Intraoperative Ultrasound in Minimally Invasive Laparoscopic and Robotic Pediatric Surgery: Our Experiences and Literature Review
Abstract
1. Introduction
2. Case Reports
2.1. Laparoscopic Lymphadenectomy
2.1.1. Case Presentation
2.1.2. Surgical Treatment
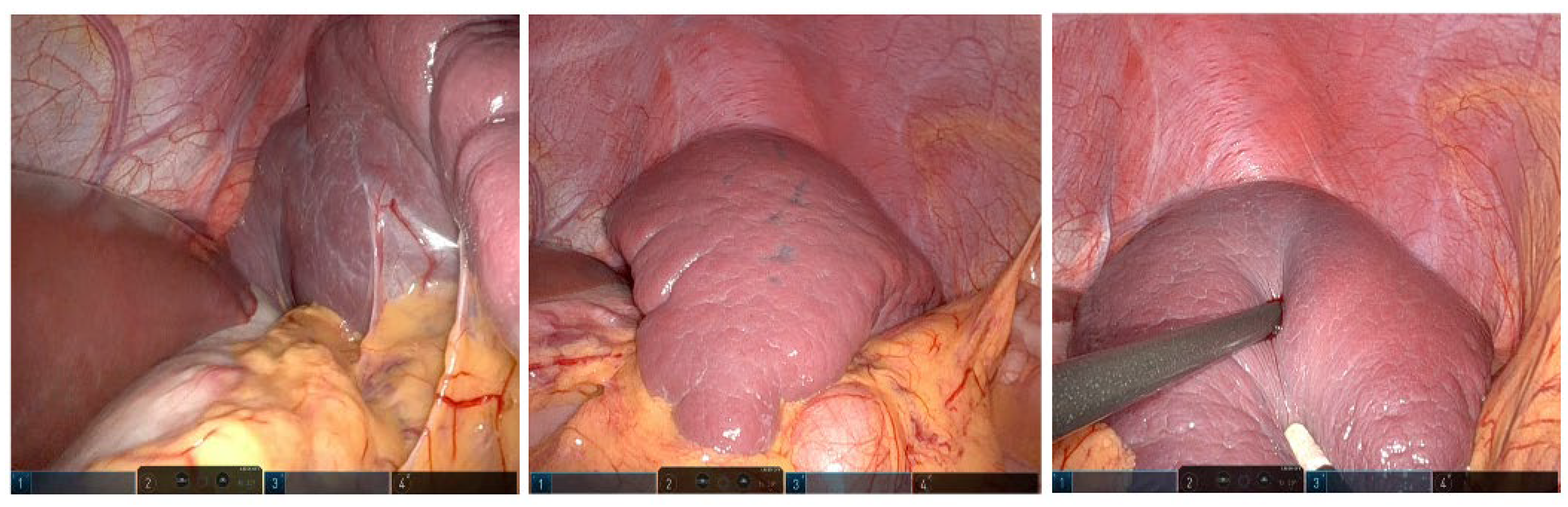
2.2. Robotic Marsupialization of a Splenic Cyst
2.2.1. Case Presentation
2.2.2. Surgical Treatment
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Parente, G.; Thomas, E.; Cravano, S.; Di Mitri, M.; Vastano, M.; Gargano, T.; Cerasoli, T.; Ruspi, F.; Libri, M.; Lima, M. ArtiSential® Articulated Wrist-Like Instruments and Their First Application in Pediatric Minimally Invasive Surgery: Case Reports and Literature Review of the Most Commonly Available Robot-Inspired Devices. Children 2021, 8, 603. [Google Scholar] [CrossRef] [PubMed]
- Pelizzo, G.; Bussani, R.; De Silvestri, A.; Di Mitri, M.; Rosone, G.; Amoroso, S.; Milazzo, M.; Girgenti, V.; Mura, G.B.; Unti, E.; et al. Laparoscopic Cholecystectomy for Symptomatic Cholecystic Disease in Children: Defining Surgical Timing. Front. Pediatr. 2020, 8, 2023. Available online: https://www.frontiersin.org/articles/10.3389/fped.2020.00203 (accessed on 16 April 2023). [CrossRef] [PubMed]
- Girgenti, V.; Pelizzo, G.; Amoroso, S.; Rosone, G.; Di Mitri, M.; Milazzo, M.; Giordano, S.; Genuardi, R.; Calcaterra, V. Emphysematous Pyelonephritis Following Ureterovesical Reimplantation for Congenital Obstructive Megaureter. Pediatric Case Report and Review of the Literature. Front. Pediatr. 2019, 7, 2. Available online: https://www.frontiersin.org/articles/10.3389/fped.2019.00002 (accessed on 16 April 2023). [CrossRef] [PubMed]
- Schlegel, J.; Diggdon, P.; Cuellar, J. The Use of Ultrasound for Localizing Renal Calculi. J. Urol. 1961, 86, 367–369. [Google Scholar] [CrossRef] [PubMed]
- Knight, P.; Newell, J. Operative use of ultrasonics in cholelithiasis. Lancet 1963, 281, 1023–1025. [Google Scholar] [CrossRef] [PubMed]
- Berber, E.; Siperstein, A.E. Laparoscopic ultrasound. Surg. Clin. N. Am. 2004, 84, 1061–1084. [Google Scholar] [CrossRef] [PubMed]
- Daskalaki, D.; Fernandes, E.; Wang, X.; Bianco, F.; Elli, E.F.; Ayloo, S.; Masrur, M.; Milone, L.; Giulianotti, P.C. Indocyanine Green (ICG) fluorescent cholangiography during robotic cholecystectomy: Results of 184 consecutive cases in a single institution. Surg. Innov. 2014, 21, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Aranda, F.P.; Škrabec, C.G.; López-Sánchez, J.; Pinedo, A.Z.; Álvarez, F.E.; Pérez, M.C.; López, J.N.; Vicente, C.H.; Piñeiro, L.V.; Andorrà, E.C. Indocyanine green (ICG) fluorescent cholangiography in laparoscopic cholecystectomy: Simplifying time and dose. Dig. Liver Dis. Off J. Ital. Soc. Gastroenterol Ital. Assoc. Study Liver. 2023, 55, 249–253. [Google Scholar] [CrossRef]
- López-Sánchez, J.; Garrosa-Muñoz, S.; Aranda, F.P.; Škrabec, C.G.; Pérez, R.L.; Rodríguez-Fortúnez, P.; Santos, J.M.S.; Muñoz-Bellvís, L. Dose and administration time of indocyanine green in near-infrared fluorescence cholangiography during laparoscopic cholecystectomy (DOTIG): Study protocol for a randomised clinical trial. BMJ Open 2023, 13, e067794. [Google Scholar] [CrossRef] [PubMed]
- Patankar, R.; Mishra, R.; Bindal, V.; Kothari, C.; Rahate, P.; Patnaik, S.; Kankaria, J.; Nayak, S. Efficacy of near-infrared fluorescence cholangiography using indocyanine green in laparoscopic cholecystectomy: A retrospective study. J. Minimal Access Surg. 2023, 19, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Gumprecht, J.D.J.; Maier, T.; Eckl, R.; Stolzenburg, J.-U.; Lüth, T.C. A new ultrasound imaging concept for laparoscopy in urology. Annu. Int. Conf. IEEE Eng. Med. Biol. Soc. IEEE Eng. Med. Biol. Soc. Annu. Int. Conf. 2010, 2010, 5991–5994. [Google Scholar] [CrossRef]
- Paterson, R.F.; Barret, E.; Siqueira, T.M.; Gardner, T.A.; Tavakkoli, J.; Rao, V.V.; Sanghvi, N.T.; Cheng, L.; Shalhav, A.L. Laparoscopic Partial Kidney Ablation with High Intensity Focused Ultrasound. J. Urol. 2003, 169, 347–351. [Google Scholar] [CrossRef] [PubMed]
- Gill, I.S.; Hsu, T.H.; Fox, R.L.; Matamoros, A.; Miller, C.D.; Leveen, R.F.; Grune, M.T.; Sung, G.T.; Fidler, M.E. Laparoscopic and percutaneous radiofrequency ablation of the kidney: Acute and chronic porcine study. Urology 2000, 56, 197–200. [Google Scholar] [CrossRef] [PubMed]
- Rawlings, C.A.; Howerth, E.W. Obtaining Quality Biopsies of the Liver and Kidney. J. Am. Anim. Hosp. Assoc. 2004, 40, 352–358. [Google Scholar] [CrossRef] [PubMed]
- Wu, B.; Liu, B.; Zhan, Y.; Chen, X.; Xie, Q. Laparoscopic ultrasonography: The wave of the future in renal cell carcinoma? Endosc. Ultrasound 2018, 7, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Fazio, L.M.; Downey, D.; Nguan, C.Y.; Karnik, V.; Al-Omar, M.; Kwan, K.; Izawa, J.I.; Chin, J.L.; Luke, P.P. Intraoperative laparoscopic renal ultrasonography: Use in advanced laparoscopic renal surgery. Urology 2006, 68, 723–727. [Google Scholar] [CrossRef] [PubMed]
- McKay, K.G.; Hanna, D.N.; Martin, L.; Datye, K.A.; Crane, G.L.; Correa, H.; Lovvorn, H.N.; Solorzano, C.C.; Zamora, I.J. Intraoperative Ultrasound Guided Laparoscopic Spleen-Preserving Distal Pancreatectomy for Primitive Neuroendocrine Tumors in a Pediatric Patient with MEN-1. Am. Surg. 2022, 88, 2241–2243. [Google Scholar] [CrossRef] [PubMed]



Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Mitri, M.; Thomas, E.; Di Carmine, A.; Manghi, I.; Cravano, S.M.; Bisanti, C.; Collautti, E.; Ruspi, F.; Cordola, C.; Vastano, M.; et al. Intraoperative Ultrasound in Minimally Invasive Laparoscopic and Robotic Pediatric Surgery: Our Experiences and Literature Review. Children 2023, 10, 1153. https://doi.org/10.3390/children10071153
Di Mitri M, Thomas E, Di Carmine A, Manghi I, Cravano SM, Bisanti C, Collautti E, Ruspi F, Cordola C, Vastano M, et al. Intraoperative Ultrasound in Minimally Invasive Laparoscopic and Robotic Pediatric Surgery: Our Experiences and Literature Review. Children. 2023; 10(7):1153. https://doi.org/10.3390/children10071153
Chicago/Turabian StyleDi Mitri, Marco, Eduje Thomas, Annalisa Di Carmine, Ilaria Manghi, Sara Maria Cravano, Cristian Bisanti, Edoardo Collautti, Francesca Ruspi, Chiara Cordola, Marzia Vastano, and et al. 2023. "Intraoperative Ultrasound in Minimally Invasive Laparoscopic and Robotic Pediatric Surgery: Our Experiences and Literature Review" Children 10, no. 7: 1153. https://doi.org/10.3390/children10071153
APA StyleDi Mitri, M., Thomas, E., Di Carmine, A., Manghi, I., Cravano, S. M., Bisanti, C., Collautti, E., Ruspi, F., Cordola, C., Vastano, M., D’Antonio, S., Libri, M., Gargano, T., & Lima, M. (2023). Intraoperative Ultrasound in Minimally Invasive Laparoscopic and Robotic Pediatric Surgery: Our Experiences and Literature Review. Children, 10(7), 1153. https://doi.org/10.3390/children10071153






