Family Needs Assessment of Patients with Cerebral Palsy Attending Two Hospitals in Accra, Ghana
Highlights
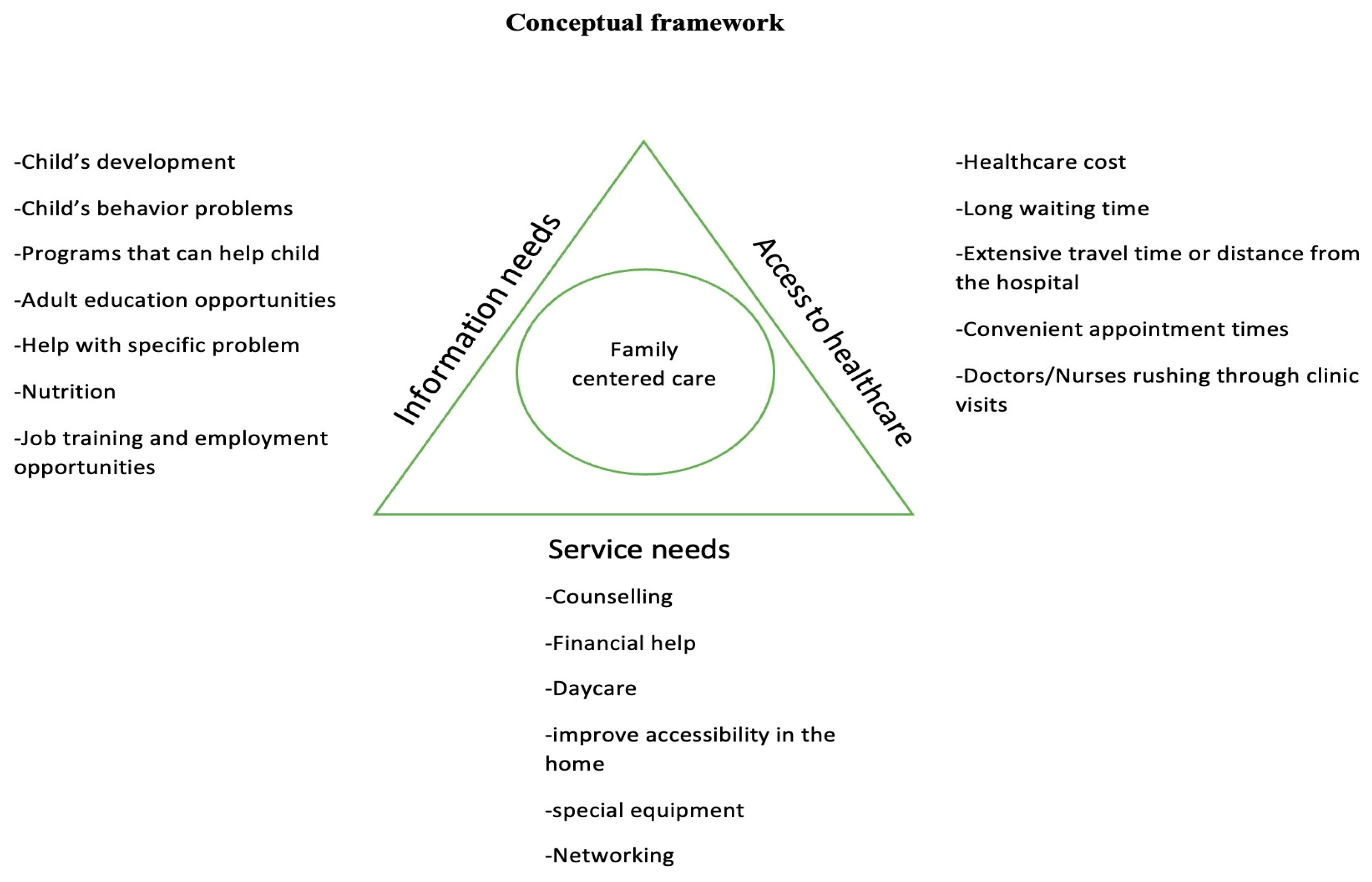
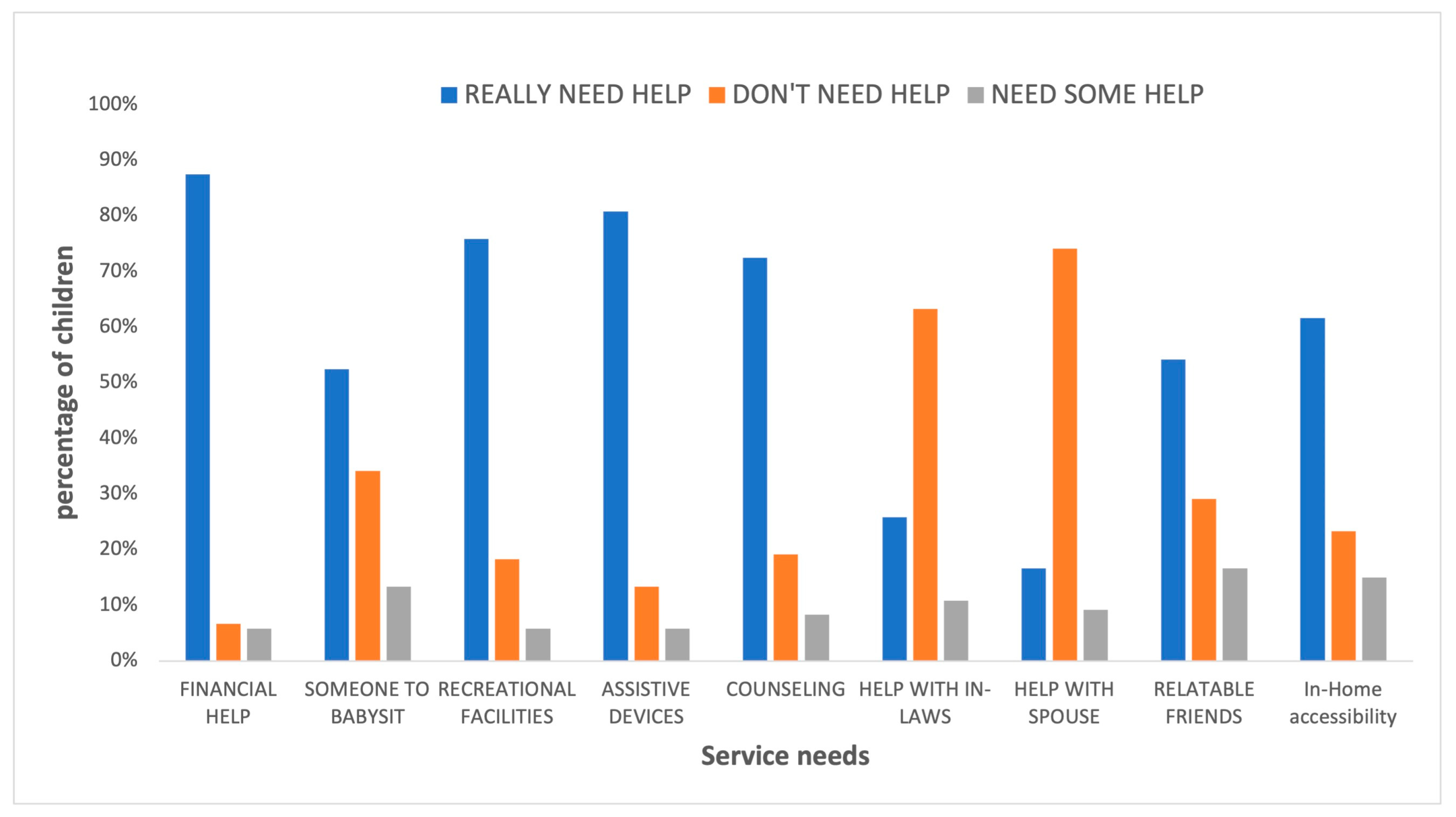
- The primary service needs identified were financial assistance, respite care, recreational facilities, in-home accessibility improvements, and assistive devices.
- Among the parents of children with cerebral palsy, three out of four were married, and caregivers—primarily mothers—generally did not require help in dealing with their spouses or in-laws.
- The key information needs included guidance on child development, behavioral issues, nutrition and feeding, and available programs to support the child. Caregivers showed a greater interest in job training and opportunities for themselves compared to adult educational resources.
- Most families were categorized as extremely poor, with one parent, usually the mother, staying home to care for the child. Despite this, 97% of these families did not receive any social welfare support; however, 96% of the children were covered by the national health insurance.
- Families of children with cerebral palsy require comprehensive support, including social security, special schools (which will also give caregivers respite), recreational facilities like gardens and playgrounds, home modifications, and assistance with acquiring assistive devices.
- It is encouraging that three out of four parents were married and demonstrated family cohesion. However, the study primarily included families from urban areas with access to neurodevelopmental clinics. Further research is needed to explore the needs of families in communities without such healthcare facilities.
- Education programs on cerebral palsy should be developed and implemented in both community settings and healthcare facilities. Healthcare professionals need enhanced training and resources to effectively educate families on managing cerebral palsy and to provide information on supportive programs, such as job opportunities for caregivers.
- Additionally, families should be informed about available social welfare and government support systems and be actively assisted in enrolling in these programs.
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Site
2.3. Study Population
2.4. Inclusion and Exclusion Criteria
2.5. Sampling Method and Sample Size Determination
2.6. Data Collection Techniques
2.7. Data Collection Tools
2.7.1. The Questionnaire
2.7.2. Family Needs Assessment Tool
2.7.3. The Gross Motor Function Classification System—Expanded & Revised (GMFCS-E&R)
2.8. Data Handling and Analysis
2.9. Ethical Consideration
3. Results
3.1. Sociodemographic Characteristics
3.2. Service Needs
3.3. Information Needs
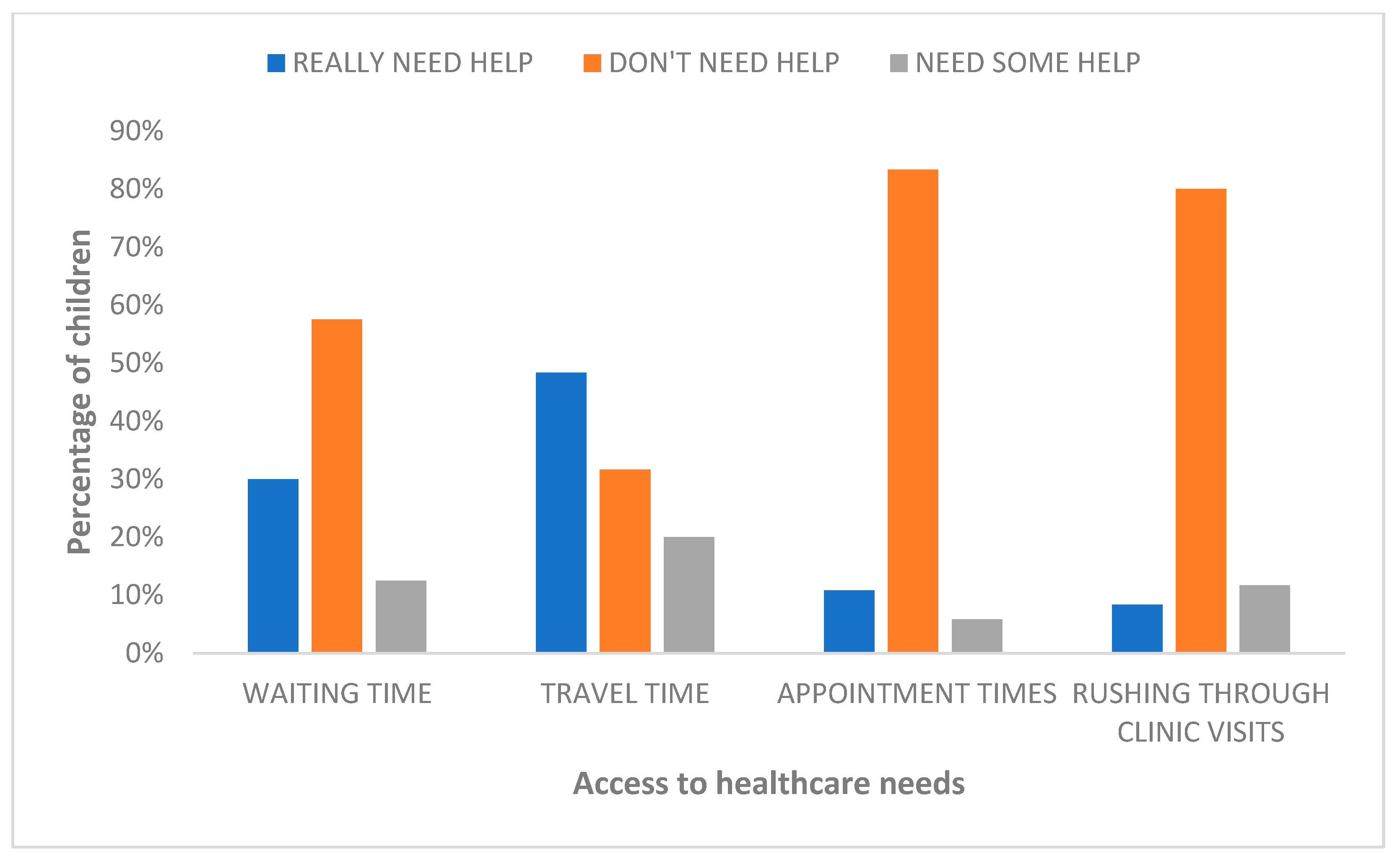
3.4. Access to Healthcare Needs
3.5. Correlation between GMFCS and Family Needs
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Krigger, K.W. Cerebral Palsy: An Overview. Am. Fam. Physician 2006, 73, 91–100. [Google Scholar]
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child. Neurol. 2007, 49, 8–14. Available online: https://onlinelibrary.wiley.com/doi/10.1111/j.1469-8749.2007.tb12610.x (accessed on 4 March 2023).
- Donald, K.A.; Kakooza, A.M.; Wammanda, R.D.; Mallewa, M.; Samia, P.; Babakir, H.; Bearden, D.; Majnemer, A.; Fehlings, D.; Shevell, M.; et al. Pediatric Cerebral Palsy in Africa: Where Are We? J. Child. Neurol. 2015, 30, 963–971. [Google Scholar] [CrossRef] [PubMed]
- Lagunju, I.A.; Fatunde, O.J. Epilepsy in Nigerian children with cerebral palsy. Dev. Med. Child. Neurol. 2007, 49, 158–159. [Google Scholar]
- Njambi, L.; Kariuki, M.; Masinde, S. Ocular findings in children attending occupational therapy clinic at Kenyatta National Hospital, Nairobi, Kenya. J. Ophthalmol. East. Cent. South. Afr. 2020, 15, 21–26. Available online: https://joecsa.coecsa.org/index.php/joecsa/article/view/158 (accessed on 7 July 2023).
- Gladstone, M. A review of the incidence and prevalence, types and aetiology of childhood cerebral palsy in resource-poor settings. Ann. Trop. Paediatr. 2010, 30, 181–196. Available online: https://www.google.com/search?q=Gladstone%2C+M.+(2010).+A+review+of+the+incidence+and+prevalence%2C+types+and+aetiology+of+childhood+cerebral+palsy+in+resource-poor+settings.+Annals+of+Tropical+Paediatrics%2C+30(3)%2C+181%E2%80%93196.+https%3A%2F%2Fdoi.org%2F10.1179%2F146532810X12786388978481&oq=Gladstone%2C+M.+(2010).+A+review+of+the+incidence+and+prevalence%2C+types+and+aetiology+of+childhood+cerebral+palsy+in+resource-poor+settings.+Annals+of+Tropical+Paediatrics%2C+30(3)%2C+181%E2%80%93196.+https%3A%2F%2Fdoi.org%2F10.1179%2F146532810X12786388978481&aqs=chrome..69i57.222j0j9&sourceid=chrome&ie=UTF-8 (accessed on 26 May 2023). [CrossRef]
- Abdel Malek, S.; Rosenbaum, P.; Gorter, J.W. Perspectives on cerebral palsy in Africa: Exploring the literature through the lens of the International Classification of Functioning, Disability and Health. Child Care Health Dev. 2020, 46, 175–186. [Google Scholar] [CrossRef]
- Hirtz, D.; Thurman, D.J.; Gwinn-Hardy, K.; Mohamed, M.; Chaudhuri, A.R.; Zalutsky, R. How common are the “common” neurologic disorders? Neurology 2007, 68, 326–337. Available online: https://n.neurology.org/content/68/5/326 (accessed on 26 May 2023). [CrossRef]
- Kyeremateng, J.D.A.; Edusei, A.; Dogbe, J.A.; Opoku, M.P.; Nketsia, W.; Hammond, C.; Afriyie, S.A. Experiences of primary caregivers of children with cerebral palsy across the trajectory of diagnoses in Ghana. Afr. J. Disabil. 2019, 8, 577. [Google Scholar] [CrossRef]
- Oskoui, M. Growing up with cerebral palsy: Contemporary challenges of healthcare transition. Can. J. Neurol. Sci. J. Can. Sci. Neurol. 2012, 39, 23–25. [Google Scholar] [CrossRef]
- Novak, I.; McIntyre, S.; Morgan, C.; Campbell, L.; Dark, L.; Morton, N.; Stumbles, E.; Wilson, S.A.; Goldsmith, S. A systematic review of interventions for children with cerebral palsy: State of the evidence. Dev. Med. Child. Neurol. 2013, 55, 885–910. [Google Scholar] [CrossRef]
- Almasri, N.; Palisano, R.; Dunst, C.; Chiarello, L.; O’Neil, M.; Polansky, M. Determinants of Needs of Families of Children and Youth with Cerebral Palsy. Child. Health Care 2011, 40, 130–154. [Google Scholar] [CrossRef]
- Bailey, D.B.; Blasco, P.M.; Simeonsson, R.J. Needs expressed by mothers and fathers of young children with disabilities. Am. J. Ment. Retard. 1992, 97, 1–10. [Google Scholar]
- King, G.; Cathers, T.; King, S.; Rosenbaum, P. Major Elements of Parents’ Satisfaction and Dissatisfaction with Pediatric Rehabilitation Services. Child. Health Care 2001, 30, 111–134. [Google Scholar] [CrossRef]
- Rosenbaum, P.; King, S.; Law, M.; King, G.; Evans, J. Family-Centred Service. Phys. Occup. Ther. Pediatr. 1998, 18, 1–20. [Google Scholar] [CrossRef]
- Brehaut, J.C.; Kohen, D.E.; Raina, P.; Walter, S.D.; Russell, D.J.; Swinton, M.; O’Donnell, M.; Rosenbaum, P. The health of primary caregivers of children with cerebral palsy: How does it compare with that of other Canadian caregivers? Pediatrics 2004, 114, e182–e191. [Google Scholar] [CrossRef]
- Brehaut, J.C.; Kohen, D.E.; Garner, R.E.; Miller, A.R.; Lach, L.M.; Klassen, A.F.; Rosenbaum, P.L. Health Among Caregivers of Children with Health Problems: Findings from a Canadian Population-Based Study. Am. J. Public Health 2009, 99, 1254–1262. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2696656/ (accessed on 7 July 2023). [CrossRef] [PubMed]
- Brehaut, J.C.; Garner, R.E.; Miller, A.R.; Lach, L.M.; Klassen, A.F.; Rosenbaum, P.L.; Kohen, D.E. Changes Over Time in the Health of Caregivers of Children with Health Problems: Growth-Curve Findings from a 10-Year Canadian Population-Based Study. Am. J. Public Health 2011, 101, 2308–2316. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3222435/ (accessed on 7 July 2023). [CrossRef]
- Lach, L.M.; Kohen, D.E.; Garner, R.E.; Brehaut, J.C.; Miller, A.R.; Klassen, A.F.; Rosenbaum, P.L. The health and psychosocial functioning of caregivers of children with neurodevelopmental disorders. Disabil. Rehabil. 2009, 31, 607–618. [Google Scholar] [CrossRef]
- Raina, P.; O’Donnell, M.; Schwellnus, H.; Rosenbaum, P.; King, G.; Brehaut, J.; Russell, D.; Swinton, M.; King, S.; Wong, M.; et al. Caregiving process and caregiver burden: Conceptual models to guide research and practice. BMC Pediatr. 2004, 4, 1. [Google Scholar] [CrossRef]
- Darrah, J.; Wiart, L.; Magill-Evans, J.; Ray, L.; Andersen, J. Are family-centred principles, functional goal setting and transition planning evident in therapy services for children with cerebral palsy? Child Care Health Dev. 2012, 38, 41–47. [Google Scholar] [CrossRef] [PubMed]
- King, S.; Teplicky, R.; King, G.; Rosenbaum, P. Family-centered service for children with cerebral palsy and their families: A review of the literature. Semin. Pediatr. Neurol. 2004, 11, 78–86. [Google Scholar] [CrossRef]
- MacKean, G.L.; Thurston, W.E.; Scott, C.M. Bridging the divide between families and health professionals’ perspectives on family-centred care. Health Expect. 2005, 8, 74–85. [Google Scholar] [CrossRef] [PubMed]
- Moore, M.H.; Mah, J.K.; Trute, B. Family-centred care and health-related quality of life of patients in paediatric neurosciences. Child Care Health Dev. 2009, 35, 454–461. [Google Scholar] [CrossRef]
- Turnbull, A.P.; Turbiville, V.; Turnbull, H.R. Evolution of family–professional partnerships: Collective empowerment as the model for the early twenty-first century. In Handbook of Early Childhood Intervention, 2nd ed.; Cambridge University Press: New York, NY, USA, 2000; pp. 630–650. [Google Scholar]
- Jeglinsky, I.; Autti-Rämö, I.; Brogren Carlberg, E. Two sides of the mirror: Parents’ and service providers’ view on the family-centredness of care for children with cerebral palsy. Child Care Health Dev. 2012, 38, 79–86. [Google Scholar] [CrossRef]
- Nijhuis, B.J.G.; Reinders-Messelink, H.A.; de Blécourt, A.C.E.; Olijve, W.G.; Haga, N.; Groothoff, J.W.; Nakken, H.; Postema, K. Towards integrated paediatric services in the Netherlands: A survey of views and policies on collaboration in the care for children with cerebral palsy. Child Care Health Dev. 2007, 33, 593–603. [Google Scholar] [CrossRef] [PubMed]
- Bamm, E.L.; Rosenbaum, P. Family-centered theory: Origins, development, barriers, and supports to implementation in rehabilitation medicine. Arch. Phys. Med. Rehabil. 2008, 89, 1618–1624. [Google Scholar] [CrossRef]
- Foster, M.; Whitehead, L.; Maybee, P. Parents’ and health professionals’ perceptions of family centred care for children in hospital, in developed and developing countries: A review of the literature. Int. J. Nurs. Stud. 2010, 47, 1184–1193. [Google Scholar] [CrossRef]
- Israel, G.D. Determining Sample Size. 1992. Available online: https://www.psycholosphere.com/Determining%20sample%20size%20by%20Glen%20Israel.pdf (accessed on 6 July 2023).
- Polack, S.; Adams, M.; O’banion, D.; Baltussen, M.; Asante, S.; Kerac, M.; Gladstone, M.; Zuurmond, M. Children with cerebral palsy in Ghana: Malnutrition, feeding challenges, and caregiver quality of life. Dev. Med. Child. Neurol. 2018, 60, 914–921. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1111/dmcn.13797 (accessed on 4 March 2023). [CrossRef]
- Zuurmond, M.; O’Banion, D.; Gladstone, M.; Carsamar, S.; Kerac, M.; Baltussen, M.; Tann, C.; Nyante, G.; Polack, S. Evaluating the impact of a community-based parent training programme for children with cerebral palsy in Ghana. PLoS ONE 2018, 13, e0202096. [Google Scholar] [CrossRef]
- Umemura, T.; Jacobvitz, D.; Messina, S.; Hazen, N. Do toddlers prefer the primary caregiver or the parent with whom they feel more secure? The role of toddler emotion. Infant. Behav. Dev. 2013, 36, 102–114. [Google Scholar] [CrossRef] [PubMed]
- USLEGAL. Primary Caretaker Law and Legal Definition|USLegal, Inc. 2023. Available online: https://definitions.uslegal.com/p/primary-caretaker/ (accessed on 22 May 2023).
- Calfee, C.; Wittwer, F.; Meredith, M. Building A Full-Service School: A Step-by-Step Guide|Wiley. 1998. Available online: https://www.wiley.com/en-us/Building+A+Full+Service+School%3A+A+Step+by+Step+Guide+-p-9780787940584 (accessed on 22 May 2023).
- Palisano, R.J.; Almarsi, N.; Chiarello, L.A.; Orlin, M.N.; Bagley, A.; Maggs, J. Family needs of parents of children and youth with cerebral palsy. Child Care Health Dev. 2010, 36, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, P.L.; Palisano, R.J.; Bartlett, D.J.; Galuppi, B.E.; Russell, D.J. Development of the Gross Motor Function Classification System for cerebral palsy. Dev. Med. Child. Neurol. 2008, 50, 249–253. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1469-8749.2008.02045.x (accessed on 1 May 2023). [CrossRef]
- Fonzi, V.; Sheriff, B.; Dalglish, S.; Anum, A.; Agyei, E.D.; Diggs, D.; Eboigbe, L.; Owusu, P.G.; Sakyi, K.S. The multifaceted care-seeking practices among caregivers of children with cerebral palsy: Perspectives from mothers and providers in Ghana. PLoS ONE 2021, 16, e0258650. Available online: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0258650 (accessed on 4 March 2023). [CrossRef]
- Chounti, A.; Hägglund, G.; Wagner, P.; Westbom, L. Sex differences in cerebral palsy incidence and functional ability: A total population study. Acta Paediatr. 2013, 102, 712–717. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1111/apa.12240 (accessed on 3 May 2023). [CrossRef]
- Ghana Statistical Service. Ghana Statistical Services. 2023. Available online: https://statsghana.gov.gh/ghfactsheet.php (accessed on 20 April 2023).
- Boychuck, Z. Creating the Content for Knowledge Translation Tools to Prompt Early Referral for Diagnostic Assessment and Rehabilitation Services for Children with Suspected Cerebral Palsy. McGill University. 2020. Available online: https://escholarship.mcgill.ca/concern/theses/p8418s53z (accessed on 20 April 2023).
- Nordin, M.N.A.; Shan, H.E.; Zanudin, A. The Unmet Needs of Parents of Highly Dependent Children with Cerebral Palsy. Int. J. Environ. Res. Public Health 2019, 16, 5145. Available online: https://www.mdpi.com/1660-4601/16/24/5145 (accessed on 18 April 2023). [CrossRef] [PubMed]
- Buran, C.F.; Sawin, K.; Grayson, P.; Criss, S. Family needs assessment in cerebral palsy clinic. J. Spec. Pediatr. Nurs. 2009, 14, 86–93. Available online: https://pubmed.ncbi.nlm.nih.gov/19356202/ (accessed on 18 April 2023). [CrossRef]
- Saygi, E.K.; Giray, E.; Peynirci Cersit, H.; Ulutatar, F.; Aydin, R. Assessment of Family Environment and Needs of Families Who Have Children with Cerebral Palsy. Türkiye Fiz Tip Ve Rehabil. Derg 2015, 61, 320–325. Available online: http://www.ftrdergisi.com/eng/makale/3883/295/Full-Text (accessed on 7 July 2023).
- Whittingham, K.; Wee, D.; Sanders, M.; Boyd, R. Sorrow, coping and resiliency: Parents of children with cerebral palsy share their experiences. Disabil. Rehabil. 2012, 20, 35. [Google Scholar] [CrossRef]
- Garip, Y.; Ozel, S.; Tuncer, O.B.; Kilinc, G.; Seckin, F.; Arasil, T. Fatigue in the mothers of children with cerebral palsy. Disabil. Rehabil. 2017, 39, 757–762. [Google Scholar] [CrossRef]
- Umar, A.B.; Yakasai, A.M.; Danazumi, M.S.; Shehu, U.T.; Badaru, U.M.; Kaka, B. Assessment of family needs of children with cerebral palsy in Northern-Nigeria: A cross-sectional study. J. Pediatr. Rehabil. Med. 2021, 14, 265–274. [Google Scholar] [CrossRef]
- Zuurmond, M.; Nyante, G.; Baltussen, M.; Seeley, J.; Abanga, J.; Shakespeare, T.; Collumbien, M.; Bernays, S. A support programme for caregivers of children with disabilities in Ghana: Understanding the impact on the wellbeing of caregivers. Child Care Health Dev. 2019, 45, 45–53. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1111/cch.12618 (accessed on 12 April 2023). [CrossRef]
- Hirose, T.; Ueda, R. Long-term follow-up study of cerebral palsy children and coping behaviour of parents. J. Adv. Nurs. 1990, 15, 762–770. [Google Scholar] [CrossRef] [PubMed]
- Weiss, K.; Marvin, R.; Pianta, R. Ethnographic detection and description of family strategies for child care: Applications to the study of cerebral palsy. J. Pediatr. Psychol. 1997, 22, 263–278. Available online: https://www.bibsonomy.org/bibtex/0a4db6a5d3b2b0bc9637018f85a6175a (accessed on 15 March 2023). [PubMed]
- Glenn, S.; Cunningham, C.; Poole, H.; Reeves, D.; Weindling, M. Maternal parenting stress and its correlates in families with a young child with cerebral palsy. Child Care Health Dev. 2009, 35, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Dogbe, J.A.; Kyeremateng, J.D.A.; Opoku, M.P.; Nketsia, W.; Hammond, C. ‘There is family tension, but they understand…’: Familial and sibling relationships following the diagnosis of cerebral palsy in children in Ghana. Int. J. Dev. Disabil. 2022, 68, 35–46. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8843311/ (accessed on 15 March 2023). [CrossRef]
- Pun, S.H.; Ma, J.L.C.; Lai, K.C.C. In search of perfect motherhood for imperfect childhood—Experiences of 22 Chinese mothers. Child Fam. Soc. Work 2004, 9, 285–293. Available online: https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1365-2206.2004.00311.x (accessed on 15 March 2023). [CrossRef]
- The World Bank. Fact Sheet: An Adjustment to Global Poverty Lines World Bank. 2023. Available online: https://www.worldbank.org/en/news/factsheet/2022/05/02/fact-sheet-an-adjustment-to-global-poverty-lines (accessed on 18 March 2023).
- Lukemeyer, A.; Meyers, M.K.; Smeeding, T.M. Expensive Children in Poor Families: Out-of-Pocket Expenditures for the Care of Disabled and Chronically Ill Children and Welfare Reform; Center for Policy Research, Syracuse University: Syracuse, NY, USA, 1997. [Google Scholar]
- Nuri, R.P.; Aldersey, H.M.; Ghahari, S. Needs of families of children with cerebral palsy in Bangladesh: A qualitative study. Child Care Health Dev. 2019, 45, 36–44. [Google Scholar] [CrossRef]
- Tseng, M.H.; Chen, K.L.; Shieh, J.Y.; Lu, L.; Huang, C.Y.; Simeonsson, R.J. Child characteristics, caregiver characteristics, and environmental factors affecting the quality of life of caregivers of children with cerebral palsy. Disabil. Rehabil. 2016, 38, 2374–2382. [Google Scholar] [CrossRef]
- Tette, E.M.A.; Sifah, E.K.; Nartey, E.T.; Nuro-Ameyaw, P.; Tete-Donkor, P.; Biritwum, R.B. Maternal profiles and social determinants of malnutrition and the MDGs: What have we learnt? BMC Public Health 2016, 16, 214. [Google Scholar] [CrossRef]
- Agyemang-Duah, W.; Peprah, C.; Peprah, P. “Let’s talk about money”: How do poor older people finance their healthcare in rural Ghana? A qualitative study. Int. J. Equity Health 2019, 18, 47. Available online: https://equityhealthj.biomedcentral.com/articles/10.1186/s12939-019-0927-0 (accessed on 20 April 2023). [CrossRef]
- Wiredu, D.N.A.; Peprah, C.; Agyemang-Duah, W. Prevalence of health insurance enrolment and associated factors among persons with disabilities in Ghana. Cogent Med. 2021, 8, 1901379. [Google Scholar] [CrossRef]
- Rawlins, P.S.; Rawlins, T.D.; Homer, M. Development of the family needs assessment tool. West. J. Nurs. Res. 1990, 12, 201–214. [Google Scholar] [CrossRef] [PubMed]
- Fawcett, T.N.; Baggaley, S.E.; Wu, C.; Whyte, D.A.; Martinson, I.M. Parental responses to health care services for children with chronic conditions and their families: A comparison between Hong Kong and Scotland. J. Child. Health Care Prof. Work Child. Hosp. Community 2005, 9, 8–19. [Google Scholar] [CrossRef] [PubMed]
- Denboba, D.; McPherson, M.G.; Kenney, M.K.; Strickland, B.; Newacheck, P.W. Achieving family and provider partnerships for children with special health care needs. Pediatrics 2006, 118, 1607–1615. [Google Scholar] [CrossRef] [PubMed]
- Farmer, J.E.; Clark, M.J.; Sherman, A.; Marien, W.E.; Selva, T.J. Comprehensive primary care for children with special health care needs in rural areas. Pediatrics 2005, 116, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Wilmshurst, J.M.; Badoe, E.; Wammanda, R.D.; Mallewa, M.; Kakooza-Mwesige, A.; Venter, A.; Newton, C.R. Child neurology services in Africa. J. Child. Neurol. 2011, 26, 1555–1563. [Google Scholar] [CrossRef]
- Paul, S.; Nahar, A.; Bhagawati, M.; Kunwar, A.J. A Review on Recent Advances of Cerebral Palsy. Oxid. Med. Cell. Longev. 2022, 2022, 2622310. [Google Scholar] [CrossRef]

| Characteristics of Participants | Number (n) | Percentage (%) |
|---|---|---|
| Characteristics of the Children | ||
| Gender | ||
| Male | 76 | 63 |
| Female | 44 | 37 |
| Age (months) | ||
| 12 | 12 | 10 |
| 13–24 | 36 | 30 |
| 25–60 | 49 | 41 |
| 61–132 | 20 | 17 |
| 133–204 | 3 | 2 |
| Age Seen at Clinic (months) | ||
| 0–12 | 64 | 53 |
| 13–24 | 28 | 23 |
| 25–60 | 19 | 16 |
| 61–132 | 7 | 6 |
| 133–204 | 2 | 2 |
| GMFCS | ||
| I | 18 | 15 |
| II | 16 | 13 |
| III | 14 | 12 |
| IV | 36 | 30 |
| V | 36 | 30 |
| Insurance | ||
| NHIS * | 115 | 96 |
| Private Health Insurance | 4 | 3 |
| Expired NHIS | 1 | 1 |
| Social Welfare Assistance | ||
| Yes | 3 | 3 |
| No | 117 | 97 |
| Characteristics of Caregivers | ||
| Marital Status | ||
| Married | 92 | 77 |
| Separated | 6 | 5 |
| Never married | 16 | 13 |
| Divorced | 4 | 3 |
| Widowed | 2 | 2 |
| Monthly Family Income (GHC) | ||
| Less than 1000 | 69 | 57 |
| 1001–2000 | 36 | 30 |
| 2001–3000 | 12 | 10 |
| 3001–4000 | 2 | 2 |
| More than 4000 | 1 | 1 |
| Ethnicity# | ||
| Ga | 25 | 21 |
| Guan | 1 | 1 |
| Ewe | 25 | 21 |
| Akan | 52 | 43 |
| Hausa | 8 | 7 |
| Other | 9 | 7 |
| Primary Caregiver’s Relationship with Child | ||
| Mother | 98 | 82 |
| Grandparent | 10 | 8 |
| Mother and Father † | 3 | 3 |
| Mother and Grandparent † | 4 | 3 |
| Father | 3 | 2 |
| Mother and Father and Grandparent † | 1 | 1 |
| Auntie | 1 | 1 |
| Primary Caregiver Completed SHS | ||
| Yes | 51 | 42 |
| No | 69 | 58 |
| Needs of Caregivers | p-Value | r(118) |
|---|---|---|
| Improved accessibility in the home to reduce hardship for child | <0.001 | 0.3 |
| Assistive devices to meet my child’s needs | 0.003 | 0.27 |
| More time for myself | 0.017 | 0.24 |
| Recreational facilities for my child | 0.009 | 0.22 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aduful, A.K.; Boamah-Mensah, F.; Nyarko, M.Y.; Neizer, M.L.; Brew, Y.N.; Williams, L.A.; Calys-Tagoe, B.N.L.; Ackun, H.K.M.; Tette, E.M.A. Family Needs Assessment of Patients with Cerebral Palsy Attending Two Hospitals in Accra, Ghana. Children 2023, 10, 1313. https://doi.org/10.3390/children10081313
Aduful AK, Boamah-Mensah F, Nyarko MY, Neizer ML, Brew YN, Williams LA, Calys-Tagoe BNL, Ackun HKM, Tette EMA. Family Needs Assessment of Patients with Cerebral Palsy Attending Two Hospitals in Accra, Ghana. Children. 2023; 10(8):1313. https://doi.org/10.3390/children10081313
Chicago/Turabian StyleAduful, Abena K., Faye Boamah-Mensah, Mame Yaa Nyarko, Margaret L. Neizer, Yvonne N. Brew, Lovia A. Williams, Benedict N. L. Calys-Tagoe, Henry K. M. Ackun, and Edem M. A. Tette. 2023. "Family Needs Assessment of Patients with Cerebral Palsy Attending Two Hospitals in Accra, Ghana" Children 10, no. 8: 1313. https://doi.org/10.3390/children10081313
APA StyleAduful, A. K., Boamah-Mensah, F., Nyarko, M. Y., Neizer, M. L., Brew, Y. N., Williams, L. A., Calys-Tagoe, B. N. L., Ackun, H. K. M., & Tette, E. M. A. (2023). Family Needs Assessment of Patients with Cerebral Palsy Attending Two Hospitals in Accra, Ghana. Children, 10(8), 1313. https://doi.org/10.3390/children10081313






