Parent-Integrated Interventions to Improve Language Development in Children Born Very Preterm
Abstract
1. Introduction
2. Materials and Methods
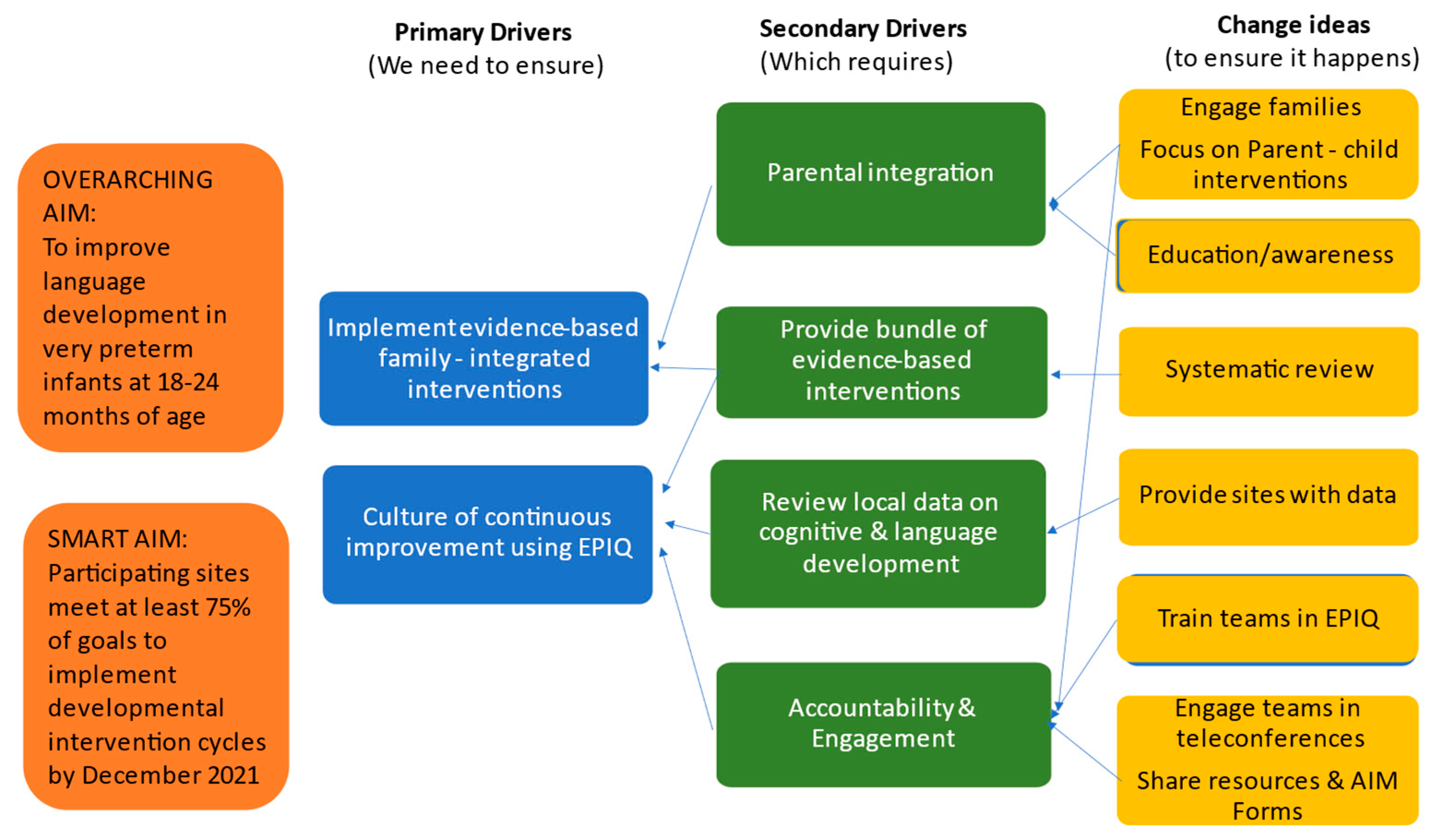
2.1. Design and Setting
2.2. Data Collection and Analyses
3. Results
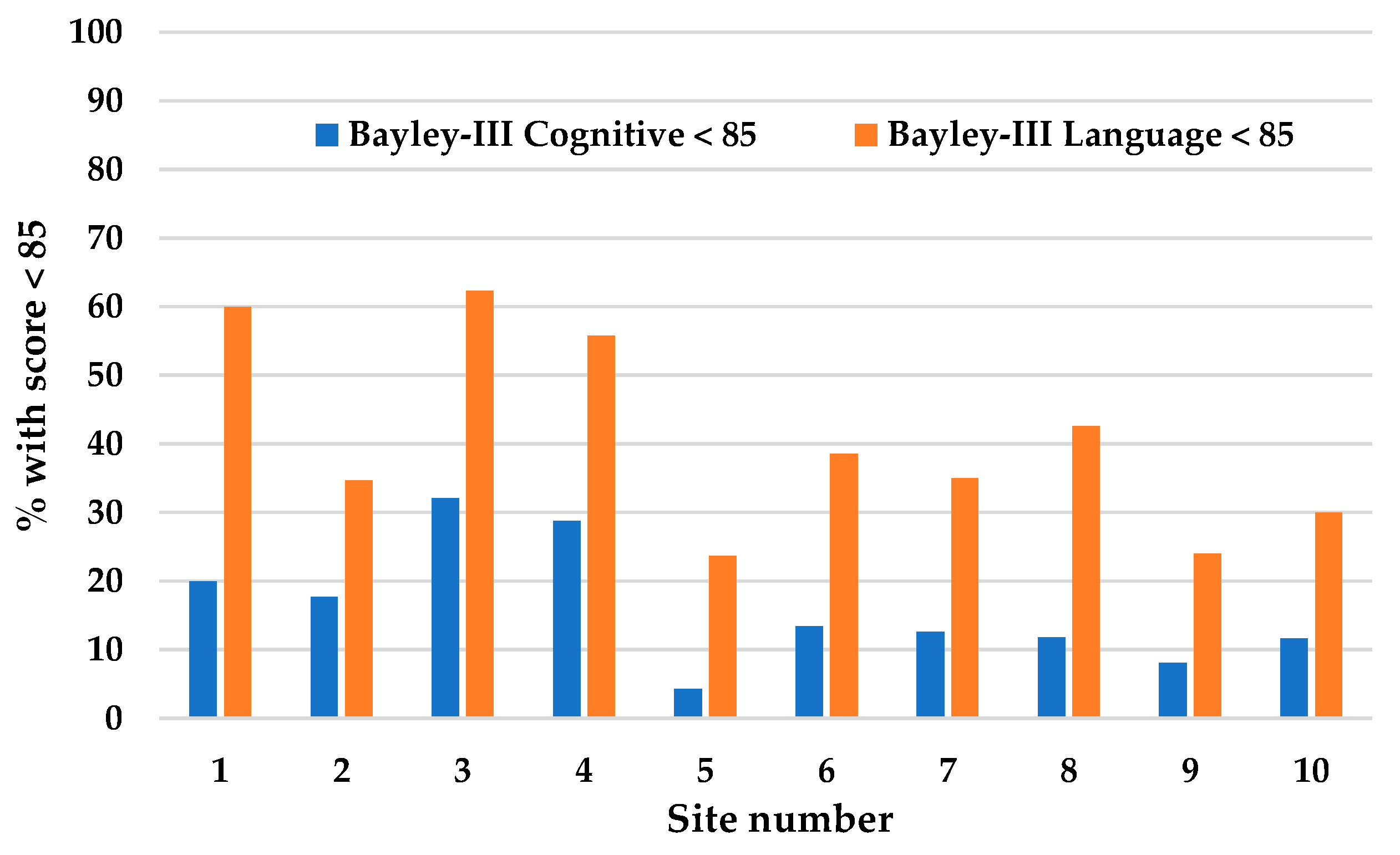
3.1. Site Description and Participation
3.2. Number of Parent-EPIQ Intervention Cycles Completed
3.3. Number of Parent-EPIQ Intervention Cycles That Met Goals
3.4. Description of Parent-EPIQ Intervention Cycles
3.5. Reasons That Parent-EPIQ Intervention Cycle Goals Were Not Met
3.6. Barriers and Facilitators
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Effectiveness of an Early Developmental Intervention to Improve Language and Social Development in at-Risk Infants—A Systematic Review
References
- Ricci, M.F.; Shah, P.; Moddemann, D.; Alvaro, R.; Ng, E.; Lee, S.K.; Synnes, A.; on behalf of the Canadian Neonatal Network and Canadian Neonatal Follow Up Network investigators. Neurodevelopmental outcomes of infants at < 29 weeks born in Canada between 2009 and 2016. J. Pediatr. 2022, 247, 60–66. [Google Scholar] [CrossRef] [PubMed]
- Bonifacio, S.L.; Glass, H.C.; Chau, V.; Berman, J.I.; Xu, D.; Brant, R.; Barkovich, A.J.; Poskitt, K.J.; Miller, S.P.; Ferriero, D.M. Extreme Premature Birth is not associated with impaired development of brain microstructure. J. Pediatr. 2010, 157, 726–732.e1. [Google Scholar] [CrossRef] [PubMed]
- Chau, V.; Brant, R.; Poskitt, K.J.; Tam, E.W.Y.; Synnes, A.; Miller, S.P. Postnatal infection is associated with widespread abnormalities of brain development in premature newborns. Pediatr. Res. 2012, 71, 274–279. [Google Scholar] [CrossRef] [PubMed]
- Tam, E.W.Y.; Chau, V.; Ferriero, D.M.; Barkovich, A.J.; Poskitt, K.J.; Studholme, C.; Fok, E.D.-Y.; Glidden, D.V.; Miller, S.P. Preterm cerebellar growth impairment after postnatal exposure to glucocorticoids. Sci. Transl. Med. 2011, 3, 105ra. [Google Scholar] [CrossRef]
- Ranger, M.; Chau, C.M.; Garg, A.; Woodward, T.S.; Beg, M.F.; Bjornson, B.; Poskitt, K.; Fitzpatrick, K.; Synnes, A.R.; Miller, S.P.; et al. Neonatal pain-related stress predicts cortical thickness at age 7 years in children born very preterm. PLoS ONE 2013, 8, e76702. [Google Scholar] [CrossRef]
- Bayley, N. Manual for the Bayley Scales of Infant and Toddler Development, 3rd ed.; The Psychological Corporation: San Antonio, TX, USA, 2006. [Google Scholar]
- Synnes, A.; Luu, T.M.; Moddemann, D.; Church, P.; Lee, D.; Vincer, M.; Ballantyne, M.; Majnemer, A.; Creighton, D.; Yang, J.; et al. Determinants of developmental outcomes in a very preterm Canadian cohort. Arch. Dis. Child. Fetal. Neonatal. 2016, 102, F235. [Google Scholar] [CrossRef]
- Resnick, M.B.; Gueorguieva, R.V.; Carter, R.L.; Ariet, M.; Sun, Y.; Roth, J.; Bucciaerelli, R.L.; Curran, J.S.; Mahan, C.S. The impact of low birth weight, perinatal conditions and sociodemographic factors on educational outcome in kindergarten. Pediatrics 1999, 104, e74. [Google Scholar] [CrossRef]
- Spittle, A.; Orton, J.; Anderson, P.J.; Boyd, R.; Doyle, L.W. Early developmental intervention programmes provided post hospital discharge to prevent motor and cognitive impairment in preterm infants. Cochrane Database Syst. Rev. 2015, 24, CD005495. [Google Scholar] [CrossRef]
- Vanderveen, J.A.; Bassler, D.; Robertson, C.M.T.; Kirpalani, H. Early interventions involving parents to improve neurodevelopmental outcomes of premature infants: A meta-analysis. J. Perinatol. 2009, 29, 343–351. [Google Scholar] [CrossRef]
- Puthussery, S.; Chutiyami, M.; Tseng, P.C.; Kilby, L.; Kapadia, J. Effectiveness of early intervention programs for parents of preterm infants: A meta-review of systematic reviews. BMC Pediatr. 2018, 18, 223. [Google Scholar] [CrossRef]
- Benzies, K.M.; Magill-Evans, J.E.; Hayden, K.A.; Ballantyne, M. Key components of early intervention programs for preterm infants and their parents: A systematic review and meta-analysis. BMC Pregnancy Childbirth 2013, 13 (Suppl. 1), S10. [Google Scholar] [CrossRef] [PubMed]
- Zuckerman, B. Promoting early literacy in pediatric practice: Twenty years of Reach Out and Read. Pediatrics 2009, 124, 1660–1665. [Google Scholar] [CrossRef] [PubMed]
- EPIQ. Evidence Based Practice to Improve Quality. Available online: https://www.epiq.ca (accessed on 9 November 2022).
- Lee, S.K.; Aziz, K.; Singhal, N.; Cronin, C.M.; James, A.; Lee, D.S.C.; Matthew, D.; Ohlsson, A.; Sankaran, K.; Seshia, M.; et al. Improving the quality of care for neonates: A cluster randomized controlled trial. CMAJ 2009, 181, 469–476. [Google Scholar] [CrossRef]
- Canadian Neonatal Network Partnerships for Health System Improvement Study Group. The Evidence-based Practice for Improving Quality method has greater impact on improvement of outcomes than dissemination of practice change guidelines and quality improvement training in neonatal intensive care units. Paediatr. Child Health 2015, 20, e1–e9. [Google Scholar] [CrossRef]
- Lee, S.K.; Shah, P.S.; Singhal, N.; Aziz, K.; Synnes, A.; McMillan, D.; Seshia, M.M.; for the Canadian EPIQ Study Group. Association of a quality improvement program with neonatal outcomes in extremely preterm infants: A prospective cohort study. CMAJ 2014, 186, E485–E494. [Google Scholar] [CrossRef]
- Gianni, M.; Picciolini, O.; Ravasi, M.; Gardon, L.; Vegni, C.; Fumagalli, M.; Mosca, F. The effects of an early developmental mother-child intervention program on neurodevelopment outcome in very low birth weight infants: A pilot study. Early Hum. Dev. 2006, 82, 691–695. [Google Scholar] [CrossRef]
- High, P.C.; LaGasse, L.; Becker, S.; Ahlgren, I.; Gardner, A. Literacy promotion in primary care pediatrics: Can we make a difference? Pediatrics 2000, 105 Pt 2, 927–934. [Google Scholar] [CrossRef] [PubMed]
- Lowell, D.I.; Carter, A.S.; Godoy, L.; Paulicin, B.; Briggs-Gowan, M.J. A randomized controlled trial of Child FIRST: A comprehensive home-based intervention translating research into early childhood practice. Child Dev. 2011, 82, 193–208. [Google Scholar] [CrossRef] [PubMed]
- Lunkenheimer, E.S.; Dishion, T.J.; Shaw, D.S.; Connell, A.M.; Gardner, F.; Wilson, M.N.; Skuban, E.M. Collateral benefits of the Family Check-Up on early childhood school readiness: Indirect effects of parents’ positive behavior support. Dev. Psychol. 2008, 44, 1737–1752. [Google Scholar] [CrossRef]
- McCormick, M.C.; Brooks-Gunn, J.; Buka, S.L.; Goldman, J.; Yu, J.; Salganik, M.; Scott, D.T.; Bennett, F.C.; Kay, L.L.; Bernbaum, J.C.; et al. Early intervention in low birth weight premature infants: Results at 18 years of age for the Infant Health and Development Program. Pediatrics 2006, 117, 771–780. [Google Scholar] [CrossRef]
- Meijssen, D.; Wolf, M.-J.; Koldewijn, K.; Houtzager, B.A.; van Wassenaer, A.; Tronick, E.; Kok, J.; van Baar, A. The effect of the Infant Behavioral Assessment and Intervention Program on mother-infant interaction after very preterm birth. J. Child Psychol. Psychiatry 2010, 51, 1287–1295. [Google Scholar] [CrossRef] [PubMed]
- Mendelsohn, A.L.; Dreyer, B.P.; Flynn, V.; Tomopoulos, S.; Rovira, I.; Tineo, W.; Pebenito, C.; Torres, C.; Torres, H.; Nixon, A.F. Use of Videotaped Interactions During Pediatric Well-Child Care to Promote Child Development: A Randomized, Controlled Trial. J. Dev. Behav. Pediatr. 2005, 26, 34–41. [Google Scholar] [PubMed]
- Schuler, M.E.; Nair, P.; Black, M.M. Ongoing maternal drug use, parenting attitudes, and a home intervention: Effects on mother-child interaction at 18 months. J. Dev. Behav. Pediatr. 2002, 23, 87–94. [Google Scholar] [CrossRef]
- Spencer-Smith, M.M.; Spittle, A.J.; Doyle, L.W.; Lee, K.J.; Lorefice, L.; Suetin, A.; Pasco, L.; Anderson, P.J. Long-term benefits of home-based preventive care for preterm infants: A randomized trial. Pediatrics 2012, 130, 1094–1101. [Google Scholar] [CrossRef]
- Spittle, A.J.; Anderson, P.J.; Lee, K.J.; Ferretti, C.; Eeles, A.; Orton, J.; Boyd, R.N.; Inder, T.; Doyle, L.W. Preventive care at home for very preterm infants improves infant and caregiver outcomes at 2 years. Pediatrics 2010, 126, e171–e178. [Google Scholar] [CrossRef]
- Tan, Z.A.; Tong, M.L.; Huang, P. Effects of early interventions to behavior development in infancy among premature and infants with low body mass at birth. Chin. J. Clin. Rehabil. 2004, 8, 2992–2993. [Google Scholar]
- van den Boom, D.C. Do first-year intervention effects endure? Follow-up during toddlerhood of a sample of Dutch irritable infants. Child Dev. 1995, 66, 1798–1816. [Google Scholar] [CrossRef] [PubMed]
- Rees, C.E.; Crampton, P.E.S.; Monrouxe, L.V. Re-visioning Academic Medicine Through a Constructionist Lens. Acad. Med. 2020, 95, 846–850. [Google Scholar] [CrossRef] [PubMed]
- Whitman, N. A review of constructivism: Understanding and using a relatively new theory. Fam. Med. 1993, 25, 517–521. [Google Scholar] [PubMed]
- Cane, J.; O’Connor, D.; Michie, S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement. Sci. 2012, 7, 37. [Google Scholar] [CrossRef]
- May, L.; Byers-Heinlein, K.; Gervain, J.; Werker, J.F. Language and the newborn brain: Does prenatal language experience shape the neonate neural response to speech? Front. Psychol. 2011, 2, 222. [Google Scholar] [CrossRef]
- Gervain, J. Plasticity in early language acquisition: The effects of prenatal and early childhood experience. Curr. Opin. Neurobiol. 2015, 35, 13–20. [Google Scholar] [CrossRef] [PubMed]
- Newnham, C.A.; Milgrom, J.; Skouteris, H. Effectiveness of a modified Mother-Infant Transaction Program on outcomes for preterm infants from 3 to 24 months of age. Infant. Behav. Dev. 2009, 32, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, T.M.; Howell, C.T.; Aoki, M.F.; Rauh, V.A. Nine-year outcome of the Vermont intervention program for low birth weight infants. Pediatrics 1993, 91, 45–55. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, P.S.; Danko, C.M.; Everhart, K.D.; Diaz, A.; Asherin, R.M.; Vogeli, J.M.; Fekri, S.M. Maternal depression and expressive communication in one-year-old infants. Infant. Behav. Dev. 2014, 37, 398–405. [Google Scholar] [CrossRef]
- Schaadt, G.; Zsido, R.G.; Villringer, A.; Obrig, H.; Männel, C.; Sacher, J. Association of postpartum maternal mood with infant speech perception at 2 and 6.5 months of age. JAMA Netw. Open 2022, 5, e2232672. [Google Scholar] [CrossRef]
- Stevens, B.; Lee, S.K.; Law, M.P.; Yamada, J.; Canadian Neonatal Network EPIC Study Group. A qualitative examination of changing practice in Canadian neonatal intensive care units. J. Eval. Clin. Pract. 2007, 13, 287–294. [Google Scholar] [CrossRef]
- Cronin, C.M.; Baker, G.R.; Lee, S.K.; Ohlsson, A.; McMillan, D.D.; Seshia, M.M.; Canadian Neonatal Network EPIQ Study Group. Reflections on knowledge translation in Canadian NICUs using the EPIQ method. Healthc. Q. 2011, 14, 8–16. [Google Scholar] [CrossRef]
- Al-baghli, F.; Church, P.; Ballantyne, M.; Girardi, A.; Synnes, A. Neonatal follow-up programs in Canada: A national survey. Paediatr. Child Health 2021, 26, e46–e51. [Google Scholar] [CrossRef]
- Proctor, E.; Silmere, H.; Raghavan, R.; Hovmand, P.; Aarons, G.; Bunger, A.; Griffey, R.; Hensley, M. Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Adm. Policy Ment. Health Ment. Health Serv. Res. 2011, 38, 65–76. [Google Scholar] [CrossRef]
- Lui, K.; Vento, M.; Modi, N.; Kusuda, S.; Lehtonen, L.; Håkansson, S.; Rusconi, F.; Bassler, D.; Reichman, B.; Yang, J.; et al. Inter-center variability in neonatal outcomes of preterm infants: A longitudinal evaluation of 298 neonatal units in 11 countries. Semin. Fetal Neonatal Med. 2021, 26, 101196. [Google Scholar] [CrossRef]
- Orton, J.; Spittle, A.; Doyle, L.; Anderson, P.; Boyd, R. Do early intervention programmes improve cognitive and motor outcomes for preterm infants after discharge? A systematic review. Dev. Med. Child Neurol. 2009, 51, 851–859. [Google Scholar] [CrossRef] [PubMed]
- Nordhov, S.M.; Rønning, J.A.; Ulvund, S.E.; Dahl, L.B.; Kaaresen, P.I. Early intervention improves behavioral outcomes for preterm infants: Randomized controlled trial. Pediatrics 2012, 129, e9–e16. [Google Scholar] [CrossRef] [PubMed]
- Ravn, I.H.; Smith, L.; Lindemann, R.; Smeby, N.A.; Kyno, N.M.; Bunch, E.H.; Sandvik, L. Effect of early intervention on social interaction between mothers and preterm infants at 12 months of age: A randomized controlled trial. Infant. Behav. 2011, 34, 215–225. [Google Scholar] [CrossRef] [PubMed]

| Site and Size | Aim 1 | Aim 2 | Aim 3 | Aim 4 | Aim 5 | Aim 6 | Aim 7 | |
|---|---|---|---|---|---|---|---|---|
| 1 Large | Aim | Improve NFU staff knowledge of importance of parent–infant interaction for language Development with >85% of NFU team attending a workshop and scoring ≥90% on post-test * | Increase knowledge of parental perceptions of early language development for preterm infants and elicit parent input on facilitators/ barriers to participation in language development activities with 10 parent interviews | Create a “Language Passport” brochure for NICU parents with information about how to stimulate early language development in NICU | Validate and improve “Language passport” by receiving feedback from >10 NICU parents | >70% of NICU families report using > 1 language-building activity > three times per week in the NICU | >50% of NICU families report using > 1 language-building activity > three times/week post-NICU discharge | Reduce from 44% to 40% NICU families who report not having been talked to about early language development |
| Audit results | 15/23 (65%) attended; 15/15 scored >90% | 13 interviews; detailed qualitative data obtained | Passport created in two languages AND video created | 14 parents provided feedback | 86% | 24/27 (89%) | Improved greatly but audit not completed | |
| 2 Medium | Aim | 80% of Parent-EPIQ team to be trained in EPIQ workshop using the planned project | 70% of NICU nurses complete education module about reading to babies in NICU | Include nurturing moments (parents reading, talking, singing to babies) to the Voyage to Home parent card as standard of care | 100% of NICU single rooms to have a book bags on admission; pamphlet of baby songs created | Increase nurturing moments (reading, talking, singing to babies) to 1 hr/day during 70% of skin-to-skin care | 90% of NICU staff trained in SENSE program | Implement family education “Limit Screen time & increase Face time awareness” at 4 mo NFU visit |
| Audit results | 80% | 55% | 100% | 100% | Increased from 56% to 64% | Achieved and now standard of care. | Became standard of care | |
| 3 # Medium | Aim | Increase knowledge of importance of early language stimulation in children born prematurely to 100% of NFU staff by watching an information session | Increase awareness of importance of language stimulation in the NICU by NICU staff from 0% to >70% via written and oral communication | Create a parent-centered language enhancement and reading program in the NICU by giving out a reading bag and verbal coaching; assess % of families receiving a reading bag | Incorporate a NFU formal language enhancement program to >90% of visits for premature children | Develop a lending library in the NICU | Start a NICU volunteer Baby Readers Program in the NICU two times per week to read when parents cannot come | |
| Audit results | 100% watched; all scored 100% on test | From four surveys, 48/65 (74%) were aware | 70% received bag and 88% were talked to | Created; 31/32 (97%) received program | Created; 160 books loaned in 11 months | Readers read for 25–52 hrs/month | ||
| 4 # Medium | Aim | Increase knowledge of importance of early language stimulation in children born prematurely to 100% of NFU staff by watching an information session | Improve awareness of the importance of language stimulation in NICU staff and Veteran Parent Program leadership from 0% to 70% via written and oral communication | Create a parent centered language enhancement and reading program in the NICU by giving out a reading bag and verbal coaching to 75% | Incorporate a NFU formal language enhancement program to >90% of visits for premature children | Develop a lending library in the NICU | Start a NICU Baby Readers Program using volunteers | |
| Audit results | 100% watched; all scored 100% on test | 79/90 (88%) aware | 83% received book bag/pamphlets and 76% talked to | 54/54 (100%) received program | Created with 35 books; mean volunteer hrs/mo = 10.5 | Created; mean volunteer hrs/mo = 13 | ||
| 5 Large | Aim | Improve awareness of language delay among NFU clinical staff by 95%; watching an information session and providing a lesson learned | Provide “The Reading Tree” (provided by the local library) to 50% of families who had not previously received it, at 4 mo to 3-year NFU visits | Increase knowledge and awareness of the importance of communication, language development, and stimulation in premature infants by 85% of NICU nurses attending an education session | Create a list of >15 useful tips to support health care professionals in promoting language development | Publish > 13 language improvement tips in the educational Neonatal Program weekly newsletter | ||
| Audit results | 96% attended or watched video | At 240 visits, 49 (20%) already had the book, 176 (73%) received the book, and 15 (6%) did not | 136 (85%) of nurses attended one of six sessions and provided implementation suggestions | 31 tips (207%) created | 16 tips (123%) published | |||
| 6 Large | Aim | Increase % of families watching an approved video on language development at 4-month NFU visit from 0 to 75% | Increase % of families attending music session at 4 or 8-month NFU visit from 0 to 50% | Implement the Read with Me program to 80% of families attending the 4 and 8-month NFU visits | Implement the Read with Me Program to 80% of families during a home visit with a nurse from the Neonatal Transition Team | |||
| Audit results | First mo: 13/17 (76%) watched; second mo: 9/9 (100%) watched | First mo: 44/49 (90%); second mo: 33/37 (89%); parents rated sessions 4.5/5 | 28/31 (90%) received book and information | First mo: 18/19 (95%); 80–100%, subsequently | ||||
| 7 Large | Aim | Improve NFU staff knowledge of importance of parent–infant interaction for language development with >85% of NFU team attending a workshop and scoring ≥90% on post-test * | Increase % of NFU visits post-NICU discharge to 6 months, during which parent–infant interaction is actively discussed to 75% | Increase % of parents aware of mental health issues related to preterm birth from 50 to 90% | Increase % of NFU parents screened for post-partum depression from 0 to 75% | |||
| Audit results | 15/17 (88%); all scored >90% | 80% | Did not get buy-in from entire team | Roll-out halted due to COVID-19 | ||||
| 8 Small | Aim | 100% of NFU staff attend an interactive workshop on community support and resources for cognitive and language development | Create standardized language development checklists for 4, 8, 12, 18, 24, and 36-month NFU visits | Implement checklists and parent language support information sheets | Book bag (book and library information) gifting at 4 or 8-month visit | |||
| Audit results | 100% attendance | Created | Implemented; estimated 75% uptake by staff | 100% of families received a bag | ||||
| 9 Small | Aim | Improve NFU staff knowledge of importance of parent–infant interaction for language development with >85% of NFU team attending a workshop and scoring ≥90% on post-test * | Increase the number of parental reading behaviors from <1 to ≥3 | Increase in % of parents aware of community resources to promote literacy from 0 to 70% | ||||
| Audit results | 5/6 (83%); all scored >90% | 86%; 100% aware of importance of reading, singing, and talking | 80% received pamphlet | |||||
| 10 Small | Aim | Increase % of parents who reported reading to their babies in NICU from 0 to 80% using a Welcome Baby Bundle | Increase % of NICU staff who engaged parents in discussion about reading, talking, or singing to baby to 80% | |||||
| Audit results | Baseline: 3/11 (27%) After: 7/8 (88%) | Baseline: 4/11 (36%) After: 5/8 (63%) |
| Question | Response |
|---|---|
| Yes (9/9) |
| Yes (8/9) |
| Yes (7/8) |
| No—(5/9) Yes—(3/9) Do not Know—(1/9) |
| Yes (9/9) |
| Mean 1.2 |
| Mean 1.8 |
| Yes (6/9) |
| Yes (7/9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Synnes, A.; Luu, T.M.; Afifi, J.; Khairy, M.; de Cabo, C.; Moddemann, D.; Hendson, L.; Reichert, A.; Coughlin, K.; Nguyen, K.A.; et al. Parent-Integrated Interventions to Improve Language Development in Children Born Very Preterm. Children 2023, 10, 953. https://doi.org/10.3390/children10060953
Synnes A, Luu TM, Afifi J, Khairy M, de Cabo C, Moddemann D, Hendson L, Reichert A, Coughlin K, Nguyen KA, et al. Parent-Integrated Interventions to Improve Language Development in Children Born Very Preterm. Children. 2023; 10(6):953. https://doi.org/10.3390/children10060953
Chicago/Turabian StyleSynnes, Anne, Thuy Mai Luu, Jehier Afifi, May Khairy, Cecilia de Cabo, Diane Moddemann, Leonora Hendson, Amber Reichert, Kevin Coughlin, Kim Anh Nguyen, and et al. 2023. "Parent-Integrated Interventions to Improve Language Development in Children Born Very Preterm" Children 10, no. 6: 953. https://doi.org/10.3390/children10060953
APA StyleSynnes, A., Luu, T. M., Afifi, J., Khairy, M., de Cabo, C., Moddemann, D., Hendson, L., Reichert, A., Coughlin, K., Nguyen, K. A., Richter, L. L., Bacchini, F., & Aziz, K. (2023). Parent-Integrated Interventions to Improve Language Development in Children Born Very Preterm. Children, 10(6), 953. https://doi.org/10.3390/children10060953






