NeoCheck: A New Checklist to Assess Performance during Newborn Life Support—A Validation Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Scenario Development
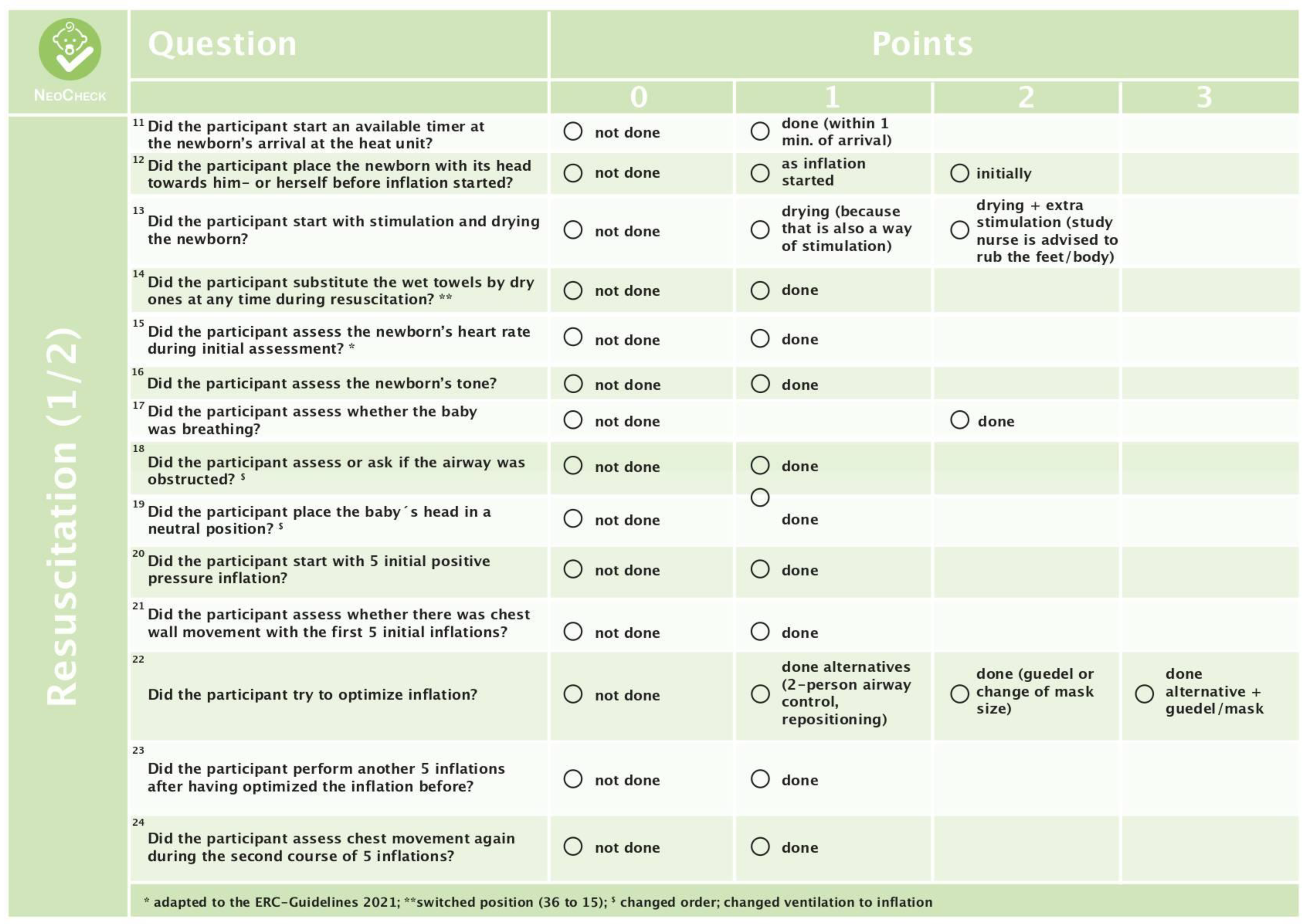
2.3. Checklist Development
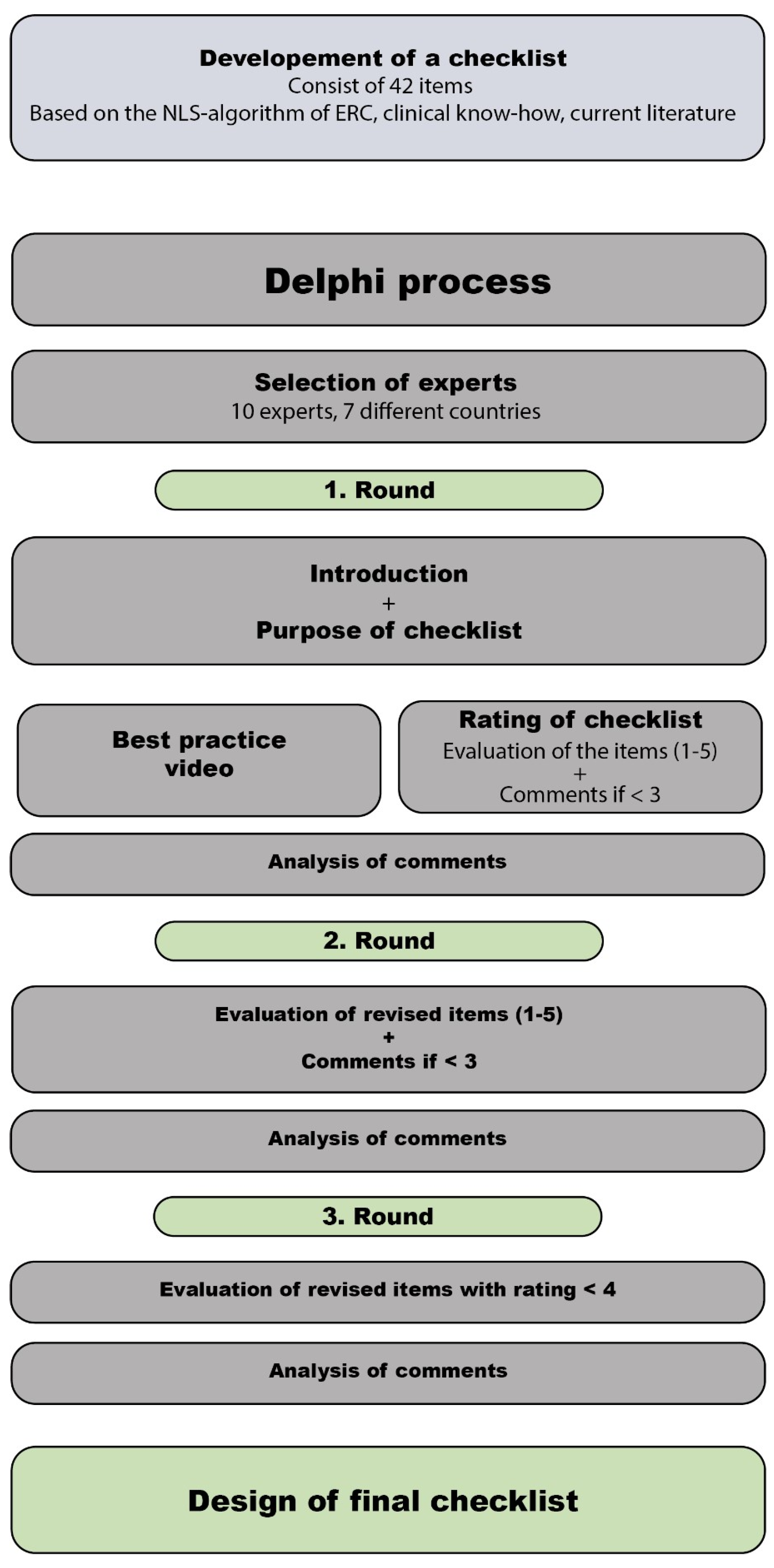
2.4. Delphi Process
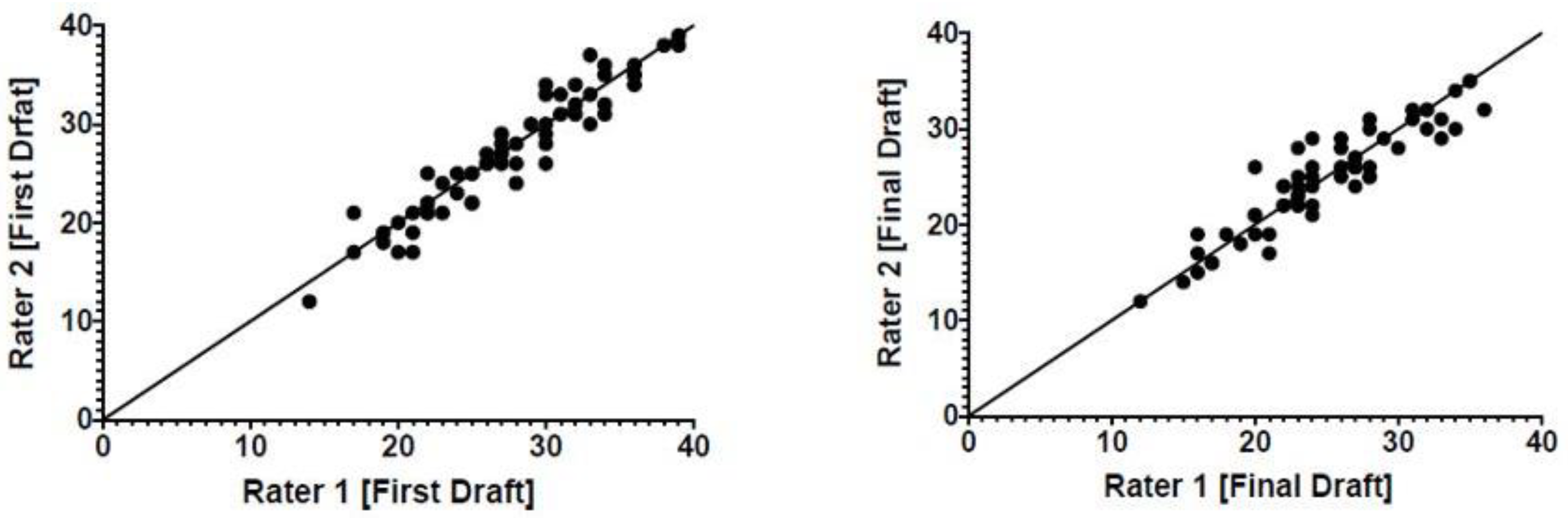
2.5. Reliability
2.6. Data Analysis
3. Results
3.1. Delphi Process
3.2. Reliability
4. Discussion
4.1. Validity
4.2. Reliability
4.3. The Checklist
4.4. Adaptation to 2021 ERC NLS Guidelines
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix



References
- Madar, J.; Roehr, C.C.; Ainsworth, S.; Ersdal, H.; Morley, C.; Rudiger, M.; Skare, C.; Szczapa, T.; Te Pas, A.; Trevisanuto, D.; et al. European Resuscitation Council Guidelines 2021: Newborn resuscitation and support of transition of infants at birth. Resuscitation 2021, 161, 291–326. [Google Scholar] [CrossRef]
- Mileder, L.P.; Urlesberger, B.; Szyld, E.G.; Roehr, C.C.; Schmölzer, G.M. Simulation-based neonatal and infant resuscitation teaching: A systematic review of randomized controlled trials. Klin. Padiatr. 2014, 226, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Yucel, C.; Hawley, G.; Terzioglu, F.; Bogossian, F. The Effectiveness of Simulation-Based Team Training in Obstetrics Emergencies for Improving Technical Skills: A Systematic Review. Simul. Healthc. 2020, 15, 98–105. [Google Scholar] [CrossRef] [PubMed]
- Escobedo, M.B.; Aziz, K.; Kapadia, V.S.; Lee, H.C.; Niermeyer, S.; Schmolzer, G.M.; Szyld, E.; Weiner, G.M.; Wyckoff, M.H.; Yamada, N.K.; et al. 2019 American Heart Association Focused Update on Neonatal Resuscitation: An Update to the American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics 2020, 145, e20191362. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Herce, J.; Carrillo, A.; Urbano, J.; Manrique, G.; Mencia, Y.S.; y Grupo Madrileño de Cuidados Intensivos Pediátricos. Evaluation of the pediatric life support instructors courses. BMC Med. Educ. 2021, 21, 71. [Google Scholar] [CrossRef]
- Carbine, D.N.; Finer, N.N.; Knodel, E.; Rich, W. Video recording as a means of evaluating neonatal resuscitation performance. Pediatrics 2000, 106, 654–658. [Google Scholar] [CrossRef]
- Wagner, M.; Bibl, K.; Hrdliczka, E.; Steinbauer, P.; Stiller, M.; Gropel, P.; Goeral, K.; Salzer-Muhar, U.; Berger, A.; Schmolzer, G.M.; et al. Effects of Feedback on Chest Compression Quality: A Randomized Simulation Study. Pediatrics 2019, 143, e20182441. [Google Scholar] [CrossRef]
- Wagner, M.; Gropel, P.; Bibl, K.; Olischar, M.; Auerbach, M.A.; Gross, I.T. Eye-tracking during simulation-based neonatal airway management. Pediatr. Res. 2020, 87, 518–522. [Google Scholar] [CrossRef]
- Clyne, B.; Smith, J.L.; Napoli, A.M. Influence of clinical experience and productivity on emergency medicine faculty teaching scores. J. Grad. Med. Educ. 2012, 4, 434–437. [Google Scholar] [CrossRef]
- Thomas, E.J.; Sexton, J.B.; Lasky, R.E.; Helmreich, R.L.; Crandell, D.S.; Tyson, J. Teamwork and quality during neonatal care in the delivery room. J. Perinatol. 2006, 26, 163–169. [Google Scholar] [CrossRef]
- Rovamo, L.; Mattila, M.M.; Andersson, S.; Rosenberg, P. Assessment of newborn resuscitation skills of physicians with a simulator manikin. Arch. Dis. Child. Fetal Neonatal Ed. 2011, 96, F383–F389. [Google Scholar] [CrossRef] [PubMed]
- Lockyer, J.; Singhal, N.; Fidler, H.; Weiner, G.; Aziz, K.; Curran, V. The development and testing of a performance checklist to assess neonatal resuscitation megacode skill. Pediatrics 2006, 118, e1739–e1744. [Google Scholar] [CrossRef] [PubMed]
- van der Heide, P.A.; van Toledo-Eppinga, L.; van der Heide, M.; van der Lee, J.H. Assessment of neonatal resuscitation skills: A reliable and valid scoring system. Resuscitation 2006, 71, 212–221. [Google Scholar] [CrossRef]
- Wyllie, J.; Bruinenberg, J.; Roehr, C.C.; Rudiger, M.; Trevisanuto, D.; Urlesberger, B. European Resuscitation Council Guidelines for Resuscitation 2015: Section 7. Resuscitation and support of transition of babies at birth. Resuscitation 2015, 95, 249–263. [Google Scholar] [CrossRef]
- Goodman, C.M. The Delphi technique: A critique. J. Adv. Nurs. 1987, 12, 729–734. [Google Scholar] [CrossRef]
- Wagner, M.; Jaki, C.; Löllgen, R.M.; Mileder, L.; Eibensteiner, F.; Ritschl, V.; Steinbauer, P.; Gottstein, M.; Abulebda, K.; Calhoun, A.; et al. Readiness for and Response to Coronavirus Disease 2019 Among Pediatric Healthcare Providers: The Role of Simulation for Pandemics and Other Disasters. Pediatr. Crit. Care Med. 2020, 22, e333–e338. [Google Scholar] [CrossRef] [PubMed]
- Morgan, P.J.; Lam-McCulloch, J.; Herold-McIlroy, J.; Tarshis, J. Simulation performance checklist generation using the Delphi technique. Can. J. Anaesth. 2007, 54, 992–997. [Google Scholar] [CrossRef] [PubMed]
- Johnston, L.; Sawyer, T.; Nishisaki, A.; Whitfill, T.; Ades, A.; French, H.; Glass, K.; Dadiz, R.; Bruno, C.; Levit, O.; et al. Neonatal Intubation Competency Assessment Tool: Development and Validation. Acad. Pediatr. 2019, 19, 157–164. [Google Scholar] [CrossRef]
- Schmutz, J.; Eppich, W.J.; Hoffmann, F.; Heimberg, E.; Manser, T. Five steps to develop checklists for evaluating clinical performance: An integrative approach. Acad. Med. 2014, 89, 996–1005. [Google Scholar] [CrossRef]
- Banayan, J.; Blood, A.; Park, Y.S.; Shahul, S.; Scavone, B.M. A modified Delphi method to create a scoring system for assessing team performance during maternal cardiopulmonary arrest. Hypertens. Pregnancy 2015, 34, 314–331. [Google Scholar] [CrossRef]
- Bauernfeind, B.; Aringer, M.; Prodinger, B.; Kirchberger, I.; Machold, K.; Smolen, J.; Stamm, T. Identification of relevant concepts of functioning in daily life in people with systemic lupus erythematosus: A patient Delphi exercise. Arthritis Rheum. 2009, 61, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Hartman, N.; Wittler, M.; Askew, K.; Manthey, D. Delphi Method Validation of a Procedural Performance Checklist for Insertion of an Ultrasound-Guided Internal Jugular Central Line. Am. J. Med. Qual. 2016, 31, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Linz, M. Scenarios for the aviation industry: A Delphi-based analysis for 2025. J. Air Transp. Manag. 2012, 22, 28–35. [Google Scholar] [CrossRef]
- Clayton, M.J. Delphi: A technique to harness expert opinion for critical decision-making tasks in education. Educ. Psychol. 1997, 17, 373–386. [Google Scholar] [CrossRef]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef] [PubMed]
- Ersdal, H.L.; Linde, J.; Mduma, E.; Auestad, B.; Perlman, J. Neonatal outcome following cord clamping after onset of spontaneous respiration. Pediatrics 2014, 134, 265–272. [Google Scholar] [CrossRef]
- O’Donnell, C.P.; Kamlin, C.O.; Davis, P.G.; Carlin, J.B.; Morley, C.J. Clinical assessment of infant colour at delivery. Arch. Dis. Child. Fetal Neonatal Ed. 2007, 92, F465–F467. [Google Scholar] [CrossRef]
- Hunziker, S.; Johansson, A.C.; Tschan, F.; Semmer, N.K.; Rock, L.; Howell, M.D.; Marsch, S. Teamwork and Leadership in Cardiopulmonary Resuscitation. J. Am. Coll. Cardiol. 2011, 57, 2381–2388. [Google Scholar] [CrossRef]
- Yamada, N.K.; Halamek, L.P. On the need for precise, concise communication during resuscitation: A proposed solution. J. Pediatr. 2015, 166, 184–187. [Google Scholar] [CrossRef]
| Number of Comments Review 1 | Number of Comments Review 2 | |
|---|---|---|
| Limitation due to simulation setting | 8 (7.7%) | 6 (15.0%) |
| Language/Grammar | 35 (33.7%) | 21 (51.2%) |
| Comprehensiveness | 11 (10.6%) | 1 (2.4%) |
| Content | 36 (34.6%) | 10 (24.4%) |
| Structure | 2 (1.9%) | 2 (4.9%) |
| Redundancy | 12 (11.5%) | 1 (2.4%) |
| Total | 104 | 41 |
| Question | Mean Rating | Reason for Elimination |
|---|---|---|
| Did the participant apply additional oxygen? | 4.10 | Lack of evidence in the current literature |
| Did the participant assess the baby’s colour? | 3.35 | Rating < 4, lack of importance in NLS, limitations in a simulated setting |
| Did the participant initiate to administer fluid? | 3.90 | Rating < 4, given the history of abruption of the placenta, may be important, but not in a general NLS scenario |
| Did the participant give verbal concerns about the decreasing heart rate? | 4.35 | Limitations due to simulation setting, the nurse leaving the room somewhat unrealistic |
| Did the participant call the nurse back to the resuscitation unit? | 3.90 | Rating < 4, Limitations due to simulation setting, the nurse leaving the room somewhat unrealistic |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bibl, K.; Eibensteiner, F.; Ritschl, V.; Steinbauer, P.; Berger, A.; Olischar, M.; Giordano, V.; Wagner, M. NeoCheck: A New Checklist to Assess Performance during Newborn Life Support—A Validation Study. Children 2023, 10, 1013. https://doi.org/10.3390/children10061013
Bibl K, Eibensteiner F, Ritschl V, Steinbauer P, Berger A, Olischar M, Giordano V, Wagner M. NeoCheck: A New Checklist to Assess Performance during Newborn Life Support—A Validation Study. Children. 2023; 10(6):1013. https://doi.org/10.3390/children10061013
Chicago/Turabian StyleBibl, Katharina, Felix Eibensteiner, Valentin Ritschl, Philipp Steinbauer, Angelika Berger, Monika Olischar, Vito Giordano, and Michael Wagner. 2023. "NeoCheck: A New Checklist to Assess Performance during Newborn Life Support—A Validation Study" Children 10, no. 6: 1013. https://doi.org/10.3390/children10061013
APA StyleBibl, K., Eibensteiner, F., Ritschl, V., Steinbauer, P., Berger, A., Olischar, M., Giordano, V., & Wagner, M. (2023). NeoCheck: A New Checklist to Assess Performance during Newborn Life Support—A Validation Study. Children, 10(6), 1013. https://doi.org/10.3390/children10061013







