Laryngeal Mask Airway Versus Endotracheal Intubation during Lacrimal Duct Stenosis Surgery in Children—A Retrospective Analysis
Abstract
1. What Is Already Known
- -
- The use of laryngeal masks for airway management has become increasingly important in the field of pediatric anesthesia in recent years.
2. What Is New
- -
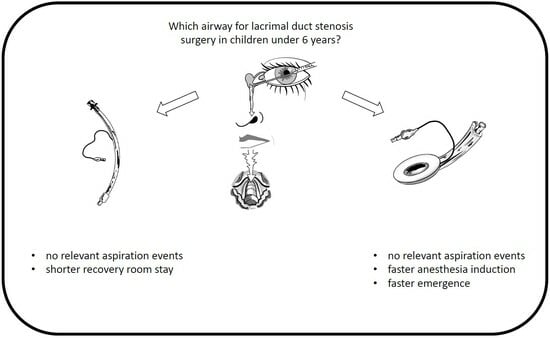
- The use of laryngeal masks for probing, dilating, and irrigating lacrimal duct stenosis results in significantly shorter induction and emergence times in pediatric patients younger than 6 years of age.
- -
- Compared to endotracheal intubation, the use of laryngeal masks does not increase complications; some complications typically associated with endotracheal intubation could be avoided, despite secretions and the release of pus into the upper airway. Signs of relevant lower airway aspiration do not appear to occur.
3. Introduction
4. Materials and Methods
4.1. Ethics Committee Approval, In-Exclusion-Criteria and Endpoints
4.2. Patient and Data Selection
4.3. General Anesthesia Administration and Documentation
4.4. Performing Lacrimal Duct Surgery
4.5. Statistical Analysis
5. Results
5.1. Demographic Data
5.2. Anesthesia Performance
5.3. Postoperative Pain Management
5.4. Oxygen and Saturation
5.5. Anesthesia Duration
5.6. Adverse Events
6. Discussion
7. Limitations
8. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Guth, J.; Jung, P.; Schiele, A.; Urban, B.; Parsch, A.; Matsche, B.; Eich, C.; Becke-Jakob, K.; Landsleitner, B.; Russo, S.G.; et al. Update 2022: Interdisciplinary statement on airway management with supraglottic airway devices in pediatric emergency medicine-The laryngeal mask is and remains state of the art: Joint statement of the Institute for Emergency Medicine and Medicine Management (INM), the University Clinic Munich, LMU Munich, Germany, the Working Group for Pediatric Critical Care and Emergency Medicine of the German Interdisciplinary Society for Critical Care and Emergency Medicine (DIVI), the Medical Directors of Emergency Medical Services in Bavaria (ALRD), the Scientific Working Group for Pediatric Anesthesia (WAKKA) of the German Society for Anesthesiology and Intensive Care Medicine (DGAI), the Scientific Working Group for Emergency Medicine of the German Society for Anesthesiology and Intensive Care Medicine (DGAI) and the Society of Neonatology and Pediatric Critical Care Medicine (GNPI). Anaesthesiologie 2023, 72, 425–432. [Google Scholar] [CrossRef]
- Eguia, A.; Jiang, Z.Y.; Brollier, L.; Matuszczak, M.; Yuksel, S.; Roy, S.; Huang, Z. Reducing intraoperative time with laryngeal mask airway and stretcher in pediatric adenotonsillectomy. Am. J. Otolaryngol. 2022, 43, 103195. [Google Scholar] [CrossRef]
- Martinez-de Los Santos, C.A.; Cruz-Cruz, E.F. Laryngeal mask in pediatrics. Rev. Esp. Anestesiol. Reanim. Engl. Ed. 2022, 69, 315–316. [Google Scholar] [CrossRef]
- Gordon, J.; Cooper, R.M.; Parotto, M. Supraglottic airway devices: Indications, contraindications and management. Minerva Anestesiol. 2018, 84, 389–397. [Google Scholar] [CrossRef]
- Waldschmidt, B.; Gordon, N. Anesthesia for pediatric ophthalmologic surgery. J. AAPOS 2019, 23, 127–131. [Google Scholar] [CrossRef]
- Engelhardt, T.; Fiadjoe, J.E.; Weiss, M.; Baker, P.; Bew, S.; Echeverry Marin, P.; von Ungern-Sternberg, B.S. A framework for the management of the pediatric airway. Paediatr. Anaesth. 2019, 29, 985–992. [Google Scholar] [CrossRef] [PubMed]
- Disma, N.; Asai, T.; Cools, E.; Cronin, A.; Engelhardt, T.; Fiadjoe, J.; Fuchs, A.; Garcia-Marcinkiewicz, A.; Habre, W.; Heath, C.; et al. Airway management in neonates and infants: European Society of Anaesthesiology and Intensive Care and British Journal of Anaesthesia joint guidelines. Eur. J. Anaesthesiol. 2024, 41, 3–23. [Google Scholar] [CrossRef] [PubMed]
- Sunder, R.A.; Joshi, C. A technique to improve the safety of laryngeal mask airway when used in lacrimal duct surgery. Paediatr. Anaesth. 2006, 16, 130–133. [Google Scholar] [CrossRef] [PubMed]
- Schnall, B.M. Pediatric nasolacrimal duct obstruction. Curr. Opin. Ophthalmol. 2013, 24, 421–424. [Google Scholar] [CrossRef]
- MacEwen, C.J.; Young, J.D. Epiphora during the first year of life. Eye 1991, 5 Pt 5, 596–600. [Google Scholar] [CrossRef] [PubMed]
- Vagge, A.; Ferro Desideri, L.; Nucci, P.; Serafino, M.; Giannaccare, G.; Lembo, A.; Traverso, C.E. Congenital Nasolacrimal Duct Obstruction (CNLDO): A Review. Diseases 2018, 6, 96. [Google Scholar] [CrossRef]
- Petris, C.; Liu, D. Probing for congenital nasolacrimal duct obstruction. Cochrane Database Syst. Rev. 2017, 7, CD011109. [Google Scholar] [CrossRef]
- Habre, W.; Disma, N.; Virag, K.; Becke, K.; Hansen, T.G.; Johr, M.; Leva, B.; Morton, N.S.; Vermeulen, P.M.; Zielinska, M.; et al. Incidence of severe critical events in paediatric anaesthesia (APRICOT): A prospective multicentre observational study in 261 hospitals in Europe. Lancet Respir. Med. 2017, 5, 412–425. [Google Scholar] [CrossRef]
- Mellin-Olsen, J.; Staender, S.; Whitaker, D.K.; Smith, A.F. The Helsinki Declaration on Patient Safety in Anaesthesiology. Eur. J. Anaesthesiol. 2010, 27, 592–597. [Google Scholar] [CrossRef]
- Smith, I.; Kranke, P.; Murat, I.; Smith, A.; O’Sullivan, G.; Soreide, E.; Spies, C.; in’t Veld, B.; European Society of Anaesthesiology. Perioperative fasting in adults and children: Guidelines from the European Society of Anaesthesiology. Eur. J. Anaesthesiol. 2011, 28, 556–569. [Google Scholar] [CrossRef]
- Frykholm, P.; Disma, N.; Andersson, H.; Beck, C.; Bouvet, L.; Cercueil, E.; Elliott, E.; Hofmann, J.; Isserman, R.; Klaucane, A.; et al. Pre-operative fasting in children: A guideline from the European Society of Anaesthesiology and Intensive Care. Eur. J. Anaesthesiol. 2022, 39, 4–25. [Google Scholar] [CrossRef]
- Boehringer, L.A.; Bennie, R.E. Laryngeal mask airway and the pediatric patient. Int. Anesthesiol. Clin. 1998, 36, 45–60. [Google Scholar] [CrossRef]
- Wilson, I.G. The laryngeal mask airway in paediatric practice. Br. J. Anaesth. 1993, 70, 124–125. [Google Scholar] [CrossRef] [PubMed]
- Sun, X.L.; Li, J.; Wang, Z.Y.; Li, M.Y.; Duan, W.; Wu, N.; Yang, O. Reinforced Laryngeal Mask in Pediatric Laparoscopic Surgery. J. Coll. Physicians Surg. Pak. 2019, 29, 915–918. [Google Scholar] [CrossRef] [PubMed]
- Von Ungern-Sternberg, B.S.; Boda, K.; Schwab, C.; Sims, C.; Johnson, C.; Habre, W. Laryngeal mask airway is associated with an increased incidence of adverse respiratory events in children with recent upper respiratory tract infections. Anesthesiology 2007, 107, 714–719. [Google Scholar] [CrossRef] [PubMed]
- De Carvalho, A.L.R.; Vital, R.B.; de Lira, C.C.S.; Magro, I.B.; Sato, P.T.S.; Lima, L.H.N.; Braz, L.G.; Modolo, N.S.P. Laryngeal Mask Airway Versus Other Airway Devices for Anesthesia in Children with an Upper Respiratory Tract Infection: A Systematic Review and Meta-analysis of Respiratory Complications. Anesth. Analg. 2018, 127, 941–950. [Google Scholar] [CrossRef] [PubMed]
- Nevescanin, A.; Vickov, J.; Elezovic Baloevic, S.; Pogorelic, Z. Laryngeal Mask Airway Versus Tracheal Intubation for Laparoscopic Hernia Repair in Children: Analysis of Respiratory Complications. J. Laparoendosc. Adv. Surg. Tech. A 2020, 30, 76–80. [Google Scholar] [CrossRef]
- Keller, C.; Brimacombe, J.; Bittersohl, J.; Lirk, P.; von Goedecke, A. Aspiration and the laryngeal mask airway: Three cases and a review of the literature. Br. J. Anaesth. 2004, 93, 579–582. [Google Scholar] [CrossRef] [PubMed]
- Dumas, G.A.; Bryant, A.S.; Ibey, J.; Long, J.A.; Vicinanzo, M.G.; Boyd, G.L. Safety Comparison of Laryngeal Mask Use with Endotracheal Intubation in Patients Undergoing Dacryocystorhinostomy Surgery. Ophthalmic Plast. Reconstr. Surg. 2018, 34, 324–328. [Google Scholar] [CrossRef] [PubMed]
- Van Esch, B.F.; Stegeman, I.; Smit, A.L. Comparison of laryngeal mask airway vs tracheal intubation: A systematic review on airway complications. J. Clin. Anesth. 2017, 36, 142–150. [Google Scholar] [CrossRef]
- Khunl-Brady, K.S. Intubation of children with or without relaxants? Anaesthesist 2011, 60, 1063, author reply 1063–1064. [Google Scholar] [CrossRef]
- Tulgar, S.; Boga, I.; Cakiroglu, B.; Thomas, D.T. Short-lasting pediatric laparoscopic surgery: Are muscle relaxants necessary? Endotracheal intubation vs. laryngeal mask airway. J. Pediatr. Surg. 2017, 52, 1705–1710. [Google Scholar] [CrossRef]
- Byun, S.H.; Kim, S.J.; Kim, E. Comparison of the clinical performance of the flexible laryngeal mask airway in pediatric patients under general anesthesia with or without a muscle relaxant: Study protocol for a randomized controlled trial. Trials 2019, 20, 31. [Google Scholar] [CrossRef]
| Cohort ET | Cohort LMA | p-Value | |
|---|---|---|---|
| n (%) | 36 (42.9) | 48 (57.1) | |
| Age, months, mean ± SD (range) | 25.2 ± 13.4 (4–57) | 23.3 ± 12.5 (5–56) | 0.49 |
| 1–11 | 8.5 ± 3.2 (4–11) | 8.8 ± 1.9 (5–11) | |
| 12–23 | 17.3 ± 2.9 (13–22) | 17.4 ± 3.6 (12–23) | |
| 24–35 | 29.8 ± 3.3 (24–35) | 27.5 ± 2.5 (24–33) | |
| 36–47 | 41.0 ± 3.9 (36–45) | 41.3 ± 4.2 (37–47) | |
| 48–59 | 55.0 ± 2.6 (52–57) | 54.3 ± 1.5 (53–56) | |
| Female gender, n (%) | 16 (44.4) | 22 (45.8) | 0.90 |
| Body weight, kg, mean ± SD (range) | 12.4 ± 2.6 (6–19) | 12.3 ± 2.6 (8–19) | 0.62 |
| 1–11 | 9.8 ± 3.1 (6–13) | 9.2 ± 1.4 (8–12) | |
| 12–23 | 11.5 ± 1.7 (8–15) | 11.4 ± 1.5 (10–15) | |
| 24–35 | 12.8 ± 1.5 (10–16) | 13.6 ± 1.7 (11–17) | |
| 36–47 | 14.9 ± 2.3 (13–18) | 15.2 ± 2.6 (14–19) | |
| 48–59 | 16.7 ± 2.1 (15–19) | 16.3 ± 1.5 (15–18) | |
| Body size, cm, mean ± SD (range) | 88.3 ± 9.1 (73–115) | 88.5 ± 10.2 (68–110) | 0.78 |
| 1–11 | 81 ± 8.5 (73–90) | 74.7 ± 4.7 (68–80) | |
| 12–23 | 82.5 ± 4.6 (73–90) | 83.0 ± 5.1 (70–92) | |
| 24–35 | 90.9 ± 4.6 (85–100) | 93.5 ± 5.1 (84–100) | |
| 36–47 | 99.0 ± 6.2 (91–106) | 100.0 ± 3.8 (97–105) | |
| 48–59 | 102.3 ± 11.2 (94–115) | 107.7 ± 3.2 (104–110) | |
| ASA PS, n (%) | 0.23 | ||
| ASA PS I | 31 (86.1) | 46 (95.8) | |
| ASA PS II | 4 (11.1) | 2 (4.2) | |
| ASA PS III | 1 (2.8) | 0 (0) |
| Cohort ET | Cohort LMA | p-Value | |
|---|---|---|---|
| Intravenous induction, n (%) | 17 (47.2) | 19 (39,6) | 0.51 |
| Inhalational induction, n (%) | 19 (52,8) | 29 (60.4) | |
| Volatile anesthetics used for maintenance, n (%) | 34 (94.4) | 47 (97.9) | 0.57 |
| Opioid used, n (%) | 0.03 | ||
| Remifentanil, n (%) | 36 (100.0) | 40 (83.3) | |
| Sufentanil, n (%) | 0 (0.0) | 5 (10.4) | |
| Fentanyl, n (%) | 0 (0.0) | 3 (6.3) | |
| Muscle Relaxants, n (%) | 5 (13.9) | 0 (0.0) | 0.01 |
| Cohort ET | Cohort LMA | p-Value | |
|---|---|---|---|
| Postoperative pain treatment, n (%) | 33 (91.7) | 44 (91.7) | 1.00 |
| Ibuprofen/Paracetamol, n (%) | 33 (91.7) | 41 (85.4) | 0.38 |
| Parenteral opioid analgesics, n (%) | 8 (22.2) | 22 (45.8) | 0.03 |
| Cohort ET | Cohort LMA | p-Value | |
|---|---|---|---|
| FiO2 intraoperative lowest (mean ± SD (range)) | 0.47 ± 0.11 (0.30–0.70) | 0.39 ± 0.11 (0.27–0.70) | <0.001 |
| Cohort ET | Cohort LMA | p-Value | |
|---|---|---|---|
| SpO2 Air (mean ± SD (range)) | 99.4 ± 1.1 (96–100) | 99.4 ± 0.94 (96–100) | 0.74 |
| SpO2 intraoperative lowest (mean ± SD (range)) | 99.7 ± 1.2 (93–100) | 99.8 ± 0.50 (98–100) | 0.77 |
| SpO2 postoperative first (mean ± SD (range)) | 97.5 ± 2.9 (85–100) | 97.2 ± 2.0 (93–100) | 0.21 |
| SpO2 recovery room lowest (mean ± SD (range)) | 97.0 ± 2.0 (91–100) | 97.0 ± 1.9 (90–100) | 0.91 |
| SpO2 recovery room discharge (mean ± SD (range)) | 98.3 ± 1.8 (91–100) | 98.3 ± 1.5 (93–100) | 0.51 |
| Cohort ET | Cohort LMA | p-Value | |
|---|---|---|---|
| Induction (mean ± SD (range)) | 14 ± 6 (4–30) | 10 ± 5 (3–26) | 0.006 |
| Recovery/Emergence (mean ± SD (range)) | 14 ± 8 (0–37) | 9 ± 6 (0–25) | 0.03 |
| Discharge recovery room (mean ± SD (range)) | 51 ± 17 (16–100) | 74 ± 33 (16–150) | 0.001 |
| No | Time | Cohort | Adverse Event | Management |
|---|---|---|---|---|
| 1 | postoperative | ET | residual neuromuscular block (TOF: 3/4) | reversal using acetylcholinesterase inhibitor |
| 2 | recovery room | ET | bronchial obstruction, respiratory distress | beta adrenergic drug application |
| 3 | postoperative | ET | laryngospasm after endotracheal tube removal | temporary desaturation, endotracheal re-intubation, prolonged wake-up |
| 4 | postoperative | ET | bronchial obstruction | beta adrenergic drug application, repeated propofol administration, ET removal and LMA insertion, prolonged wake-up |
| 5 | intraoperative | ET | airway loss, tube dislocation | temporary desaturation, endotracheal re-intubation |
| 6 | recovery room | LMA | emergence agitation | propofol administration in recovery room |
| 7 | recovery room | LMA | emergence agitation | propofol administration in recovery room |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leister, N.; Heindl, L.M.; Rokohl, A.C.; Böttiger, B.W.; Menzel, C.; Ulrichs, C.; Schick, V.C. Laryngeal Mask Airway Versus Endotracheal Intubation during Lacrimal Duct Stenosis Surgery in Children—A Retrospective Analysis. Children 2024, 11, 320. https://doi.org/10.3390/children11030320
Leister N, Heindl LM, Rokohl AC, Böttiger BW, Menzel C, Ulrichs C, Schick VC. Laryngeal Mask Airway Versus Endotracheal Intubation during Lacrimal Duct Stenosis Surgery in Children—A Retrospective Analysis. Children. 2024; 11(3):320. https://doi.org/10.3390/children11030320
Chicago/Turabian StyleLeister, Nicolas, Ludwig M. Heindl, Alexander C. Rokohl, Bernd W. Böttiger, Christoph Menzel, Christoph Ulrichs, and Volker C. Schick. 2024. "Laryngeal Mask Airway Versus Endotracheal Intubation during Lacrimal Duct Stenosis Surgery in Children—A Retrospective Analysis" Children 11, no. 3: 320. https://doi.org/10.3390/children11030320
APA StyleLeister, N., Heindl, L. M., Rokohl, A. C., Böttiger, B. W., Menzel, C., Ulrichs, C., & Schick, V. C. (2024). Laryngeal Mask Airway Versus Endotracheal Intubation during Lacrimal Duct Stenosis Surgery in Children—A Retrospective Analysis. Children, 11(3), 320. https://doi.org/10.3390/children11030320