Abstract
Background: European guidelines recommend the use of pulse oximetry (PO) during newborn resuscitation, especially when there is a need for positive pressure ventilation or supplemental oxygen. The objective was to evaluate (i) to what extent PO was used, (ii) the time and resources spent on the application of PO, and (iii) the proportion of time with a useful PO signal during newborn resuscitation. Methods: A prospective observational study was conducted at Stavanger University Hospital, Norway, between 6 June 2019 and 16 November 2021. Newborn resuscitations were video recorded, and the use of PO during the first ten minutes of resuscitation was recorded and analysed. Results: Of 7466 enrolled newborns, 289 (3.9%) received ventilation at birth. The resuscitation was captured on video in 230 cases, and these newborns were included in the analysis. PO was applied in 222 of 230 (97%) newborns, median (quartiles) 60 (24, 58) seconds after placement on the resuscitation table. The proportion of time used on application and adjustments of PO during ongoing ventilation and during the first ten minutes on the resuscitation table was 30% and 17%, respectively. Median two healthcare providers were involved in the PO application. Video of the PO monitor signal was available in 118 (53%) of the 222 newborns. The proportion of time with a useful PO signal during ventilation and during the first ten minutes on the resuscitation table was 5% and 35%, respectively. Conclusion: In total, 97% of resuscitated newborns had PO applied, in line with resuscitation guidelines. However, the application of PO was time-consuming, and a PO signal was only obtained 5% of the time during positive pressure ventilation.
1. Introduction
Approximately 5% of newborns require resuscitation with positive pressure ventilations (PPV) at birth [1,2,3,4]. According to resuscitation guidelines, heart rate (HR) should be assessed after birth to evaluate the transition and identify newborns in need of resuscitation [5]. PPV should be initiated within 60 s if the newborn has not established effective breathing and HR is <100 beats per minute (bpm) and not increasing in response to initial drying and stimulation. Auscultation by stethoscope is an inexpensive and simple method that provides a rapid and intermittent assessment of HR, but HR is sometimes underestimated [2,6]. Continuous monitoring with pulse oximetry (PO) ± electrocardiogram (ECG) has the advantage of providing a more dynamic indication of HR changes and information on the responses to resuscitative interventions [5]. Several studies have shown that ECG presents HR more rapidly than PO, and that PO may underestimate HR in the initial minutes [7,8,9,10,11,12]. The Consensus on Science with Treatment Recommendations (CoSTR) from the International Liaison Committee on Resuscitation (ILCOR) therefore recommend the use of ECG for newborn HR assessment during delivery room resuscitation whenever possible [3,5]. Where ECG is not available, HR assessment with PO is a reasonable alternative, but the limitations should be kept in mind.
ECG does not replace the need for PO for evaluation of oxygenation and subsequent titration of oxygen to avoid hyper- and hypoxia [2,11]. International guidelines recommend the use of PO during PPV or when providing supplemental oxygen [2,3], and PO is common practice during newborn resuscitation in many high-resource settings [13].
The objectives were to evaluate (i) to what extent PO was used during newborn resuscitations; (ii) the number of healthcare providers (HCPs) involved, the number of single-use sensors required for the application of PO, time spent on application or adjustments of PO; and (iii) the proportion of time with a PO signal during provision of positive pressure ventilation at birth.
2. Materials and Methods
2.1. Setting
A prospective observational study was conducted at Stavanger University Hospital, Norway from 6 June 2019 to 16 November 2021. The hospital is well suited for population-based studies, being the only hospital in the region with obstetric and neonatal services and 4200 annual deliveries. Vaginal births take place in the labour ward and the midwife-run low-risk ward, and the caesarean sections in the operating theatre. PPV is provided to 3.6% of newborns, mainly by flow-driven t-piece resuscitator (NeoPuff, Fischer and Paykel, Auckland, New Zealand), alternatively a self-inflating silicone resuscitator (Laerdal, Stavanger, Norway) [4]. The paediatric resident and midwife initiate anticipated resuscitations, with the addition of a neonatologist, neonatal nurse, and an anaesthetic team for advanced resuscitations. The national resuscitation guidelines derive from the European Resuscitation Council Guidelines [2].
2.2. Data Collection and Equipment
Video recordings of resuscitations were obtained passively using motion-triggered cameras placed above the resuscitation tables, capturing the newborn and the hands of the HCPs. Dry-electrode ECG (NeoBeat, Laerdal Medical, Stavanger, Norway) was placed on the chest or upper abdomen of the newborn by the midwife assistants as soon as possible after birth. NeoBeat displays and stores HR within seconds of birth and provide continuous HR measurements. If a newborn required PPV, the cord was clamped and cut, and the newborn was carried to the resuscitation table. HCPs were instructed to apply 3-lead gel-electrode ECG (CareFusion, San Diego, CA, USA) on the newborns’ chest and PO (Massimo LNCS Neo wraparound sensor, Massimo, Irvine, CA, USA) on the newborns’ right hand or wrist. The order of ECG and PO placement was left to the discretion of the HCPs. However, in anticipated events, one HCP was assigned the task of applying the PO sensor. The monitor used was Carescape Patient monitor B450 or B650 (GE Healthcare, Boston, MA, USA). Video recordings were used to evaluate the time from birth to the start of ventilation, duration of PPV, application of PO and ECG, and to detect HR and PO signals displayed on the monitor. Extraction of patient characteristics were automated from electronic medical records.
2.3. Inclusion Criteria
Parents were informed and consented to participation during routine follow up in pregnancy. Newborns born at gestational age (GA) ≥ 28 weeks who required resuscitation with PPV at birth with the resuscitation captured on video, were enrolled.
2.4. Calculations and Definitions
All videos were manually reviewed by independent researchers (V.K. and S.R. or H.P.). Timelines were started when the newborn was placed on the resuscitation table, and for a duration of ten minutes. Videos were annotated using the ELAN 5.8 tool (The Language Archive, Nijmegen, The Netherlands). The start of PPV was defined as when the first inflation was provided. The duration of PPV was defined as the time difference between the first and last inflation. The number of HCPs involved in applying the PO equipment and the number of single-use PO sensors used were recorded. The time spent applying the PO was defined from when one started drying the skin or picking up the sensor, whichever came first, until the PO was attached, regardless of whether a useful signal was obtained. The PO adjustment time included repositioning or reapplying the sensor, reattaching the PO cord to the monitor and/or changing the sensor. The PO signal was annotated based on reviewing a recording of the monitor screen. The time to reliable PO signal was defined as the time when a continuous pulse wave, HR, and/or saturation values were displayed for at least 3 s [7,12,14].
2.5. Statistical Analysis
Data and annotations were extracted and analysed using Matlab R2022b (MathWorks Inc., Natick, MA, USA). Continuous variables are expressed as median (quartiles) or count (%).
2.6. Ethical Considerations
This study was a part of the Safer Births Stavanger research project on newborn resuscitation, with ethical approval from the Norwegian regional ethical committee 27 April 2018 (ref.2018/338).
3. Results
In total, 10,539 newborns were born during the study period, of which 10,503 with gestational age ≥28 weeks. Of these, 7466 (71%) parents agreed to participation, of which 289 (3.9%) received PPV at birth. The resuscitation was captured on video in 230/289 cases, and these newborns were included in the analysis. A flow diagram of over participants and patient characteristics is shown in Figure 1 and Table 1, respectively.
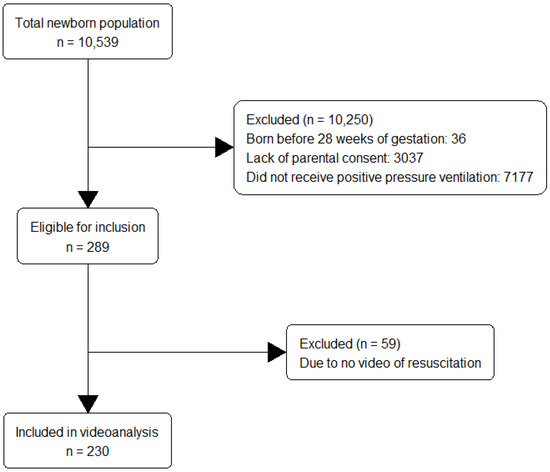
Figure 1.
A flow diagram of over participants.

Table 1.
Characteristics of 230 newborns included in the analysis. Characteristics are reported as median (quartiles) or count (%).
3.1. Use of Auscultation, ECG and PO Assessment during Resuscitation
Among 230 resuscitated newborns, 222 (97%) had PO applied during the first 10 min on the resuscitation table. PO was applied median (quartiles) 60 (24, 58) seconds after placement on the resuscitation table.
Auscultation with the stethoscope was performed in 211 (92%) median 39 (10, 110) seconds after placement on the table.
ECG was applied in 220 (96%) newborns. Standard 3-lead gel-electrode ECG was placed in 192 newborns at a median of 60 (41, 109) seconds. Dry-electrode ECG was in most instances placed in the delivery room, and the time of placement of NeoBeat was therefore median 0 (0, 3) seconds from placement on the resuscitation table (n = 204).
3.2. Number of HCPs Involved and Equipment Used for Application and Adjustment of PO
For 40% of newborns, one HCP was involved in the placement of PO. For 32% and 22% of newborns, two and three HCPs were involved, respectively. For the remaining 6%, four to six HCPs were at some time involved in the placement of PO. In 82% of the 222 resuscitations, one single-use sensor was used, whereas two sensors were used in the remaining 18% of cases.
3.3. Time Spent on the Application and Adjustment of PO
The median time to start the application of PO was 60 (23, 118) seconds after the newborn was placed on the resuscitation table. Time spent on applying and adjusting PO in the first 10 min of resuscitation was median 99 (44, 223) seconds. The time spent placing the PO is illustrated in blue lines in Figure 2. The proportion of time used on application and adjustments of PO during PPV and during the first ten minutes was 30% and 17%, respectively. In 58 (26%) newborns assessed with PO, the application was not completed by the time PPV ended.
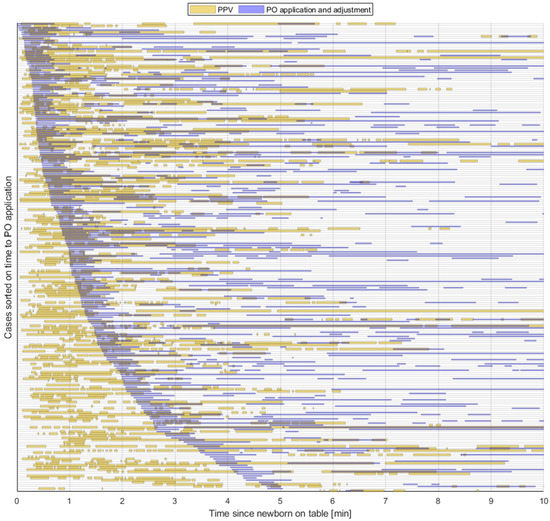
Figure 2.
The figure shows 222 newborns that received PPV at birth and had PO applied. Each horizontal line represents a newborn from the time of placement on the resuscitation table (time = 0) and the first consecutive ten minutes. Provision of PPV is illustrated in orange lines. Application and/or adjustment of PO is illustrated in blue lines. Newborns are sorted by time from placement on the resuscitation table to start application of PO. PPV = positive pressure ventilation, PO = pulse oximetry.
3.4. Feedback on PO Signal
Video of the PO monitor signal was available in 118 (53%) of the 222 newborns. In 110 of 118 newborns a PO signal was obtained within the first ten minutes on the resuscitation table. The time when a PO signal was first displayed and the proportion of time with a PO signal in relation to PPV is shown in Figure 3a and b, respectively. The median time to obtain PO signal was 238 (129, 324) seconds. PPV started a median of 21 (11, 51) seconds after placement on the resuscitation table, and lasted for a duration of 126 (65, 232) seconds (data available for 222 newborns). In 85 of 118 of newborns, PO was applied during PPV. Among these, a median time with a PO signal displayed during the provision of PPV was 9 (0, 84) seconds. The proportion of time with a PO signal during PPV and during the first ten minutes after placement on the resuscitation table was 5% (0%, 31%) and 35% (9%, 49%), respectively.
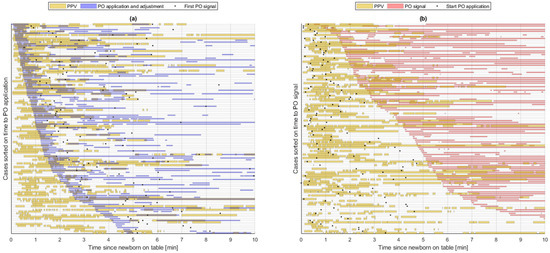
Figure 3.
The figure shows the 118 newborns where video of the PO monitor was available. Each horizontal line represents a newborn from the time of placement on the resuscitation table and throughout the first ten minutes. (a) shows the application and adjustment of PO illustrated in blue lines in relation to PPV in orange lines, and time when the first PO signal was displayed illustrated as a black dot. (b) shows the proportion of time with a PO signal illustrated in pink lines in relation to PPV illustrated in orange lines. The black dot represents the start of PO application. PPV = positive pressure ventilation, PO = pulse oximetry.
4. Discussion
In this population-based video study of 230 newborns receiving PPV at birth, we found that PO was applied in 97% of resuscitations, in line with guideline recommendations [2,5]. However, HCPs spent 30% of the active resuscitation with PPV applying and adjusting the PO sensor, and median two HCPs were involved. Throughout the duration of PPV, a PO signal was only displayed 5% of the time.
An accurate HR assessment is considered important to evaluate the newborn condition, to guide management, and to evaluate the effect of resuscitative interventions. PO has several limitations with regard to monitoring HR in the delivery room. Our group has recently shown that PO displayed HR values later and for a shorter proportion of newborn resuscitation, when compared to the dry-electrode ECG device NeoBeat or standard three-lead ECG [15]. PO may furthermore underestimate HR signal for the first five to six minutes during newborn transition or resuscitation, especially in the more compromised newborns [12,15,16,17].
In the current study, the median time to obtain a PO signal was 237 s after placement on the resuscitation table. Similar findings have been reported previously, with a success rate in obtaining saturation measurements varying between 20–100% at one minute after birth [18]. Several studies have found that reliable PO signals are rarely available in the first two minutes after birth [6,7,8,19,20]. A previous study by our team demonstrated that PO signal may be delayed in newborns with low APGAR scores, who represent the group in most need of HR feedback [7]. Others have evaluated the order of sensor application to the newborn with respect to the acquisition of a reliable PO signal [21,22,23,24], and video recordings in the present study showed that the practise did vary. The type of PO sensor used can also affect the time to a reliable signal during newborn resuscitations [25].
The results challenge the role of PO in the assessment of HR during newborn resuscitations. PO does, however, have an important role in the titration of oxygen provision during resuscitation in order to avoid hypoxia and hyperoxia with oxidative stress [25]. Although none of our videos showed a sign that PO disrupted or delayed PPV, the effort of placing PO rarely provided useful signal on HR or tissue oxygenation during ventilation. Most resuscitations in our setting were of short duration with moderately asphyxiated newborns. PO may have a more prominent role in prolonged and advanced resuscitations or stabilization of preterms. PO is also used to confirm if the newborn has the capacity to maintain stable oxygenation within the recommended range [26], and may help identify newborns in need of admission to the neonatal intensive care unit.
Considerable resources went into the placement of PO. HCPs spent 30% of the time during active resuscitation applying PO, without obtaining PO signal in the majority of cases. Where resources are limited, prioritizing the placement of PO during ventilation may be impractical.
This study was limited by the loss of PO signal data in 104 newborns due to technical errors, including frame freezing of the monitor video and loss of resuscitation videos due to a server failure without a backup. In this study, we analysed the availability of PO signal during resuscitation, but have not evaluated the HR signal accuracy compared to the gold standard ECG. The population was limited to newborns with gestational age ≥28 weeks, since extremely premature newborns were resuscitated and stabilized in incubators not equipped with video cameras. The strengths of the study are the population-based design and a high number of included newborns. The setting is representative of high-resource contexts.
5. Conclusions
During delivery room resuscitation, 97% of newborns had PO applied in line with European Resuscitation Council Guideline recommendations. However, the application of PO was time-consuming, and PO signal were only displayed for 5% of the time of active resuscitation with PPV.
Author Contributions
Conceptualization, S.R., V.K., H.P. and H.E.; methodology, S.R., V.K., H.P., H.E. and J.E.; data extraction and processing, J.E. and V.K.; validation, S.R., V.K., H.P., H.E., J.E. and F.B.; formal analysis, S.R., V.K. and J.E.; investigation, V.K. and S.R.; resources, S.R. and H.E.; data curation, S.R., V.K., J.E. and F.B.; writing—original draft preparation, V.K. and S.R.; writing—review and editing, V.K., S.R., H.P., H.E., J.E. and F.B.; visualization, J.E., V.K. and F.B.; supervision, S.R. and H.E.; project administration, S.R.; funding acquisition, S.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Stavanger University Hospital and Laerdal Foundation (Safer Healthcare grant no 5007). The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki and approved by the national Ethics Committee (reference number 2018/338), ethical date is 27 April 2018.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy statements made in informed consent obtained from participants.
Acknowledgments
We thank participating mothers and their newborns, and HCPs at Stavanger University Hospital for taking part in the study.
Conflicts of Interest
J.E. is an employee at Laerdal Medical. S.R. received an unconditional research grant by Laerdal Foundation. The other four authors declare no conflict of interest.
References
- Skare, C.; Kramer-Johansen, J.; Steen, T.; Odegaard, S.; Niles, D.E.; Nakstad, B.; Solevag, A.L.; Nadkarni, V.M.; Olasveengen, T.M. Incidence of Newborn Stabilization and Resuscitation Measures and Guideline Compliance during the First Minutes of Life in Norway. Neonatology 2015, 108, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Madar, J.; Roehr, C.C.; Ainsworth, S.; Ersdal, H.; Morley, C.; Rudiger, M.; Skare, C.; Szczapa, T.; Te Pas, A.; Trevisanuto, D.; et al. European Resuscitation Council Guidelines 2021: Newborn resuscitation and support of transition of infants at birth. Resuscitation 2021, 161, 291–326. [Google Scholar] [CrossRef] [PubMed]
- Wyckoff, M.H.; Wyllie, J.; Aziz, K.; de Almeida, M.F.; Fabres, J.W.; Fawke, J.; Guinsburg, R.; Hosono, S.; Isayama, T.; Kapadia, V.S.; et al. Neonatal Life Support 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation 2020, 156, A156–A187. [Google Scholar] [CrossRef] [PubMed]
- Bjorland, P.A.; Oymar, K.; Ersdal, H.L.; Rettedal, S.I. Incidence of newborn resuscitative interventions at birth and short-term outcomes: A regional population-based study. BMJ Paediatr. Open 2019, 3, e000592. [Google Scholar] [CrossRef]
- Wyckoff, M.H.; Greif, R.; Morley, P.T.; Ng, K.C.; Olasveengen, T.M.; Singletary, E.M.; Soar, J.; Cheng, A.; Drennan, I.R.; Liley, H.G.; et al. 2022 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations: Summary from the Basic Life Support; Advanced Life Support; Pediatric Life Support; Neonatal Life Support; Education, Implementation, and Teams; and First Aid Task Forces. Circulation 2022, 146, e483–e557. [Google Scholar] [CrossRef]
- Kamlin, C.O.; O’Donnell, C.P.; Everest, N.J.; Davis, P.G.; Morley, C.J. Accuracy of clinical assessment of infant heart rate in the delivery room. Resuscitation 2006, 71, 319–321. [Google Scholar] [CrossRef]
- Bjorland, P.A.; Ersdal, H.L.; Oymar, K.; Rettedal, S.I. Compliance with guidelines and efficacy of heart rate monitoring during newborn resuscitation: A prospective video study. Neonatology 2020, 117, 175–181. [Google Scholar] [CrossRef]
- Katheria, A.; Rich, W.; Finer, N. Electrocardiogram provides a continuous heart rate faster than oximetry during neonatal resuscitation. Pediatrics 2012, 130, e1177–e1181. [Google Scholar] [CrossRef]
- Iglesias, B.; Rodriguez, M.J.; Aleo, E.; Criado, E.; Herranz, G.; Moro, M.; Martinez Orgado, J.; Arruza, L. Pulse oximetry versus electrocardiogram for heart rate assessment during resuscitation of the preterm infant. Anales Pediatría 2016, 84, 271–277. [Google Scholar] [CrossRef]
- Mizumoto, H.; Tomotaki, S.; Shibata, H.; Ueda, K.; Akashi, R.; Uchio, H.; Hata, D. Electrocardiogram shows reliable heart rates much earlier than pulse oximetry during neonatal resuscitation. Pediatr. Int. 2012, 54, 205–207. [Google Scholar] [CrossRef]
- Perlman, J.M.; Wyllie, J.; Kattwinkel, J.; Wyckoff, M.H.; Aziz, K.; Guinsburg, R.; Kim, H.S.; Liley, H.G.; Mildenhall, L.; Simon, W.M.; et al. Part 7: Neonatal resuscitation: 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation 2015, 132 (Suppl. S1), S204–S241. [Google Scholar] [CrossRef]
- van Vonderen, J.J.; Hooper, S.B.; Kroese, J.K.; Roest, A.A.; Narayen, I.C.; van Zwet, E.W.; te Pas, A.B. Pulse oximetry measures a lower heart rate at birth compared with electrocardiography. J. Pediatr. 2015, 166, 49–53. [Google Scholar] [CrossRef]
- Johnson, P.A.; Cheung, P.Y.; Lee, T.F.; O’Reilly, M.; Schmolzer, G.M. Novel technologies for heart rate assessment during neonatal resuscitation at birth—A systematic review. Resuscitation 2019, 143, 196–207. [Google Scholar] [CrossRef]
- Dawson, J.A.; Saraswat, A.; Simionato, L.; Thio, M.; Kamlin, C.O.; Owen, L.S.; Schmölzer, G.M.; Davis, P.G. Comparison of heart rate and oxygen saturation measurements from Masimo and Nellcor pulse oximeters in newly born term infants. Acta Paediatr. 2013, 102, 955–960. [Google Scholar] [CrossRef]
- Rettedal, S.; Eilevstjonn, J.; Kibsgaard, A.; Kvaloy, J.T.; Ersdal, H. Comparison of Heart Rate Feedback from Dry-Electrode ECG, 3-Lead ECG, and Pulse Oximetry during Newborn Resuscitation. Children 2021, 8, 1092. [Google Scholar] [CrossRef]
- Narayen, I.C.; Smit, M.; van Zwet, E.W.; Dawson, J.A.; Blom, N.A.; te Pas, A.B. Low signal quality pulse oximetry measurements in newborn infants are reliable for oxygen saturation but underestimate heart rate. Acta Paediatr. 2015, 104, e158–e163. [Google Scholar] [CrossRef]
- Iglesias, B.; Rodri Guez, M.A.J.; Aleo, E.; Criado, E.; Marti Nez-Orgado, J.; Arruza, L. 3-lead electrocardiogram is more reliable than pulse oximetry to detect bradycardia during stabilisation at birth of very preterm infants. Arch. Dis. Child. Fetal Neonatal Ed. 2018, 103, F233–F237. [Google Scholar] [CrossRef]
- Dawson, J.A.; Davis, P.G.; O’Donnell, C.P.; Kamlin, C.O.; Morley, C.J. Pulse oximetry for monitoring infants in the delivery room: A review. Arch. Dis. Child. Fetal Neonatal Ed. 2007, 92, F4–F7. [Google Scholar] [CrossRef]
- Reddy, K.S.; Venkataravanappa, S.T.; Gururaja, G. Feasibility of Oxygen Saturation Monitoring During Neonatal Resuscitation in Indian Scenario. Indian Pediatr. 2018, 55, 999. [Google Scholar] [CrossRef]
- Gandhi, B.; Rich, W.; Finer, N. Time to achieve stable pulse oximetry values in VLBW infants in the delivery room. Resuscitation 2013, 84, 970–973. [Google Scholar] [CrossRef]
- Louis, D.; Sundaram, V.; Kumar, P. Pulse oximeter sensor application during neonatal resuscitation: A randomized controlled trial. Pediatrics 2014, 133, 476–482. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, C.P.; Kamlin, C.O.; Davis, P.G.; Morley, C.J. Obtaining pulse oximetry data in neonates: A randomised crossover study of sensor application techniques. Arch. Dis. Child. Fetal Neonatal Ed. 2005, 90, F84–F85. [Google Scholar] [CrossRef] [PubMed]
- Saraswat, A.; Simionato, L.; Dawson, J.A.; Thio, M.; Kamlin, C.O.; Owen, L.; Schmolzer, G.; Davis, P.G. Determining the best method of Nellcor pulse oximeter sensor application in neonates. Acta Paediatr. 2012, 101, 484–487. [Google Scholar] [CrossRef] [PubMed]
- O’Donnell, C.P.; Kamlin, C.O.; Davis, P.G.; Morley, C.J. Feasibility of and delay in obtaining pulse oximetry during neonatal resuscitation. J. Pediatr. 2005, 147, 698–699. [Google Scholar] [CrossRef]
- Baquero, H.; Alviz, R.; Castillo, A.; Neira, F.; Sola, A. Avoiding hyperoxemia during neonatal resuscitation: Time to response of different SpO2 monitors. Acta Paediatr. 2011, 100, 515–518. [Google Scholar] [CrossRef]
- Boldingh, A.M.; Skare, C.; Nakstad, B.; Solevag, A.L. Suboptimal heart rate assessment and airway management in infants receiving delivery room chest compressions: A quality assurance project. Arch. Dis. Child. Fetal Neonatal Ed. 2020, 105, 545–549. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).