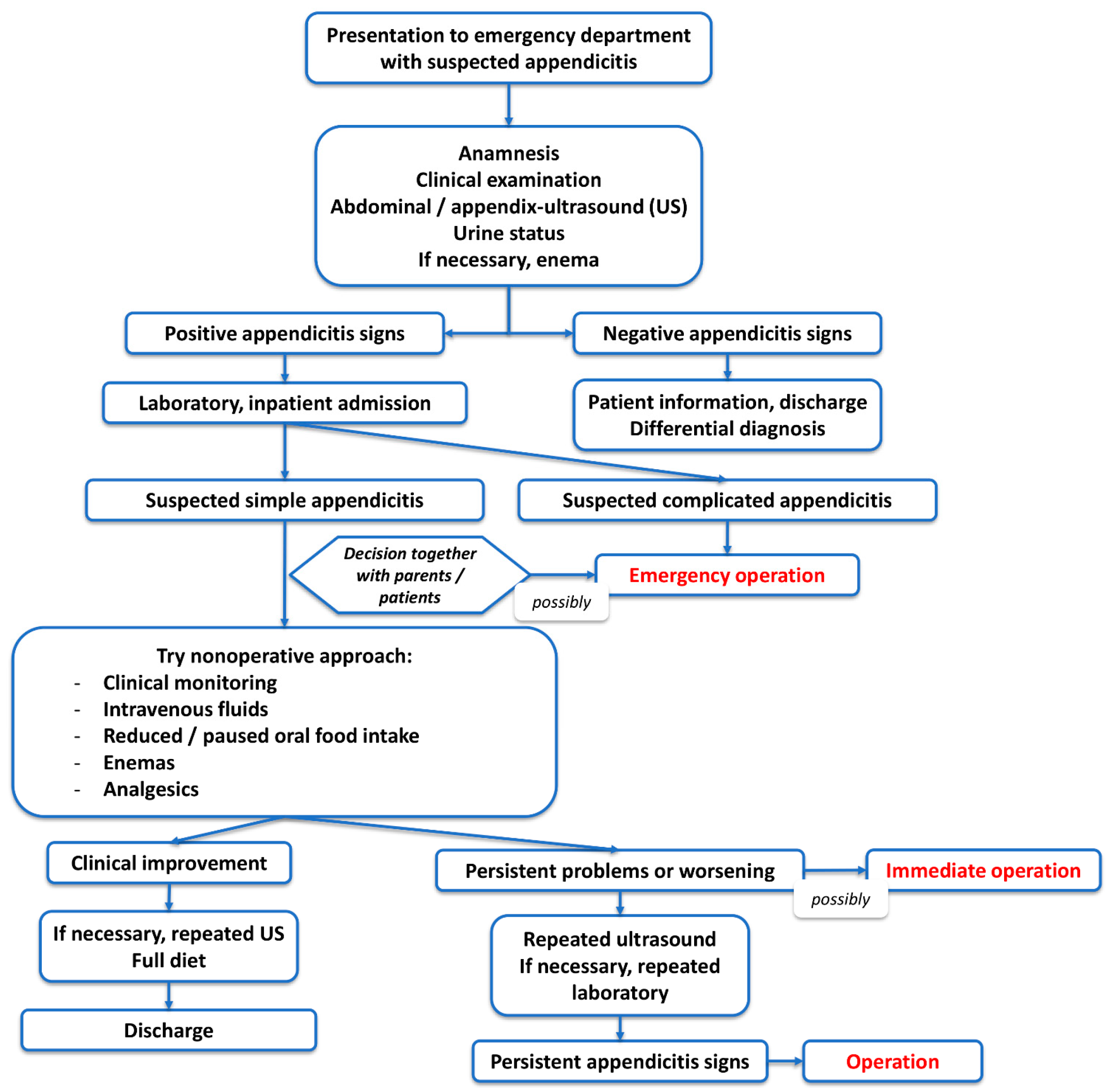
2. Materials and Methods
2.1. Study Design, Population, and Parameters
- ▪
- Patient demographic data: Age and sex.
- ▪
- Clinical signs and symptoms: Nausea or vomiting, right lower quadrant (RLQ) tenderness, rebound pain, and fever.
- ▪
- Ultrasonographic findings: Free intraabdominal fluid, visible appendix, appendix diameter, and appendicolith.
- ▪
- Biochemical parameters: Leukocytosis, C-reactive protein (CRP) elevation, and neutrophilia.
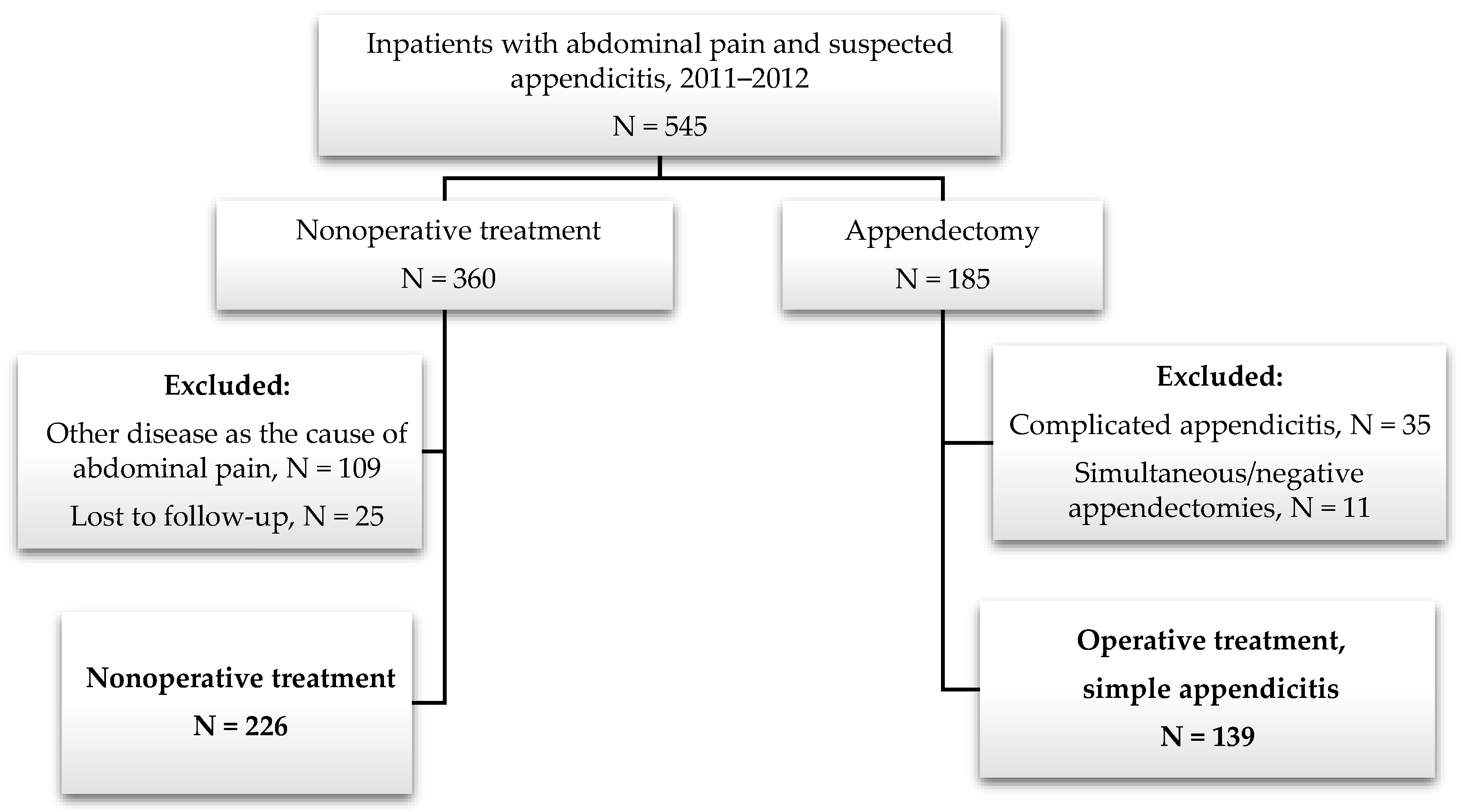
2.2. Inclusion and Exclusion Criteria
2.3. Subgroup of Nonoperatively Treated Patients
2.4. Outcomes of Interest
2.5. Statistical Analysis
3. Results
3.1. Study Population
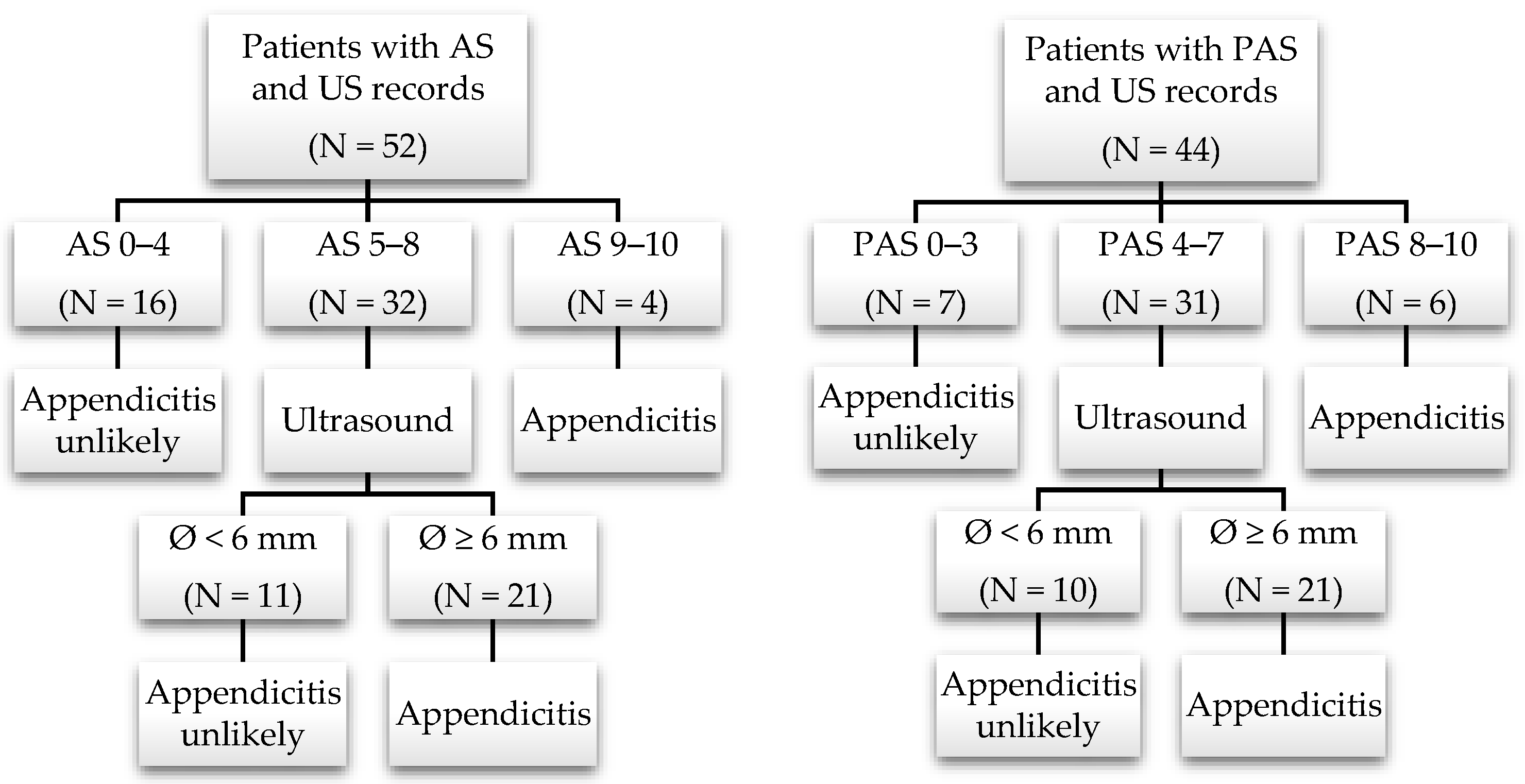
Nonoperative Treatment: Subgroup with Available Appendicitis Scores and Appendix Diameter on US
3.2. Population Characteristics and Parameters
3.3. Outcomes
3.3.1. Length of Hospital Stay during Index Hospitalization
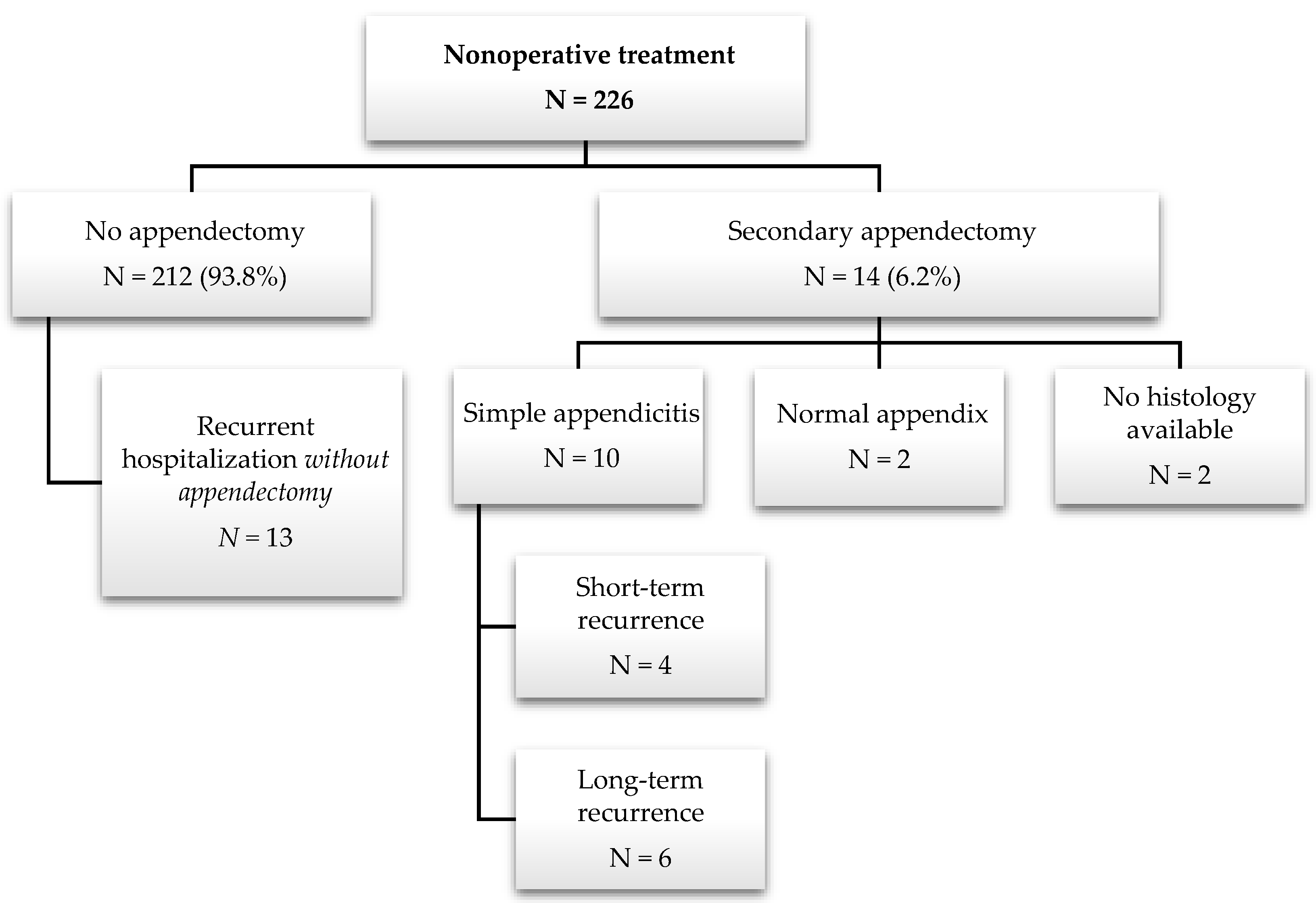
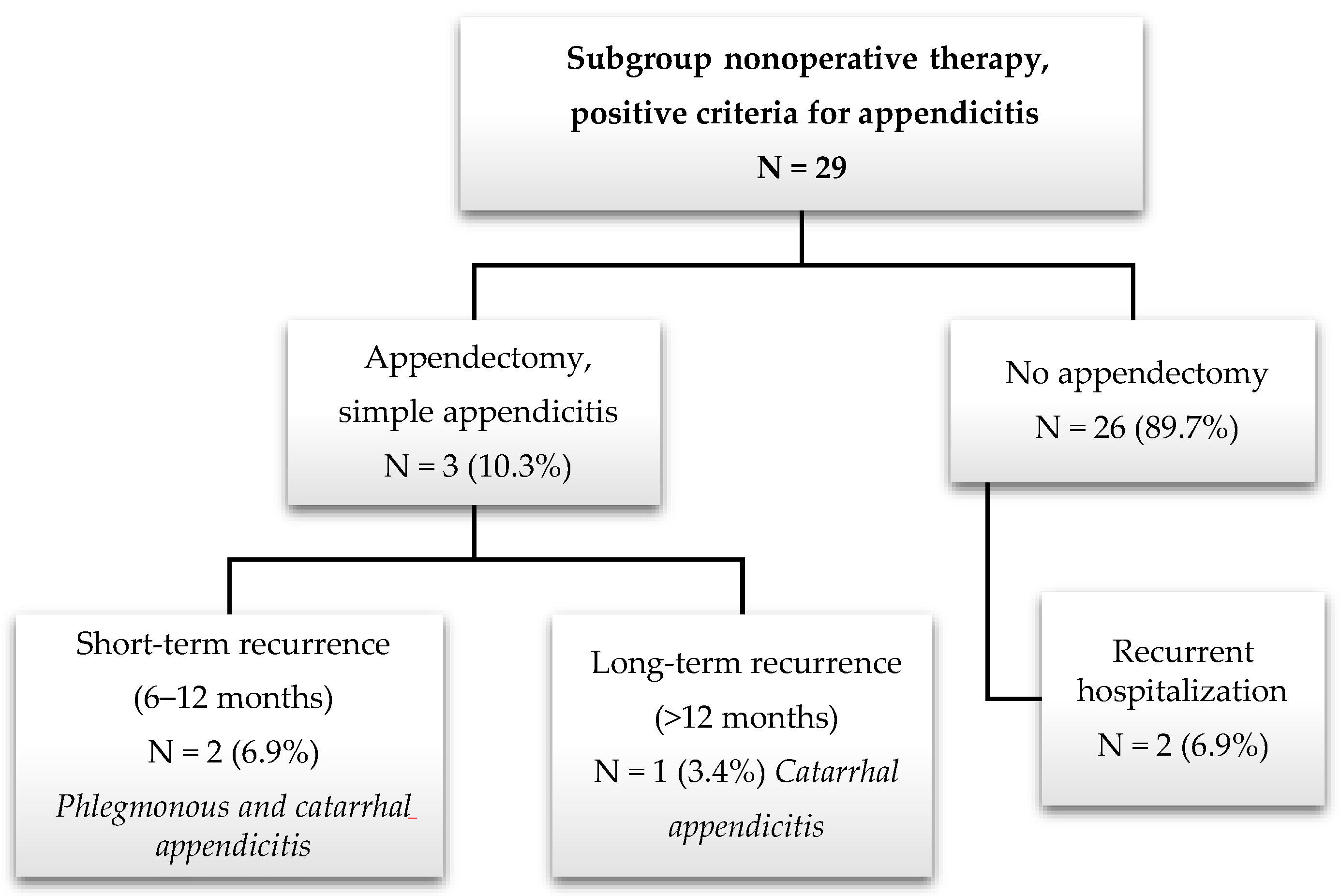
3.3.2. Follow-Up after Nonoperative Treatment: Secondary Appendectomies, Recurrent Abdominal Pain, and Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
References
- Morrow, S.E.; Newman, K.D. Current management of appendicitis. Semin. Pediatr. Surg. 2007, 16, 34–40. [Google Scholar] [CrossRef]
- Hontschik, B. Kurze Geschichte der Appendektomie: Mythen, Fakten, Perspektiven; Marseille-Verlag: München, Germany, 2012; ISBN 9783886161423. [Google Scholar]
- Di Saverio, S.; Podda, M.; de Simone, B.; Ceresoli, M.; Augustin, G.; Gori, A.; Boermeester, M.; Sartelli, M.; Coccolini, F.; Tarasconi, A.; et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J. Emerg. Surg. WJES 2020, 15, 27. [Google Scholar] [CrossRef] [PubMed]
- Flum, D.R.; Davidson, G.H.; Monsell, S.E.; Shapiro, N.I.; Odom, S.R.; Sanchez, S.E.; Drake, F.T.; Fischkoff, K.; Johnson, J.; Patton, J.H.; et al. A Randomized Trial Comparing Antibiotics with Appendectomy for Appendicitis. N. Engl. J. Med. 2020, 383, 1907–1919. [Google Scholar] [CrossRef] [PubMed]
- Lamm, R.; Kumar, S.S.; Collings, A.T.; Haskins, I.N.; Abou-Setta, A.; Narula, N.; Nepal, P.; Hanna, N.M.; Athanasiadis, D.I.; Scholz, S.; et al. Diagnosis and treatment of appendicitis: Systematic review and meta-analysis. Surg. Endosc. 2023, 37, 8933–8990. [Google Scholar] [CrossRef] [PubMed]
- Svensson, J.F.; Patkova, B.; Almström, M.; Naji, H.; Hall, N.J.; Eaton, S.; Pierro, A.; Wester, T. Nonoperative treatment with antibiotics versus surgery for acute nonperforated appendicitis in children: A pilot randomized controlled trial. Ann. Surg. 2015, 261, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Svensson, J.F.; Hall, N.J.; Eaton, S.; Pierro, A.; Wester, T. A review of conservative treatment of acute appendicitis. Eur. J. Pediatr. Surg. 2012, 22, 185–194. [Google Scholar] [CrossRef] [PubMed]
- Lawrence, A.E.; Deans, K.J.; Minneci, P.C. The Criteria for Treating Appendicitis Non-operatively. Curr. Surg. Rep. 2018, 6, 10. [Google Scholar] [CrossRef]
- Decker, E.; Ndzi, A.; Kenny, S.; Harwood, R. Systematic Review and Meta-analysis to Compare the Short- and Long-term Outcomes of Non-operative Management with Early Operative Management of Simple Appendicitis in Children After the COVID-19 Pandemic. J. Pediatr. Surg. 2023. [Google Scholar] [CrossRef]
- Hutchings, N.; Wood, W.; Reading, I.; Walker, E.; Blazeby, J.M.; Van’t Hoff, W.; Young, B.; Crawley, E.M.; Eaton, S.; Chorozoglou, M.; et al. CONTRACT Study—CONservative TReatment of Appendicitis in Children (feasibility): Study protocol for a randomised controlled Trial. Trials 2018, 19, 153. [Google Scholar] [CrossRef]
- Kessler, U.; Mosbahi, S.; Walker, B.; Hau, E.M.; Cotton, M.; Peiry, B.; Berger, S.; Egger, B. Conservative treatment versus surgery for uncomplicated appendicitis in children: A systematic review and meta-analysis. Arch. Dis. Child. 2017, 102, 1118–1124. [Google Scholar] [CrossRef]
- Podda, M.; Gerardi, C.; Cillara, N.; Fearnhead, N.; Gomes, C.A.; Birindelli, A.; Mulliri, A.; Davies, R.J.; Di Saverio, S. Antibiotic Treatment and Appendectomy for Uncomplicated Acute Appendicitis in Adults and Children: A Systematic Review and Meta-analysis. Ann. Surg. 2019, 270, 1028–1040. [Google Scholar] [CrossRef]
- Oktay, C.; Goksu, M.; Yavuz, S. Prevalence of appendicolith in children with acute appendicitis and its correlation with disease severity. North. Clin. Istanb. 2023, 10, 631–635. [Google Scholar] [CrossRef]
- Rentea, R.M.; Peter, S.D.S.; Snyder, C.L. Pediatric appendicitis: State of the art review. Pediatr. Surg. Int. 2017, 33, 269–283. [Google Scholar] [CrossRef]
- Lamps, L.W. Appendicitis and infections of the appendix. Semin. Diagn. Pathol. 2004, 21, 86–97. [Google Scholar] [CrossRef]
- Carr, N.J. The pathology of acute appendicitis. Ann. Diagn. Pathol. 2000, 4, 46–58. [Google Scholar] [CrossRef]
- Ohba, G.; Hirobe, S.; Komori, K. The Usefulness of Combined B Mode and Doppler Ultrasonography to Guide Treatment of Appendicitis. Eur. J. Pediatr. Surg. 2016, 26, 533–536. [Google Scholar] [CrossRef] [PubMed]
- Park, H.C.; Kim, M.J.; Lee, B.H. Randomized clinical trial of antibiotic therapy for uncomplicated appendicitis. Br. J. Surg. 2017, 104, 1785–1790. [Google Scholar] [CrossRef] [PubMed]
- Andersson, R.E. The natural history and traditional management of appendicitis revisited: Spontaneous resolution and predominance of prehospital perforations imply that a correct diagnosis is more important than an early diagnosis. World J. Surg. 2007, 31, 86–92. [Google Scholar] [CrossRef]
- Andersson, R.E. Does Delay of Diagnosis and Treatment in Appendicitis Cause Perforation? World J. Surg. 2016, 40, 1315–1317. [Google Scholar] [CrossRef] [PubMed]
- Bhangu, A.; Søreide, K.; Di Saverio, S.; Assarsson, J.H.; Drake, F.T. Acute appendicitis: Modern understanding of pathogenesis, diagnosis, and management. Lancet 2015, 386, 1278–1287. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.K.; Strait, R.T.; Sato, T.T.; Hennes, H.M. A randomized clinical trial of analgesia in children with acute abdominal pain. Acad. Emerg. Med. 2002, 9, 281–287. [Google Scholar] [CrossRef] [PubMed]
- Green, R.; Bulloch, B.; Kabani, A.; Hancock, B.J.; Tenenbein, M. Early analgesia for children with acute abdominal pain. Pediatrics 2005, 116, 978–983. [Google Scholar] [CrossRef] [PubMed]
- Gorter, R.R.; van der Lee, J.H.; Heijsters, F.A.C.J.; Cense, H.A.; Bakx, R.; Kneepkens, C.M.F.; Wijnen, M.H.; van der Steeg, A.F.W.; In’t Hof, K.H.; Offringa, M.; et al. Outcome of initially nonoperative treatment for acute simple appendicitis in children. J. Pediatr. Surg. 2018, 53, 1849–1854. [Google Scholar] [CrossRef]
- Marcinkevics, R.; Reis Wolfertstetter, P.; Wellmann, S.; Knorr, C.; Vogt, J.E. Using Machine Learning to Predict the Diagnosis, Management and Severity of Pediatric Appendicitis. Front. Pediatr. 2021, 9, 662183. [Google Scholar] [CrossRef] [PubMed]
- Alvarado, A. A practical score for the early diagnosis of acute appendicitis. Ann. Emerg. Med. 1986, 15, 557–564. [Google Scholar] [CrossRef]
- Samuel, M. Pediatric appendicitis score. J. Pediatr. Surg. 2002, 37, 877–881. [Google Scholar] [CrossRef] [PubMed]
- Escribá, A.; Gamell, A.M.; Fernández, Y.; Quintillá, J.M.; Cubells, C.L. Prospective validation of two systems of classification for the diagnosis of acute appendicitis. Pediatr. Emerg. Care 2011, 27, 165–169. [Google Scholar] [CrossRef]
- Saucier, A.; Huang, E.Y.; Emeremni, C.A.; Pershad, J. Prospective evaluation of a clinical pathway for suspected appendicitis. Pediatrics 2014, 133, e88–e95. [Google Scholar] [CrossRef]
- Schülin, S.; Schlichting, N.; Blod, C.; Opitz, S.; Suttkus, A.; Stingu, C.S.; Barry, K.; Lacher, M.; Bühligen, U.; Mayer, S. The intra- and extraluminal appendiceal microbiome in pediatric patients: A comparative study. Medicine 2017, 96, e9518. [Google Scholar] [CrossRef]
- Mussack, T.; Schmidbauer, S.; Nerlich, A.; Schmidt, W.; Hallfeldt, K.K. Die chronische Appendizitis als eigenständige klinische Entität. Chirurg 2002, 73, 710–715. [Google Scholar] [CrossRef]
- Jukić, M.; Nizeteo, P.; Matas, J.; Pogorelić, Z. Trends and Predictors of Pediatric Negative Appendectomy Rates: A Single-Centre Retrospective Study. Children 2023, 10, 887. [Google Scholar] [CrossRef]
- Dingemann, J.; Ure, B. Imaging and the use of scores for the diagnosis of appendicitis in children. Eur. J. Pediatr. Surg. 2012, 22, 195–200. [Google Scholar] [CrossRef]
- Nepogodiev, D.; Wilkin, R.J.W.; Bradshaw, C.J.; Skerritt, C.; Ball, A.; Moni-Nwinia, W.; Blanco-Colino, R.; Chauhan, P.; Drake, T.M.; Frasson, M.; et al. Appendicitis risk prediction models in children presenting with right iliac fossa pain (RIFT study): A prospective, multicentre validation study. Lancet Child. Adolesc. Health 2020, 4, 271–280. [Google Scholar] [CrossRef]
- Park, H.-C.; Kim, B.-S.; Lee, B.H. Efficacy of short-term antibiotic therapy for consecutive patients with mild appendicitis. Am. Surg. 2011, 77, 752–755. [Google Scholar] [CrossRef] [PubMed]
- Stackievicz, R.; Milner, R.; Werner, M.; Arnon, S.; Steiner, Z. Follow-up ultrasonographic findings among children treated conservatively for uncomplicated acute appendicitis. Pediatr. Radiol. 2023, 53, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Andersson, R.; Hugander, A.; Thulin, A.; Nyström, P.O.; Olaison, G. Indications for operation in suspected appendicitis and incidence of perforation. BMJ 1994, 308, 107–110. [Google Scholar] [CrossRef]
- Kiss, N.; Minderjahn, M.; Reismann, J.; Svensson, J.; Wester, T.; Hauptmann, K.; Schad, M.; Kallarackal, J.; von Bernuth, H.; Reismann, M. Use of gene expression profiling to identify candidate genes for pretherapeutic patient classification in acute appendicitis. BJS Open 2021, 5, zraa045. [Google Scholar] [CrossRef] [PubMed]
- Migraine, S.; Atri, M.; Bret, P.M.; Lough, J.O.; Hinchey, J.E. Spontaneously resolving acute appendicitis: Clinical and sonographic documentation. Radiology 1997, 205, 55–58. [Google Scholar] [CrossRef]
- Huang, L.; Yin, Y.; Yang, L.; Wang, C.; Li, Y.; Zhou, Z. Comparison of Antibiotic Therapy and Appendectomy for Acute Uncomplicated Appendicitis in Children: A Meta-analysis. JAMA Pediatr. 2017, 171, 426–434. [Google Scholar] [CrossRef]
- Salminen, P.; Sippola, S.; Haijanen, J.; Nordström, P.; Rantanen, T.; Rautio, T.; Sallinen, V.; Löyttyniemi, E.; Hurme, S.; Tammilehto, V.; et al. Antibiotics versus placebo in adults with CT-confirmed uncomplicated acute appendicitis (APPAC III): Randomized double-blind superiority trial. Br. J. Surg. 2022, 109, 503–509. [Google Scholar] [CrossRef]
- Randal Bollinger, R.; Barbas, A.S.; Bush, E.L.; Lin, S.S.; Parker, W. Biofilms in the large bowel suggest an apparent function of the human vermiform appendix. J. Theor. Biol. 2007, 249, 826–831. [Google Scholar] [CrossRef]
- Petruzziello, C.; Saviano, A.; Ojetti, V. Probiotics, the Immune Response and Acute Appendicitis: A Review. Vaccines 2023, 11, 1170. [Google Scholar] [CrossRef]
- Hall, N.J.; Eaton, S.; Sherratt, F.C.; Reading, I.; Walker, E.; Chorozoglou, M.; Beasant, L.; Wood, W.; Stanton, M.; Corbett, H.; et al. CONservative TReatment of Appendicitis in Children: A randomised controlled feasibility Trial (CONTRACT). Arch. Dis. Child. 2021, 106, 764–773. [Google Scholar] [CrossRef]
- Vandevelde, A.; Gera, P. Carcinoid tumours of the appendix in children having appendicectomies at Princess Margaret Hospital since 1995. J. Pediatr. Surg. 2015, 50, 1595–1599. [Google Scholar] [CrossRef] [PubMed]
- Lobeck, I.N.; Jeste, N.; Geller, J.; Pressey, J.; von Allmen, D. Surgical management and surveillance of pediatric appendiceal carcinoid tumor. J. Pediatr. Surg. 2017, 52, 925–927. [Google Scholar] [CrossRef] [PubMed]
- Pogorelić, Z.; Ercegović, V.; Bašković, M.; Jukić, M.; Karaman, I.; Mrklić, I. Incidence and Management of Appendiceal Neuroendocrine Tumors in Pediatric Population: A Bicentric Experience with 6285 Appendectomies. Children 2023, 10, 1889. [Google Scholar] [CrossRef] [PubMed]
- Marcinkevičs, R.; Reis Wolfertstetter, P.; Klimiene, U.; Chin-Cheong, K.; Paschke, A.; Zerres, J.; Denzinger, M.; Niederberger, D.; Wellmann, S.; Ozkan, E.; et al. Interpretable and intervenable ultrasonography-based machine learning models for pediatric appendicitis. Med. Image Anal. 2023, 91, 103042. [Google Scholar] [CrossRef]
| Alvarado Score (AS) | Pediatric Appendicitis Score (PAS) | ||
|---|---|---|---|
| Diagnostic Criteria | Value | Diagnostic Criteria | Value |
| Migration of pain | 1 | Migration of pain | 1 |
| Anorexia/Ketones in urine | 1 | Anorexia | 1 |
| Nausea/Vomiting | 1 | Nausea/Emesis | 1 |
| Tenderness in the right lower quadrant | 2 | Tenderness in the right lower quadrant | 2 |
| Rebound pain | 1 | Cough/Percussion/Hopping tenderness | 2 |
| Elevation of temperature (≥37.3 °C) | 1 | Fever (≥38 °C) | 1 |
| Leukocytosis (≥10.000/µL) | 2 | Leukocytosis (≥10.000/µL) | 1 |
| Neutrophilia (≥75%) | 1 | Neutrophilia (≥75%) | 1 |
| Included | Excluded |
|---|---|
| Hospital admission to the pediatric surgery unit due to abdominal pain and suspected appendicitis. | Outpatients. |
| Age < 18 years. | Patients who have undergone appendectomy before. |
| Surgical group: histological uncomplicated appendicitis (catarrhal, phlegmonous, or chronic). | Surgical group: negative and incidental appendectomy, complicated appendicitis (gangrenous, abscess, or perforated). |
| Another relevant diagnosis as the cause of abdominal pain (intussusception, pneumonia, or ovarian torsion) or relevant comorbidities (neoplasia or chronic intestinal disease, such as Crohn’s disease and ulcerative colitis). | |
| Conservative group: antibiotics during hospitalization; loss to follow-up. |
| Parameters * | Appendectomy N = 139 | Nonoperative Treatment N = 226 | p-Value § | Subgroup Nonoperative Treatment N = 29 | p-Value §§ |
|---|---|---|---|---|---|
| Demographics | |||||
| Sex | 0.161 | 0.686 | |||
| Male | 75 (54%) | 104 (46%) | 17 (59%) | ||
| Female | 64 (46%) | 122 (54%) | 12 (41%) | ||
| Age in years (mean) | 10.8 (SD 3.4) | 10.6 (SD 3.3) | 0.501 | 10 (SD 2.3) | 0.249 |
| Inflammatory parameters | |||||
| Leukocytosis (≥10/nL) | 104 b (75%) | 108 a (48%) | 0.000 | 23 (79%) | 0.812 |
| CRP elevated (>5 mg/L) | 92 c (68%) | 73 (32%) | 0.000 | 14 (48%) | 0.057 |
| Neutrophilia (≥75%) | 97 e (73%) | 66 d (30%) | 0.000 | 15 (52%) | 0.044 |
| Clinical parameters | |||||
| Nausea or vomiting (yes) | 69 f (57%) | 94 a (42%) | 0.010 | 17 (59%) | 1.000 |
| RLQ tenderness (yes) | 138 (99%) | 197 a (88%) | 0.000 | 29 (100%) | 1.000 |
| Rebound pain (yes) | 56 h (50%) | 42 g (20%) | 0.000 | 9 o (32%) | 0.137 |
| Fever (temp. ≥ 38 °C) | 64 (46%) | 40 (18%) | 0.000 | 7 (24%) | 0.038 |
| Ultrasound records | |||||
| Free intraabdominal fluid + | 47 j (37%) | 46 i (21%) | 0.002 | 6 o (21%) | 0.129 |
| Visible appendix + | 69 l (54%) | 61 k (28%) | 0.000 | 29 (100%) | 0.000 |
| Appendix diameter in mm (mean) | 7.6 n (SD 1.6) | 6.6 m (SD 2.4) | 0.009 | 7.5 (SD 2.2) | 0.835 |
| Length of hospital stay | |||||
| Days (mean) | 4.5 (SD 2.7) | 1.9 (SD 0.8) | 0.000 | 2.1 (SD 0.9) | 0.000 |
| Primary Appendectomy Group | N = 139 |
|---|---|
| Phlegmonous appendicitis | 106 (76.3%) |
| Catarrhal appendicitis | 20 (14.4%) |
| Chronic appendicitis | 13 (9.3%) |
| Secondary Appendectomy Group | N = 14 |
|---|---|
| Phlegmonous appendicitis | 4 (28.6%) |
| Catarrhal appendicitis | 3 (21.4%) |
| Chronic appendicitis | 3 (21.4%) |
| Normal appendix | 2 (14.3%) |
| No histology available * | 2 (14.3%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Reis Wolfertstetter, P.; Ebert, J.B.; Barop, J.; Denzinger, M.; Kertai, M.; Schlitt, H.J.; Knorr, C. Suspected Simple Appendicitis in Children: Should We Use a Nonoperative, Antibiotic-Free Approach? An Observational Study. Children 2024, 11, 340. https://doi.org/10.3390/children11030340
Reis Wolfertstetter P, Ebert JB, Barop J, Denzinger M, Kertai M, Schlitt HJ, Knorr C. Suspected Simple Appendicitis in Children: Should We Use a Nonoperative, Antibiotic-Free Approach? An Observational Study. Children. 2024; 11(3):340. https://doi.org/10.3390/children11030340
Chicago/Turabian StyleReis Wolfertstetter, Patricia, John Blanford Ebert, Judith Barop, Markus Denzinger, Michael Kertai, Hans J. Schlitt, and Christian Knorr. 2024. "Suspected Simple Appendicitis in Children: Should We Use a Nonoperative, Antibiotic-Free Approach? An Observational Study" Children 11, no. 3: 340. https://doi.org/10.3390/children11030340
APA StyleReis Wolfertstetter, P., Ebert, J. B., Barop, J., Denzinger, M., Kertai, M., Schlitt, H. J., & Knorr, C. (2024). Suspected Simple Appendicitis in Children: Should We Use a Nonoperative, Antibiotic-Free Approach? An Observational Study. Children, 11(3), 340. https://doi.org/10.3390/children11030340