Therapeutic Strategies of Primary Molar Infraocclusion: A Systematic Review
Abstract
1. Introduction
1.1. Incidence and Etiology
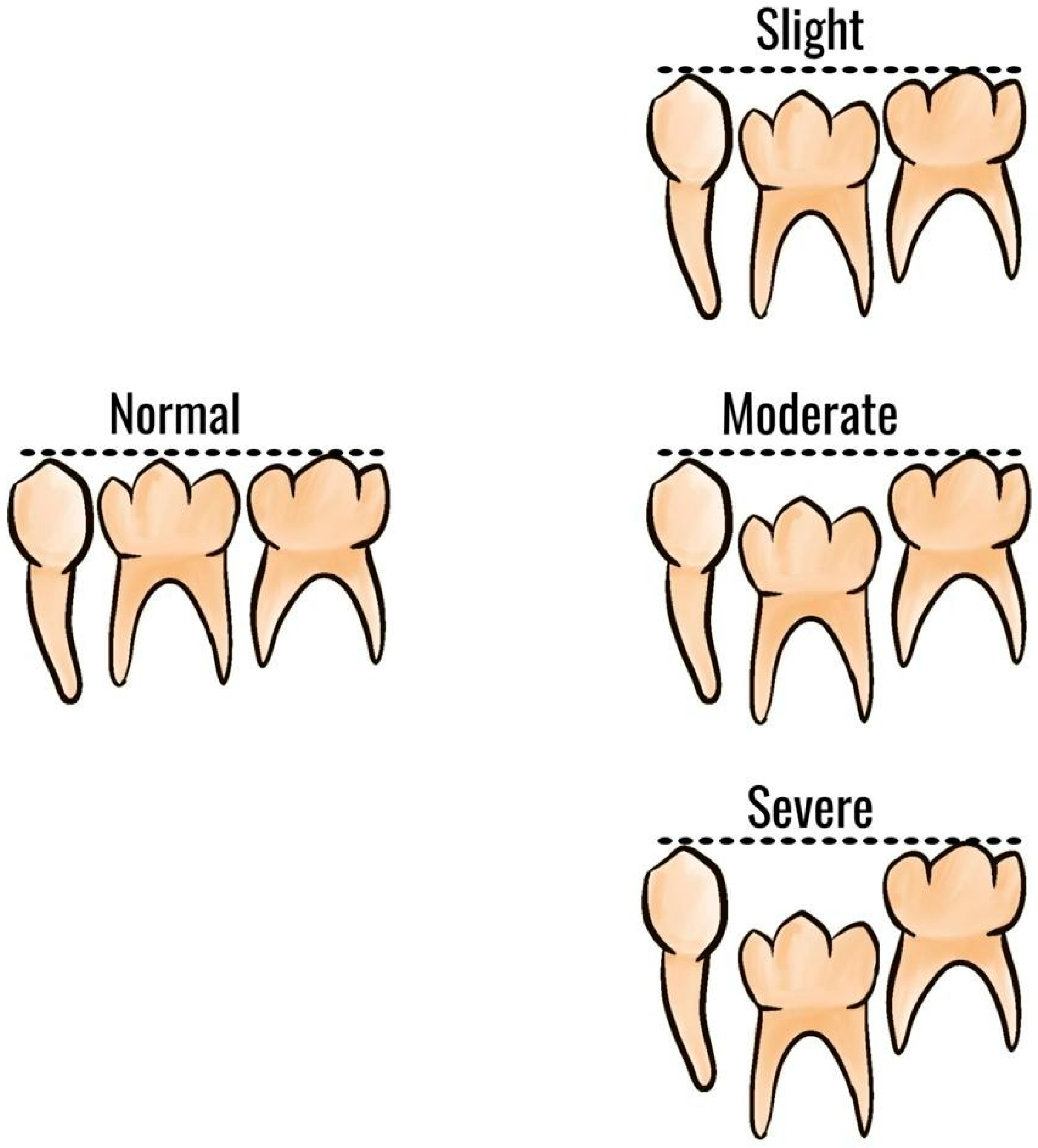
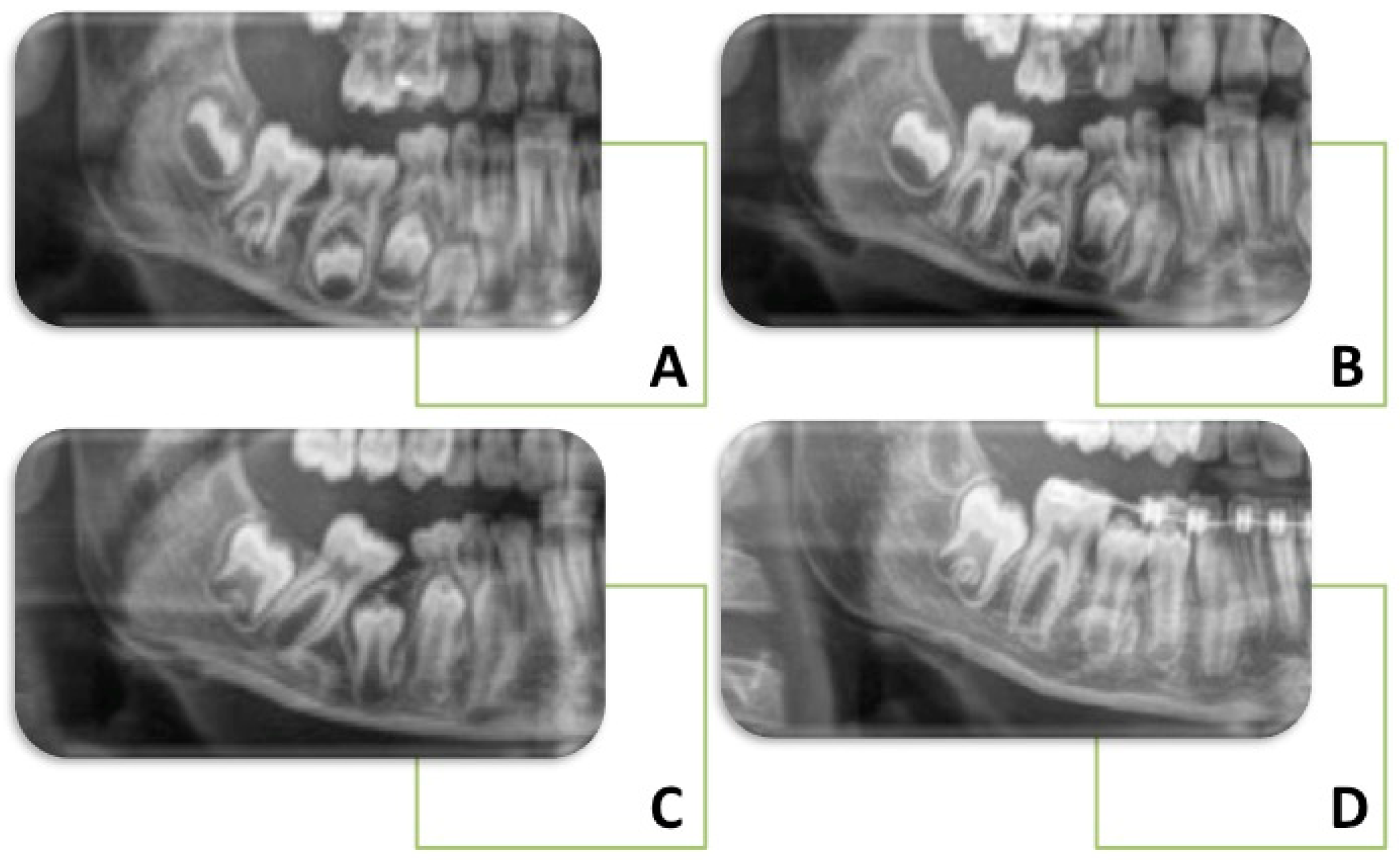
1.2. Clinical Features and Diagnosis
1.3. Orthodontic Implications
2. Materials and Methods
3. Results
General Characteristics of the Articles Included
4. Discussion
4.1. Interpretation of the Results
4.1.1. Infraocclusion of Primary Molars
- Phase 1—migration period (from tooth bud to early root formation). Two conditions can be encountered:
- ○
- Ankylosed deciduous molars are extracted as soon as diagnosed. Sometimes, premolars tooth germs are extracted. If they are not extracted, the permanent crown can be malformed;
- ○
- Not ankylosed deciduous molars are extracted when root development of the premolars has begun. Premolars should be monitored and, if feasible, saved.
- Phase 2 (the period before the premolar penetrates the gingiva). There were two possible scenarios:
- ○
- Abnormal premolar eruption and absence of primary molars exfoliation. Unclear are the causes behind the retained primary molars. There are only assumptions such as:
- ▪
- Segmental bone dysplasia, in which premolar eruption is delayed → primary molars should be removed once premolar eruptive movements have begun;
- ▪
- Ectoderm deviations → extraction of primary molars before root closure of premolars.
- ○
- Abnormal premolar eruption after extraction of primary molars. If, for example, there were root resorptions of the permanent root, with repair attempts or a prolonged eruption stop, the ankylosed premolars could not erupt and were therefore extracted.
- Phase 3 (premolar eruption after penetration of gingiva). Premolars ankylosed could be observed. The cause is generally attributed to resorption of the permanent periodontal membrane due to malfunction in the peripheral nerve tissue (genetically determined or caused by virus attacks) or primary failure of tooth eruption (PFE) (defect in the receptor for parathyroid hormone, PTH1R). Surgery might be the only treatment and, in very few cases, orthodontic treatment.
4.1.2. Association between Infraocclusion of Deciduous Molars and Other Conditions
Ankylosis
Hypophosphatasia
Hypodontia
- No crowding with Angle Class I occlusion, normal overbite, and overjet with the primary molar in overall good condition;
- Vertical deep bite, no crowding, mandibular clockwise rotation, and incompatible growth pattern with extractions, no or minor primary molars infraocclusion, root resorption less than half of the root, and no caries or fillings of these elements. Preservation of the primary molars may be a good option with long-term stability;
- Augmented overbite, reduced lower facial height, retroclination of the lower incisors, ipodivergence, and no crowding in the lower arch.
- Severe issues such as root resorption, infraocclusion, and decays of the roots of the second primary molar (at ages 10–11 years);
- Crowding with mesial tipping of the first mandibular molar, normal or minimal overbite, Angle Class I occlusion, regular growth pattern, and normal incisal inclination. In addition, consider extraction of the remaining three second premolars.
- Fixed orthodontics space closure, also with TADs aid;
- Spontaneous mesialisation of permanent molars: Between the age of 8–9 years, before the extraction of the second deciduous molar, slicing and then hemisection of its crown is advised. In this way, there is a controlled mesialization of the first permanent molar, avoiding crown tipping, especially if the extraction is performed after the completed root development of the first permanent molar;
- Dental element autotransplantation when the space closing is challenging or impossible. It has been seen that the maxillary third molar is an excellent candidate for insertion at the level of the mandibular second deciduous molar;
- Placement of an implant and prosthetic crown. This is a choice to be made when alveolar bone development has been completed (age > 20 years) because the implant blocks the growth of the alveolar process;
- Fixed prosthesis: such as implants. This option interferes with alveolar bone growth.
4.2. Limitations of the Evidence Included in the Review
4.3. Implications of the Results for Practice, Policy, and Future Research
5. Conclusions
- The cause of infraoccluded deciduous molars is not fully understood, and the best resolution approach has yet to be determined [48];
- Early diagnosis of infraoccluded primary elements is fundamental and cannot be postponed [56];
- Preservation of the primary molars may be a valid option with long-term stability if there is no or moderate primary molar infraocclusion, root resorption of less than half of the root, and no decays or restoration [52];
- Good clinical situations for early extractions: class I, crowding, normal OVB, and OVJ, normal intermaxillary relation, normal incisor inclination;
- Primary molars preservation in case of delayed extractions after 12–13 years; diastemas; no or minor infraocclusion; no caries or filling; vertical deep bite cases; class III tendency or plane mandibular angle; root resorption < than half of the root.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| C. R. | Case Report |
| L. O. S. | Longitudinal observational study |
| F. | Female |
| M. | Male |
| CBCT | Cone Beam Computed Tomography |
| OPG | Orthopantomography |
| OVB | Overbite |
| OVJ | Overjet |
| TAD | Temporary Anchorage Devices |
References
- Doğramacı, E.; Rossi-Fedele, G. Infraposition or Infraocclusion- Is It Time to Rename? Dent. Traumatol. 2021, 37, 813–814. [Google Scholar] [CrossRef]
- Caliskan, S.; Tuloglu, N.; Celik, O.; Ozdemir, C.; Kizilaslan, S.; Bayrak, S. A Pilot Study of a Deep Learning Approach to Submerged Primary Tooth Classification and Detection. Int. J. Comput Dent. 2021, 24, 1–9. [Google Scholar] [CrossRef]
- Murtaugh, J. Submerged Primary Molars. J. Am. Dent. Assoc. 2013, 144, 978. [Google Scholar] [CrossRef]
- Sella Tunis, T.; Sarne, O.; Hershkovitz, I.; Finkelstein, T.; Pavlidi, A.M.; Shapira, Y.; Davidovitch, M.; Shpack, N. Dental Anomalies’ Characteristics. Diagnostics 2021, 11, 1161. [Google Scholar] [CrossRef] [PubMed]
- Halterman, C. Ankylosed primary molars. J. Am. Dent. Assoc. 2013, 144, 975. [Google Scholar] [CrossRef]
- Kurol, J. Infraocclusion of Primary Molars: An Epidemiologic and Familial Study. Commun. Dent. Oral. Epidemiol. 1981, 9, 94–102. [Google Scholar] [CrossRef]
- Odeh, R.; Mihailidis, S.; Townsend, G.; Lähdesmäki, R.; Hughes, T.; Brook, A. Prevalence of Infraocclusion of Primary Molars Determined Using a New 2D Image Analysis Methodology. Aust. Dent. J. 2016, 61, 183–189. [Google Scholar] [CrossRef] [PubMed]
- Via, W.F. Submerged deciduous molars: Familial tendencies. J. Am. Dent. Assoc. 1964, 69, 127–129. [Google Scholar] [CrossRef] [PubMed]
- Lanteri, V.; Maspero, C.; Cavone, P.; Marchio, V.; Farronato, M. Relationship between Molar Deciduous Teeth Infraocclusion and Mandibular Growth: A Case-Control Study. Eur. J. Paediatr. Dent. 2020, 21, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Arhakis, A.; Boutiou, E. Etiology, Diagnosis, Consequences and Treatment of Infraoccluded Primary Molars. Open Dent. J. 2016, 10, 714–719. [Google Scholar] [CrossRef]
- Bjerklin, K. Orthodontic Management of Agenesis of Mandibular Second Premolars. APOS 2019, 9, 206–210. [Google Scholar] [CrossRef]
- Baccetti, T. Tooth Anomalies Associated with Failure of Eruption of First and Second Permanent Molars. Am. J. Orthod. Dentofacial. Orthop. 2000, 118, 608–610. [Google Scholar] [CrossRef] [PubMed]
- Tieu, L.D.; Walker, S.L.; Major, M.P.; Flores-Mir, C. Management of Ankylosed Primary Molars with Premolar Successors: A Systematic Review. J. Am. Dent. Assoc. 2013, 144, 602–611. [Google Scholar] [CrossRef] [PubMed]
- Pasciuti, E.; Coloccia, G.; Inchingolo, A.D.; Patano, A.; Ceci, S.; Bordea, I.R.; Cardarelli, F.; Venere, D.D.; Inchingolo, F.; Dipalma, G. Deep Bite Treatment with Aligners: A New Protocol. Appl. Sci. 2022, 12, 6709. [Google Scholar] [CrossRef]
- Odeh, R.; Townsend, G.; Mihailidis, S.; Lähdesmäki, R.; Hughes, T.; Brook, A. Infraocclusion: Dental Development and Associated Dental Variations in Singletons and Twins. Arch. Oral. Biol. 2015, 60, 1394–1402. [Google Scholar] [CrossRef]
- Alshaya, S.I.; Alanazi, A.F.; Aldawish, S.S.; Alsuhaim, M.M.; Alomar, M.S.; Almuaytiq, Y.M.; Alfahad, S.A.; Almousa, A.A.S.; Alassaf, A.; Mallineni, S.K. Infraocclusion: Prevalence, Characteristics, and Associated Dental Anomalies in Arabian Children. Biomed. Res. Int. 2022, 2022, 6624804. [Google Scholar] [CrossRef]
- Dewhurst, S.N.; Harris, J.C.; Bedi, R. Infraocclusion of Primary Molars in Monozygotic Twins: Report of Two Cases. Int. J. Paediatr. Dent. 1997, 7, 25–30. [Google Scholar] [CrossRef]
- Jenkins, F.R.; Nichol, R.E. Atypical Retention of Infraoccluded Primary Molars with Permanent Successor Teeth. Eur. Arch. Paediatr. Dent. 2008, 9, 51–55. [Google Scholar] [CrossRef]
- Brearley, L.J.; McKibben, D.H. Ankylosis of Primary Molar Teeth. I. Prevalence and Characteristics. ASDC J. Dent. Child 1973, 40, 54–63. [Google Scholar]
- Patano, A.; Cardarelli, F.; Montenegro, V.; Ceci, S.; Inchingolo, A.D.; Semjonova, A.; Palmieri, G.; Di Pede, C.; Mancini, A.; Maggiore, M.E.; et al. Early Functional Orthodontic Treatment of Bad Oral Habits with AMCOP® Bio-Activators. J. Biol. Regul. Homeost. Agents 2022, 36, 91–110. [Google Scholar]
- Tong, A.; Chow, Y.-L.; Xu, K.; Hardiman, R.; Schneider, P.; Tan, S.-S. Transcriptome Analysis of Ankylosed Primary Molars with Infraocclusion. Int. J. Oral. Sci. 2020, 12, 7. [Google Scholar] [CrossRef]
- Farronato, M.; Farronato, D.; Giannì, A.B.; Inchingolo, F.; Nucci, L.; Tartaglia, G.M.; Maspero, C. Effects on Muscular Activity after Surgically Assisted Rapid Palatal Expansion: A Prospective Observational Study. Bioengineering 2022, 9, 361. [Google Scholar] [CrossRef] [PubMed]
- Suprabha, B.S.; Pai, S.M. Ankylosis of Primary Molar along with Congenitally Missing First Permanent Molar. J. Indian. Soc. Pedod. Prev. Dent. 2006, 24 (Suppl. S1), S35–S37. [Google Scholar] [PubMed]
- Albers, D.D. Ankylosis of Teeth in the Developing Dentition. Quintessence Int. 1986, 17, 303–308. [Google Scholar]
- Inchingolo, A.D.; Ceci, S.; Patano, A.; Inchingolo, A.M.; Montenegro, V.; Di Pede, C.; Malcangi, G.; Marinelli, G.; Coloccia, G.; Garibaldi, M.; et al. Elastodontic Therapy of Hyperdivergent Class II Patients Using AMCOP® Devices: A Retrospective Study. Appl. Sci. 2022, 12, 3259. [Google Scholar] [CrossRef]
- McGeown, M.; O’Connell, A. Management of Primary Molar Infraocclusion in General Practice. J. Ir. Dent. Assoc. 2014, 60, 192–198. [Google Scholar] [PubMed]
- Eşian, D.; Bica, C.I.; Stoica, O.E.; Dako, T.; Vlasa, A.; Bud, E.S.; Salcudean, D.; Beresescu, L. Prevalence and Manifestations of Dental Ankylosis in Primary Molars Using Panoramic X-Rays: A Cross-Sectional Study. Children 2022, 9, 1188. [Google Scholar] [CrossRef]
- Malcangi, G.; Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Garibaldi, M.; Inchingolo, A.M.; Piras, F.; Cardarelli, F.; Settanni, V.; et al. Impacted Central Incisors in the Upper Jaw in an Adolescent Patient: Orthodontic-Surgical Treatment—A Case Report. Appl. Sci. 2022, 12, 2657. [Google Scholar] [CrossRef]
- Tian, X.; Yuan, G.H. Etiology, diagnosis and treatment of infraoccluded primary second molars. Zhonghua Kou Qiang Yi Xue Za Zhi 2022, 57, 192–195. [Google Scholar] [CrossRef]
- Shalish, M.; Har-Zion, G.; Zini, A.; Harari, D.; Chaushu, S. Deep Submersion: Severe Phenotype of Deciduous-Molar Infraocclusion with Biological Associations. Angle. Orthod. 2014, 84, 292–296. [Google Scholar] [CrossRef]
- Ekim, S.L.; Hatibovic-Kofman, S. A Treatment Decision-Making Model for Infraoccluded Primary Molars. Int. J. Paediatr. Dent. 2001, 11, 340–346. [Google Scholar] [CrossRef]
- Kurol, J.; Thilander, B. Infraocclusion of Primary Molars and the Effect on Occlusal Development, a Longitudinal Study. Eur. J. Orthod. 1984, 6, 277–293. [Google Scholar] [CrossRef] [PubMed]
- Hvaring, C.L.; Øgaard, B.; Stenvik, A.; Birkeland, K. The Prognosis of Retained Primary Molars without Successors: Infraocclusion, Root Resorption and Restorations in 111 Patients. Eur. J. Orthod. 2014, 36, 26–30. [Google Scholar] [CrossRef] [PubMed]
- Cardoso Silva, C.; Maroto Edo, M.; Soledad Alvaro Llorente, M.; Barbería Leache, E. Primary Molar Infraocclusion: Frequency, Magnitude, Root Resorption and Premolar Agenesis in a Spanish Sample. Eur. J. Paediatr. Dent. 2014, 15, 258–264. [Google Scholar] [PubMed]
- Lin, S.; Ashkenazi, M.; Karawan, M.; Teich, S.T.; Gutmacher, Z. Management of Ankylotic Root Resorption Following Dental Trauma: A Short Review and Proposal of a Treatment Protocol. Oral. Health Prev. Dent. 2017, 15, 467–474. [Google Scholar] [CrossRef]
- Inchingolo, A.M.; Malcangi, G.; Ferrara, I.; Viapiano, F.; Netti, A.; Buongiorno, S.; Latini, G.; Azzollini, D.; De Leonardis, N.; de Ruvo, E.; et al. Laser Surgical Approach of Upper Labial Frenulum: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 1302. [Google Scholar] [CrossRef] [PubMed]
- Spinas, E.; Aresu, M.; Canargiu, F.; Giannetti, L. Preventive Treatment of Post-Traumatic Dental Infraocclusion: Study on the Knowledge of Dental Decoronation in a Sample of Italian Dental Students and Dentists. Eur. J. Paediatr. Dent. 2015, 16, 279–283. [Google Scholar]
- Peretz, B.; Absawi-Huri, M.; Bercovich, R.; Amir, E. Inter-Relations between Infraocclusion of Primary Mandibular Molars, Tipping of Adjacent Teeth, and Alveolar Bone Height. Pediatr. Dent. 2013, 35, 325–328. [Google Scholar]
- Calheiros-Lobo, M.J.; Costa, F.; Pinho, T. Infraocclusion Level and Root Resorption of the Primary Molar in Second Premolar Agenesis: A Retrospective Cross-Sectional Study in the Portuguese Population. Dent. Med. Probl. 2022, 59, 195–207. [Google Scholar] [CrossRef]
- Lin, J.C.-Y.; Tsai, S.-J.; Liou, E.J.W.; Bowman, S.J. Treatment of Challenging Malocclusions with Invisalign and Miniscrew Anchorage. J. Clin. Orthod. 2014, 48, 23–36. [Google Scholar]
- Kurol, J.; Koch, G. The Effect of Extraction of Infraoccluded Deciduous Molars: A Longitudinal Study. Am. J. Orthod. 1985, 87, 46–55. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.D.; Carpentiere, V.; Piras, F.; Netti, A.; Ferrara, I.; Campanelli, M.; Latini, G.; Viapiano, F.; Costa, S.; Malcangi, G.; et al. Orthodontic Surgical Treatment of Impacted Mandibular Canines: Systematic Review and Case Report. Appl. Sci. 2022, 12, 8088. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Healthcare Interventions: Explanation and Elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Kjær, I. Abnormal Premolar Eruption: Classification, Aetiology, and Treatment Based on a Case Series Study. Eur. Arch. Paediatr. Dent. 2021, 22, 1077–1086. [Google Scholar] [CrossRef]
- Garcovich, D.; Aiuto, R.; Martin, M.A. Space Regaining Made Easy: The Case of a Severely Infraoccluded Primary Molar. Case Rep. Dent. 2019, 2019, e6916839. [Google Scholar] [CrossRef] [PubMed]
- Atia, S.G.; Elton, V.; Woodmason, K. Management of an Incidental Radiographic Finding of a Severely Infraoccluded Primary Molar. Dent. Update 2018, 45, 135–140. [Google Scholar] [CrossRef]
- Nagayama, K.; Ogaya, Y.; Hamada, M.; Okawa, R.; Uzawa, N.; Nakano, K. Severe Dislocation of Mandibular Second Premolar Associated with Deep Ankylosis of Primary Molar. Pediatr. Dent. J. 2022, 32, 116–122. [Google Scholar] [CrossRef]
- Saitoh, I.; Fukumoto, S.; Iwase, Y.; Hayasaki, H.; Yamasaki, Y. Unilateral Open-Bite Caused by an Impacted Primary Molar with Ankylosis: A Case Report. Pediatr. Dent. J. 2017, 27, 147–152. [Google Scholar] [CrossRef]
- Hamada, M.; Okawa, R.; Matayoshi, S.; Ogaya, Y.; Nomura, R.; Uzawa, N.; Nakano, K. Ankylosed Primary Molar in a Japanese Child with Hypophosphatasia. Dent. J. 2020, 9, 3. [Google Scholar] [CrossRef]
- Hvaring, C.L.; Birkeland, K. The Long-Term Fate of Persisting Deciduous Molars and Canines in 42 Patients with Severe Hypodontia: A 12-Year Follow-Up. Eur. J. Orthod. 2019, 42, 581–586. [Google Scholar] [CrossRef]
- Lin, I.P.; Kumchai, H.; AlRejaye, N.; Sun, A.F.; Drizen, K.; Liu, J.L.-J. Interdisciplinary Approach to Treat Patients With Tooth Agenesis: A Case Report. Clin. Adv. Periodontics 2019, 9, 34–46. [Google Scholar] [CrossRef] [PubMed]
- Ng, A.; Ong, D.; Goh, P. Management of a Patient with a Severely Infraoccluded Primary Molar and Hypodontia. Clin. Case Rep. 2022, 10, e6482. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Ferrara, I.; Viapiano, F.; Netti, A.; Campanelli, M.; Buongiorno, S.; Latini, G.; Carpentiere, V.; Ciocia, A.M.; Ceci, S.; et al. Rapid Maxillary Expansion on the Adolescent Patient: Systematic Review and Case Report. Children 2022, 9, 1046. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Patano, A.; Coloccia, G.; Ceci, S.; Inchingolo, A.M.; Marinelli, G.; Malcangi, G.; Di Pede, C.; Garibaldi, M.; Ciocia, A.M.; et al. Treatment of Class III Malocclusion and Anterior Crossbite with Aligners: A Case Report. Medicina 2022, 58, 603. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, A.M.; Malcangi, G.; Costa, S.; Fatone, M.C.; Avantario, P.; Campanelli, M.; Piras, F.; Patano, A.; Ferrara, I.; Di Pede, C.; et al. Tooth Complications after Orthodontic Miniscrews Insertion. Int. J. Environ. Res. Public Health 2023, 20, 1562. [Google Scholar] [CrossRef]
- Ben-Bassat, Y.; Brin, I.; Fuks, A.B. Occlusal Disturbances Resulting from Neglected Submerged Primary Molars. ASDC J. Dent. Child 1991, 58, 129–133. [Google Scholar] [PubMed]

| Articles screening strategy | KEYWORDS: (“infraocclus *” OR “ankylos *” OR “submer *” OR “secondary retention”) AND “molar”. Timespan: from January 2017 up to November 2022. Electronic Databases: PubMed, Scopus, Web of Science. |
| Author, Year | Type | Subject | Main Issue | Treatment | Outcome |
|---|---|---|---|---|---|
| Atia et al., 2018 | C. R. | F., 12 years | Severe infraoccluded upper second deciduous molar with successor | Extraction | Resolution of dental crowding |
| Garcovich et al., 2019 | C. R. | M., 8 years | Severe infraoccluded lower second deciduous molar with successor | Extraction and wait and watch | Premolar spontaneous eruption |
| Hamada et al., 2020 | C. R. | M., 9 years | Mild infraoccluded lower primary molar with the successor | Extraction and wait and watch | Premolar tendency to erupt |
| Hvaring and Birkeland 2019 | L. O. S. | 24 F., 26 M., Average 13.5 years | Slight/mild infraoccluded upper/lower deciduous molar teeth without successor | No extraction | Infraoccluded teeth tend to remain over time |
| Kjær 2021 | C. R.s | n. a. | Phase 1: Ankylosed primary molars Not ankylosed primary molars with successor | Extraction | Premolar tendency to erupt |
| Phase 2: Retained primary molars with successor | Early extraction | Premolar tendency to erupt | |||
| Lin et al., 2019 | C. R. | M., 18 years | Mild infraoccluded upper/lower primary molar without a successor | Extraction | Implant-prosthetic rehabilitation |
| Nagayama et al., 2022 | C. R. | M., 10 years | Severe infraoccluded lower second deciduous molar with the successor | Extraction and wait and watch | n. a. |
| Ng et al., 2022 | C. R. | M., 14 years | Severe infraoccluded lower second deciduous molar with successor | Extraction | Orthodontic treatment for space closure |
| Saitoh et al., 2017 | C. R. | F., 7 years | Severe infraoccluded upper second deciduous molar with successor | Extraction and wait and watch | Premolar spontaneous eruption |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patano, A.; Inchingolo, A.M.; Laudadio, C.; Azzollini, D.; Marinelli, G.; Ceci, S.; Latini, G.; Rapone, B.; Inchingolo, A.D.; Mancini, A.; et al. Therapeutic Strategies of Primary Molar Infraocclusion: A Systematic Review. Children 2023, 10, 582. https://doi.org/10.3390/children10030582
Patano A, Inchingolo AM, Laudadio C, Azzollini D, Marinelli G, Ceci S, Latini G, Rapone B, Inchingolo AD, Mancini A, et al. Therapeutic Strategies of Primary Molar Infraocclusion: A Systematic Review. Children. 2023; 10(3):582. https://doi.org/10.3390/children10030582
Chicago/Turabian StylePatano, Assunta, Angelo Michele Inchingolo, Claudia Laudadio, Daniela Azzollini, Grazia Marinelli, Sabino Ceci, Giulia Latini, Biagio Rapone, Alessio Danilo Inchingolo, Antonio Mancini, and et al. 2023. "Therapeutic Strategies of Primary Molar Infraocclusion: A Systematic Review" Children 10, no. 3: 582. https://doi.org/10.3390/children10030582
APA StylePatano, A., Inchingolo, A. M., Laudadio, C., Azzollini, D., Marinelli, G., Ceci, S., Latini, G., Rapone, B., Inchingolo, A. D., Mancini, A., Inchingolo, F., Di Venere, D., Tartaglia, G. M., Dipalma, G., & Malcangi, G. (2023). Therapeutic Strategies of Primary Molar Infraocclusion: A Systematic Review. Children, 10(3), 582. https://doi.org/10.3390/children10030582
















