Cross-Bite and Oral-Health-Related Quality of Life (OHRQoL) in Preadolescents Aged 11 to 14 Years Old: A Pilot Case-Control Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. OHRQoL Analysis
2.3. Statistical Analysis
3. Results
3.1. Description of the Sample
3.2. Descriptive Analysis of the Child Perceptions Questionnaire (CPQ-Esp11–14)
3.3. Comparison among Study Groups
3.4. Analysis of the Influence of Sex on OHRQoL
3.5. Analysis of the Influence of Age on OHRQoL
4. Discussion
4.1. Limitations
4.2. Recommendations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Macena, M.C.; Katz, C.R.; Rosenblatt, A. Prevalence of a posterior crossbite and sucking habits in Brazilian children aged 18–59 months. Eur. J. Orthod. 2009, 31, 357–361. [Google Scholar] [CrossRef] [PubMed]
- Bukhari, A.; Kennedy, D.; Hannam, A.; Aleksejūnienė, J.; Yen, E. Dimensional changes in the palate associated with slow maxillary expansion for early treatment of posterior crossbite. Angle Orthod. 2018, 88, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Petrén, S.; Bjerklin, K.; Bondemark, L. Stability of unilateral posterior crossbite correction in the mixed dentition: A randomized clinical trial with a 3-year follow-up. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Petrén, S.; Bondemark, L. Correction of unilateral posterior crossbite in the mixed dentition: A randomized controlled trial. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Malandris, M.; Mahoney, E.K. Aetiology, diagnosis and treatment of posterior cross-bites in the primary dentition. Int. J. Paediatr. Dent. 2004, 14, 155–166. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, G.; Vena, F.; Negri, P.; Pagano, S.; Barilotti, C.; Paglia, L.; Colombo, S.; Orso, M.; Cianetti, S. Worldwide prevalence of malocclusion in the different stages of dentition: A systematic review and meta-analysis. Eur. J. Paediatr. Dent. 2020, 21, 115–122. [Google Scholar]
- Ugolini, A.; Agostino, P.; Silvestrini-Biavati, A.; Harrison, J.E.; Batista, K.B. Orthodontic treatment for posterior crossbites. Cochrane Database Syst. Rev. 2021, 12, CD000979. [Google Scholar]
- McNamara, J.A., Jr. Early intervention in the transverse dimension: Is it worth the effort? Am. J. Orthod. Dentofac. Orthop. 2002, 121, 572–574. [Google Scholar] [CrossRef]
- D’Onofrio, L. Oral dysfunction as a cause of malocclusion. Orthod. Craniofac. Res. 2019, 22, 43–48. [Google Scholar] [CrossRef]
- Schmid, K.M.; Kugler, R.; Nalabothu, P.; Bosch, C.; Verna, C. The effect of pacifier sucking on orofacial structures: A systematic literature review. Prog. Orthod. 2018, 19, 8. [Google Scholar] [CrossRef]
- Agostino, P.; Ugolini, A.; Signori, A.; Silvestrini-Biavati, A.; Harrison, J.E.; Riley, P. Orthodontic treatment for posterior crossbites. Cochrane Database Syst. Rev. 2014, 8, CD000979. [Google Scholar] [CrossRef] [PubMed]
- Ellabban, M.T.; Abdul-Aziz, A.I.; Fayed, M.M.S.; Aboul Fotouh, M.H.; Elkattan, E.S.; Dahaba, M.M. Positional and dimensional temporomandibular joint changes after correction of posterior crossbite in growing patients: A systematic review. Angle Orthod. 2018, 88, 638–648. [Google Scholar] [CrossRef] [PubMed]
- Iodice, G.; Danzi, G.; Cimino, R.; Paduano, S.; Michelotti, A. Association between posterior crossbite, masticatory muscle pain, and disc displacement: A systematic review. Eur. J. Orthod. 2013, 35, 737–744. [Google Scholar] [CrossRef]
- Le Gall, M.; Philip, C.; Bandon, D. Les anomalies maxillomandibulaires du sens transversal chez l’enfant [Diagnosis and treatment of cross-bite in children]. Arch. Pediatr. 2009, 16, 209–213. [Google Scholar] [CrossRef]
- Kim, H.Y.; Kim, J.; Hong, S.M. Do the oral health-related quality of life and the magnitude of its association with malocclusion differ by developmental stages of schoolchildren? Am. J. Orthod. Dentofac. Orthop. 2023, 163, 777–785. [Google Scholar] [CrossRef]
- Aldrigui, J.M.; Abanto, J.; Carvalho, T.S.; Mendes, F.M.; Wanderley, M.T.; Bönecker, M.; Raggio, D.P. Impact of traumatic dental injuries and malocclusions on quality of life of young children. Health Qual. Life Outcomes 2011, 9, 78. [Google Scholar] [CrossRef]
- Thomson, W.M.; Broder, H.L. Oral-Health-Related Quality of Life in Children and Adolescents. Pediatr. Clin. N. Am. 2018, 65, 1073–1084. [Google Scholar] [CrossRef]
- Lourdes-Ribeiro, M.L.; Pereira Martins, L.; Bittencourt, J.M.; Paiva, S.M.; Pimenta Vale, M.; Bendo, C.B. Adolescents’ and Parents’ Perspective on Impact of Dental Caries and Malocclusion on Quality of Life. J. Dent. Child. 2022, 89, 136–142. [Google Scholar]
- Abreu, L.G.; Melgaço, C.A.; Abreu, M.H.; Lages, E.M.; Paiva, S.M. Perception of parents and caregivers regarding the impact of malocclusion on adolescents’ quality of life: A cross-sectional study. Dental Press J. Orthod. 2016, 21, 74–81. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Jokovic, A.; Locker, D.; Stephens, M.; Kenny, D.; Tompson, B.; Guyatt, G. Measuring parental perceptions of child oral health-related quality of life. J. Public Health Dent. 2003, 63, 67–72. [Google Scholar] [CrossRef]
- Jokovic, A.; Locker, D.; Stephens, M.; Guyatt, G. Agreement between mothers and children aged 11–14 years in rating child oral health-related quality of life. Community Dent. Oral Epidemiol. 2003, 31, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Azaustre, M.P.; Greco, R.; Llena, C. Oral Health-Related Quality of Life in Adolescents as Measured with the Child-OIDP Questionnaire: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 12995. [Google Scholar] [CrossRef] [PubMed]
- Ruff, R.R.; Sischo, L.; Chinn, C.H.; Broder, H.L. Development and validation of the Child Oral Health Impact Profile—Preschool version. Commun. Dent. Health 2017, 34, 176–182. [Google Scholar]
- Ludovichetti, F.S.; Zuccon, A.; Cantatore, D.; Zambon, G.; Girotto, L.; Lucchi, P.; Stellini, E.; Mazzoleni, S. Early Childhood Caries and Oral Health-Related Quality of Life: Evaluation of the Effectiveness of Single-Session Therapy Under General Anesthesia. Eur. J. Dent. 2022, 28. [Google Scholar] [CrossRef]
- Raghu, R.; Gauba, K.; Goyal, A.; Kapur, A.; Gupta, A.; Singh, S.K. Oral Health-related Quality of Life of Children with Early Childhood Caries before and after Receiving Complete Oral Rehabilitation under General Anesthesia. Int. J. Clin. Pediatr. Dent. 2021, 14, 117–123. [Google Scholar]
- Curto, A.; Mihit, F.; Curto, D.; Albaladejo, A. Assessment of Orthodontic Treatment Need and Oral Health-Related Quality of Life in Asthmatic Children Aged 11 to 14 Years Old: A Cross-Sectional Study. Children 2023, 10, 176. [Google Scholar] [CrossRef]
- Dawoodbhoy, I.; Delgado-Angulo, E.K.; Bernabé, E. Impact of malocclusion on the quality of life of Saudi children. Angle Orthod. 2013, 83, 1043–1048. [Google Scholar] [CrossRef]
- Agou, S.; Locker, D.; Streiner, D.L.; Tompson, B. Impact of self-esteem on the oral-health-related quality of life of children with malocclusion. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 484–489. [Google Scholar] [CrossRef]
- Kolawole, K.A.; Otuyemi, O.D.; Oluwadaisi, A.M. Assessment of oral health-related quality of life in Nigerian children using the Child Perceptions Questionnaire (CPQ 11–14). Eur. J. Paediatr. Dent. 2011, 12, 55–59. [Google Scholar]
- Barbosa, T.S.; Tureli, M.C.; Gavião, M.B. Validity and reliability of the Child Perceptions Questionnaires applied in Brazilian children. BMC Oral Health 2009, 9, 13. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet 2007, 370, 1453–1457. [Google Scholar] [CrossRef] [PubMed]
- Brook, P.H.; Shaw, W.C. The development of an index of orthodontic treatment priority. Eur. J. Orthod. 1989, 11, 309–320. [Google Scholar] [CrossRef] [PubMed]
- Almeida, R.R.; Almeida, M.R.; Oltramari-Navarro, P.V.; Conti, A.C.; Navarro, R.L.; Marques, H.V. Posterior crossbite—Treatment and stability. J. Appl. Oral Sci. 2012, 20, 286–294. [Google Scholar] [CrossRef]
- Salinas-Martínez, A.M.; Hernández-Elizondo, R.T.; Núñez-Rocha, G.M.; Ramos Peña, E.G. Psychometric properties of the Spanish version of the short-form Child Perceptions Questionnaire for 11–14-year-olds for assessing oral health needs of children. J. Public Health Dent. 2014, 74, 168–174. [Google Scholar] [CrossRef]
- Locker, D.; Jokovic, A.; Tompson, B.; Prakash, P. Is the Child Perceptions Questionnaire for 11–14 year olds sensitive to clinical and self-perceived variations in orthodontic status? Community Dent. Oral Epidemiol. 2007, 35, 179–185. [Google Scholar] [CrossRef]
- Aydoğan, C.; Yılmaz, A.C.; Alagöz, A.; Sadıkzade, D.S. Child perceptions questionnaire 11–14 in Turkish language in an orthodontic patient sample. Eur. Oral Res. 2018, 52, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Jokovic, A.; Locker, D.; Stephens, M.; Kenny, D.; Tompson, B.; Guyatt, G. Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J. Dent. Res. 2002, 81, 459–463. [Google Scholar] [CrossRef] [PubMed]
- Foster Page, L.A.; Thomson, W.M.; Jokovic, A.; Locker, D. Epidemiological evaluation of short-form versions of the Child Perception Questionnaire. Eur. J. Oral Sci. 2008, 116, 538–544. [Google Scholar] [CrossRef] [PubMed]
- Merdad, L.; El-Housseiny, A.A. Do children’s previous dental experience and fear affect their perceived oral health-related quality of life (OHRQoL)? BMC Oral Health 2017, 17, 47. [Google Scholar] [CrossRef]
- Ribeiro, L.G.; Antunes, L.S.; Küchler, E.C.; Baratto-Filho, F.; Kirschneck, C.; Guimarães, L.S.; Antunes, L.A.A. Impact of malocclusion treatments on Oral Health-Related Quality of Life: An overview of systematic reviews. Clin. Oral Investig. 2023, 27, 907–932. [Google Scholar] [CrossRef]
- Alrashed, M.; Alqerban, A. The relationship between malocclusion and oral health-related quality of life among adolescents: A systematic literature review and meta-analysis. Eur. J. Orthod. 2021, 43, 173–183. [Google Scholar] [CrossRef]
- Sun, L.; Wong, H.M.; McGrath, C.P.J. Association Between the Severity of Malocclusion, Assessed by Occlusal Indices, and Oral Health Related Quality of Life: A Systematic Review and Meta-Analysis. Oral Health Prev. Dent. 2018, 16, 211–223. [Google Scholar] [PubMed]
- Sun, L.; Wong, H.M.; McGrath, C.P. Relationship Between the Severity of Malocclusion and Oral Health Related Quality of Life: A Systematic Review and Meta-analysis. Oral Health Prev. Dent. 2017, 15, 503–517. [Google Scholar]
- Ukra, A.; Foster Page, L.A.; Thomson, W.M.; Farella, M.; Tawse Smith, A.; Beck, V. Impact of malocclusion on quality of life among New Zealand adolescents. N. Z. Dent. J. 2013, 109, 18–23. [Google Scholar] [PubMed]
- Cunningham, S.J.; Hunt, N.P. Quality of life and its importance in orthodontics. J. Orthod. 2001, 28, 152–158. [Google Scholar] [CrossRef] [PubMed]
- Broder, H.L.; McGrath, C.; Cisneros, G.J. Questionnaire development: Face validity and item impact testing of the Child Oral Health Impact Profile. Community Dent. Oral Epidemiol. 2007, 35, 8–19. [Google Scholar] [CrossRef]
- Pahel, B.T.; Rozier, R.G.; Slade, G.D. Parental perceptions of children’s oral health: The Early Childhood Oral Health Impact Scale (ECOHIS). Health Qual. Life Outcomes 2007, 5, 6. [Google Scholar] [CrossRef] [PubMed]
- Tadakamadla, S.K.; Mangal, G.; Quadri, M.F.A.; Nayeem, M.; Tadakamadla, J. Psychometric Analyses of the Indian (Hindi) Version of the Child Perception Questionnaire (CPQ11–14). Children 2020, 7, 175. [Google Scholar] [CrossRef]
- De Stefani, A.; Bruno, G.; Irlandese, G.; Barone, M.; Costa, G.; Gracco, A. Oral health-related quality of life in children using the child perception questionnaire CPQ11–14: A review. Eur. Arch. Paediatr. Dent. 2019, 20, 425–430. [Google Scholar] [CrossRef]
- Kallunki, J.; Sollenius, O.; Paulsson, L.; Petrén, S.; Dimberg, L.; Bondemark, L. Oral health-related quality of life among children with excessive overjet or unilateral posterior crossbite with functional shift compared to children with no or mild orthodontic treatment need. Eur. J. Orthod. 2019, 41, 111–116. [Google Scholar] [CrossRef]
- Baskaradoss, J.K.; Geevarghese, A.; Alsaadi, W.; Alemam, H.; Alghaihab, A.; Almutairi, A.S.; Almthen, A. The impact of malocclusion on the oral health related quality of life of 11–14-year-old children. BMC Pediatr. 2022, 22, 91. [Google Scholar] [CrossRef] [PubMed]
| Total Sample (n = 120) | Group | Chi-Square Test | ||||
|---|---|---|---|---|---|---|
| Control (n = 40) | UPCB (n = 40) | BPCB (n = 40) | Statistical | p-Value | ||
| Age | 2.17 ns | 0.904 | ||||
| 11 years old | 25.8% (n = 31) | 25.0% (n = 10) | 20.0% (n = 8) | 32.5% (n = 13) | ||
| 12 years old | 39.2% (n = 47) | 42.5% (n = 17) | 40.0% (n = 16) | 35.0% (n = 14) | ||
| 13 years old | 23.3% (n = 28) | 22.5% (n = 9) | 27.5% (n = 11) | 20.0% (n = 8) | ||
| 14 years | 11.7% (n = 14) | 10.0% (n = 4) | 12.5% (n = 5) | 12.5% (n = 5) | ||
| Sex | 1.40 ns | 0.497 | ||||
| Female | 50.0% (n = 60) | 45.0% (n = 18) | 47.5% (n = 19) | 57.5% (n = 23) | ||
| Male | 50.0% (n = 60) | 55.0% (n = 22) | 52.5% (n = 21) | 42.5% (n = 17) | ||
| Categories | Centrality | Variability | Form | Kolmogorov–Smirnov Test p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| Mean [95% CI] | Medium | Range | Standard Deviation | Interquartile Range | Skewness | Kurtosis | ||
| Oral symptoms | 1.30 (1.25–1.35) | 1.33 | 0.83/2.17 | ±0.29 | 0.33 | 0.97 | 0.50 | 0.000 |
| Functional limitations | 1.33 (1.29–1.38) | 1.33 | 0.89/2.00 | ±0.24 | 0.33 | 0.62 | −0.09 | 0.000 |
| Emotional wellbeing | 1.36 (1.32–1.40) | 1.33 | 0.89/2.00 | ±0.22 | 0.22 | 0.81 | 0.19 | 0.000 |
| Social wellbeing | 1.25 (1.21–1.28) | 1.23 | 0.85/1.77 | ±0.19 | 0.15 | 0.56 | −0.14 | 0.000 |
| Total score | 1.30 (1.27–1.34) | 1.22 | 0.97/1.73 | ±0.19 | 0.27 | 0.78 | −0.48 | 0 |
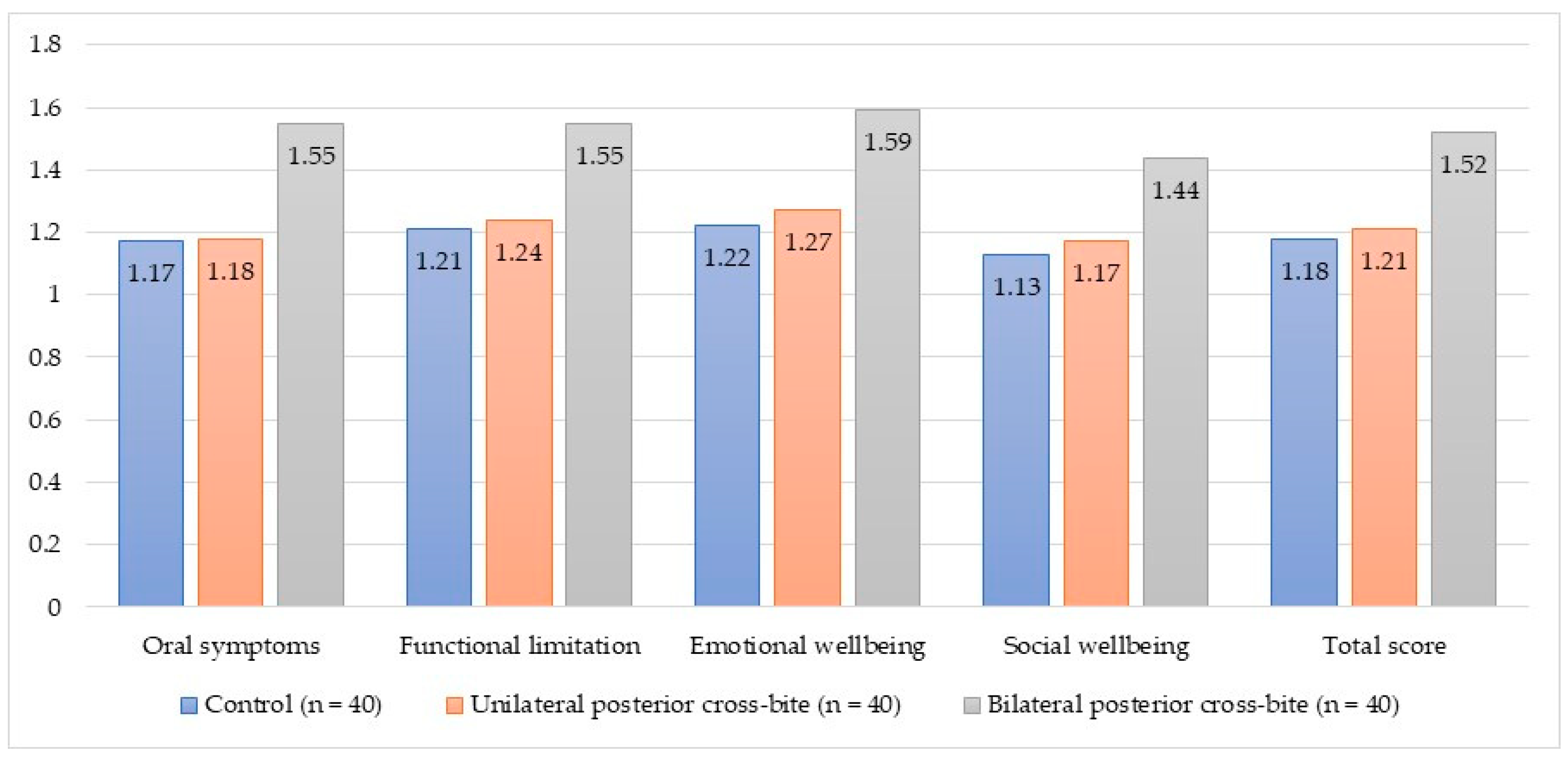
| Categories | Mean (±Standard Deviation) | Kruskal–Wallis Test | Effect Size: R2 | |||
|---|---|---|---|---|---|---|
| Control (n = 40) | UPCB (n = 40) | BPCB (n = 40) | Statistical | p-Value | ||
| Oral symptoms | 1.17 (±0.17) | 1.18 (±0.16) | 1.55 (±0.31) | 38.94 ** | 0.000 | 0.384 |
| Functional limitation | 1.21 (±0.14) | 1.24 (±0.14) | 1.55 (±0.24) | 44.73 ** | 0.000 | 0.426 |
| Emotional wellbeing | 1.22 (±0.09) | 1.27 (±0.14) | 1.59 (±0.21) | 59.60 ** | 0.000 | 0.529 |
| Social wellbeing | 1.13 (±0.11) | 1.17 (±0.10) | 1.44 (±0.18) | 54.42 ** | 0.000 | 0.515 |
| Total score | 1.18 (±0.08) | 1.21 (±0.09) | 1.52 (±0.17) | 63.46 ** | 0.000 | 0.629 |
| Categories | Mean (±Standard Deviation) | Mann–Whitney U Test | Effect Size: R2 | ||
|---|---|---|---|---|---|
| Boys (n = 60) | Girls (n = 60) | Statistical | p-Value | ||
| Oral symptoms | 1.24 (±0.26) | 1.36 (±0.30) | 2.37 * | 0.018 | 0.042 |
| Functional limitations | 1.32 (±0.23) | 1.35 (±0.25) | 0.59 ns | 0.556 | 0.003 |
| Emotional wellbeing | 1.35 (±0.22) | 1.37 (±0.23) | 0.42 ns | 0.675 | 0.003 |
| Social wellbeing | 1.23 (±0.17) | 1.26 (±0.21) | 0.17 ns | 0.685 | 0.004 |
| Total score | 1.28 (±0.18) | 1.32 (±0.21) | 0.92 ns | 0.355 | 0.011 |
| Categories | Mean (±Standard Deviation) | Mann–Whitney U Test | Effect Size: R2 | ||
|---|---|---|---|---|---|
| 11–12 Years (n = 78) | 13–14 Years (n = 42) | Statistical | p-Value | ||
| Oral symptoms | 1.31 (±0.29) | 1.27 (±0.28) | 1.07 ns | 0.286 | 0.007 |
| Functional limitations | 1.32 (±0.22) | 1.35 (±0.26) | 0.14 ns | 0.891 | 0.002 |
| Emotional wellbeing | 1.35 (±0.21) | 1.38 (±0.25) | 0.40 ns | 0.687 | 0.005 |
| Social wellbeing | 1.24 (±0.19) | 1.26 (±0.20) | 0.48 ns | 0.632 | 0.004 |
| Total score | 1.30 (±0.18) | 1.31 (±0.21) | 0.54 ns | 0.589 | 0.011 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Curto, A.; Albaladejo, A.; Alvarado-Lorenzo, A.; Zubizarreta-Macho, Á.; Curto, D. Cross-Bite and Oral-Health-Related Quality of Life (OHRQoL) in Preadolescents Aged 11 to 14 Years Old: A Pilot Case-Control Study. Children 2023, 10, 1311. https://doi.org/10.3390/children10081311
Curto A, Albaladejo A, Alvarado-Lorenzo A, Zubizarreta-Macho Á, Curto D. Cross-Bite and Oral-Health-Related Quality of Life (OHRQoL) in Preadolescents Aged 11 to 14 Years Old: A Pilot Case-Control Study. Children. 2023; 10(8):1311. https://doi.org/10.3390/children10081311
Chicago/Turabian StyleCurto, Adrián, Alberto Albaladejo, Alfonso Alvarado-Lorenzo, Álvaro Zubizarreta-Macho, and Daniel Curto. 2023. "Cross-Bite and Oral-Health-Related Quality of Life (OHRQoL) in Preadolescents Aged 11 to 14 Years Old: A Pilot Case-Control Study" Children 10, no. 8: 1311. https://doi.org/10.3390/children10081311
APA StyleCurto, A., Albaladejo, A., Alvarado-Lorenzo, A., Zubizarreta-Macho, Á., & Curto, D. (2023). Cross-Bite and Oral-Health-Related Quality of Life (OHRQoL) in Preadolescents Aged 11 to 14 Years Old: A Pilot Case-Control Study. Children, 10(8), 1311. https://doi.org/10.3390/children10081311








